Abstract
Background
Although health public services recommend prevention strategies for COVID-19 some of these recommendations have not been taken seriously by young people. Understanding why some people comply with these recommendations and others do not seem to be crucial in helping public health services to predict behavior and compliance with rules, especially for young people. Previous studies suggest that knowledge, attitudes, and practices (KAP) are useful to assess compliance with the preventive measures and public health policies. Being afraid has also been found to correlate with more engagement with preventive measures. This study aims to assess the KAP and fear of COVID-19 of Spanish university students and to understand the relation between diagnosis, KAP and the level of fear.
Method
Participants of this cross-sectional study were 598 college students (69.4% women) from different Spanish Universities. Data were collected for a month using an online questionnaire through Sphinx iQ2.
Results
Levels of KAP among Spanish students were satisfactory and results suggest the presence of fear among them. More importantly, fear of COVID-19 mediated the impact of the diagnosis on the KAP.
Conclusions
Feeling fear seems to be the mechanism underlying the relationship between diagnosis and KAP. Diagnosis is associated with KAP when the diagnosis it is accompanied by measures of fear. KAP, diagnosis, or perceived fear of COVID must be taken together in consideration for health interventions and public health campaigns design.
Similar content being viewed by others
Background
The coronavirus SARS-CoV-2, responsible for the COVID-19 epidemic, was first identified in Wuhan (China) in December 2019 and the World Health Organization (WHO) recognized a global pandemic on 11 March 2020. At of 30 August 2023, the number of COVID-19 confirmed cases reported by WHO has been 770,085,713, including 6,956,173 deaths. Europe has seen 275,912,918 confirmed cases, of which 13,980,340 are in Spain [1]. In Spain, the first cases were identified on January 31, 2020 [2].
The Spanish Government implemented on March 14, 2020, a general lockdown period with a stay-at-home requirement. That state of alarm was maintained with a second state which ended on 9 May 2021 [3]. In this case the free movement of citizens was limited between hours, territories and number of people who can meet.
More than one million university students were confined when the state of alarm started in Spain. Students began online education, distance learning and digital instruction at the university from March 2020, until the end of the academic year in July 2020. Between September 2020 to July 2021, a hybrid and flexible model (face-to-face instruction and distance learning) started in all Spanish Universities [4].
Although The Centers for Disease Control and Prevention (CDC) and governments of different countries recommend prevention strategies for COVID-19, such as social distancing, there is evidence that some of these recommendations have not been taken seriously by adolescent and young adult (AYA) populations [5,6,7,8,9,10,11]. In Spain, adherence to the preventive strategies has been found to be associated to age. People under 45 years old were less likely to follow the acceptance and adherence to the main preventive measures, such as wearing a mask, washing their hands, and keeping distance [12]. These results have also been found in other countries [13,14,15,16].
Previous studies suggest that knowledge, attitudes, and practices (KAP) are useful to assess compliance with preventive measures [16,17,18]. Indeed, health interventions and public health policies have been designed based on KAP surveys outcomes [19]. Although there are studies that have showed consistence between students KAP [6, 20,21,22,23,24,25] some others have not found this association between knowledge and attitudes or practices [19, 26, 27].
Knowledge seems to help to identify why some people comply with the measures and others do not. In addition, knowledge provides information on which people interventions should be aimed at [16]. A greater adherence to preventive strategies is associated with a higher risk perception [18, 27,28,29,30]. However, individuals that are aware to some extent of the risk of COVID-19 typically underestimate their personal risk relative to that of others [18]. In this sense, young people reported lower high-risk perception than adults [11].
Being afraid has been found to be associated with risk perception [29] and to correlate with more engagement with preventive measures [27, 28, 30]. Although this last relationship between fear and preventive measures has not always been found [10]. Fear can be defined as an emotional response to a real or imagined danger causing physiological changes in the body to rise an escape or defensive behavior [29, 31].
Fear of COVID-19 has been found among the population during the pandemic [32,33,34,35,36]. Specifically in Spain, university students do not report particularly high scores of fears, although data suggest the presence of fear [37]. Older people, those with a lower level of education and those belonging to the most socioeconomically vulnerable group showed higher scores in fear [29]. Moreover, one’s own infection or having a person in immediate surroundings infected by COVID-19 (i.e., family member, friend, coworker) increases the probability of fear [29, 38].
Understanding why some people comply with preventive measures and others do not appears to be crucial in helping public health services establishing meaningful predictors of population behavior and compliance, especially for young people. This study aims to assess the knowledge, attitude, behavior (KAP) and fear of COVID-19 of Spanish university students to the COVID‑19 outbreak. In addition, an attempt was made to understand the relation between the diagnosis and the knowledge, attitudes, and practices. Fear of COVID-19 can be a potential mechanism by which diagnosis can produce changes on knowledge, attitudes, and practices.
