Abstract
Background
Previous investigations have primarily examined the relationship between various dietary patterns and the risk of chronic obstructive pulmonary disease (COPD); however, there have been limited studies that have evaluated the association between diet quality presented by Healthy Eating Index 2010 (HEI-2010) and COPD. The aim of this study was to investigate this association in Iranian population.
Methods
This case-control study recruited 84 cases and 252 healthy controls who were randomly selected. Diet, smoking, and physical activity were assessed using validated questionnaires. The HEI-2010 score ranged from zero to hundred twenty, with zero indicating an unhealthy diet and hundred twenty indicating a healthy diet. Logistic regression models were utilized to analyze the association between HEI-2010 and the odds of COPD.
Results
Results from logistic regression showed that individuals with higher HEI scores had a significantly lower odds of COPD (OR: 0.34; 95% CI: 0.16–0.72). After adjusting for confounders, individuals with the highest HEI score were 82% less likely to have COPD (OR: 0.18; 95% CI: 0.03–0.96). This association remained significant after adjusting for smoking and physical activity (OR: 0.08; 95% CI: 0.01–0.93) and with additional adjustment for BMI (OR: 0.08; 95% CI: 0.01–0.92).
Conclusions
This study found a significant association between a higher HEI-2010 score and a lower odd of COPD in the Iranian population. These results suggest that a healthy diet may play a crucial role in reducing the odds of COPD and in improving the function of the lungs. However, further prospective studies are warranted to elucidate this relationship.
Similar content being viewed by others
Background
COPD is a major global health issue that causes a significant burden on countries worldwide. According to the World Health Organization (WHO), Chronic obstructive pulmonary disease (COPD) is the third leading cause of death worldwide, causing 3.23 million deaths in 2019 [1]. It is described as progressive and poorly reversible disease of the lungs with significant morbidity and mortality [2]. Incidence of COPD is increasing due to prevalence of smoking and advanced age [3]. The worldwide mean prevalence of COPD is 13.1%, but the rate differs significantly among countries and populations [4]. Patients with COPD are at increased risk of developing pneumonia [5], lung cancer [6], and cardiovascular diseases [7], among others. The economic burden of COPD in USA reached $32.1 billion in 2010, and have increased to 49 billion in 2020 [8].
Although smoking is the leading cause of impaired lung function, several other factors, including diet, contribute to COPD incidence [9]. In terms of diet, an inverse association between higher dietary intake of fiber, fruit and vegetables, and fish and lower risk of COPD have been found in previous studies [10,11,12]. However, examining the link between whole diet and chronic conditions can provide additional information. The Healthy Eating Index (HEI) is a measure of whole diet quality that assesses the adherence to the dietary guidelines [13]. The association between HEI and risk of several conditions, including obesity [14], depression [15], diabetes [16], and mortality [17] was examined in earlier publications. While previous studies have found a protective association between a prudent dietary pattern (rich in whole grains, fish, vegetables, and fruits) and COPD [18,19,20], no study has yet examined the relationship between HEI-2010 and COPD, despite several dietary factors being associated with COPD in previous publications [21,22,23].
It must be kept in mind that the associations between dietary intakes and risk of COPD were mainly examined in western countries [24, 25] and limited information are available in this regard from developing nations [26]. This is particularly relevant when the dietary intakes of people in developing countries, especially those in the Middle East, are significantly different from those in western countries [27]. For instance, people in the Middle East are taking a higher percent of their energy from carbohydrates [28], which are mostly from refined sources. In addition, they are experiencing a nutrition transition, moving from their healthy traditional diets to non-healthy western diets [29]. There is evidence that the spread of Western diet and lifestyle worldwide has led to an increase in the availability and affordability of foods associated with a Western diet in developing countries [30]. Also, prevalence of factors contributing to COPD might be geographically different. Smoking [31], physical activity [32] and air pollution [33] may differ between regions and countries. Therefore, examining the association between diet and COPD in specific regions can provide valuable insights into the diet-disease link. In this study, we aimed to assess the association between adherence to the HEI-2010 and odds of COPD in a specific region of Iran. While our findings may not be generalizable to the entire Iranian population, they provide important information about the relationship between diet and COPD in this particular region.
