Abstract
Background
Malaysia introduced the two dose measles-mumps-rubella (MMR) vaccine in 2004 as part of its measles elimination strategy. However, despite high historical coverage of MCV1 and MCV2, Malaysia continues to report high measles incidence. This study suggests a novel indicator for investigating population immunity against measles in the Malaysian population.
Methods
We define effective vaccine coverage (EVC) of measles as the proportion of a population vaccinated with measles-containing vaccine (MCV) and effectively protected against measles infection. A quantitative evaluation of EVC throughout the life course of Malaysian birth cohorts was conducted accounting for both vaccine efficacy (VE) and between-dose correlation (BdC). Measles vaccination coverage was sourced from WHO-UNICEF estimates of Malaysia’s routine immunisation coverage and supplementary immunisation activities (SIAs). United Nations World population estimates and projections (UNWPP) provided birth cohort sizes stratified by age and year. A step wise joint Bernoulli distribution was used to proportionate the Malaysian population born between 1982, the first year of Malaysia’s measles vaccination programme, and 2021, into individuals who received zero dose, one dose and multiple doses of MCV. VE estimates by age and doses received are then adopted to derive EVC. A sensitivity analysis was conducted using 1000 random combinations of BdC and VE parameters.
Results
This study suggests that no birth cohort in the Malaysian population has achieved > 95% population immunity (EVC) conferred through measles vaccination since the measles immunisation programme began in Malaysia.
Conclusion
The persistence of measles in Malaysia is due to pockets of insufficient vaccination coverage against measles in the population. Monitoring BdC through immunisation surveillance systems may allow for the identification of susceptible subpopulations (primarily zero-dose MCV individuals) and increase the coverage of individuals who are vaccinated with multiple doses of MCV. This study provides a tool for assessment of national-level population immunity of measles conferred through vaccination and does not consider subnational heterogeneity or vaccine waning. This tool can be readily applied to other regions and vaccine-preventable diseases.
Similar content being viewed by others
Background
Measles is a highly infectious virus in the paramyxovirus family, transmitted through respiratory droplets or particle aerosols [1] with a basic reproduction number of 12 – 18 [2]. Despite significant progress in the global reduction of measles incidence and mortality since 2000, a joint report by the World Health Organization (WHO) and the United States Centers for Disease Control and Prevention (CDC) showed that the global incidence of measles rose to the highest level in 23 years in 2019, largely driven by large outbreaks in several countries [3]. Though the reasons for these outbreaks varied on a community level, low MCV1 coverage, decreases in vaccine confidence, and unidentified immunity gaps were identified as notable drivers [3].
Progress towards measles elimination targets as defined by the 2012 Global Vaccine Action Plan (GVAP) has regressed since the global resurgence of measles in 2017 [3], and despite the decline of measles cases by 80% in 2020 compared to the prior year, the COVID-19 pandemic also saw over 22 million children miss their first dose of measles vaccine alongside a decline in surveillance activities, leading a growing risk of further measles outbreaks as immunity gaps widen [4]. The theoretical threshold of population immunity required for the interruption of measles transmission is 92–94%, meaning that even in areas of high coverage, the spatial clustering of non-vaccinated individuals poses continued risks to achieving measles elimination, as observed in the outbreaks between 2017 and 2019 [3, 5, 6].
In 2009, updated WHO guidelines recommended MCV2 vaccination for all children, ensuring that individuals who missed the first dose or did not seroconvert after the first dose received a second opportunity at protection. A review of field effectiveness of measles vaccination found the median vaccine efficacy (VE) of first dose of MCV ranged from 84% (IQR 72.0%–95.0%) to 92.5% (IQR 84.8%–97.0%) depending on age; provision of a second dose of MCV increased VE point estimates to 94–100%, justifying the current coverage targets of 95% of both MCV1 and MCV2 and MCV2 introduction [7].