Method
Participants and design
Participants of this cross-sectional study were 598 (69.4% women, Mage = 21.9, SD = 4.7) college students from different Spanish Universities. The proportion of responses was 0.03% of the total population of Spanish college students (1,679,518 students on that academic year) [39].
Procedure
The study data were collected for a month using an online questionnaire through Sphinx iQ2 and was shared via social media applications (Facebook, LinkedIn, and WhatsApp) to reach the study population. Also, the link was sent to the Students Department of all Spanish universities to be shared with their students by email. Data were collected over 4 weeks from April 3 to May 9 of 2021, one year after the lockdown measures and movement restrictions were implemented.
All information regarding the study, participant’s rights, and researcher’s contact details were provided on the first page of the survey questionnaire. Information about the study objectives and the procedure was given to the participants followed by their consent to participate. Once they consented to participate, they could access the rest of the questionnaire. None of the incomplete data would be used in the analyses.
Research instruments / measurements
The survey questionnaire, tailored specifically for this study, had 6 sections. Section 1: brief about the background and the need for the survey. Section 2: informed written consent. Section 3: questions about sociodemographic variables (sex and age). Section 4: eight questions regarding exposure to COVID-19 and related vulnerability issues. Section 5: regarding KAP towards COVID-19 (2 items about knowledge (symptoms and spreading), 18 items about attitudes and 8 items about practices). The total score of the participants’ knowledge about COVID-19 symptoms ranged from 0 to 17 (greater score indicates more knowledge) and a cut off level of ≥ 9 was set for more accurate knowledge. Participants also selected all items they considered to be a COVID-19 spread vias. The total score ranged from 0 to 4 (greater score indicates more knowledge) and a cut off level of ≥ 3 was set. The attitude section assessed beliefs and perceptions towards the COVID-19 pandemic, including the risk of transmission and symptom development (4 items), and the perceived effectiveness of risk reduction strategies (14 items). Responses of each item was indicated on a 5-point Likert scale (1 = completely disagree, 5 = completely agree). Ratings between items referring to the same issue were inter-correlated, so they were averaged to create 2 composite indexes: perceived own risk of transmission and symptom development (3 items; α = 0.71); perceived risk of spreading (1 item); perceived effectiveness of risk reduction strategies (14 items; α = 0.84). The index was scored such that higher numbers indicate more favorable attitudes toward the topics. Practices assessment included 8 items regarding strategies to control COVID-19 outbreak. The strategies were about hygiene-related behaviors and avoidance-related behaviors. Participants were asked how much they used the risk reduction strategies in a 5-point Likert scale (1 = never, 2 = rarely, 3 = sometimes, 4 = often, 5 = every time/ always). Ratings were inter-correlated (α = 0.79), so they were averaged to create a composite index. The index was scored such that higher numbers indicate more adaptative behavior regarding risk reduction strategies. Section 6: The Fear of COVID-19 Scale (FCV-19 S [32]; validated Spanish university students’ version [37]).
Statistical analysis
Frequencies and percentages for categorical variables, measures of central tendency and dispersion were calculated. Student’s t and ANOVA tests were used to determine the relation between means of knowledge, attitudes, and practices scores and socio-demographic variables. Mediation analyses were used to evaluate how being diagnosed with COVID 19 can change knowledge, attitudes, or practices scores. All data analyses were performed using Statistical Package for the Social Sciences (SPSS) software, version 22 and the PROCESS add-on for SPSS [40]. A value of p < .05 was considered statistically significant.
Results
Exposure to COVID-19 and related vulnerability issues
Table 1 shows the responses to the exposure to COVID-19 and related vulnerability issues.
Knowledge, attitudes, and practices
Knowledge about the COVID-19 pandemic
Out of the 598 students, 532 (88.9%) students answered ≥ 9/17 questions correctly about COVID-19 symptoms and 476 (79.6%) students answered ≥ 3/4questions correctly COVID-19 spreading. Knowledge assessment of the participants regarding common symptoms and ways of spreading are shown in Table 2. The total knowledge (symptoms) score ranged from 1 to 17, with a mean of 10.95 ± 3.29. The total knowledge (spread) score ranged from 1 to 4, with a mean of 3.27 ± 0.91.
Attitudes
For each question focused on attitude, the statistics of responses from participants are presented in Table 3. Participant’s perceptions about their own risk of acquiring COVID-19 and the perceived impact on their health mean was 2.72 ± 0.80, with a range of 1 to 5, and a symmetrical and mesokurtic distribution. It is important to notice that they believed to be at risk of getting COVID-19 to a greater extent (3.56 ± 0.99) than of developing severe symptoms (2.62 ± 1.01; t(597) = 20.44, p < .001) or even dying (1.98 ± 1.02; t(597) = 31.41, p < .001). Perceived risk of spreading the disease was higher (4.02 ± 0.99) than the perceived risk of getting COVID-19 (3.56 ± 0.99); t(597) = -10.30, p < .001.