Methods and materials
Participants
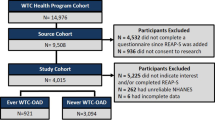
This case-control study was done in Al-Zahra University Hospital Isfahan, Iran, between 2015 and 2016. Sample size was calculated using type 1 error as 5% and study power of 90%. The ratio of control to cases was considered as 3 to 1 and the odds ratio of COPD among those in the highest score of HEI-2010 was compared to those in the lowest score and was considered as 1.5. The common ratio was considered as 0.25 for those who were at the highest score of HEI-2010. Using this information, we reached 84 cases and 252 controls. Cases were randomly selected from the hospital database using a computer-generated random number sequence. Random sampling was used to ensure that the cases were representative of the population of interest and to minimize selection bias. 84 newly diagnosed COPD patients were recruited in Al-Zahra University hospital in Isfahan, Iran. Cases in our study were patients over the age of 30 who had been diagnosed with COPD by a pulmonologist. The diagnosis was based on the results of a spirometry test, which measures lung function. Specifically, patients were considered to have COPD if their forced expiratory volume in 1 s (FEV1) divided by their forced vital capacity (FVC) was less than 70%, or if their FEV1 was less than 80% of the predicted value [34]. The control group consisted of 252 healthy controls without a history of COPD from the same hospital. Cases and controls were matched in terms of age (range 5 years) and sex. Controls were subjects at the same hospital as the cases who attended outpatients’ clinics and were recruited at the same time as the cases. Inclusion criteria for cases was being diagnosed with COPD based on physician diagnosis and spirometry test. We excluded participants if they had a history of a stroke, dementia, or any health condition that would prevent them from an interview. Also, individuals having renal failure, inflammatory bowel disease, long time treatment by steroids drugs, severe heart failure, chronic infections (tuberculosis, HIV etc.), chronic liver cirrhosis, cachexia, uncontrolled thyroid disease, rheumatoid arthritis, cancer in the past 3 years, and other pulmonary problems were not included in the study due to their impact on the ability to respond to the interview or their effect on the patients’ dietary pattern. Finally, all 336 participants participated in the study (supplementary figure). To control selection bias in our study, adjustment for the matching variables (age and sex) were done in the logistic regression analysis and “balanced matching” was applied to improve test power [35]. Also, we have carefully selected our controls from the same source population as our cases and have ensured that they are representative of the exposure distribution in the source population. Additionally, we have used stratification and other statistical methods to control potential confounding factors that could have caused selection bias. The whole project was approved by institutional review board (IRB) of Isfahan University of Medical Sciences, Isfahan, Iran. All participants have signed an informed consent.
Dietary intakes assessment
Assessment of usual dietary intakes of participants over the past year was done using 168-item semiquantitative FFQ where its validity and reliability was mentioned previously [36]. The FFQ included 168 food items where each food item had a standard serving size commonly consumed by Iranians. Face-to-face interview was done by a trained interviewer. All study subjects were requested to report their consumption frequency of a given food item in the previous year on a daily, weekly, or monthly basis considering the serving size given for each food item. Reported frequency consumptions were converted to grams per day using household measures by multiplying the frequency of each food to its specific serving size [37]. To compute nutrient intakes from the FFQ, we used the Nutritionist IV software [38, 39], which was modified for Iranian foods. This software allowed us to accurately estimate energy, macronutrient, micronutrient, and HEI-2010 food group intakes for each participant based on their reported consumption frequencies. Energy intake was computed by summing the caloric content of all reported foods. Macronutrient intakes were calculated by summing the intakes of carbohydrates, proteins, and fats from all reported foods. Micronutrient intakes were estimated by summing the intakes of vitamins and minerals from all reported foods. Finally, HEI-2010 food group intakes were measured by classifying each reported food item into one of the HEI-2010 food groups and summing the intakes of all foods within that group.
