Abstract
Introduction
Dolutegravir (DTG)-based regimen was included in the expanded formulary of China's National Free Antiretroviral Treatment Program at the end of 2021. Yet high price of DTG and lack of health economic evaluation in China present barriers for implementation of the regimen. The study aims to investigate the lifetime cost-effectiveness of DTG-based regimen for treatment-naive HIV infection in China.
Methods
A decision-analytic Markov model was used to obtain the costs and effectiveness of four regimens: Arm A, efavirenz (EFV)-based regimen; Arm B, DTG-based regimen; Arm C, elvitegravir/cobicistat/tenofovir alafenamide/emtricitabine (EVG/c/FTC/TAF) regimen; Arm D, abacavir/lamivudine/dolutegravir (ABC/3TC/DTG) regimen. The potential impact of national centralized drug procurement policy was assessed in scenario analysis. The results were further validated through sensitivity analysis.
Results
Compared with other three regimens, DTG-based regimen led to the fewest cumulative adverse reactions, opportunistic infections and deaths. Compared with EFV-based regimen, the base-case ICERs for DTG-based regimen were 13,357 (USD/QALY) and 13,424 (USD/QALY) from the healthcare system and societal perspective respectively. In the policy scenario analysis with the procurement price of DTG equal to that of LPV/r, DTG-based regimen would be dominant. The model results remained robust in sensitivity analyses.
Conclusions
DTG-based regimen for treatment-naive patients is likely to be cost-effective and deserve wider implementation in China. This study strongly suggests the centralized procurement of DTG to minimize cost and maximize cost-effectiveness.
Similar content being viewed by others
Background
The pilot for the China's National Free Antiretroviral Treatment Program (NFATP) began in Henan province in 2002, and the program fully began in 2003 [1]. Free first-line regimen for antiretroviral treatment (ART) is efavirenz (EFV) or nevirapine (NVP) + tenofovir disoproxil fumarate (TDF) or zidovudine (AZT) + lamivudine (3TC) [2]. This program has contributed greatly to case fatality rate reduction and life quality improvement [3]. However, there are ongoing challenges, including adverse reactions, drug resistance, and complications. A cohort study conducted on patients who had used free antiretroviral drugs for 4 or 5 years found that 69.9% of the patients had at least one adverse drug reaction [4].
In 2019, World Health Organization (WHO) [5] recommended dolutegravir (DTG, an integrase strand transfer inhibitor)-based regimens as the preferred first-line antiretroviral regimen for adults and adolescents because of the high potency and barrier to resistance, low incidence of adverse reactions, and virologic failure. DTG-based regimen was also the first-line antiretroviral regimen recommended by the United States and Europe [6] [7]. By the end of 2021, DTG was covered under the national free AIDS antiretroviral drug list in China [8]. This initiative not only provided an alternative for patients with severe central nervous system (CNS) symptoms and hepatotoxicity caused by EFV, but also ensured drug change for patients with multi-resistance of nucleoside and non-nucleoside reverse transcriptase inhibitors. However, DTG is still in the planning of centralized government procurement, and the average price per person-year for DTG is still as high as about USD 1 700 [9], far higher than the global price (USD 85 in lower-middle-income countries and USD 183 in upper-middle-income countries [10]), which may be the fundamental reason why DTG has not been really popularized in China (the utilization rate of DTG in first-line antiretroviral therapy is less than 3% in China). Considering the limited national budget for free drugs, economy is also an important criterion for drug selection in addition to drug effectiveness and safety. Although studies in Africa [11], France [12], India [13], Italy [14], Canada [15] and other countries have also confirmed that DTG was more cost-effective than EFV. The long-term economic value of DTG in the Chinese context has not been investigated previously.
The study aims to evaluate the lifetime cost-effectiveness of two first-line regimens (EFV-based regimen, DTG-based regimen) and two self-paying regimens for treatment-naive HIV infection from both health-care system and societal perspectives. Further, the study aims to explore the potential impact of national centralized drug procurement policy (NCDP) on the regimen selection.
Methods
Data sources
Details of costs and utilities, and clinical parameters were collected based on clinical data (from a designated AIDS hospitals in Jiangsu province [Nantong No.3 hospital affiliated to Nantong University], from November 2015 to November 2020, N = 2,934), government documents, published literature and expert opinions (four experienced clinical experts and several HIV-infected patients were interviewed). This study followed the recommendations of the Consolidated Health Economic Evaluation Reporting Standards (CHEERS) reporting guideline [16]. The study was approved by the Medical Ethics Committee of Nantong University (Approval number: No. [2020] 4). All participants signed an informed consent form.