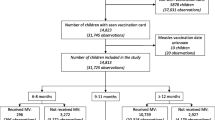
In Malaysia, the introduction of MCV1 in 1982 and MCV2 in 2004 led to a decline in measles incidence from 65.2 cases per million to 6.6 in 2013, in line with the expanded programme on immunisation and global measles elimination targets [8]. However, since 2013, increasing vaccine hesitancy and other implementation challenges have led to an increase in outbreaks, increasing incidence to 14.8 cases per million in 2020 [8, 9]. Currently, Malaysia administers MCV1 at 9 months of age and MCV2 at 12 months of age, a policy introduced in 2016 following a recommendation by the WHO [8]. Figure 1 summarises changes to the measles vaccination schedule and national measles immunisation campaigns since 1982.
Despite its public health benefits, the introduction of a second measles vaccine dose presents some programmatic challenges. In settings where there is low coverage of MCV1, implementing MCV2 routine or supplementary immunisation activities (SIAs) to increase the proportion of two-dose individuals may result in a smaller effect than reaching zero-dose MCV individuals [10]. Delayed 1st dose of MCV may also be incorrectly reported in administrative records as 2nd dose of MCV, leading to incorrect assumptions of overall population immunity [11]. Given VE, to effectively control outbreak risk, measles immunisation programmes aim to understand the relationship between zero-dose, MCV1, and MCV2 immunisation proportions in individuals [12]. To contribute to this understanding, this study suggests a novel concept—between dose correlation (BdC). It represents the correlation between whether an individual has been vaccinated previously and whether the individual will be vaccinated in the next round of immunisation activity.
For demonstration purposes, assume a cohort has been targeted in \(i-1\) immunisation activities already, and is eligible for the \({i}^{th}\) immunisation activity. A perfect positive BdC means that the \({i}^{th}\) immunisation vaccine doses are primarily allocated to individuals already vaccinated previously. A random BdC assumes an equal likelihood of being vaccinated in the \({i}^{th}\) immunisation activity regardless of whether an individual has been vaccinated previously. A perfect negative correlation claims that individuals missing the previous \(i-1\) immunisation activities are prioritised in the \({i}^{th}\) immunisation activity, resulting in fewer zero-dose individuals. With BdC, we are able to estimate the proportions of zero-dose, single-dose (or one-dose), and multiple-dose individuals for any birth cohort through time. In practice, surveillance systems are not designed to monitor BdC. Determining the relative proportions of single-, multiple- and zero-dose populations is therefore challenging. Vaccination programme managers tend to rely on aggregated subnational administrative and population data for coverage estimates [13], from which BdC is inferred.
These assumptions are critical for setting national vaccination targets and reducing the endemic transmission of measles. However, given recent outbreaks among older age groups, population immunity should be evaluated across the life course, accounting for both VE and BdC [14]. This study aims to determine the effective measles vaccine coverage (EVC) in Malaysian birth cohorts since 1982 using this approach with a particular focus on people under 18 years of age.
Methodology
Data sources
Measles routine immunisation coverage data from 1982 to 2021 in Malaysia was provided by WHO/UNICEF estimates of national immunisation coverage (WUENIC) [15], while WHO subnational campaign data was scaled to provide campaign coverage estimates at the national level. United Nations population estimates and projections (UNWPP) were used for cohort population sizes from the year 1982 until 2021 [16].
Variable definitions
Between dose correlation (BdC)
Some papers on similar themes assume random correlation between vaccination activities [17, 18]. In this study, BdC represents the correlation between whether an individual has been vaccinated previously and whether the individual will be vaccinated in the next vaccination activity.
Vaccine efficacy (VE)
The probability that vaccination offers complete lifelong protection.
Effective measles vaccination coverage (EVC)
The proportion of a population/cohort effectively vaccinated against measles, i.e. an indicator of population immunity. It discounts individuals ineffectively vaccinated, i.e. those who are vaccinated but still susceptible to infection. Waning is not considered in this paper as it is out of scope. The evaluation of EVC is cohort-based and driven by vaccination coverage, BdC, and VE.