Construction of HEI-2010
Assessment of diet was done using the HEI-2010 index considered as a reference for a healthy diet [40]. It’s composed of 12 food groups: fruits (including fruit juice and whole fruit), refined grains, vegetables, whole grains, dairy, beans and greens, protein foods, plant proteins and sea food, fatty acids, empty calories, and sodium). No data about alcohol intake was assessed in this study. To construct HEI-2010 score, we used the residual method to calculate the intake of all food groups after adjusting for energy intake. Then we categorized participants according to the decile categories of these food components. In each of the 12 HEI-2010 food groups, decile categories were made. Participants have the highest score of 10 when they were in the highest decile category of the healthy food group (i.e., fruits, whole grains, vegetables, nuts and legumes, long chain omega-3 fats and polyunsaturated fatty acids), while they scored the lowest score of 0 when they were in the lowest decile category of these food groups. Regarding the unhealthy food groups (i.e., red and processed meat, sugar sweetened drinks, fruit juice, sodium intake, trans fat, saturated fatty acids and added sugars), a score of 10 was given for participants in the lowest decile category of these food groups, whereas a score of zero was given for participants on the highest deciles of these food groups. Participants in the deciles 9 to 2 (counting downwards) of these food items took the scores of 2 to 9 (counting upwards) respectively. Finally, to determine HEI-2010 score, scores were summed up to reach a score ranging from zero to hundred twenty.
Assessment of pulmonary function
A trained technician assessed the lung function using spirometry testing and FEV1, FVC, and FEV1/FVC were acquired. Some important respiratory symptoms include breathlessness, sputum production and chronic cough. Chronic cough is characterized as coughing for greater than 3 weeks [41]. Sputum production refers to production of sputum for more than 3 months in 2 consecutive years [42, 43]. Breathlessness is described using a visual analogue scale which is a 100-mm horizontal line with clarifying words on both sides to help individuals elaborate about their breathlessness rate using graphical observation [44]. Shortness of breath was measured using a spirometry test.
Assessment of other variables
Data on socio-demographic variables that included information about age, education level (illiterate, elementary, high school, diploma, university), marital status (single, married, widow, divorced), gender, socioeconomic status (owning a car, owning a home and employment) and family history of pulmonary disorders were collected using a questionnaire. Weight was measured with individuals in minimal cloth with no shoes to the nearest 100 g. Height was carried out with individuals’ bare feet and with relaxed shoulders. Body mass index (BMI) was computed as weight (kg) divided by height (m2). Physical activity was evaluated by the long form of International Physical Activity Questionnaire and expressed as MET-h/wk where its validity was mentioned elsewhere [45, 46]. Information about cigarette smoking (active smoker (smoking at least one cigarette a day) or using waterpipe (i.e. hookah), ex-smoker (someone who has smoked more than 100 cigarettes in their lifetime but has not smoked in the last 28 days) and non-smoker (not smoking tobacco), as well as passive smoking (involuntary inhaling of smoke from other people’s cigarettes, cigars, or pipes)) were also collected using a pre-tested self-administered questionnaire. The smoking questionnaire used in our study was pre-tested to ensure its validity and reliability. This involved administering the questionnaire to a small sample of participants and analyzing their responses to identify any issues with the questions or response options. Based on the results of the pre-test, revisions were made to the questionnaire to improve its clarity and accuracy [47].
Statistical methods
For continuous variables independent sample Student’s t test was used, whereas for categorical variables the chi-square test. The dietary intakes and general characteristics were also assessed across categories of the HEI-2010 score using ANOVA test (one-way analysis of variance) applied for continuous variables while chi-square test applied for categorical variables. Conditional logistic regression was fitted to assess the association between HEI-2010 score and COPD by using multi-models. Gender (male/female), residence (urban/ industrial/rural), age (continuous), relationship status (married/single/divorced), social economic status (SES) (employment, owning a car/home), education level (illiterate, elementary, high school, diploma, university), family history of COPD (yes/no) were adjusted for in the first model. Physical activity and smoking were additionally adjusted in the second model. We adjusted further for body mass index (BMI) in the third model. Confounders were selected in reference to earlier publications. The IBM SPSS statistics 25 program was used for the statistical analyses carried in this study. Level of significance was measured at p < 0.05.