Model structure
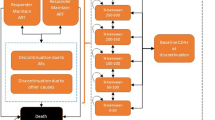
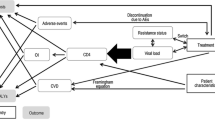
A decision-analytic Markov model was built in this study, which consisted of a decision tree (Fig. 1A) reflecting the 4 regimens: Arm A: the current first-line free regimens (EFV-based regimen [EFV + TDF or AZT + 3TC], converted to LPV/r-based regimen [LPV/r + AZT or TDF + 3TC] in the fifth year); Arm B: DTG-based regimen (DTG + TDF + 3TC, has been incorporated into the national free AIDS antiretroviral drug list, to be implemented); Arm C: EVG/c/FTC/TAF (Genvoya, self-paying); Arm D: ABC/3TC/DTG (Triumeq, self-paying).
In China in 2020, there were about 81,000 newly-diagnosed HIV-infected individuals [17], among whom 92% initiated first-line ART during the same year [18]. Thus, it was assumed that the age at the start of the ART was 30 years old [19].Therefore, the cohort was set with 75,000 patients at the age of 30 years who initiated antiretroviral treatment (ART) following diagnosis of HIV infection per year. Due to the chronic condition of HIV/AIDS, a lifetime horizon of 40 years was applied, assuming a total lifetime expectancy of 70 years (life expectancy among people with HIV receiving ART were within 10 years of those of the general population [20], which is 76 years in China [21]). The Markov model consisted of four CD4 states (< 200, 200–349, 350–499, and 500- cells/μL) and one absorbing mortality state. The initial CD4 distribution were set as < 200: 30%, 200–349: 30%, 350–499: 20%, and 500-: 20% [22]. It was assumed that the CD4 states can only maintain the original state, transfer to the adjacent state, or directly lead to death in one cycle (one year), according to the related studies results that the CD4 cell counts of patients who receive ART can increase by approximately 150 cells/μL every year on average [23]. Figure 1B shows the transitional relationship between Markov states. TreeAge Pro 2021 (TreeAge Software, LLC, Williamstown, Massachusetts, USA) was used to build the model, and the cycle period was defined as one year with half cycle correction.
The main model outcomes included HIV-related health outcomes; total costs; QALYs; and incremental cost-effectiveness ratios (ICERs). Costs and ICERs were reported in 2020 US dollars. According to the WHO standard [24], cost-effectiveness was determined based on whether ICER was smaller than three times China’s GDP per capita (USD 31 241 in 2020) [25].
Model inputs
From the societal perspective, the following cost items were considered in the model: (1) Direct medical costs, including ARV, testing, treatment of adverse reactions, and opportunistic infections; (2) direct non-medical costs, including transportation, accompanying care, and nutrition; (3) and indirect costs, including work stoppage. The human capital approach (HCA) [26] was used to calculate indirect costs, as follows [26]: indirect cost = wage standard × loss of working time. The wage standard was the per capita disposable income of national residents in 2020 [25]. The loss of working time was the average days of hospital stay per year, which were obtained from the hospital clinical data. All costs were converted to the values in 2020 using the Chinese consumer price index (CPI) [25], and were converted to US dollars at an exchange rate of 6.8974 Chinese yuan per dollar [21]. Further details of the costs are provided in the Table 1. The health-care system perspective only included the direct medical costs (eTable 1 in the Supplementary Data).
QALY was used as the utility measurement. The utility values (Table 2) were associated with four CD4 states, adverse reactions, and opportunistic infections. Costs and utility values were analyzed at a discount rate of 5% per annum [29].
The transition between different states was reflected by the transition probability, including the change rate of CD4 count status and mortality (Table 3). The change rate of CD4 count status were estimated by clinical experts according to the virological inhibition rate and the patient’s immunological reestablishment [33]. The cumulative transition probability was converted into the annual transition rate using the formula [34] \(r=[-\mathrm{log}\left(1-prob\right)]/t\) (r, annual incidence rate; prob, cumulative transition probability for t years). The instantaneous incidence rate for each event was converted into the annual transition probability included in the model using the formula [35] \(p=1-\mathrm{exp}(-r*t)\) (p, annual transition probability; r, annual incidence rate; t, time,). Other parameters that reflected the effects of regimens included incidences of adverse reactions, and opportunistic infections (eTable2 in the Supplement Data).