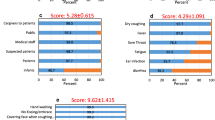
Participants’ attitude towards the degree of effectiveness of measures to reduce personal risk from COVID-19 was satisfactory as the mean attitude score was 3.76 ± 0.58, with a range of 1.29 to 5 (Table 3). Figure 1 shows the perceptions towards the degree of effectiveness of measures to reduce personal risk from COVID-19. Ventilation of spaces and washing hands were considered to have high to very high effectiveness (N = 562, 94% and N = 562, 94%, respectively), followed by wearing a mask (N = 561, 93.8%), taking a diagnostic test (N = 554, 92.7%), vaccine (N = 533, 89.1%), disinfection of spaces (N = 525, 87.8%), limited capacity of places (N = 521, 87.1%) and social distance (N = 505, 84.4%).
Practices
Participant’s adoption of practices to prevent COVID-19 was satisfactory as the mean practices score was 28.40 ± 6.19, with a range of 11 to 40 (Table 4). Figure 2 shows the degree of adoption of each practice. The most common strategies to control COVID-19 outbreak were the hygiene-related behaviors: 576 (96.3%) students wear often or always a mask and 460 (76.9%) washed their hands often or always. Wearing a mask was mandatory in Spain at the time data were collected. Taking in consideration only the avoidance-related behaviors results showed that the most common strategy was reducing the number of social contacts with family (N = 387, 64.7%), followed by reducing the number of social contacts with friends (N = 340, 56.9%), keeping social distance (N = 293, 48.9%) and avoiding going to bars or public events (N = 288, 48.1%).
Fear of COVID-19
Participants’ mean value on the FCV-19 S (α = 0.86) was 15.08 (SD = 5.75), median = 14.00, with a range of 7 to 35.
Relationships between variables
In order to facilitate the analysis, a Knowledge Index was created combining the two items related to knowledge (r =. 27) and an Attitude Index combining the 3 attitudes items related to attitudes (α = 0.51).
There was a positive correlation (r = .12) between knowledge and attitudes scores (p = .003) and knowledge and practices score (r = .13, p = .001); attitude and practice scores increased as knowledge scores were increasing. There was also a moderate positive correlation (r = .33) between attitude and practices score (p < .001); practices scores increased as attitude scores were increasing. This correlation was stronger analyzing only the attitudes toward effectiveness of risk reduction strategies and practices scores (r = .49, p < .001). As the perceived effectiveness of risk reduction strategies scores increased the adoption of strategies to control COVID-19 scores also increased.
Women, compared to men, reported having more knowledge (M = 7.40, SD = 1.68), more positive attitudes (M = 3.55, SD = 0.56) and adopted more risk reduction strategies (M = 3.63, SD = 0.74) than men (M = 6.45, SD = 1.96, t(304) = -5.69, p < .001; M = 3.39, SD = 0.60, t(596) = -3.03, p < .001; M = 3.36, SD = 0.81, t(596) = -4.11, p < .001; respectively). There was a positive correlation between age and attitudes (r = .12, p = .003); as well as a correlation between age and practices scores (r = .21, p < .001).
Those participants who reported being vulnerable to Covid-19 due to a medical condition reported more positive attitudes (M = 3.75, SD = 0.59) and adopted more risk reduction strategies (M = 3.86, SD = 0.78) than those who are less vulnerable (M = 3.47, SD = 0.57, t(596) = -3.56, p < .001; M = 3.51, SD = 0.77, t(596) = -3.3, p = .001; respectively). Participants having a relative vulnerable to COVID-19 also reported more positive attitudes (M = 3.53, SD = 0.56) and adopted more risk reduction strategies (M = 3.58, SD = 0.69) than those who did not (M = 3.31, SD = 0.63, t(596) = -3.52, p < .001; M = 3.38, SD = 0.69, t(153.3) = -2.69, p = .008; respectively). Those participants who had been diagnosed with COVID-19 reported more knowledge (M = 7.63, SD = 1.91) and lower positive attitudes (M = 3.39, SD = 0.56) than those who had not (M = 7.00, SD = 1.79, t(596) = -3.14, p = .002; M = 3.52, SD = 0.58, t(596) = 2.05, p = .04; respectively). Also, participants who had a relative that had been diagnosed with COVID-19 reported more knowledge (M = 7.32, SD = 1.75) than those who did not (M = 6.88, SD = 1.87, t(596) = -2.95, p = .003).
There was a moderate positive correlation (r = .39) between fear of COVID-19 and attitude scores (p < .001); attitude scores increased as fear of COVID-19 scores were increasing. There was a moderate positive correlation (r = .35) between fear of COVID-19 and practices scores (p < .001); practices scores increased as fear of COVID-19 scores were increasing. A small positive correlation (r = .22) was observed between fear scores and knowledge scores (p < .001).