Results
Table 1 shows descriptive characteristics of cases and control. Cases were more likely to have a positive pulmonary history and less likely to be physically active, educated, employed, married, and owning a car or a home. In terms of smoking status, cases were more likely to be active, passive, non-smokers or using water pipe, while controls were more likely to be previous smokers. No other significant results were reached in respect to other general characteristics of cases and control. As for the distribution of study participants in terms of general characteristics across quartiles of HEI-2010 score, controls in the highest quartiles were more likely to be older, employed, owning a car or a home, physically active compared to those in the lowest quartile. As for cases, subjects in the highest quartile of HEI-2010 score were less likely to be married and more likely to be educated, owning a car or a home compared to those in the lowest quartile. In terms of smoking status, cases in the highest quartile of HEI-2010 score were more likely to be active smokers while less likely to be non-smokers compared to those in the lowest quartile. As for controls, subjects in the highest quartile of HEI-2010 score were less likely to be active smokers, ex-smokers or using waterpipe while more likely to be non-smokers or passive smokers. No other significant results were reached in terms of general characteristics across quartiles of HEI-2010 score.
Table 2 presents the disease severity characteristics of the cases in the study. As expected [48], cases were more likely to have phlegm, cough, while controls were more likely to have higher FEV1% predicted value, FVC and FEV1/FVC ratio. No other significant results were reached in terms of disease severity characteristics across quartiles of HEI-2010 score.
Dietary intakes of cases and controls across the quartiles of HEI-2010 score are presented in Table 3. Cases had higher intakes of total energy, carbohydrates, and vitamin A compared to controls. On the food groups level of HEI-2010 index, participants with COPD had greater intakes of dairy, empty calories while having less intakes of sea food and plant proteins and whole grains. Table 3 presents cases and controls compared in relation to their dietary intake across quartiles of HEI-2010 score levels. Cases in the top category of HEI-2010 score had higher intake of energy, protein, carbohydrates, fiber, and fat compared with participants in the bottom category of HEI-2010 score. In addition, cases in the top quartile of HEI-2010 had higher intakes of calcium, riboflavin, vitamins A, C, and E, thiamin,, and folate compared to individuals in the bottom category. They had also higher intakes of vegetables, whole fruits, dairy, seafood and plant proteins, ,and whole grain compared to those in the lowest category. As for controls, subjects in the highest quartile of HEI-2010 score had higher intakes of energy, carbohydrates, fiber and fats compared to those in the lowest quartile of HEI-2010 score. In terms of micronutrients, controls in the top category og HEI-2010 score have higher intakkes of calcium, riboflavin, vitamin A, E and C, thiamin, niacin and folate compared to those in the lowest category of HEI-2010 score. In terms of HEI-2010 food groups, controls in the top category of HEI-2010 score have higher intakes of whole and refined grains, total and whole fruits, vegetables, dairy, total protein foods and sea food and plant proteins compared to those in the bottom category of HEI-2010 score.
HEI-2010 score and dietary food groups intake of COPD cases according to disease severity are presented in Table 4. Cases in the higher COPD severity level had significantly higher HEI-2010 score and whole grains consumption compared to the lowest COPD severity level. No other significant results were reached in terms of other dietary food groups and COPD severity levels.
Findings from logistic regression about the association between HEI-2010 and COPD are presented in Table 5. Individuals with more compliance to HEI-2010 recommendations (higher HEI score) had significantly lower odds of COPD (OR: 0.34; 95% CI: 0.16–0.72) in comparison to participants having lower HEI-2010 score. After controlling for possible confounders, individuals with the highest HEI score (having more healthy diet) were 82% less prone to have COPD in relation with participants with lowest HEI score (having less healthy diet) (OR: 0.18; 95% CI: 0.03–0.96). This significant association continued after adjusting for smoking and physical activity (OR: 0.08; 95% CI: 0.01–0.93) and with additional adjustment for BMI (OR: 0.08; 95% CI: 0.01–0.92).
Discussion
In this case-control study, we found a significant inverse association between adherence to HEI-2010 recommendations and odds of COPD. This association remained significant after adjusting for several confounding variables. As far as we know, this study is the earliest to examine the association between HEI-2010 and the odds of COPD in a Middle Eastern region.