Scenario and sensitivity analyses
In 2021, Chinese government issued the National Centralized Drug Procurement (NCDP) policy for drug price and cost control [8]. We conducted a policy scenario assuming the procurement price of DTG equal to that of LPV/r. The stability of the model was evaluated by one-way sensitivity analysis and probabilistic sensitivity analysis (PSA) for all parameters. The ranges of parameters for one-way sensitivity analysis were based on maximum and minimum values reported in the literature, when available. For unavailable ranges, the values of ± 25% were adopted. Using a second-order Monte Carlo simulation (5,000 iterations), PSA was performed to examine the effects of all parameters’ distributions. Further information on the parameter range and distribution is provided in Tables 1, 2 and 3.
Results
Clinical outcomes
Based on the simulated cohort of 75,000 HIV infection, over lifetime horizon, 30,790 cases of death occurred in arm B (DTG-based regimen), reducing 9,729 cases than arm A (the free regimen); 82,734 cases of adverse reactions occurred in arm B, reducing 546,678 cases than arm A; 50,677 cases of opportunistic infections occurred in arm B, reducing 31,254 cases than arm A. The HIV-related health outcomes of Arm C (Genvoya) and arm D (Triumeq) were inferior to that of arm B, with more cases of deaths, adverse reactions, and opportunistic infections (Table 4).
Cost and cost-effectiveness outcomes
Pairwise incremental analysis (cost and effectiveness comparisons between two arms) were conducted based on the China Guidelines for Pharmacoeconomic Evaluations (2020) [29], from the health-care system perspective. First, all arms were ranked according to their costs, from low to high, that is, USD 1,181,508,179, USD 2,384,721,209, USD 3,003,817,442, and USD 6,024,007,347 for arms A, B, C, and D, respectively. Second, an incremental analysis was conducted between arms C and D because of their higher costs; arm D costs more than arm C (6,024,007,347 > 3,003,817,442) but with fewer QALYs (954,888 < 968,102). As arm D was a more strictly dominated regimen, it was eliminated first. Subsequently, arms C and B were compared; arm C cost more than arm B (3,003,817,442 > 2,384,721,209), but with fewer QALYs (968,102 < 972,746); therefore, arm C was eliminated. Finally, for the remaining arms A and B, arm B increased total costs by USD 1,203,213,030 and QALYs by 972,746, with an ICER of 13,357 (USD/QALY), which was smaller than three times GDP per capita of USD 31,241, indicating that the increased cost of arm B was worthwhile. Thus, arm B (the last regimen retained from all incremental analyses) was the most cost-effective regimen (see Table 5). In terms of cost-effectiveness, arm C (Genvoya) and arm D (Triumeq) were generally inferior to arm B.
Similarly, from the societal perspective, arm D and arm C were strictly dominated regimen and were eliminated from the ranking in turn. Arm B increased total costs by USD 1,209,292,998 and QALYs by 90,083, with an ICER of 13,424 (USD/QALY). Arm B was the most cost-effective regimen.
Scenario and sensitivity analyses
In a scenario analysis assuming three self-paying regimens were included in the national free AIDS antiretroviral drug list, at a price on parity with LPV/r, it significantly reduced the total costs of arms B, C, and D. Arm B resulted in a dominant regimen, with lower costs and greater QALYs than all other arms from the health-care system and societal perspectives (Table 5).
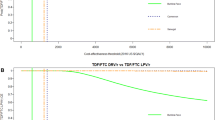
The model results remained robust in sensitivity analyses. From health-care system and societal perspective, one-way sensitivity analysis suggested that the variables that had a significant association with ICER (arm A vs arm B) were the CD4 increase rate for arm B, drug price of arm B, and utility of the CD4 > 500 patients (Fig. 2A, B). Notably, all ICERs were less than three times China’s GDP per capita (USD 31,241) during one-way sensitivity analysis. In PSA, after a second-order Monte Carlo simulation (5,000 iterations), the cost-effectiveness acceptability curve (Fig. 2E, F) showed the probability of the four arms being cost-effective in a range of willingness-to-pay (WTP). Considering a WTP of three times of China’s GDP per capita (USD 31,241), arm B had 58.11% probability of being cost-effective among four arms from the health-care system perspective (Fig. 2E), and 56.81% probability of being cost-effective among four arms from the societal perspective (Fig. 2F). Moreover, an incremental cost-effectiveness scatterplot (Fig. 2C, D) of arm B vs arm A was conducted, which found that there was 67.72% probability that arm B was cost-effective versus arm A at a WTP USD 31,241 from the health-care system perspective (Fig. 2C), and 65.85% probability from the societal perspective (Fig. 2D). Therefore, we could consider arm B to be the most cost-effective option. One-way sensitivity analysis and incremental cost-effectiveness scatterplot of arm B vs arm C and arm B vs arm D were shown in eFigure1-eFigure 2 (in the Supplementary Data).
