Abstract
Background
While screening for cardiovascular disease (CVD) risk can help low-resource health systems deliver low-cost, effective prevention, evidence is needed to adapt international screening guidelines for maximal impact in local settings. We aimed to establish how the cost-effectiveness of CVD risk screening in Sri Lanka varies with who is screened, how risk is assessed, and what thresholds are used for prescription of medicines.
Methods
We used data for people aged 35 years and over from a 2018/19 nationally representative survey in Sri Lanka. We modelled the costs and quality adjusted life years (QALYs) for 128 screening program scenarios distinguished by a) age group screened, b) risk tool used, c) definition of high CVD risk, d) blood pressure threshold for treatment of high-risks, and e) prescription of statins to all diabetics. We used the current program as the base case. We used a Markov model of a one-year screening program with a lifetime horizon and a public health system perspective.
Results
Scenarios that included the WHO-2019 office-based risk tool dominated most others. Switching to this tool and raising the age threshold for screening from 35 to 40 years gave an incremental cost-effectiveness ratio (ICER) of $113/QALY. Lowering the CVD high-risk threshold from 20 to 10% and prescribing antihypertensives at a lower threshold to diabetics and people at high risk of CVD gave an ICER of $1,159/QALY. The findings were sensitive to allowing for disutility of daily medication.
Conclusions
In Sri Lanka, CVD risk screening scenarios that used the WHO-2019 office-based risk tool, screened people above the age of 40, and lowered risk and blood pressure thresholds would likely be cost-effective, generating an additional QALY at less than half a GDP per capita.
Similar content being viewed by others
Background
Identification of people at high risk for cardiovascular disease (CVD) and managing them with a combination of lifestyle advice and pharmacological treatment is a cornerstone of the World Health Organization (WHO) Package of Essential Noncommunicable Disease Interventions (PEN) [1, 2]. Using a total CVD risk approach, the PEN, supplemented by WHO HEARTS [3, 4], set out guidelines for screening and management of risk factors – hypertension, diabetes, and hypercholesterolaemia – in primary care settings in low- and middle-income countries (LMICs) to prevent CVD.
There is some evidence of improvement in clinical outcomes following PEN implementation [5] and on the cost-effectiveness of PEN variations in South Asia [6]. However, a systematic review of CVD screening programs in LMICs emphasised the importance of assessing the appropriateness of international guidelines in local settings [7]. Designing the pharmacological component of a CVD risk screening and treatment program involves specification of 1) the age groups to screen, 2) the CVD risk prediction tool to use, 3) the threshold to use to identify high CVD risk, 4) whether to lower the blood pressure treatment threshold for people with diabetes, and 5) whether to give statins to all people with diabetes regardless of CVD risk. These choices potentially have important consequences for cost and effectiveness [7,8,9].
Screening the working-age population can potentially detect CVD risks sufficiently early to avert negative outcomes. But with limited resources, screening at younger ages can have high opportunity costs and may weaken program effectiveness [7].
Most LMICs lack a CVD risk prediction tool derived from domestic data and must rely on tools derived from cohort data from another country [10] or from multiple countries [11]. Validation for use in LMICs is difficult given the lack of accurate morbidity data and longitudinal datasets [12]. The choice of tool may be largely determined by ease of use and WHO endorsement [13]. Compared with an office-based tool, a laboratory-based tool, which requires a blood test for total cholesterol or a lipid profile, is more accurate but also more expensive.
CVD screening programs differ in the CVD risk threshold that is used to trigger statin treatment and, in some programs, to lower the blood pressure threshold for prescription of antihypertensives and determine follow-up frequency. Some countries use lower thresholds of 7.5%—10% risk of a CVD event within ten years [14,15,16], while others use 20% and above [17, 18]. Many LMICs adopt thresholds used in high-income countries despite possibly facing very different costs and impacts, or they adopt a suggested higher threshold assuming lower affordability [19] but without fully considering lower prices at which medicines may be available.
For prescription of antihypertensives, recent WHO guidelines recommend lower blood pressure thresholds for diabetics (≥ 130/80 mmHg) [3, 4], and for people at high risk of CVD (≥ 130 mmHg) [20]. Several guidelines recommend statins for diabetics without consideration of CVD risk [3, 21, 22].
Since 2011, Sri Lanka has set up over 1,000 Healthy Lifestyle Centres (HLCs) to detect people with high CVD risk and associated risk factors [23, 24]. CVD risk screening and treatment guidelines were published in 2012 [25]. In 2018, these were updated by reducing the CVD risk threshold from 30 to 20% for prescription of statins, and broadening the age group screened from 40–65 years to 35 years and above [17]. There was no published analysis of the health and cost consequences of these changes. Nor has there been analysis of the cost-effectiveness of the current program compared with alternatives that would screen at 40 years and above, use an alternative CVD risk tool, lower the CVD risk threshold to 10% in line with several high-income countries, lower the blood pressure treatment threshold for diabetics and those with high CVD risk, and prescribe statins for all diabetics. By conducting such cost-effectiveness analysis, this study aimed to help decision makers in Sri Lanka, and possibly elsewhere, optimise the CVD risk screening program.
Methods
Data
We used data from the Sri Lanka Health and Ageing Study (SLHAS), which is a nationally-representative sample of 6,665 adults aged 18 years and older interviewed in 2018/9. The sample was selected using stratified, multi-stage cluster random sampling [26]. Weights were applied to make the sample representative of the adult population of Sri Lanka in 2019. The dataset had risk factor data needed to simulate screening and predict CVD events for each individual [27]. Except for smoking, each predictor was missing at random in < 1% of the sample. Smoking status was missing for 2.9% of all participants, 3.8% of females, and 4.1% of urban participants. We used chained multiple imputation to impute missing data.