Methods
The methodological basis for this evaluation was developed by the Vaccine Impact Modelling Consortium (VIMC) [19]. In the VIMC methodology, BdC is dependent on the number of doses an individual has been vaccinated with. In this paper, we simplify this by assuming the BdC is only related to whether an individual has been vaccinated previously. R programming software (version 4.0.2) was used for data management, analysis, and visualization.
Measles routine immunisation coverage estimates, i.e. MCV1 and MCV2, are sourced from the WHO routine immunisation data portal. Subnational supplementary immunisation activity (SIA) coverage estimates are scaled to the national level using vaccination doses divided by target population size. Vaccination doses through SIAs in the same year are aggregated assuming doses are allocated to different regions of a country. The target population size is defined through UNWPP estimates of population size by birth cohort and year.
To determine EVC of measles derived from vaccination in the Malaysian population, we first used a stepwise joint Bernoulli distribution to cluster individuals into those who have received zero, one, or multiple doses of measles vaccine, accounting for BdC. We then applied VE estimates to the clustered population to estimate EVC. Details of the approach are as follows.
For a birth cohort of interest, assume they (will) have benefited from \(i \in \{1,...,K\}\) immunisation activities. We intend to cluster the cohort into zero-dose, single-dose (or one-dose), and multiple-dose populations through their life course. Denote random variables: \({V}_{i-1}\) as whether an individual is vaccinated in any of the first \(i-1\) immunisation activities, \({M}_{i-1}\) as whether an individual is vaccinated with multiple doses through the first \(i-1\) immunisation activities, and \({N}_{i}\) as whether an individual is vaccinated in the \({i}^{th}\) immunisation activity. Each of the three random variables follows a Bernoulli distribution. Assume the probability of each variable are \({v}_{i-1}\), \({m}_{i-1}\) and \({n}_{i}\), which represents the proportion of individuals vaccinated in the first \(i-1\) immunisation activities, the proportion of multiple-dose population after the first \(i-1\) immunisation activities, and vaccination coverage of the \({i}^{th}\) immunisation activity.
Further denote joint Bernoulli distributions \(F({V}_{i-1},{N}_{i},{\theta }_{1})\) and \(F({M}_{i-1},{N}_{i},{\theta }_{2})\), where \({\theta }_{1}\) and \({\theta }_{2}\) are corresponding BdC. In this study, we make a simplification on BdC by assuming \({\theta }_{1}={\theta }_{2}\). That means whether an individual is vaccinated in the \({i}^{th}\) immunisation activity is only dependent on if the individual has been vaccinated previously. We use these joint distributions to estimate vaccine coverage \({v}_{i}\) and multiple-dose proportion \({m}_{i}\). Zero- and Single-dose proportions are calculated as \({z}_{i}={1-v}_{i}\) and \({s}_{i}={v}_{i}-{m}_{i}\), respectively.
Set \({s}_{0}={m}_{0}={v}_{0} = 0\), we cluster a cohort into zero-, single- and multiple-dose categories for each \(i\) step-wisely. Further taking into account vaccine efficacy (VE), effective vaccine coverage (EVC) can be calculated through \(EV{C}_{i} ={s}_{i}*V{{E}^{s}}_{i}+{m}_{i}*V{{E}^{m}}_{i}\), where \(V{E}^{s}\) and \(V{E}^{m}\) represent single-dose and multiple-dose vaccine efficacy.
BdC data disaggregated by country is scarce, and in practice, ranges between -1 to 1 in the population due to varying vaccination strategies based on local context. As such, we conducted a sensitivity analysis by sampling 1,000 sets of BdC and VE values from distributions from available literature [7]. Table 1 and Table 2 depict the characteristics of input parameters for BdC and vaccine efficacy, respectively.