A One-way sensitivity analysis (arm B vs arm A), health-care system perspective. B One-way sensitivity analysis (arm B vs arm A), societal perspective. C Incremental cost-effectiveness scatterplot (arm B vs arm A), health-care system perspective. D Incremental cost-effectiveness scatterplot (arm B vs arm A), societal perspective. E Cost-effectiveness acceptability curve, health-care system perspective. F Cost-effectiveness acceptability curve, societal perspective
Discussion
Although DTG has been included in the national AIDS free drug list at the end of 2021, it still takes some time and effort to implement the national centralized procurement. The average price per person-year for DTG is still as high as about USD 1,700 [9], far higher than the global price (USD 85 in lower-middle-income countries and USD 183 in upper-middle-income countries [10]), which may be the fundamental reason why DTG has not been really popularized in China (the proportion of DTG in first-line antiretroviral therapy is less than 3% in China). The study aims to evaluate the lifetime cost-effectiveness of DTG-based regimen for treatment naive HIV infection from societal and health-care system perspective, and to simulate the influence of price change on cost-effectiveness after the update of the list. The study aims to evaluate the lifetime cost-effectiveness of DTG-based regimen for treatment naive HIV infection from societal and health-care system perspective, and to simulate the influence of price change on cost-effectiveness after the implementation of centralized procurement.
In this study, a decision-analytic Markov model was developed to compare the lifetime cost-effectiveness of the existing free regimens (EFV-based regimen, converted to LPV/r-based regimen in the fifth year) and three self-paying regimens (DTG-based regimen, Genvoya, and Triumeq) for treatment-naive HIV infection, from a societal perspective. The results showed that DTG-based regimen significantly reduced the cases of deaths, adverse reactions, and opportunistic infections. From the health-care system and societal perspective, DTG-based regimen resulted in ICERs of 13,357 (USD/QALY) and 13,424 (USD/QALY) compared with the free regimen, respectively. In a scenario analysis assuming three self-paying regimens were simulated in the national free AIDS antiretroviral drug list at the price of parity to LPV/r, DTG-based regimen was a dominant regimen, with lower costs and greater QALYs than all comparators. These findings provided an economic argument supporting the 2019 WHO guidelines and the recently updated national free AIDS antiretroviral drug list.
To our knowledge, only one study [43] had performed a 5-year cost-effectiveness analysis of DTG-based regimen in China, compared to EFV-based regimen and LPV/r-based regimen, using a Markov model. It reported that DTG dominated (with fewer costs and higher QALYs) in both settings, when DTG was priced on parity to LPV/r. However, the long-term economic value of DTG in the Chinese context has not been investigated previously. Our study evaluated the cost-effectiveness of self-paying regimens at the current market price and considered lifetime horizon.
It was found that patients who used EFV-based regimen were more likely to switch to LPV/r-based regimen because of severe adverse drug reactions and drug resistance when collecting data from research field hospitals, which was consistent with the findings in the literature [44,45,46], and the average time of switching change was five years [47]. Therefore, in this study, arm A was set as initial treatment with EFV-based regimen and converted to LPV/r-based regimen in the fifth year (second-tenth year in sensitivity analysis). Arm A was the most used in Chinese clinical settings, with a market share of nearly 90%. Arm B (DTG-based regimen) was the preferred first-line antiretroviral regimen recommended by the WHO [5], and was covered under the national free AIDS antiretroviral drug list in China by the end of 2021[8]. Arm C (Genvoya) was included in China’s reimbursement list in 2019 [48], and arm D (Triumpq) was recommended by the guidelines of the United States [6] and the European Union [7].
From the societal perspective, direct medical costs, non-direct medical costs, and indirect costs were included in this study. The health-care system perspective only included the direct medical costs. HIV management costs were included in the medical service costs (such as testing, treatment of adverse reactions, and opportunistic infections). Due to the difference in major types of adverse reactions among regimens, for example, EFV-based regimen was CNS symptoms, while LPV/r-based regimen was digestive system diseases. The major adverse reactions of each regimen (CNS symptoms, digestive system diseases, anemia, hepatotoxicity, and dermatitis) were included as much as possible. In addition, ABC in Arm D may cause hypersensitivity, once it occurs, the drug should be stopped for lifetime [33]. On the other hand, the clinical experts believe that Arm D is a compound preparation of ABC/3TC/DTG, with a big size tablet, which led to the decrease the tolerance and compliance of patients, thus reducing the treatment effects. This may be the reasons for the difference in health outcomes of arms B and D despite their similar elements.