Screening scenarios
We simulated screening of a cohort of adults aged 35 years and older with no previous history of CVD (angina, coronary artery disease, myocardial infarction or stroke). We modelled programs that would screen at 70% of the capacity of HLCs (20 patients per week in 1,000 HLCs) for 48 weeks of one year (672,000 people), with follow-up of the cohort for 10-years.
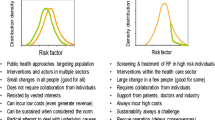
We modelled two main modifications to the current screening protocol that would change the risk prediction tool and the age group screened (Fig. 1). We compared eight screening tools consisting of office- and laboratory-based versions of each of WHO International Society of Hypertension (WHO-ISH) [11], WHO-2019 [28], Framingham [10], and Globorisk [29] (current protocol: office-based WHO-ISH). We used tool-specific definitions of each risk factor used for predictions (Additional file 1: Table S1). We compared three age groups: 40–65 years (previous protocol), 35 years and older (35 +) (current protocol), and 40 years and older (40 +). In all scenarios modelled, screening included glucose tests. Scenarios that used lab-based risk tools also included cholesterol tests in the initial screening.
Screening and treatment parameters modelled in previous protocol, current protocol and potential scenarios. Notes: a Office- and lab-based risk tools modelled. Current protocol deviates from previous protocol only in age group screened and definition of high CVD risk. b These parameter values were only assessed as part of the previous protocol. In all, there were 129 scenarios (8 × 2 × 2 × 2 × 2 + 1) including the base case. In the main text, we show results for scenarios that used WHO-ISH and WHO-2019 tools. Results for scenarios that used Framingham and Globorisk are in Additional file 1
Treatment scenarios
In all scenarios modelled, those with blood pressure ≥ 140/90 would be given antihypertensives. Those with fasting blood glucose ≥ 126 mg/dL or random blood glucose ≥ 200 mg/dL would be given hypoglycaemics. In scenarios with lab-based risk tools, those with a total cholesterol ≥ 300 mg/dL would be given statins.
We modelled scenarios that differed in the criteria used to treat additional groups with statins and antihypertensives. First, we varied the CVD high-risk threshold that is used to determine eligibility for statins, and for lowering the blood pressure threshold in some scenarios, from 30% (previous protocol) to 20% (current protocol) to 10% (potential protocol). Second, we modelled giving statins to all diabetics irrespective of total cholesterol and CVD risk. Third, we modelled lowering the blood pressure threshold for prescription of antihypertensives to 130/80 for all diabetics and those classified as high CVD risk.
We modelled follow-up according to the Sri Lankan screening guidelines [17]. Anyone classified as high CVD risk was assumed to be followed up and given a glucose test twice per year. Those who were not high CVD risk but who qualified for any medication were assumed to be followed up and given a glucose test once per year, with an additional follow-up in the initial year. We assumed that all those qualifying for these medications continued to require them after the first year of follow-up. For scenarios with laboratory-based risk tools, total cholesterol was assumed to be measured on each follow-up visit if the initial CVD risk was high. For diabetics, we only modelled follow-up for management of CVD risk, not for diabetes management.
Outcomes
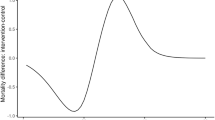
We used a Markov model with a 1-year cycle for the first 10 years of modelling (Fig. 2). For all scenarios, we fed each individual’s risk factor data into the WHO-2019 laboratory risk tool to estimate the 10-year probability of developing each of coronary heart disease (CHD) and stroke assuming that this tool would be the most accurate for the Sri Lankan population (Additional file 1: Figure S1). We converted the 10-year probabilities to 1-year probabilities (Additional file 1: Text S2). The WHO-2019 tool defined CHD as International Classification of Disease-10 (ICD-10) code I21-I25, and stroke as I60-I69. We utilised 2019 Global Burden of Disease estimates of deaths and incidence of ischaemic heart disease and stroke, by sex and five-year age group [30] to produce mortality ratios for each individual age (Additional file 1: Figure S2). The transition probabilities for a non-fatal event to death in subsequent cycles were obtained by transforming 5-year mortality rates post CHD from 1990–1999 in the Framingham cohort [31] and post stroke from 2000–2004 in a Singaporean cohort study [32]. The transition probability from no diagnosed CVD, to death without any CVD event was calculated by age and sex using WHO life tables [33]. Since the focus is on primary prevention, we did not model multiple CVD events, which would be influenced by the intensity of secondary prevention [34]. Mortality risks from non-fatal events included elevated mortality risk caused by any subsequent CVD event. We assumed that all people alive at the end of 10 years will transition to death using the probability of natural death for that age group, regardless of whether they had a CVD event or not. Cycles continued for each participant until death or the participant reached 100 years of age. Each transition was half-cycle corrected.
Markov model of population with no known history of CVD. Notes: All participants started with no diagnosed CVD. Each solid arrow shows a possible transition at each cycle. Dashed lines with arrow show the breakdown within the same cycle: e.g., a stroke event is either non-fatal or fatal, and fatal stroke is related to death
The baseline utility at the start of year 1 was calculated for each participant using a Sri Lankan valuation of their responses to the EQ-5D-5L questionnaire [35]. For each subsequent yearly cycle, we calculated the utility for each individual by applying the marginal disutility of one year increase in age, as well as non-fatal stroke and non-fatal CHD for people who transitioned to these states (Table 1).
Impact of treatment
We used estimates from a metanalysis [37] for the effects of statins on the probabilities of non-fatal stroke and myocardial infarction (as a proxy for CHD). We used another metanalysis [38] for the effects of antihypertensives on the risks of CHD and stroke. We used the conservative estimates of these effects for a baseline blood pressure of 140–159 mmHg. Since this meta-analysis did not distinguish between effects of antihypertensives on CHD and stroke mortality, we used the estimated effect on cardiovascular disease mortality for both conditions. We also assumed, conservatively, that there would be no reduction of CHD or stroke risk after treatment of 10 years, though treatment would continue for the individual’s lifetime.