Results
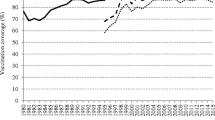
From 2005 to 2021, after the change to MCV1 administration from 12 to 9 months, our findings show that the proportion of children under 18 with multiple measles vaccine doses rises gradually from 45.9% (IQR 43.7—49.4%) to 56.8% (IQR 56.4—57.4%). Although Malaysia has had high MCV1 and MCV2 coverage (84–98%) since 2005, the proportion of multiple-dose population in the under-18 s is relatively low (< 60%). This is mainly due to the fact that MCV2 was introduced targeting age 7, and only shifted to age 1 from 2016. Specifically, cohorts born between 2010 and 2015 (age 6 to 11 by year 2021) are predominantly vaccinated with only one dose of MCV by year 2021. Concurrently, the number of children under 18 with a single dose decreases from 50.1% (IQR 43.0—54.4%) in 2005 to 42.2% (IQR 40.8—42.9%) in 2021 with the number of zero-dose children decreasing from 4.0% (IQR 1.9—7.6%) to 1.1% (IQR 0.6—1.9%) during the same period. The single dose population was only larger than the multi-dose population in the first year of MCV2 introduction in 2004, and Malaysia has consistently maintained > 95% coverage of children under 18 years of age receiving at least one dose of measles vaccination since the year 2005 in this subpopulation (Table 3). In the 17 years since the introduction of MCV2, national SIAs, and subnational SIAs, the single dose population has decreased by 15.77%.
There was a steady rise in under-18 s EVC from 1982 until 2003, followed by a sharp rise from 70.0% (60.6–79.1%) to 83.0% (75.9–90.1%) in 2004. Despite continued periods of increase in EVC following 2004, EVC never reaches the required 95% herd immunity target in children under 18 (Fig. 2).
The heatmap shown in Fig. 3 represents the relative levels of immunity of birth cohorts from 1982–2021 based on mean EVC values. Overall, the EVC of the Malaysian population represented here improves over time. The age at which mean EVC shifted to above 80% was between ages seven and fifteen prior to 2004; this has decreased to age one starting in 2011.
Figure 4 shows the upper bound of 95% interquartile range of EVC in the Malaysian population, where some cohorts have crossed the 95% population immunity threshold beginning 2004, after the introduction of MCV2.
Discussion
The Western Pacific Regional Plan of Action for Measles Elimination (2003) aims to ‘achieve and maintain 95% population immunity to measles in each birth cohort within each district of each country in the Region’ as one of its three main strategies towards measles elimination [20]. This is the first study that aims to do so by evaluating immunity conferred from measles vaccination in Malaysian birth cohorts throughout the life course. Our findings show that the Effective Vaccination Coverage (EVC) throughout the life course of Malaysian birth cohorts since 1982 is below the 95% immunity target threshold required to achieve measles elimination, contributing to the persistence of measles in Malaysia.
This study provides an assessment of national-level population immunity of measles, and does not consider subnational heterogeneity or vaccine waning. Additionally, there is no published literature as yet on national-level serological assessments of measles immunity. However, district and national laboratory serological assessments are available for comparison. One subnational study collected results of measles seroassays from September 2014 to January 2015 from government health clinics in a Malaysian district, r; here, individuals aged 15 to 24 years old showed a 74% positive titre (95% CI 70–78%) and children aged 6 to 9 years old showed 90% positive titre (95% CI 87–94%) [21]. A prior study conducted in the year 2008 using measles samples from Malaysian hospitals showed that 82.8% of individuals above the age of seven were seropositive for measles [22]. Malaysia has consistently reported more than 95% coverage of MCV1 and MCV2 in most years since 1982, yet the observations in this study and previous serological assessments show WUENIC estimates may not be the most accurate representation of measles population immunity in the country.
In 2013, updated guidelines for measles elimination were published by WPRO to recommend that countries ‘achieve and maintain > 95% vaccination coverage of two doses of MCV through routine immunisation, adding SIAs when required’ [23]. We find that the Malaysian population immunity conferred through measles vaccination increased significantly through the introduction of MCV2 and national immunisation campaigns. As noted in this study, a larger proportion of individuals receive MCV2 beginning in 2004; given that efficacy of measles vaccination improves with subsequent doses, EVC improves in these birth cohorts. Our findings corroborate this, showing that in 2.5% of samples, i.e. the best-case scenario, EVC crosses the 95% threshold. However, the study also finds that there is still a significant proportion of individuals in Malaysia who have not received any measles vaccination or only received MCV1.