When collecting data from research field hospitals, it was found that most of the patients who used self-paying regimens were advanced treatment-naive or drug-resistant patients, which was consistent with the consensus of Chinese clinical experts [49]. Therefore, the efficacy of self-paying regimens might be underestimated, and the costs of treating adverse reactions might be overestimated. Moreover, when calculating the indirect costs, hospital stay was assessed as work stoppage hours, ignoring non-hospital hours, such as productivity loss due to drug-induced CNS symptoms. This might underestimate the indirect costs, especially for the EFV-based regimen. For these reasons, the cost-effectiveness of the DTG -based regimen may be underrated.
Our study has some strengths. First, this is the first study to estimate the costs and health effects of antiretroviral regimen in the long term in the Chinese context. Second, it considered more comprehensive regimens, including four major ART regimens in the Chinese market, which accounted for more than 90% of the market share [50]. In addition, actual drug prices in the domestic market were adopted in this study, and the clinical parameters were combined with hospital data, reflecting the real status quo in China. The study found that DTG-based regimen for treatment-naive patients is likely to be cost-effective. The reduction in infections can also be attributed to the immediate decrease in viral load resulting from the implementation of the DTG-based regimen, which highlights the need for broader adoption in China. The findings of this study may serve as a scientific foundation for the development of national strategies for AIDS prevention and control, as well as for the rational allocation of resources.
This study’s limitations are related to the representativeness of the model parameters. First, due to the lack of large-sample efficacy data for DTG, some clinical parameters were obtained from small-sample RCTs, which might be different from long-term real-world data. Second, QALY was estimated using the utility derived from overseas literature, as these data were not available on the Chinese literature. We will adjust further the data if there are future reports of utility values in China. Third, in PSA, a certain proportion in the incremental cost-effectiveness scatterplot had near-zero effectiveness, which may render ICERs ineffective as a tool for assessment. Finally, as this study neither measured treatment-experienced patients nor considered rising trend of HIV infection in China, the impact of DTG-based regimen may under-estimated.
Conclusions
DTG-based regimen for treatment-naive patients is likely to be cost-effective and deserve wider implementation in China. This study strongly suggests the centralized procurement of DTG to minimize cost and maximize cost-effectiveness.
Availability of data and materials
The dataset supporting the conclusion of this article is available upon reasonable request from the corresponding author.
Abbreviations
- 3TC:
-
Lamivudine
- ABC/3TC/DTG:
-
Abacavir/lamivudine/dolutegravir
- ART:
-
Antiretroviral treatment
- AZT:
-
Zidovudine
- CHEERS:
-
Consolidated Health Economic Evaluation Reporting Standards
- CNS:
-
Central nervous system
- CPI:
-
Chinese consumer price index
- DTG:
-
Dolutegravir
- EFV:
-
Efavirenz
- EVG/c/FTC/TAF:
-
Elvitegravir/cobicistat/tenofovir alafenamide/emtricitabine
- HCA:
-
Human capital approach
- ICER:
-
Incremental cost-effectiveness ratio
- NCDP:
-
National Centralized Drug Procurement policy
- NFATP:
-
National Free Antiretroviral Treatment Program
- NVP:
-
Nevirapine
- PSA:
-
Probabilistic sensitivity analysis
- QALYs:
-
Quality-adjusted life years
- TDF:
-
Tenofovir disoproxil fumarate
- WHO:
-
World Health Organization
- WTP:
-
Willingness-to-pay
References
Wu Z, Sullivan SG, Wang Y, Rotheram-Borus MJ, Detels R. Evolution of China’s response to HIV/AIDS. Lancet. 2007;369(9562):679–90.
Chinese center for disease control and prevention, STD and AIDS prevention and control center. National handbook of free AIDS antiviral treatment, 4th Edition. Beijing: People’s Medical Publishing House; 2016.
Yao C, Zhu P, Xie D. Advances in antiretroviral therapy and drug development for AIDS. Progress in Pharmaceutical Sciences. 2018;42(02):84–98.
Wei X, Wu Y, Qin M, Wei D. Efficacy and adverse drug reactions of antiretroviral therapy for 4–5 years. Chinese Journal of AIDS & STD. 2020;26(06):632–5.
WHO. Update of recommendations on first-and second-line antiretroviral regimens. https://www.who.int/publications/i/item/WHO-CDS-HIV-19.15. 2019–07–17/ 2021–05–27.
Guidelines for the use of antiretroviral agents in adults and adolescents living with HIV. https://clinicalinfo.hiv.gov/en/guidelines/adult-and-adolescent-arv/initiation-antiretroviral-therapy. 2019–01–03/ 2021–09–28.