Costs
We calculated costs over a lifetime horizon from a public health system perspective. Medicines costs, laboratory costs, admission costs for CHD and stroke, and costs of usual care for 2019 were calculated using locally available data (Additional file 1: Text S1). All costs were converted to December 2019 US dollars (US$1 = LKR 181.63), which is the time the SLHAS was completed, the year for which most cost data were available, and an effective way to handle costing in a setting with fluctuating inflation [41].
Cost-effectiveness analysis
The base-case scenario was the current Sri Lanka CVD screening program (Fig. 1). An incremental cost-effectiveness ratio (ICER) was calculated for each alternative scenario. Incremental costs were plotted against incremental QALYs, and cost-effectiveness frontiers drawn. We identified scenarios that were strongly dominated (another scenario produced more QALYs at lower cost) or weakly dominated (another scenario produced more total QALYs at a lower ICER). As there were no cost-effectiveness thresholds (CET) derived from local data, we compared ICERs to a threshold of gross domestic product (GDP) per capita [42]. We also used lower thresholds of half and a quarter of a GDP per capita based on application of an approach to estimate CETs [43,44,45]. We used 2019 GDP per capita in current US dollars of $4,083 [46]. All costs and QALYs were discounted at 3% per year [7]. Subgroup analysis of costs and impact was performed by 5-year age-groups for selected scenarios.
Sensitivity analysis
In a deterministic sensitivity analysis, we tested sensitivity to increasing the effect of antihypertensives on the risk of non-fatal stroke to the higher estimate at SBP ≥ 160 mmHg [33]. We tested reducing the discount rate to 0% and raising it to 6%. We tested the effect of lowering the utility score for myocardial infarction to a value similar to that of stroke [47, 48]. We also tested changing the cost of usual care to 80% and 120% of the value used, and changed the ratio used to inflate the cost of usual care for all people with CHD and stroke to 1 and 3.
In a separate one-way sensitivity analysis, we applied a disutility of 0.00384 to all participants newly prescribed medication, based on a small study from a high-income country [49] to account for a possible burden of taking long-term daily medications [49,50,51]. Although this value aimed to capture the inconvenience of taking medications, “pill disutility” could also apply to the possibility of side-effects [49].
Probabilistic sensitivity analysis (PSA) was performed on all scenarios on the cost-effectiveness frontier that used WHO-ISH or WHO 2019 risk tools, which are most likely to be considered by the Sri Lankan Ministry of Health (MOH). 1,000 simulations were performed, randomly drawing from the distributions in Table 1, and cost-effectiveness acceptability curves (CEAC) were plotted.
We reported using the Consolidated Health Economic Evaluation Reporting Standards (CHEERS) checklist [52] (Additional file 1: Table S2). All analyses were done using Stata V.17.0 (Stata, College Station, Texas, USA).
Results
Table 2 shows the percentage of people newly prescribed medications, the incremental QALYs, incremental costs and ICERs compared to the base case, for selected scenarios that used the WHO-ISH or WHO-2019 risk tools. The same scenarios are shown along with the cost-effectiveness frontier in Fig. 3. The base case, which modelled the current screening protocol (WHO-ISH office tool, 20% risk threshold, 35 +), the old protocol (WHO-ISH office tool, 30% risk threshold, 40–65) and all non-dominated scenarios are included. The results for all other scenarios, including those that used the Globorisk and Framingham screening tools, are shown in Additional file 1: Table S3 and Table S4. Table 2 also shows the ICER from the nearest scenario on the cost-effectiveness frontier.
Cost-effectiveness frontier for all scenarios using WHO-ISH and WHO-2019 risk tools. Notes: Letters denote scenarios labelled in Table 2. Triangles denote scenarios that used the WHO-ISH office tool, filled circles denote scenarios that used the WHO-2019 office tool. The hollow diamond denotes a scenario that used the WHO-2019 tool with hypertension medication at a lower blood pressure threshold. The full diamond denotes a scenario that used the WHO-2019 tool with statins for all diabetics and hypertension medication at a lower blood pressure
Of the 672,000 people screened, the percentage of people newly commenced on at least one of the three medications ranged from 21.2% – 30.5% for antihypertensives, 0.9% – 14.5% for statins, 8.1% – 8.5% for antidiabetics, and 22.3% to 27.2%% for at least one of the three medications. The incremental cost ($19.0 million) of the most expensive scenario on the cost-effectiveness frontier, for screening one cohort and following this cohort over a lifetime is estimated to be 1.5% of the government’s annual recurrent health expenditure in 2019 ($1.3 billion).
The old protocol (Scenario C) was dominated by the current protocol (Scenario “Base” in Table 2). Switching from the WHO-ISH to WHO-2019 tool (Scenario A) was cost saving, with a small loss in QALYs. Using the WHO-2019 tool and changing the age group screened to 40 + (Scenario B) had an ICER of $113 compared to the base case. Reducing the risk threshold to 10% (Scenario D) resulted in a gain of 6,129 QALYs with an ICER of $1,009/QALY. Moving from one scenario to the next most effective scenario along the frontier cost around 0.25 × to 0.5 × GDP per capita per QALY).
WHO-2019 lab tool with cholesterol testing compared to WHO-2019 office tool
The incremental costs and QALYs gained from using the WHO-2019 lab tool are compared to the office tool in Additional file 1: Figure S3 for four combinations of ages screened (35 + or 40 +) and risk thresholds (10% or 20%). Compared with the base case, the ICER of most scenarios using the lab tool are below 0.5 × GDP per capita per QALY. All are dominated by scenarios using the WHO-2019 office tool.