Women reported having more fear of COVID-19 (M = 16.07, SD = 5.76) compared to men (M = 12.83, SD = 5.05, t(394) = -6.93, p < .001).
There was a positive correlation between age and fear of COVID-19 (r = .005, p = .90). Level of fear increased as the age increased.
Those participants suffering from any disease that makes them vulnerable to COVID-19 reported having more fear of COVID-19 (M = 17.98, SD = 1.68) than those who did not (M = 14.76, SD = 5.51, t(66) = -3.44, p = .001).
Participants who had been diagnosed with COVID-19 reported less fear of COVID-19 (M = 13.96, SD = 5.27) than those who had not (M = 15.29, SD = 5.81, t(596) = 2.10, p = .04).
There were no differences in the fear of COVID-19 scale between participants who had a relative that had been diagnosed with COVID-19 (M = 16.00, SD = 5.55) and those who did not (M = 15.05, SD = 5.95, t(596) = − 0.10, p = .92). It is important to note that results of the ANOVA of the severity of the relative’s symptoms on fear of COVID-19 were significant, F(3,310) = 4.21, p = .004. Participants who had suffered the death of a relative from COVID-19 reported significantly more fear (M = 17.56, SD = 6.69) compared with those whose relatives had passed the illness with mild symptoms (M = 14.59, SD = 5.02; p = .01) or asymptomatic (M = 13.41, SD = 5.22; p = .008).
Mediation
Mediation analysis was conducted to determine whether fear of COVID-19 mediated the relationships between having been diagnosed with COVID-19 and KAP. The unstandardized coefficients for the indirect effects were as follows: β = − 0.09, 95% CI [-0.021, − 0.02] for the Knowledge Index; β = − 0.05, 95% CI [–0.09, –0.006] for the Attitude Index; β = − 0.06, 95% CI [-0.12, − 0.01] for the Practices Index. These results showed that fear of COVID-19 mediated the impact of the diagnosis on the KAP variables (see Fig. 3).
Discussion
Most of the participants of this study were knowledgeable about COVID-19 like other similar university students’ samples [19, 21, 23, 25, 41]. The participants’ attitude towards the degree of effectiveness of measures to reduce personal risk from COVID-19 was satisfactory. However, participants’ perceptions about their own risk acquiring COVID-19 were lower than the perceived risk of spreading the disease. Moreover, they believe to be at risk of getting COVID-19 to a greater extent than of developing severe symptoms or even dying. These results are coherent with those claiming that, although, individuals can be aware to some extent of the risk of the COVID-19, they typically underestimate their personal risk [18] or were more worried for their family and friends not to get infected than themselves [42]. Participants’ adoption of practices to prevent COVID-19 were also satisfactory as in other university students’ samples [21, 25, 41].
All measures of KAP showed a relationship between them, as knowledge increased so did attitudes and adherence to preventive strategies as in previous studies [6, 20,21,22,23,24,25, 43]. Also, as attitudes scores increased (i.e., more risk perception and more perception of the preventive strategies effectiveness) more compliance with the strategies was found. Similarly, other studies have been demonstrated that, although knowledge influences the attitudes, the attitudes are the ones that influences practices [44], particularly toward COVID-19 [45]. It is important to notice that the relationship was stronger between the perceived effectiveness of risk reduction strategies and the adoption of strategies to control COVID-19. Coherently, a previous study showed that involvement in more COVID-19 preventive practices was associated with greater COVID-19 perceived risk, in turn, with more COVID-19 fear [46].
Vulnerability was not related to knowledge. However, participants who were more vulnerable or had a vulnerable close person reported more positive attitudes and adopted more risk reduction strategies than those who are less vulnerable themselves or close family or friends.
Results suggest that being diagnosed or having a relative that has been diagnosed with COVID-19 is related to more knowledge. But it does not seem to be related to having more positive attitudes or more engagement with the preventive strategies. Indeed, this study showed that being diagnosed is related to lower attitudes.
Similar to other study carried out in Spain with university students, participants do not inform of high scores of fears, although they suggest the presence of fear [37]. The probability of feeling fear of COVID-19 was related to KAP, for example not maintaining social relation with non-cohabiting people [47]. As previous research had shown [25, 30, 48] participants reporting more knowledge, more positive attitudes or more compliance with preventive strategies also reported feeling more fear. Moreover, higher risk perceptions increased the probability of feeling fear [29]. Being vulnerable or having close vulnerable friends or family members increased the probability of feeling fear as living with a chronically ill family member is related to high negative emotional responses in young people [47].