These ‘best-case scenario’ findings, driven by higher vaccine efficacy, between dose coverage (BdC), proportion of individuals with MCV2, and a lower proportion of zero-dose individuals, represents the strategy required for immunisation programmes to meet the 95% threshold for measles control. Achieving these outcomes, however, requires immunisation programme capacity to monitor BdC. Since 1982, Malaysia has made significant strides towards the elimination of measles, implementing evidence-based vaccination policies that have resulted in a decreased burden. However, Malaysia is reliant on paper-based mechanisms for immunisation coverage reporting [24]. Paper-based systems depend on the aggregated facility or district-level data, and may be subject to delays or lags. This results in overreporting of estimates and increases the risk of unreadable, missing, or inconsistent vaccination coverage data. Electronic immunisation registries (EIR) circumvent these issues, especially ones that are interoperable with other electronic systems that handle patient records and civil registration systems for more accurate population and vaccine dose data [25, 26]. For Malaysia, a country aiming for measles elimination, the objective is to maintain high coverage and BdC through routine immunisation with periodic SIAs to cover immunity gaps. Conversely, in a country with a high burden of measles and low MCV1 coverage looking to achieve disease control, decorrelating measles vaccination doses provides a greater opportunity for zero-dose individuals to receive MCV1.
However, the implementation of a mechanism for monitoring BdC must consider contextual health system factors and feasibility. Developing health information management systems is costly and laborious, butalleviate user workload when compared to traditional paper-based systems [27, 28]. In this regard, there have been examples of innovative mixed paper and electronic immunisation registries that have shown promise in low-resource settings. Given the budgetary, infrastructural, and technical considerations at the national level in most digital health projects, it remains to be seen if this technology can be scalable [29].
There are several methodological strengths in this study. The use of probability theory to proportionate the population by the number of doses provides an opportunity to account for BdC in settings that do not have a mechanism for its monitoring. It also estimates the zero-dose population and gives insight into the effectiveness of SIAs in vaccinating susceptible populations. This is important as relying solely on vaccination coverage data may underestimate the proportion of susceptible individuals, as individuals with MCV1 may be subject to re-vaccination in these campaigns [30]. Future research should explore the age distribution of measles cases within the Malaysian population and correlate the findings of EVC by birth cohorts at the district level. This will better inform programme managers on the need for age-targeted immunisation campaigns as well as serological studies to evaluate population immunity against measles. This methodology provides flexibility in application, as it can be used for other multi-dose vaccination programmes.
Depending on the type of vaccine and efficacy data available, incorporating primary vaccination failure as a function of the methodology may need to be considered in subsequent research. This study uses the ‘all-or-nothing’ approach to define measles vaccine efficacy, and does not consider the waning of immunity conferred through vaccination as it does not play a significant role in measles transmission [31]. Future research should build upon the aforementioned aspects in order to provide more reliable estimates on the effectiveness of measles vaccination in a given population.
Uncertainty within our findings may stem from our use of UNWPP estimates of population demography and vaccination coverage estimates, given that the study methodology matched these estimates to immunisation data to allow for temporal analysis of population immunity. This may result in an overestimation or underestimation of the target population given that these are external sources of population estimates, and not in-country demographic statistics used by measles vaccine programme managers in Malaysia. Target population estimates influence the precision of vaccination coverage figures significantly, and increasingly so in settings with higher coverage levels [32]. Further, the temporal EVC changes seen within the population are based on vaccination delivery occurring as per the routine immunisation schedule. This may not necessarily reflect the situation in real life [33, 34]. Delays in vaccination administration may result in a child being part of the susceptible group for a longer period, shifting changes in EVC values in birth cohorts to higher age groups. Future research should explore the timeliness of measles vaccination to determine the proportion of children who receive measles immunisation at the recommended age.