Statins for all diabetics and lowering BP threshold for high-risk individuals
The impact of adding statins for diabetics (SD) and a lowered blood pressure threshold (LBP) for high-risk individuals is shown in Fig. 3 (Scenarios E and F) and Additional file 1: Figure S4. Compared to the base case, adding SD and LBP to the scenarios using WHO-2019 office tools had an ICER of approximately 0.5 × GDP per capita/QALY or less. However, most of the scenarios with SD or LBP lie above the cost-effectiveness frontier (meaning they are dominated by other more cost-effective alternatives). There are two exceptions: Scenario E, which added LBP to scenario D (WHO-2019, 10%, 40 +) has an ICER of 1,511 (less than 0.5 × GDP per capita/QALY) compared to scenario D, and lies on the cost-effectiveness frontier. Scenario F, which further adds SD to scenario E, also lies on the cost-effectiveness frontier, however it has a higher ICER of $2,090/QALY (0.5 × GDP per capita/QALY) compared to scenario E.
Framingham and Globorisk tools
The impact of switching from WHO-2019 office to Framingham office and Globorisk office tools are shown in Additional file 1: Figure S5. Almost all scenarios with Framingham and Globorisk tools are dominated by scenarios using WHO-2019 office tools. Globorisk scenario G, which uses a 20% threshold, lies on the cost-effectiveness frontier close to scenarios using the WHO-2019 tool with a 10% threshold. Whilst some scenarios on the cost-effectiveness frontier using the Globorisk tool generate the highest impact, they also have larger ICERs (0.8 – 2.3 × GDP per capita/QALY) in comparison to the closest cheaper model on the frontier.
Sensitivity analysis
Results of the deterministic sensitivity analysis are shown in Fig. 4 for Scenario F (WHO-2019 office, 10% threshold, 40 + , SD and LBP). Increasing the impact of antihypertensives on stroke reduced the ICER by 8% to $1,352/QALY from $1,464/QALY. Increasing the discount rate to 6% reduced the ICER to $1,198/QALY, whilst removing the discount rate increased the ICER to $1,886/QALY. Increasing the disutility of having a myocardial infarction reduced the ICER to $1,308/QALY. Deflating and inflating the estimated costs for usual care by 20% changed the ICER marginally. Reducing the relative costs of usual care for CHD stroke patients to be the same as the general population increased the ICER to $1,520/QALY, and increasing the relative costs to be three times that of the general population reduced the ICER to $1,400 per QALY. Results from the PSA are shown in Additional file 1: Figure S6. All scenarios on the cost-effectiveness frontier have more than an 90% probability of having an ICER of 0.5 × GDP per capita/QALY or less.
Sensitivity to pill-taking disutility
Overall, when pill-taking disutility is included, the QALY gain is diminished and ICERs increase, particularly in scenarios which place a large proportion of individuals on new medication. Scenarios using the Globorisk tool (H, I) on the cost-effectiveness frontier, and scenarios using the Framingham and Globorisk tool with 10% thresholds move from costing less than 0.5 × GDP per capita/QALY when the pill-taking disutility is set to 0 (Additional file 1: Figure S5), to more than 0.5 × GDP per capita/QALY when pill-taking disutility is -0.00384 (Additional file 1: Figure S7).
Impact by age group
The incremental costs and impact by age group for Scenario F (WHO-2019 office, 10% threshold, 40 + , SD and LBP scenario) are shown in Additional file 1: Figure S8. In general, older age groups have lower ICERs than younger age groups.
Discussion
Switching the Sri Lankan CVD screening program from the WHO-ISH to WHO-2019 office risk tool would be cost-effective and have a far higher impact, particularly if combined with lowering the high-risk threshold to 10%. Raising the lower age threshold for screening from 35 to 40 years has a very low ICER of $113/QALY. Although lifetime exposure to low-density lipoprotein cholesterol, including in early adulthood can pose a great CVD risk, and so interventions should not neglect younger people [53], we recognise that the health system has limited screening capacity and resources. Given these constraints, greater impact and better cost-effectiveness are achieved by screening adults aged 40 and above. The ICER of younger age-groups is consistently higher than older age groups (Additional file 1: Figure S8).
Prescribing antihypertensives at a lower threshold to people classified as high-risk of CVD and diabetics has an ICER of around 0.25 × GDP per capita/QALY. Prescribing statins to all diabetics regardless of CVD risk is somewhat more expensive, with some scenarios costing around 0.5 × GDP per capita/QALY. Age and gender-specific risk thresholds may be needed for statin initiation given possible side effects, which increase with age [19]. However, a recent metanalysis did not find an increased risk in serious adverse events with low-intensity statin treatment [54]. Nevertheless, in sensitivity analyses, when we modelled a disutility for taking medications, which could also include disutility from potential side-effects, ICERs for all scenarios increased. The scenarios using the WHO-2019 office tool on the cost-effectiveness frontier were robust, and remained on or very close to the new cost-effectiveness frontier, and still had ICERs less than 0.5 × GDP per capita/ QALY. However, scenarios which resulted in larger proportions of people newly commenced on medications were more sensitive to “pill disutility”.
Compared to the current screening protocol, using the WHO-2019 laboratory tool and including cholesterol testing costs less than 1 × GDP per capita/ QALY. However, as it is dominated by scenarios that use the WHO-2019 office tool, it could be argued that the WHO-2019 office tool may be sufficient in resource-constrained environments.
The study used a public health system perspective, which is appropriate since CVD screening protocols are established by the MOH and public healthcare costs are of most interest to decision makers. A societal perspective would include travel costs to facilities, but also the likely much larger increase in labour productivity from reduced CVD events [55] that would be partially offset by future non-medical expenditures [56]. A lifetime perspective is used as CVD preventative treatment is long-term, and restricting analysis to a shorter time period would not capture long-term costs and benefits [57, 58].