European AIDS clinical socirty. European guidelines Version 10.1 October 2020 https://www.eacsociety.org/files/guidelines-10.1_5.pdf. 2020–10–01/ 2020–10–12.
National Medical Insurance Administration. The Department of Human Resources and Social Security of the National Medical Insurance Administration issued the Catalogue of Medicines for National Basic Medical Insurance, Industrial Injury Insurance and Maternity Insurance (2021). http://www.nhsa.gov.cn/art/2021/12/3/art_37_7429.html. 2021–12–03/2022–02–10.
Centre of China Government Procurement. Drug Prices. 2020. http:// www.ccgp.gov.cn/. 2020–03–03.
UNAIDS. Upper-middle-income countries pay more for HIV medicines, but price reductions can be achieved. https://www.unaids.org/en/resources/presscentre/featurestories/2021/october/20211018_hiv-medicines-price-reductions-can-be-achieved. 2021–10–08/2022–08–09.
Bousmah MA, Nishimwe ML, Tovar-Sanchez T, Lantche Wandji M, Mpoudi-Etame M, Maradan G, et al. New Antiretroviral and Monitoring Strategies in HIV-infected Adults in Low-Income Countries (NAMSAL) ANRS 12313 Study Group. Cost-Utility Analysis of a Dolutegravir-Based Versus Low-Dose Efavirenz-Based Regimen for the Initial Treatment of HIV-Infected Patients in Cameroon (NAMSAL ANRS 12313 Trial). Pharmacoeconomics. 2021;39(3):331–43.
Pialoux G, Marcelin AG, Cawston H, Guilmet C, Finkielsztejn L, Laurisse A, et al. Cost-effectiveness of dolutegravir/abacavir/lamivudine in HIV-1 treatment-Naive (TN) patients in France. Expert Rev Pharmacoecon Outcomes Res. 2018;18:83–91.
Zheng A, Kumarasamy N, Huang M, et al. The cost-effectiveness and budgetary impact of a dolutegravir-based regimen as first-line treatment of HIV infection in India. J Int AIDS Soc. 2018;21: e25085.
Restelli U, Rizzardini G, Antinori A, Paltiel AD, Mayer KH, Rewari BB, et al. Cost-effectiveness analysis of dolutegravir plus backbone compared with raltegravir plus backbone, darunavir+ritonavir plus backbone and efavirenz/tenofovir/emtricitabine in treatment naïve and experienced HIV-positive patients. Ther Clin Risk Manag. 2017;13:787–97.
Despiégel N, Anger D, Martin M, Monga N, Cui Q, Rocchi A, et al. Cost-Effectiveness of Dolutegravir in HIV-1 Treatment-Naive and Treatment-Experienced Patients in Canada. Infect Dis Ther. 2015;4:337–53.
Husereau D, Drummond M, Augustovski F, de Bekker-Grob E, Briggs AH, Carswell C, et al. CHEERS 2022 ISPOR Good Research Practices Task Force. Consolidated Health Economic Evaluation Reporting Standards 2022 (CHEERS 2022) Statement: Updated Reporting Guidance for Health Economic Evaluations. Value Health. 2022;25(1):3–9.
China | HIV/AIDS Data Hub for the Asia-Pacific Region. https://www.aidsdatahub.org/country-profiles/china. 2022–02–10.
Han MJ, Chen QF, Xu P, Ying S. Make great efforts to make AIDS prevention and control in the 13th Five-Year Plan a new journey-review and prospect of AIDS prevention and control in China. China AIDS and STD. 2021;27(12):1327–31.
Dou Z, Zhang F, Zhao Y, Jin C, Zhao D, Gan X, et al. Progress on China’s national free antiretroviral therapy strategy in 2002–2014. Chinese Journal of Epidemiology. 2015;36(12):1345–50.
Smiley CL, Rebeiro PF, Cesar C, Belaunzaran-Zamudio PF, Crabtree-Ramirez B, Padgett D, et al. Estimated life expectancy gains with antiretroviral therapy among adults with HIV in Latin America and the Caribbean: a multisite retrospective cohort study. Lancet HIV. 2021;8(5):e266–73.
Statistical Bulletin of National Economic and Social Development of the People’s Republic of China in 2020. http://www.stats.gov.cn/tjsj/zxfb/202102/t20210227_1814154.html. 2021–12–28/2022–03–03.
Lv F, Chen F. National HIV/AIDS epidemic estimation and interpretation in China. Chin J Epidemiol. 2019;10:1191–6.