Although evidence has shown that the probability of fear of infection increases if the person has been infected by COVID-19 or if a close person has been infected [29, 38] results did not show this relationship. Indeed, participants who had been diagnosed with COVID-19, reported less fear of COVID-19. However, when analyzing the data differentiating between the several consequences of the diagnosis, severity of the symptoms of the relative was found to be related to more fear. As in previous studies [38, 49], participants who have suffered the death of a relative from COVID-19 reported significantly more fear, higher anxiety symptom and stress. In this sense, this lack of fear can be explained because most of the sample who had been diagnosed reported being asymptomatic or with mild symptoms. Being asymptomatic or with mild symptoms could also be the explanation of the lower positive attitudes of the students diagnosed with COVID-19 compared who those who had not, despite having a higher knowledge.
The mediation analysis can explain the differences between the results found in this study and previous research. Fear of COVID-19 mediated the impact of the diagnosis on the KAP variables. Feeling fear seems to be the mechanism underlying the relationship between diagnosis and KAP. Diagnosis is associated with KAP when the diagnosis it is accompanied by measures of fear. It is important to take in consideration that high intolerance of uncertainty is one factor that explains COVID-19 fear in the Spanish population [50] and the survey of the present study was conducted in a very uncertain context: media reports were constant, there was a great lack of knowledge about the disease and its long-term consequences; and population vaccination was still limited. In Spain, the vaccination campaign started at the end of December 2020, in old people’s homes and health-care staff. In February the vaccination campaign was offer to other groups of populating organized by age and starting with people over-80s. At the time of the survey only the vulnerable students could have access to the vaccine.
These findings could help public health services in developing effective health promotion campaigns. It is important to improve people attitudes producing a consequent healthy behavior [51]. Also, public health campaigns and doctors when giving the diagnosis could target fear as a useful tool in some situations. Fear produces behavioral change when people feel a sense of efficacy [52]. Increasing KAP could also increase the sense of efficacy. Attitudes regarding the expectations of effectiveness of the measure against COVID-19 and the very use of prevention practices against COVID-19 is in themselves the exit strategy to the threat.
This study has some limitations. First, the questionnaire used has not been validated, which could lead to information bias. Secondly, although we tried to reach all Spanish universities, we failed to do it and thus, this may not be a good representative of all Spanish university students. Because it was an online questionnaire, students without internet connections could not provide their opinions.
Conclusions
Taking together the results of this study and previous research it seems that health interventions and public health policies cannot only be designed based on KAP surveys outcomes, diagnosis, or perceived fear by themselves. All variables must be taken together in consideration. These findings suggest a need for continuous health education and health promotion to improve adherence to prevention measures for COVID-19 or other pandemics. Future research must focus on the use of fear tactics as a useful tool in a public health campaign to improve the compliance with preventive behaviors in new epidemic contexts.
Data Availability
The data that support the findings of this study are available from Universidad Villanueva but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request to the corresponding author (acancela@villanueva.edu) and with permission of Universidad Villanueva.
References
WHO COVID-19 Dashboard [Internet]. World Health Organisation. 2022. [cited 30 August 2023] Available from: https://covid19.who.int.
COVID-19 [Internet]. Isciii.es. 2021. [cited 24 November 2020] Available from: https://cnecovid.isciii.es/covid19/#documentaci%C3%B3n-y-datos.
Real Decreto 956/. 2020, de 3 de noviembre, por el que se prorroga el estado de alarma declarado por el Real Decreto 926/2020, de 25 de octubre, por el que se declara el estado de alarma para contener la propagación de infecciones causadas por el SARS-CoV-2 [Royal Decree 956/2020, of 3 November, extending the alarm state declared by Royal Decree 926/2020, of 25 October, which states the alarm state in order to content the spread of infections caused by SARS-CoV-2.]. (Boletín Oficial del Estado, number 291, 4 November 2020). Available from: https://www.boe.es/eli/es/rd/2020/11/03/956.
CRUE-Universidades Españolas. La universidad frente a la pandemia: actuaciones de CRUE Universidades Españolas ante la COVID‐19. [The university in the face of the pandemic: actions of CRUE Spanish Universities in the face of COVID-19]. 2020. Available from: https://www.crue.org/wp-content/uploads/2020/12/La-Universidad-frente-a-la-Pandemia.pdf.
Abbott A, Askelson N, Scherer AM, Afifi RA. Critical reflections on COVID-19 communication efforts targeting adolescents and young adults. J Adolesc Health. 2020;67:159–60. https://doi.org/10.1016/j.jadohealth.2020.05.013.
Angelo AT, Alemayehu DS, Dacho AM. Knowledge, attitudes, and practices toward covid-19 and associated factors among university students in Mizan Tepi University, 2020. Infect Drug Resist. 2021;14:349–60. https://doi.org/10.2147/IDR.S299576.
Barrett C, Cheung KL. Knowledge, socio-cognitive perceptions and the practice of hand hygiene and social distancing during the COVID-19 pandemic: a cross-sectional study of UK university students. BMC Public Health. 2021;21:426. https://doi.org/10.1186/s12889-021-10461-0.
Cohen AK, Hoyt LT, Dull B. A descriptive study of COVID-19 related Experiences and Perspectives of a National Sample of College Students in Spring 2020. Int J Environ Res Public Health. 2020;19:834. https://doi.org/10.3390/ijerph19020834.