While our modelling suggests that modifications to CVD risk screening in Sri Lanka would be highly cost effective, the efficiency gain may not materialise in a real-world situation [5, 59]. Though limited in size and follow-up duration, some studies in LMICs suggest the impact of PEN interventions can be muted due to inadequate follow-up, high drug costs and poor adherence [60]. Sri Lanka has very low drug costs, as well as an established system for follow-up, although public sector drug availability is facing pressures due to the economic crisis [61] that further underlines the importance of cost-effective preventative medicine [62].
Individual-level risk-factor data used in the model are collected in WHO STEPwise approach to surveillance (STEPS) surveys in LMICs [63], suggesting that similar analyses may be feasible in other LMICs with CVD screening programs.
Our findings may assist healthcare policy makers in Sri Lanka to further refine the CVD risk screening protocol for maximal impact. It enriches the evidence base to guide policy makers elsewhere in designing screening protocols that implement the PEN and HEARTS packages.
Limitations
As Sri Lanka does not have data to accurately estimate willingness to pay for QALYs, we could not define cost-effectiveness thresholds that could be used to identify program scenarios as highly, moderately, or not cost-effective. Instead, we provided incremental cost per QALY for all scenarios on the cost-effectiveness frontier [42]. We also compared the ICERs with thresholds of 0.25, 0.5 and 1 × GDP per capita/QALY [64].
We did not recalibrate the CVD risk prediction tools for use in Sri Lanka given the lack of high-quality data on incidence of CVD in the country. However, we do not aim to establish whether each risk tool is accurate, and we did model scenarios that set high CVD risk at various thresholds for each tool.
Several limitations could lead to upwardly biased estimates of ICERs. First, we assumed no impact on morbidity and mortality beyond 10 years, although we modelled the costs of treatment and follow-up over a lifetime. It is possible that the reduction in CVD risks persist beyond 10 years. Second, since the focus was on cardiovascular disease, health gains from diabetes screening and management due to reduced microvascular complications, such as diabetic retinopathy, nephropathy and neuropathy, were not modelled, although the costs of hypoglycemics and yearly glucose checks were included. However, it is expected that most of the reduction in disease burden from diabetes and CVD risk screening programs will come from the prevention of cardiovascular disease, rather than the prevention of other complications of diabetes [65]. Third, conservative estimates were used for impacts of treatment with antihypertensives and statins and for the disutility of myocardial infarction. The sensitivity analysis suggests less conservative estimates would reduce the ICER by 18%. Fourth, we allowed for the potential disutility of pill taking in recognition of the possibility that when potentially a substantial number of people are put on medications many may experience side effects or simply resent the effort of routinely taking medicines. However, there is very little research available in LMICs to quantify this disutility, and we relied on an estimate from a small study in a HIC setting.
Conclusions
Subject to the acknowledged limitations, this study has delivered evidence that modifications to the CVD risk screening program in Sri Lanka would be cost effective. Changing to the WHO-2019 office screening tool, increasing the age at which screening starts to 40 + , lowering the CVD risk threshold for statin treatment to 10%, lowering the blood pressure threshold of high-risk people for prescription of antihypertensives, and prescribing statins to diabetics, are all likely to generate health improvements at reasonable incremental costs.
Availability of data and materials
The data that support the findings of this study are available from the SLHAS Consortium but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. The SLHAS Consortium, which has adopted an Open Data policy will provide access to SLHAS Wave 1 data from 2024, on application to the Consortium by interested researchers. The specific data file used for this paper can be obtained from Nilmini Wijemunige upon reasonable request, and with permission of the SLHAS Consortium.
Abbreviations
- CHEERS:
-
Consolidated Health Economic Evaluation Reporting Standards
- CVD:
-
Cardiovascular Disease
- GDP:
-
Gross Domestic Product
- HEARTS:
-
HEARTS Technical Package for Cardiovascular Disease Management in Primary Health Care
- HLCs:
-
Healthy Lifestyle Centres
- ICD-10:
-
International Classification of Disease-10
- ICERs:
-
Incremental Cost-Effectiveness Ratios
- ISH:
-
International Society of Hypertension
- LBP:
-
Lowered Blood Pressure threshold
- LMICs:
-
Low- and Middle-Income Countries
- PEN:
-
Package of Essential Noncommunicable Disease Interventions
- QALYs:
-
Quality Adjusted Life Years
- SD:
-
Statins for Diabetics
- SLHAS:
-
Sri Lanka Health and Ageing Study
- WHO:
-
World Health Organization
- WHO-ISH:
-
World Health Organization International Society of Hypertension
- WHO-2019:
-
World Health Organization 2019
References
World Health Organisation. WHO package of essential noncommunicable (PEN) disease interventions for primary health care. Geneva: World Health Organisation; 2010.
World Health Organisation. WHO package of essential noncommunicable (PEN) disease interventions for primary health care. Geneva: World Health Organisation 2020:Licence: CC BY-NC-SA 3.0 IGO.
World Health Organization. HEARTS: Technical package for cardiovascular disease management in primary health care. Geneva: World Health Organization; 2018.
World Health Organization. HEARTS D: diagnosis and management of type 2 diabetes. Geneva: World Health Organization; 2020.
Tripathy JP, Mishra S. How effective was implementation of the package of essential non-communicable disease (PEN) interventions: A review of evidence? Diabetes Metab Syndr. 2021;15(5):102266. https://doi.org/10.1016/j.dsx.2021.102266.
Singh K, Chandrasekaran AM, Bhaumik S, et al. Cost-effectiveness of interventions to control cardiovascular diseases and diabetes mellitus in South Asia: A systematic review. BMJ Open. 2018;8(4):e017809. https://doi.org/10.1136/bmjopen-2017-017809.