Qiu T, Ding P, Liu X, Guo H, Fu G, Xu X, et al. Analysis on CD4+T of HIV/AIDS receiving highly active antiretroviral therapy for one year in Jiangsu province. Acte Universitatis Medicinalis Nanjing (Natural Science). 2015;35(03):425–9+432.
WHO. Choosing interventions that are cost effective (WHO-CHOICE), threshold values for intervention cost-effectiveness by region. http://www.who.int/entity/choice/costs/CER_thresholds_regions.xls 2021–06–05.
China Statistical Yearbook 2020. http://www.stats.gov.cn/tjsj/ndsj/2020/indexch.htm. 2021–01–01.
Cui P, Liu N, Duan Z. Research progress on the economic burden of disease. Chinese Journal of Preventive Medicine. 2016;17(08):612–6.
Ma L. Research on the cost, effect and effectiveness of different Antiretroviral treatment strategies in AIDS single positive families. Doctoral thesis. Chinese Center for Disease Control and Prevention. 2016.
Guo Z. The direct medical costs analysis of national free Antiretroviral treatment for HIV/AIDS patients. MA thesis. Peking Union Medical College. 2008.
Liu G. China guidelines for pharmacoeconomic evaluations. Beijing: China Market Press; 2020:1–76.
Tsevat J, Sherman SN, McElwee JA, et al. The will to live among HIV-infected patients. Ann Intern Med. 1999;131(3):194–8.
Kauf TL, Roskell N, Shearer A, Mandell KL, Simbartl LA, Sonnenberg FA, et al. A predictive model of health state utilities for HIV patients in the modern era of highly active antiretroviral therapy. Value Health. 2008;11(7):1144–53.
Simpson KN, Pei PP, Möller J, Baran RW, Dietz B, Woodward W, et al. Lopinavir/ritonavir versus darunavir plus ritonavir for HIV infection: a cost-effectiveness analysis for the United States. Pharmacoeconomics. 2013;31(5):427–44.
Aids and Hepatitis C Group of Infectious Diseases Branch of Chinese Medical Association, China Center for Disease Control and Prevention. Guide to AIDS Diagnosis and Treatment in China (2021 Edition). Chinese Journal of AIDS & STD. 2021;27(11):1182–201.
Lim KC, Wang VW, Siddiqui FJ, Shi L, Chan ES, Oh HC, et al. Cost-Effectiveness Analysis of Liver Resection Versus Transplantation for Early Hepatocellular Carcinoma Within the Milan Criteria. Hepatology. 2015;61(1):227–37.
Fleurence RL, Hollenbeak CS. Rates and probabilities in economic modelling: transformation, translation and appropriate application. Pharmacoeconomics. 2007;25(1):3–6.
Cohen C, Davis K, Meyers J. Abstracts of the eleventh international congress on drug therapy in HIV infection, 11–15 November 2012, Glasgow UK. J Int AIDS Soc. 2012;15 Suppl 4(Suppl 4):18060–301.
Aboud M, Kaplan R, Lombaard J, Zhang F, Hidalgo JA, Mamedova E, et al. Dolutegravir versus ritonavir-boosted lopinavir both with dual nucleoside reverse transcriptase inhibitor therapy in adults with HIV-1 infection in whom first-line therapy has failed (DAWNING): an open-label, non-inferiority, phase 3b trial. Lancet Infect Dis. 2019;19(3):253–64.
Sax PE, Pozniak A, Montes ML, Koenig E, DeJesus E, Stellbrink HJ, et al. Coformulated bictegravir, emtricitabine, and tenofovir alafenamide versus dolutegravir with emtricitabine and tenofovir alafenamide, for initial treatment of HIV-1 infection (GS-US-380-1490): a randomised, double-blind, multicentre, phase 3, non-inferiority trial. Lancet. 2017;390(10107):2073–82.
Sax PE, Wohl D, Yin MT, Post F, DeJesus E, Saag M, et al. Tenofovir alafenamide versus tenofovir disoproxil fumarate, coformulated with elvitegravir, cobicistat, and emtricitabine, for initial treatment of HIV-1 infection: two randomised, double-blind, phase 3, non-inferiority trials. Lancet. 2015;385(9987):2606–15.
Walmsley SL, Antela A, Clumeck N, Duiculescu D, Eberhard A, Gutiérrez F, et al. Dolutegravir plus abacavir-lamivudine for the treatment of HIV-1 infection. N Engl J Med. 2013;369(19):1807–18.
Lewden C, Chene G, Morlat P, Raffi F, Dupon M, Dellamonica P, et al. HIV-infected adults with a CD4 cell count greater than 500 cells/mm3 on long-term combination antiretroviral therapy reach same mortality rates as the general population. J Acquir Immune Defic Syndr. 2007;46(1):72–7.