Dhanaraj V, Natarajan G, Asha J, Revathy PR, Mohan D, Udayakumar JR. COVID-19 knowledge, misconceptions and practices among the non-medical college students in Tamil Nadu. J Med Allied Sci. 2021;11:77–83. https://doi.org/10.5455/jmas.7787.
Van Nhu H, Tuyet-Hanh TT, Van N, Linh T, Tiene TQ. Knowledge, attitudes, and Practices of the vietnamese as key factors in Controlling COVID-19. J Community Health. 2020;45:1263–9. https://doi.org/10.1007/s10900-020-00919-4.
World Health Organization. Young people and COVID-19: behavioural considerations for promoting safe behaviours: policy brief. 2021. Available from: https://apps.who.int/iris/bitstream/handle/10665/341695/9789240028319-eng.pdf?sequence=1.
Beca-Martínez MT, Romay‐Barja M, Falcón‐Romero M, Rodríguez‐Blázquez C, Benito‐Llanes A, Forjaz MJ. Compliance with the main preventive measures of COVID‐19 in Spain: the role of knowledge, attitudes, practices, and risk perception. Transbound Emerg Dis. 2022;69:e871–82. https://doi.org/10.1111/tbed.14364.
Lennon RP, Sakya SM, Miller EL, Snyder B, Yaman T, Zgierska AE, Ruffin MT, Van Scoy LJ. Public intent to comply with COVID-19 public health recommendations. Health lit res Pract. 2020;4:e161–5. https://doi.org/10.3928/24748307-20200708-01.
MacIntyre CR, Nguyen P, Chughtai AA, Trent M, Gerber B, Steinhofel K, Seale H. Mask use, risk-mitigation behaviours and pandemic fatigue during the COVID-19 pandemic in five cities in Australia, the UK and USA: a cross-sectional survey. Int J Infect Dis. 2021;106:199–207. https://doi.org/10.1016/j.ijid.2021.03.
Mouchtouri VA, Agathagelidou E, Kofonikolas K, Rousou X, Dadouli K, Pinaka O, Agathocleous E, Anagnostopoulou L, Chatziligou C, Christoforidou EP, Chalntoupi T, Kalomoiris L,Kapoula C, Kokkinou V, Constantinides A, Konstantinou P, Kostara E, Kourentis L, Lantou A, … Hadjichristodoulou C. Nationwide survey in Greece about knowledge, risk perceptions,and preventive behaviors for covid19 during the general lockdown in April 2020. Int J Environ Res Public Health. 2020; 17:1–13. https://doi.org/10.3390/ijerph17238854.
Norman P, Wilding S, Conner M. Reasoned action approach and compliance with recommended behaviours to prevent the transmission of the SARS-CoV-2 virus in the UK. Br J Health Psychol. 2020;25:1006–19. https://doi.org/10.1111/bjhp.12474.
Ajilore K, Atakiti I, Onyenankeya K. College students’ knowledge, attitudes and adherence to public service announcements on Ebola in Nigeria: suggestions for improving future Ebola prevention education programmes. Health Educ J. 2017;76:648–60. https://doi.org/10.1177/0017896917710969.
Wise T, Zbozinek TD, Michelini G, Hagan CC, Mobbs D. Changes in risk perception and self-reported protective behaviour during the first week of the COVID-19 pandemic in the United States: COVID-19 risk perception and behavior. R Soc Open Sci. 2020;7:200742. https://doi.org/10.6084/m9.figshare.c.5120379.
Aynalem YA, Akalu TY, Gebresellassie Gebregiorgis B, Sharew NT, Assefa HK, Shiferaw WS. Assessment of undergraduate student knowledge, attitude, and practices towards COVID-19 in Debre Berhan University, Ethiopia. PLoS ONE. 2021;16. https://doi.org/10.1371/journal.pone.0250444.
Afzal MS, Khan A, Qureshi UUR, Saleem S, Saqib MAN, Shabbir RMK, Naveed M, Jabbar M, Zahoor S, Ahmed H. Community-based assessment of knowledge, attitude, practices and risk factors regarding COVID-19 among Pakistanis residents during a recent outbreak: a cross-sectional survey. J Community Health. 2021;46:476–86. https://doi.org/10.1007/s10900-020-00875-z.
Duong MC, Nguyen HT, Duong BT. A cross-sectional study of knowledge, attitude, and practice towards face mask use amid the COVID-19 pandemic amongst university students in Vietnam. J Community Health. 2021;46:975–81. https://doi.org/10.1007/s10900-021-00981-6.
Iradukunda PG, Pierre G, Muhozi V, Denhere K, Dzinamarira T. Knowledge, attitude, and practice towards COVID-19 among people living with HIV/AIDS in Kigali, Rwanda. J Community Health. 2021;46:245–50. https://doi.org/10.1007/s10900-020-00938-1.