Infants have protection from maternal antibodies against measles infection which wanes around 6 months from birth. The first dose of routine measles vaccination (MCV1) is usually given to infants at 9 months old. The methodology proposed in this paper does not account for maternal protection and the gap between its waning and the first dose of MCV vaccination, because this paper is primarily interested in vaccine induced immunity. Immunity induced by natural infection is also out of the scope in this paper. To be able to account for disease induced immunity, additional input of age specific measles cases and deaths are required. We consider this as a future research topic.
Conclusion
While Malaysia has made considerable progress towards measles elimination, this study concludes that the current measles vaccination strategy in Malaysia has not conferred 95% population immunity in any of the Malaysian birth cohorts throughout the life course since 1982. Despite consistently maintaining > 95% MCV1 coverage of children under 18 years of age since the year 2005, Malaysia still reports measles cases. These findings highlight the need for the incorporation of BdC monitoring mechanisms into measles immunisation surveillance systems in Malaysia. Identifying immunity gaps and susceptible subpopulations will remain critical for immunisation programme strengthening.
Availability of data and materials
Measles vaccination coverage data was gathered from the World Health Organisation database. Available from: https://immunizationdata.who.int/pages/coverage/mcv.html.
Malaysia population prospects was gathered from the Population Division, United Nations database. Available from: https://population.un.org/wpp/.
Abbreviations
- BdC:
-
Between-dose Correlation
- CDC:
-
United States Centers for Disease Control and Prevention
- EPI:
-
Expanded Programme on Immunisation
- EVC:
-
Effective Vaccine Coverage
- GAVI:
-
Gavi, The Vaccine Alliance
- JRF:
-
Joint Reporting Form
- MCV1:
-
Measles-containing-vaccine first-dose
- MCV2:
-
Measles-containing-vaccine second-dose
- MMR:
-
Measles-Mumps-Rubella
- SIA:
-
Supplementary Immunisation Activities
- UNICEF:
-
United Nations Children’s Fund
- UNWPP:
-
United Nations Population Estimates and Projections
- VPD:
-
Vaccine-preventable Diseases
- WHO:
-
World Health Organization
- WPRO:
-
World Health Organization Regional Office for the Western Pacific
- WUENIC:
-
World Health Organization and United Nations Children’s Fund estimates of national immunization coverage
References
Laksono BM, de Vries RD, McQuaid S, Duprex WP, de Swart RL. Measles Virus Host Invasion and Pathogenesis. Viruses. 2016;8(8):210.
Guerra FM, Bolotin S, Lim G, Heffernan J, Deeks SL, Li Y, et al. The basic reproduction number (R0) of measles: a systematic review. Lancet Infect Dis. 2017;17(12):e420–8.
Patel MK. Progress Toward Regional Measles Elimination — Worldwide, 2000–2019. MMWR Morb Mortal Wkly Rep. 2020;69. Available from: https://www.cdc.gov/mmwr/volumes/69/wr/mm6945a6.htm. Accessed 24 Aug 2021.
Dixon MG, Ferrari M, Antoni S, et al. Progress Toward Regional Measles Elimination — Worldwide, 2000–2020. MMWR Morb Mortal Wkly Rep. 2021;70:1563–9. https://doi.org/10.15585/mmwr.mm7045a1.
Moss WJ, Shendale S, Lindstrand A, O’Brien KL, Turner N, Goodman T, et al. Feasibility assessment of measles and rubella eradication. Vaccine. 2021;39(27):3544–59.
Fine P, Eames K, Heymann DL. “Herd Immunity”: A Rough Guide. Clin Infect Dis. 2011;52(7):911–6.
Uzicanin A, Zimmerman L. Field Effectiveness of Live Attenuated Measles-Containing Vaccines: A Review of Published Literature. J Infect Dis. 2011;204(suppl_1):S133-149. Available from: https://academic.oup.com/jid/article/204/suppl_1/S133/2193498. Accessed 6 Aug 2021.
Rahman NAA, Ismail WRW, Rahman RA, Yusof MP, Idris IB. Who Would Get Measles in Petaling District? A Trend Analysis of Measles Outbreak From 2014–2018. Mal J Med Health Sci. 2020;16(3):67–72.