Department of population and employment statistics national bureau of statistics. China population and employment statistics yearbook 2020. Beijing: China statistics press; 2020:20–100.
Punekar YS, Guo N, Tremblay G, Piercy J, Holbrook T, Young B. Improving access to antiretrovirals in China: economic analyses of dolutegravir in HIV-1 patients. Cost Eff Resour Alloc. 2019;17:26.
Xu S, Zhang H, Zheng X, Lin C, He D, Liu M, et al. Analysis on free second-line antiretroviral drugs used on HIV/AIDS, Fuzhou city, 2020. Preventive Medicine Tribune. 2021;27(01):23–7.
Wei L. Analysis of the reasons for replacement of initial antiviral therapy for AIDS. MA thesis. Guangxi Medical University. 2019.
Chen M, Wu Y, Zhao D, Dou Z, Gan X, Hu X, et al. Differences and risks factors of regimen modification in acquired immunodeficiency syndrome patients who initiated antiretroviral treatment. Chin J Infect Dis. 2017;35(04):193–7.
Zhang M, Shang M, Yang W, Chen J, Wang Z, Shang H. Treatment effect and drug-resistant mutations in Chinese AIDS patients switching to second-line antiretroviral therapy. PLoS ONE. 2014;9(10):e110259.
National medical insurance administration, ministry of human resources and social security. List of medicines allowed in the national medical insurance negotiations in 2019. 2019.http://www.nhsa.gov.cn/art/2019/11/28/art_14_2052.html. 2019–11–28/2020–11–12.
Lu H, Shen Y. Expert consensus on the clinical use of integrase inhibitors. Chinese Journal of Infectious Diseases. 2018;36(09):521–7.
Ma C, Wang Q, Zhang Y, Meng X. Analysis on the composition of free antiviral drugs for AIDS treatment in China from 2009 to 2019. China Madical Herald. 2021;18(17):157–60 +168+198.
Acknowledgements
The author would like to thank Joint United Nations Programme on HIV/AIDS (UNAIDS) for the funding and guidance (Wei Guo, Huiling Weng) of this study, thank the experts from the WHO (Zhongdan Chen), University of North Carolina Project-China (Weiming Tang) and the Chinese Center for Disease Prevention (Fan Lv, Houlin Tang, Chuntao Ma, Dongmin Li, Yan Zhao) for their helpful suggestions on model design, data collection, interpretation of results, and the manuscript drafts. Thanks to Dean Guihua Zhuang, School of Public Health, Xi’an Jiaotong University, and his team (Li Xie, Zhuoru Zou) for the technical support. Thanks to Nantong No.3 hospital affiliated to Nantong university for their contributions to data collection. We would like to thank Editage (www.editage.cn) for English language editing.
Disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of Joint United Nations Programme on HIV/AIDS (UNAIDS).
Funding
This work was supported by the Joint United Nations Programme on HIV/AIDS (UNAIDS) in China, National Science and Technology Major Project on A Multimodality model guided tailored screening, precise diagnosis, and prevention strategy (MODERN) for HIV Prevention and Control (2022YFC2304901), Postgraduate Research & Practice Innovation Program of Jiangsu Province (KYCX23_3435), and General Project of Scientific Research Projects of Nantong Health Committee (MB2021075).
Author information
Authors and Affiliations
Contributions
Min Li, Yuxin Cao designed and analysed the cost-effectiveness model, and drafting the article. Hao Huang collected and analysed the data. Yuxin Cao summarized the cost, utility and clinical parameters. Gang Qin, Minjie Chu had advised on model design, data c AQ ollection, interpretation of results. Meiyin Zou interpreted the data and verified the representativeness of data, Xun Zhuang was the overall study lead.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval for the study was provided by the Medical Ethics Committee of Nantong University (Approval number: No. [2020] 4). All participants signed an informed consent form. We confrm that all methods were performed in accordance with the relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: eTable 1.
Cost-Effectiveness Impact Inventory demonstrating types of health outcomes and costs included in each perspective. eTable 2. Annual incidences of adverse reactions and opportunistic infections. eFigure 1. One-way Sensitivity Analysis (arm B vs arm C, arm B vs arm D). eFigure 2. Incremental Cost-effectiveness Scatterplot (arm B vs arm C, arm B vs arm D).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Li, M., Cao, Y., Huang, H. et al. Cost-effectiveness analysis of antiretroviral drugs for treatment-naive HIV infection in China. BMC Public Health 23, 2228 (2023). https://doi.org/10.1186/s12889-023-17052-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-023-17052-1