Sharma M, John R, Afrin S, et al. Cost-Effectiveness of population screening programs for cardiovascular diseases and diabetes in low- and middle-income countries: a systematic review. Front Public Health. 2022;10:820750. https://doi.org/10.3389/fpubh.2022.820750
Moran AE, Farrell M, Cazabon D, et al. Building the health-economic case for scaling up the WHO-HEARTS hypertension control package in low- and middle-income countries. Rev Panam Salud Publica. 2022;46:e140. https://doi.org/10.26633/rpsp.2022.140
Lee JT, Lawson KD, Wan Y, et al. Are cardiovascular disease risk assessment and management programmes cost effective? A systematic review of the evidence. Prev Med. 2017;99:49–57. https://doi.org/10.1016/j.ypmed.2017.01.005.
D’Agostino RB, Vasan RS, Pencina MJ, et al. General cardiovascular risk profile for use in primary care: The Framingham Heart Study. Circulation. 2008;117(6):743–53.
World Health Organization. Prevention of Cardiovascular Disease: Pocket Guidelines for Assessment and Management of Total Cardiovascular Risk. (WHO/ISH Cardiovascular Risk Prediction Charts for WHO epidemiological sub-regions SEAR B, SEAR D). Geneva: WHO, 2007.
Zhang Y, Miao H, Chia YC, et al. Cardiovascular risk assessment tools in Asia. J Clin Hypertens (Greenwich). 2022;24(4):369–77. https://doi.org/10.1111/jch.14336.
Olayemi E, Asare EV, Benneh-Akwasi Kuma AA. Guidelines in lower-middle income countries. Br J Haematol. 2017;177(6):846–54. https://doi.org/10.1111/bjh.14583.
Bibbins-Domingo K, Grossman DC, Curry SJ, et al. Statin use for the primary prevention of cardiovascular disease in adults: US Preventive Services Task Force recommendation statement. JAMA. 2016;316(19):1997–2007.
NICE. Costing report: Lipid modification. Implementing the NICE guideline on lipid modification (CG181). Manchester: NICE; 2014.
U. S. Preventive Services Task Force. Statin use for the primary prevention of cardiovascular disease in adults: US preventive services task force recommendation statement. JAMA. 2016;316(19):1997–2007. https://doi.org/10.1001/jama.2016.15450
Ministry of Health. Cardiovascular Risk Management (Total Cardiovascular Risk Assessment Approach). Guidelines for Primary Health Care providers. Colombo: Ministry of Health 2018.
Enas EA, Dharmarajan TS. The Lipid Association of India (LAI) Expert Consensus Statement on Management of Dyslipidemia in Indians 2016: A Giant Leap Forward! J Assoc Physicians India 2016;64(6):102.
Yebyo HG, Zappacosta S, Aschmann HE, et al. Global variation of risk thresholds for initiating statins for primary prevention of cardiovascular disease: A benefit-harm balance modelling study. BMC Cardiovasc Disord. 2020;20(1):418. https://doi.org/10.1186/s12872-020-01697-6.
Organization WH. Guideline for the pharmacological treatment of hypertension in adults. Geneva: World Health Organization; 2021.
Murphy A, Faria-Neto JR, Al-Rasadi K, et al. World Heart Federation Cholesterol Roadmap. Glob Heart. 2017;12(3):179–97.e5. https://doi.org/10.1016/j.gheart.2017.03.002.
Ray KK, Ference BA, Severin T, et al. World Heart Federation Cholesterol Roadmap 2022. Glob Heart. 2022;17(1):75. https://doi.org/10.5334/gh.1154.
Mallawaarachchi DV, Wickremasinghe SC, Somatunga LC, et al. Healthy Lifestyle Centres: a service for screening noncommunicable diseases through primary health-care institutions in Sri Lanka. WHO South-East Asia Journal of Public Health. 2016;5(2):89–95.
Ministry of Health. Annual Health Bulletin, 2019. Colombo: Ministry of Health; 2021.
Ministry of Health. National Policy and Strategic Framework on Cancer Prevention & Control. Colombo: Ministry of Health, 2014.
Rannan-Eliya RP, Wijemunige N, Perera P, et al. Prevalence and associations of hypertension in Sri Lankan adults: Estimates from the SLHAS 2018–19 survey using JNC7 and ACC/AHA 2017 guidelines. Glob Heart. 2022;17(1):50. https://doi.org/10.5334/gh.1135.
Wijemunige N, Rannan-Eliya RP, Maurer J, et al. Cost-effectiveness and distributional impact of opportunistic screening for people at high-risk of cardiovascular disease in Sri Lanka: A modelling study. Glob Heart. 2022;17(1):89. https://doi.org/10.5334/gh.1174.
WHO CVD Risk Chart Working Group. World Health Organization cardiovascular disease risk charts: revised models to estimate risk in 21 global regions. Lancet Glob Health. 2019;7(10):e1332–45. https://doi.org/10.1016/S2214-109X(19)30318-3.
Ueda P, Woodward M, Lu Y, et al. Laboratory-based and office-based risk scores and charts to predict 10-year risk of cardiovascular disease in 182 countries: a pooled analysis of prospective cohorts and health surveys. Lancet Diabetes Endocrinol. 2017;5(3):196–213.
Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2019 (GBD 2019) Results. Seattle, United States: Institute for Health Metrics and Evaluation (IHME), 2020.
Velagaleti RS, Pencina MJ, Murabito JM, et al. Long-term trends in the incidence of heart failure after myocardial infarction. Circulation. 2008;118(20):2057–62. https://doi.org/10.1161/CIRCULATIONAHA.108.784215.
Sun Y, Lee SH, Heng BH, et al. 5-year survival and rehospitalization due to stroke recurrence among patients with hemorrhagic or ischemic strokes in Singapore. BMC Neurol. 2013;13:133. https://doi.org/10.1186/1471-2377-13-133.