World Health Organization. Regional Office for the Western Pacific. Measles-Rubella Bulletin 2021. Manila: WHO Regional Office for the Western Pacific; 2021.
Cutts FT, Dansereau E, Ferrari MJ, Hanson M, McCarthy KA, Metcalf CJE, et al. Using models to shape measles control and elimination strategies in low- and middle-income countries: A review of recent applications. Vaccine. 2020;38(5):979–92.
Yitbarek K, Tilahun T, Debela T, Abdena D, Girma T. Measles epidemiology and vaccination coverage in Oromia Region, Ethiopia: Evidence from surveillance, 2011–2018. Vaccine. 2021;39(31):4351–8.
McKee A, Ferrari MJ, Shea K. Correlation between measles vaccine doses: implications for the maintenance of elimination. Epidemiol Infect. 2018;146(4):468–75.
Brown DW. Definition and use of “valid” district level vaccination coverage to monitor Global Vaccine Action Plan (GVAP) achievement: evidence for revisiting the district indicator. J Glob Health. 2018;8(2):020404.
Dissecting the indirect effects caused by vaccines into the basic elements. 2015. p. 2142–57.
WHO/UNICEF estimates of national immunization coverage. Available from: https://www.who.int/teams/control-of-neglected-tropical-diseases/yaws/diagnosis-and-treatment/immunization-analysis-and-insights. Accessed 4 Sept 2021.
World Population Prospects - Population Division - United Nations. Available from: https://population.un.org/wpp/. Accessed 4 Sept 2021.
Plans-Rubió P. Vaccination Coverage for Routine Vaccines and Herd Immunity Levels against Measles and Pertussis in the World in 2019. Vaccines. 2021;9(3):256. https://doi.org/10.3390/vaccines9030256.
Plans-Rubió P. Are the Objectives Proposed by the WHO for Routine Measles Vaccination Coverage and Population Measles Immunity Sufficient to Achieve Measles Elimination from Europe? Vaccines. 2020;8(2):218. https://doi.org/10.3390/vaccines8020218.
Vaccine Impact Modelling Consortium. Clustering vaccine coverage and estimating the indirect benefits of immunisation - an introduction to methodology. Available from: https://www.vaccineimpact.org/resources/. Accessed 13 Mar 2022.
World Health Organization. Western Pacific Regional Plan of Action For Measles Elimination. 2003. Available from: https://apps.who.int/iris/handle/10665/207572. Accessed 4 Sept 2021.
Hazlina Y, Marlindawati MA, Shamsuddin K. Serological assessment of the establishment of herd immunity against measles in a health district in Malaysia. BMC Infect Dis. 2016;16(1):740.
Saraswathy TS, Zahrin HN, Norhashmimi H, Az-Ulhusna A, Zainah S, Rohani J. Impact of a measles elimination strategy on measles incidence in Malaysia. Southeast Asian J Trop Med Public Health. 2009;40(4):742–7.
World Health Organization. Measles elimination field guide. Available from: https://apps.who.int/iris/rest/bitstreams/920747/retrieve. Accessed 24 Aug 2021.
World Health Organization. Fourth Biregional Cross-border Meeting on Polio, Measles, Rubella and Other Vaccine Preventable Diseases. 2019. Available from: https://apps.who.int/iris/bitstream/handle/10665/333047/RS-2019-GE-55-MYS-eng.pdf?sequence=1&isAllowed=y. Accessed 24 Aug 2021.
Immunization Data: Evidence for Action. A Realist Review of What Works to Improve Data Use for Immunization, Evidence from Low- and Middle Income Countries. Seattle: PATH; Washington, DC: PAHO; 2019.
Scobie HM, Edelstein M, Nicol E, Morice A, Rahimi N, MacDonald NE, et al. Improving the quality and use of immunization and surveillance data: Summary report of the Working Group of the Strategic Advisory Group of Experts on Immunization. Vaccine. 2020;38(46):7183–97.