Patwary MM, Disha AS, Bardhan M, Haque MZ, Kabir MP, Billah SM, Hossain MR, Alam MA, Browning MH, Shuvo FK, Piracha A, Zhao B, Swed S, Shah J, Shoib S. Knowledge, attitudes, and Practices toward Coronavirus and Associated anxiety symptoms among University students: a cross-sectional study during the early stages of the COVID-19 pandemic in Bangladesh. Front Psychiatry. 2022;13. https://doi.org/10.3389/fpsyt.2022.856202.
Jia Y, Ma S, Bai L, Xiao Q, Wu Y, Gao Y, Han Y, Xie Z, Tang X, Ge J. Health literacy and disparities in knowledge, attitude and practice regarding COVID-19 among college students during the COVID-19 outbreak in China: a cross-sectional study. Risk Manag Healthc Policy. 2021;14:4477. https://doi.org/10.2147/RMHP.S319331.
Licata F, Oliverio A, Di Gennaro G, Nobile CGA, Bianco A. Insight on knowledge, risk perception and practices to prevent the spread of covid-19: a cross-sectional study among italian university students. Appl Sci. 2021;11:9031. https://doi.org/10.3390/app11199031.
Matovu JKB, Kabwama SN, Ssekmatte T, Ssenkunsu J, Wanyenze RK. COVID–19 awareness, adoption of COVID–19 preventive measures, and Effects of COVID–19 lockdown among adolescent Boys and Young Men in Kampala, Uganda. J Community Health. 2021;46:842–53. https://doi.org/10.1007/s10900-021-00961-w.
Yorguner N, Bulut NS, Akvardar Y. An analysis of the Psychosocial Challenges Faced by the University students during COVID-19 pandemic, and the students’ knowledge, attitudes, and Practices toward the Disease. Noro Psikiyatr Ars. 2021;58:3–10. https://doi.org/10.29399/npa.27503.
Harper CA, Satchell LP, Fido D, Latzman RD. Functional fear predicts public health compliance in the COVID-19 pandemic. Int J Men Health Addict. 2021;19:1875–88. https://doi.org/10.1007/s11469-020-00281-5.
Recio-Vivas AM, Font-Jiménez I, Mansilla-Domínguez JM, Belzunegui-Eraso A, Díaz-Pérez D, Lorenzo-Allegue L, Peña-Otero D. Fear and attitude towards SARS-CoV-2 (COVID-19) infection in Spanish Population during the period of confinement. Int J Environ Res Public Health. 2022;19:834. https://doi.org/10.3390/ijerph19020834.
Habib MA, Dayyab FM, Iliyasu G, Habib AG. Knowledge, attitude and practice survey of COVID-19 pandemic in Northern Nigeria. PLoS ONE. 2021;16:e0245176. https://doi.org/10.1371/journal.pone.0245176.
Espinola M, Shultz JM, Espinel Z, Althouse BM, Cooper JL, Baingana F, Marcelino LH, Cela T, Jerez T, Mazurik L, Green MC, Beck A, Fredrickson M, Mclean A, Rechkemmer A. Fear-related behaviors in situations of mass threat. Disaster Health. 2016;3:102–11. https://doi.org/10.1080/21665044.2016.1263141.
Ahorsu DK, Lin CY, Imani V, Saffari M, Griffiths MD, Pakpour AH. The fear of COVID-19 scale: development and initial validation. Int J Men Health Addict. 2020;20:537–1545. https://doi.org/10.1007/s11469-020-00270-8.
Barbisch D, Koenig KL, Shih FY. Is there a case for Quarantine? Perspectives from SARS to Ebola. Dis M Public H Prep. 2015;9:547–53. https://doi.org/10.1017/dmp.2015.38.
Lin CY. Social reaction toward the 2019 novel coronavirus (COVID-19). Social Health and Behavior. 2020;3:1–2. https://doi.org/10.4103/SHB.SHB_11_20.
Rubin GJ, Wessely S. The psychological effects of quarantining a city. BMJ. 2020;368. https://doi.org/10.1136/bmj.m313.
Shigemura J, Ursano R, Morganstein JC, Kurosawa M, Benedek D. Public responses to the novel 2019 coronavirus (2019-nCoV) in Japan: mental health consequences and target populations. Psychiatry Clin Neurosci. 2020;74:281–2. https://doi.org/10.1111/pcn.12988.
Martínez-Lorca M, Martínez-Lorca A, Criado-Álvarez JJ, Cabañas Armesilla MD, Latorre JM. The fear of COVID-19 scale: Validation in spanish university students. Psychiatry Res. 2020;293:113350. https://doi.org/10.1016/j.psychres.2020.113350.