World Health Organization. Life Tables by country (GHE: Life tables). 16/12/2020 ed: World Health Organization, Global Health Observatory, 2020.
Perel P, Avezum A, Huffman M, et al. Reducing premature cardiovascular morbidity and mortality in people with atherosclerotic vascular disease: The World Heart Federation roadmap for secondary prevention of cardiovascular disease. Glob Heart. 2015;10(2):99–110. https://doi.org/10.1016/j.gheart.2015.04.003.
Kularatna S, Chen G, Byrnes J, et al. Mapping Sri Lankan EQ-5D-3L to EQ-5D-5L value sets. Value Health Reg Issues. 2017;12:20–3. https://doi.org/10.1016/j.vhri.2017.01.001.
Institute for Health Policy. IHP Analaysis of Registrar General’s Mortality Data, Sri Lanka. Sri Lanka: Registrar General’s Department; 2015.
Mills EJ, Wu P, Chong G, et al. Efficacy and safety of statin treatment for cardiovascular disease: a network meta-analysis of 170,255 patients from 76 randomized trials. QJM. 2011;104(2):109–24. https://doi.org/10.1093/qjmed/hcq165.
Brunstrom M, Carlberg B. Association of blood pressure lowering with mortality and cardiovascular disease across blood pressure levels: a systematic review and meta-analysis. JAMA Intern Med. 2018;178(1):28–36. https://doi.org/10.1001/jamainternmed.2017.6015.
Amarasinghe SN, Dalpatadu KCS, Rannan-Eliya RP. Sri Lanka Health Accounts: National Health Expenditure 1990–2019. Colombo: Institute for Health Policy 2021.
Perera C, Rannan-Eliya RP, Senanayake S, et al. Public Hospital Inpatient Discharge Survey 2005. Colombo: Institute for Health Policy, 2006.
Turner HC, Lauer JA, Tran BX, et al. Adjusting for inflation and currency changes within health economic studies. Value Health. 2019;22(9):1026–32. https://doi.org/10.1016/j.jval.2019.03.021.
Marseille E, Larson B, Kazi DS, et al. Thresholds for the cost-effectiveness of interventions: alternative approaches. Bull World Health Organ. 2015;93(2):118–24. https://doi.org/10.2471/BLT.14.138206.
Woods B, Revill P, Sculpher M, et al. Country-level cost-effectiveness thresholds: initial estimates and the need for further research. Value Health. 2016;19(8):929–35. https://doi.org/10.1016/j.jval.2016.02.017.
Ochalek J, Lomas J, Claxton K. Estimating health opportunity costs in low-income and middle-income countries: a novel approach and evidence from cross-country data. BMJ Global Health 2018;3(6):e000964. doi: https://doi.org/10.1136/bmjgh-2018-000964
Kazibwe J, Gheorghe A, Wilson D, et al. The use of cost-effectiveness thresholds for evaluating health interventions in low- and middle-income countries from 2015 to 2020: a review. Value Health. 2022;25(3):385–9. https://doi.org/10.1016/j.jval.2021.08.014.
World Bank. World Development Indicators. Washington (DC): World Bank Group, 2022.
Pandya A, Sy S, Cho S, et al. Cost-effectiveness of 10-year risk thresholds for initiation of statin therapy for primary prevention of cardiovascular disease. JAMA. 2015;314(2):142–50. https://doi.org/10.1001/jama.2015.6822.
Smith L, Atherly A, Campbell J, et al. Cost-effectiveness of a statewide public health intervention to reduce cardiovascular disease risk. BMC Public Health. 2019;19(1):1234. https://doi.org/10.1186/s12889-019-7573-8.
Heller DJ, Coxson PG, Penko J, et al. Evaluating the impact and cost-effectiveness of statin use guidelines for primary prevention of coronary heart disease and stroke. Circulation. 2017;136(12):1087–98. https://doi.org/10.1161/circulationaha.117.027067.
Fontana M, Asaria P, Moraldo M, et al. Patient-accessible tool for shared decision making in cardiovascular primary prevention: balancing longevity benefits against medication disutility. Circulation. 2014;129(24):2539–46. https://doi.org/10.1161/CIRCULATIONAHA.113.007595.
Hutchins R, Viera AJ, Sheridan SL, et al. Quantifying the utility of taking pills for cardiovascular prevention. Circ Cardiovasc Qual Outcomes. 2015;8(2):155–63. https://doi.org/10.1161/CIRCOUTCOMES.114.001240.
Husereau D, Drummond M, Augustovski F, et al. Consolidated Health Economic Evaluation Reporting Standards (CHEERS) 2022 explanation and elaboration: a report of the ISPOR CHEERS II Good Practices Task Force. Value Health. 2022;25(1):10–31. https://doi.org/10.1016/j.jval.2021.10.008.
Heidenreich PA, Clarke SL, Maron DJ. Time to relax the 40-year age threshold for pharmacologic cholesterol lowering. J Am Coll Cardiol. 2021;78(20):1965–7. https://doi.org/10.1016/j.jacc.2021.08.072.
Chou R, Cantor A, Dana T, et al. Statin use for the primary prevention of cardiovascular disease in adults: updated evidence report and systematic review for the US preventive services task force. JAMA. 2022;328(8):754–71. https://doi.org/10.1001/jama.2022.12138.
Epstein D, García-Mochón L, Kaptoge S, et al. Modeling the costs and long-term health benefits of screening the general population for risks of cardiovascular disease: a review of methods used in the literature. Eur J Health Econ. 2016;17(8):1041–53. https://doi.org/10.1007/s10198-015-0753-2.
Meltzer D. Accounting for future costs in medical cost-effectiveness analysis. J Health Econ. 1997;16(1):33–64. https://doi.org/10.1016/s0167-6296(96)00507-3.