Heidebrecht CL, Quach S, Pereira JA, Quan SD, Kolbe F, Finkelstein M, et al. Incorporating Scannable Forms into Immunization Data Collection Processes: A Mixed-Methods Study. PLoS ONE. 2012;7(12):e49627.
Adams WG, Conners WP, Mann AM, Palfrey S. Immunization Entry at the Point of Service Improves Quality, Saves Time, and Is Well-Accepted. Pediatrics. 2000;106(3):489–92.
Kelley LT, Fujioka J, Liang K, Cooper M, Jamieson T, Desveaux L. Barriers to Creating Scalable Business Models for Digital Health Innovation in Public Systems: Qualitative Case Study. JMIR Public Health Surveill. 2020;6(4):e20579.
Lessler J, Metcalf CJE, Grais RF, Luquero FJ, Cummings DAT, Grenfell BT. Measuring the Performance of Vaccination Programs Using Cross-Sectional Surveys: A Likelihood Framework and Retrospective Analysis. PLoS Med. 2011;8(10):e1001110.
Gastañaduy PA, Funk S, Lopman BA, Rota PA, Gambhir M, Grenfell B, et al. Factors Associated With Measles Transmission in the United States During the Postelimination Era. JAMA Pediatr. 2020;174(1):56–62.
World Health Organization. Assessing and Improving the Accuracy of Target Population Estimates for Immunization Coverage. Available from: https://www.who.int/immunization/monitoring_surveillance/data/Denominator_guide.pdf. Accessed 4 Sept 2021.
Hu Y, Wang Y, Chen Y, Liang H, Chen Z. Measles vaccination coverage, determinants of delayed vaccination and reasons for non-vaccination among children aged 24–35 months in Zhejiang province, China. BMC Public Health. 2018;27(18):1298.
Bielicki JA, Achermann R, Berger C. Timing of Measles Immunization and Effective Population Vaccine Coverage. Pediatrics. 2012;130(3):e600–6.
Acknowledgements
The methodology for this project was developed by the Science and Policy team at the Vaccine Impact Modelling Consortium, a research group that models the impact of vaccination programmes globally.
Funding
This work was carried out as part of the Vaccine Impact Modelling Consortium (VIMC, www.vaccineimpact.org). VIMC is jointly funded by Gavi, the Vaccine Alliance, and by the Bill Melinda Gates Foundation. The views expressed are those of the authors and not necessarily those of the Consortium or its funders. The funders were given the opportunity to review this paper prior to publication, but the final decision on the content of the publication was taken by the authors. Consortium members received funding from Gavi and BMGF via VIMC during the course of the study. This work was supported, in whole or in part, by the Bill & Melinda Gates Foundation, via the Vaccine Impact Modelling Consortium (Grant Number OPP1157270 / INV-009125). AMH, XL, KAMG also acknowledge funding from the MRC Centre for Global Infectious Disease Analysis (reference MR/R015600/1), jointly funded by the UK Medical Research Council (MRC) and the UK Foreign, Commonwealth Development Office (FCDO), under the MRC/FCDO Concordat agreement and is also part of the EDCTP2 programme supported by the European Union; and acknowledge funding by Community Jameel.
Author information
Authors and Affiliations
Contributions
Shurendar Selva Kumar: Methodology, Formal analysis, Data curation, Writing- original draft, Writing- review and editing, Visualisation; Anna-Maria Hartner: Methodology, Writing- original draft, Writing- review and editing; Arunah Chandran: Data curation, Validation, Writing- review and editing; Katy Gaythorpe: Conceptualisation, Methodology, Validation, Formal analysis, Data curation, Writing- original draft, Writing- review and editing, Supervision, Project administration, Funding acquisition; Xiang Li: Conceptualisation, Methodology, Software, Validation, Formal analysis, Investigation, Data curation, Writing- original draft, Writing- review and editing, Supervision.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kumar, S.S., Hartner, AM., Chandran, A. et al. Evaluating effective measles vaccine coverage in the Malaysian population accounting for between-dose correlation and vaccine efficacy. BMC Public Health 23, 2351 (2023). https://doi.org/10.1186/s12889-023-17082-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-023-17082-9