Mazza C, Ricci E, Biondi S, Colasanti M, Ferracuti S, Napoli C, Roma PA. Nationwide Survey of Psychological distress among italian people during the COVID-19 pandemic: Immediate psychological responses and Associated factors. Int J Environ Res Public Health. 2020;17:3165. https://doi.org/10.3390/ijerph17093165.
Subdirección General de Actividad Universitaria Investigadora de la Secretaría General de Universidades. Facts and figures of the Spanish University System Publication 2021–2022. [Datos y cifras del Sistema Universitario Español Publicación 2021–2022]. Available from: https://www.universidades.gob.es/wp-content/uploads/2022/11/Datos_y_Cifras_2021_22.pdf.
Hayes AF. Introduction to mediation, moderation, and conditional process analysis. 2nd ed. New York: The Guilford Press; 2018.
Alzoubi H, Alnawaiseh N, Al-Mnayyis AA, Abu-Lubad M, Aqel A, Al-Shagahin H. COVID-19 - knowledge, attitude and practice among medical and non-medical University students in Jordan. J Pure Appl Microbiol. 2020;14:17–24. https://doi.org/10.22207/JPAM.14.1.04.
Sheraba NS, Orayj K, Alqahtani A, El-Sokkary RH, Khalid M. A questionnaire-based cross-sectional survey of knowledge, attitudes, and Practices toward COVID-19 among students and staff in Asir, Saudi Arabia during the Second Wave of the pandemic. Vaccines (Basel). 2022;10(12):2014. https://doi.org/10.3390/vaccines10122014.
Al Ahdab S. A cross-sectional survey of knowledge, attitude and practice (KAP) towards COVID-19 pandemic among the syrian residents. BMC Public Health. 2021;21(1):296. https://doi.org/10.1186/s12889-021-10353-3.
Ajzen I, Fishbein M. The influence of attitudes on behavior. In: Albarracin D, Johnson BT, Zanna MP, editors. The handbook of attitudes. Mahwah: Lawrence Erlbaum Associates; 2005. pp. 173–221.
Nocari I, Fadel D, Dano D, El-Bikai R, Abbas N. Knowledge, attitudes, and practices (kap) toward covid-19: a cross-sectional study among university students in Lebanon. J Hum Behav Social Environ. 2023. https://doi.org/10.1080/10911359.2023.2187913.
Serpas DG, Ignacio DA. COVID-19 fear mediates the relationship between perceived risk and preventive behaviors: the moderating role of perceived effectiveness. Psychol Health. 2022;37(12):1457–70. https://doi.org/10.1080/08870446.2021.1980566.
Cantarero Prieto D, Lanza-León P, Moreno P, et al. Coronavirus fear of contagion and compliance with social distancing measures: evidence for a sample of a spanish university community. PeerJ. 2023;11:e14771. https://doi.org/10.7717/peerj.14771.
Fang F, Chen S, Geng X, Kiprop E. Survey on public awareness, attitudes and self-protective behavior adoption in different periods of COVID-19. Front Public Health. 2023;10:1063384. https://doi.org/10.3389/fpubh.2022.1063384.
Ozamiz-Etxebarria N, Dosil-Santamaria M, Idoiaga Mondragon N, Picaza Gorrotxategi M, Olaya B, Santabárbara J. The emotional state of young people in northern Spain after one year and a half of the COVID-19 pandemic. Eur J Psychiatry. 2023;37(2):109–16. https://doi.org/10.1016/j.ejpsy.2022.09.007.
Sandín B, Valiente RM, García-Escalera J, Chorot P. Impacto psicológico de la pandemia de COVID-19: Efectos negativos y positivos en población española asociados al periodo de confinamiento nacional. RPPC. 2020;25(1):1–22. https://doi.org/10.5944/rppc.27569.
Petty RE, Barden J, Wheeler SC. The elaboration likelihood model of persuasion: developing health promotions to produce sustained behavior change. In: DiClemente RJ, Crosby RA, Kegler M, editors. Emerging theories in health promotion practice and research. San Francisco: Jossey-Bass; 2009. pp. 185–214.
Witte K, Allen M. A meta-analysis of fear appeals: implications for effective public health campaigns. Health Educ Behav. 2000;27:591–615. https://doi.org/10.1177/109019810002700506.
Acknowledgements
Not Applicable.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
AC y MG-N wrote the main manuscript text and A.V. recruited participants and prepared all figures and tables. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study procedure was performed in accordance with the ethical principles of the Declaration of Helsinki and was approved by the Universidad Villanueva Ethics Committee (Reference No. 2021-01).
Consent to Participate
Volunteers were informed that their participation was anonymous and voluntary and that they could, at any point, close the window and discontinue participation. Informed consent was obtained from all individual participants included in the study.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Cancela, A., González-Noriega, M. & Visiers, A. Fear of COVID-19: the mediation role between the COVID-19 diagnosis and KAP in Spanish university students. BMC Public Health 23, 1909 (2023). https://doi.org/10.1186/s12889-023-16777-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-023-16777-3