Grover SA, Coupal L, Lowensteyn I. Determining the cost-effectiveness of preventing cardiovascular disease: are estimates calculated over the duration of a clinical trial adequate? Can J Cardiol. 2008;24(4):261–6. https://doi.org/10.1016/s0828-282x(08)70174-0.
Hiligsmann M, Wyers CE, Mayer S, et al. A systematic review of economic evaluations of screening programmes for cardiometabolic diseases. Eur J Public Health. 2017;27(4):621–31. https://doi.org/10.1093/eurpub/ckw237.
Maningat P, Gordon BR, Breslow JL. How do we improve patient compliance and adherence to long-term statin therapy? Curr Atheroscler Rep. 2013;15(1):291. https://doi.org/10.1007/s11883-012-0291-7.
Capuno J, Kraft A, O'Donnell O. Effectiveness of clinic-based cardiovascular disease prevention: a randomized encouragement design experiment in the Philippines. Soc Sci Med. 2021;283:114194. https://doi.org/10.1016/j.socscimed.2021.114194
Sarkar S. The devastating health consequences of Sri Lanka's economic collapse. BMJ. 2022;377:o1543. https://doi.org/10.1136/bmj.o1543
Matthias AT, Jayasinghe S. Worsening economic crisis in Sri Lanka: impacts on health. Lancet Global Health. 2022;10(7):e959. https://doi.org/10.1016/S2214-109X(22)00234-0
Riley L, Guthold R, Cowan M, et al. The World Health Organization STEPwise approach to noncommunicable disease risk-factor surveillance: methods, challenges, and opportunities. Am J Public Health. 2016;106(1):74–8. https://doi.org/10.2105/AJPH.2015.302962.
Bertram MY, Lauer JA, De Joncheere K, et al. Cost-effectiveness thresholds: pros and cons. Bull World Health Organ. 2016;94(12):925–30. https://doi.org/10.2471/BLT.15.164418.
Basu S, Wagner RG, Sewpaul R, et al. Implications of scaling up cardiovascular disease treatment in South Africa: a microsimulation and cost-effectiveness analysis. Lancet Glob Health. 2019;7(2):e270–80. https://doi.org/10.1016/s2214-109x(18)30450-9.
Acknowledgements
The authors thank their colleagues in the Sri Lanka Health and Ageing Study consortium, consisting of the Institute for Health Policy, University of Colombo, University of Ruhuna and University of Peradeniya, for their input into the design of the survey tools and support of data collection, in particular Dr Renuka Jayatissa (Medical Research Institute) whose staff supported the laboratory analyses; and colleagues in the Ministry of Health, who facilitated the SLHAS, in particular, Dr Sridharan (Deputy Director General (Planning), Ministry of Health), and Dr Anuji Gamage (Kotelawala Defence University). We also thank Professor Vajira Dissanayake for his comments on the final draft of the paper.
Funding
The data collection underlying this research, and analysis, was supported by the Swiss Agency for Development Cooperation (SDC) and the Swiss National Science Foundation (SNSF) through the Swiss Programme for Research on Global Issues for Development (r4d programme) by the grant “Inclusive social protection for chronic health problems” (Grant number 400640_160374), and the Institute for Health Policy Public Interest Research Fund (Grant number PIRF-2018–02).
Author information
Authors and Affiliations
Contributions
NW, RRE and OOD conceived and designed the study. NW and RRE carried out data collection, analysis and interpretation of data. NW wrote the first draft. OOD and PVB provided input for critical revisions. All authors contributed to the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethics approval for Sri Lanka Health and Ageing Study data collection and analysis was obtained from the Sri Lanka Medical Association (ERC/18–022). Informed consent was obtained from all individual participants included in the study. Only participants who were able to provide valid informed consent were recruited, and exclusion criteria included those with mental or cognitive impairment who were not able to give informed consent. No clinical or patient data were accessed in SLHAS apart from what was obtained from participants and personal records the participants shared with us with their consent. The analysis for this paper was done on deidentified data which cannot be linked back to individuals. Data collection and analysis was carried out in accordance with relevant guidelines and regulations in the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
Variables and definitions used for screening tools. Table S2. CHEERS checklist. Table S3. Incremental costs, QALYs and ICERs of all scenarios (sorted by incremental costs). Table S4. Incremental costs, QALYs and ICERs of all scenarios (sorted by scenario). Table S5. Distribution of inpatient and outpatient encounters, costs, and cost per capita. Table S6. Coefficients and 95% confidence intervals of negative binomial regression to assess the impact of CHD and stroke on inpatient and outpatient encounter numbers. Figure S1. Comparison of percentage of people who will develop cardiovascular disease between 2019-2028 by age and prediction tool. Figure S2. Mortality rates by age and gender, for coronary heart disease and stroke. Figure S3. Comparison of ICERs of the current protocol, and proposed scenarios using the WHO-2019 lab tool versus WHO-2019 office tool. Figure S4. Cost‑effectiveness frontier - LBP and SD for WHO 2019 office risk tool.Figure S5. Comparison of ICERs of the old program, and proposed programs using any risk tool, and modifying risk thresholds and age-groups screened . Figure S6. Probabilistic sensitivity analysis of scenarios on the cost‑effectiveness frontier. Figure S7. Impact on cost, impact and cost-effectiveness frontier, when including pill disutility . Figure S8. Incremental costs and QALYs by age category for Scenario G (WHO-2019 office, 10% threshold, 40+, SD and LBP) model compared to the base-case. Text S1. Text S2.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wijemunige, N., Rannan-Eliya, R.P., van Baal, P. et al. Optimizing cardiovascular disease risk screening in a low-resource setting: cost-effectiveness of program modifications in Sri Lanka modelled with nationally representative survey data. BMC Public Health 23, 1792 (2023). https://doi.org/10.1186/s12889-023-16640-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-023-16640-5