Chronic Obstructive Pulmonary Disease (COPD) is a significant contributor to morbidity and mortality on a global scale. Our study found that adherence to the HEI-2010 guidelines was linked to a decreased likelihood of COPD. These findings corroborate previous studies that have reported an inverse relationship between healthy dietary patterns and the incidence of COPD [19,20,21, 24, 26, 49,50,51,52,53]. Several studies have investigated the relationship between dietary patterns and the risk of COPD. For instance, a cross-sectional study of American adults found that a higher Dietary Approaches to Stop Hypertension (DASH) diet score was associated with a lower risk of COPD [24] Similarly, a case-control study in Iranian adults reported an inverse association between adherence to a low-carbohydrate diet (LCD) and the odds of COPD [26]. In an Asian population cohort, adherence to multiple recommended dietary patterns was associated with a 14–28% lower risk of death from respiratory diseases [50]. Similarly, the Swiss Cohort Study on Air Pollution and Lung and Heart Diseases in Adults (SAPALDIA) found a protective association between consumption of a diet rich in fruits, vegetables, fish, and nuts and age-related chronic respiratory disease [49]. In contrast, a Chinese population cohort reported that a Western-like dietary pattern was associated with an increased incidence of cough with phlegm [51]. In addition, a study done in Iran found an association between decreased scores of HEI and Mediterranean diet indices and severity of COPD symptoms, but results were not statistically significant [54]. In the mentioned study, the author investigated the association between adherence to healthy dietary patterns and severity of COPD symptoms. In contrast, our current study assessed the association between adhering to HEI-2010 dietary guidelines and the odds of COPD. An important factor considered in this study is the use of HEI-2010 index as a healthy reference for dietary pattern, whereas previous studies used different dietary patterns. Another difference is the low prevalence of smoking among Iranian women compared to other countries [55]. Overall, these findings suggest that healthy dietary intakes may be protectively associated with COPD and its symptoms. However, further studies in developing countries are required to reach firm conclusions.
After prolonged exposure to risk factors like tobacco smoke and air pollution, the primary mechanisms that cause COPD are oxidative stress and inflammation in the lungs and bloodstream [56]. Dietary factors play an important role in improving inflammation, oxidative stress and the regulation of immunity and metabolism [57]. As a result, we hypothesize that the nutritious ingredients in the HEI-2010 diet could potentially hinder or postpone the development of COPD. Additionally, dietary factors may be involved in the modification of the gut microbiota, which can enhance the immunity, metabolism and inflammation by producing short chain fatty acids (SCFAs), considered important active metabolites [57]. Other studies have concluded that diets rich in high-fiber plants, influenced the gut microbiota which enhance the circulation levels of SCFA which in turn have an anti-inflammatory effect. In contrast, diets rich in animal products, which are high in choline and carnitine, have been linked to increased levels of Trimethylamine N-oxide (TMAO), associated with the risk of cardiovascular disorders, atherosclerosis, and death [58]. High dietary fiber intake has been linked to increased levels of SCFAs, which have a protective effect against inflammatory airway disease due to their anti-inflammatory properties [59]. while TMAO levels have been associated with mortality in COPD patients [60]. An evolving concept is the gut-lung axis, where modulation of intestinal microbiota can aid in the management of respiratory diseases [61]. SCFAs have been found in sputum, indicating a link between the lungs and the intestine [62]. They help maintain lung immune-metabolic tone and can act on various parts of the innate immune defenses of the lungs [63]. Butyrate and propionate may help restore and maintain the barrier function of damaged airway epithelium by increasing the expression of ZO-1 tight junction proteins [64]. This is important because airway epithelial barrier dysfunction and impaired tight cell contacts can develop in smoking and COPD [65]. Therefore, SCFAs may have clinical significance in regulating barrier function [64].
Some strengths of the current study include the use of a healthy dietary index rather than individual components of a healthy diet, the use of a validated food frequency questionnaire (FFQ), adjustment for several confounders, and being the first study in a Middle Eastern population to assess the relationship between the HEI-2010 and the risk of COPD. Our study has some limitations that should be considered when interpreting the results. One limitation is the significant differences between the case and control groups in terms of age, marital status, education level, social and economic status, physical activity level, and smoking status. While we adjusted for these variables in our analysis using logistic regression and matched the case and control groups based on age and sex, these differences could still potentially impact our results. Another limitation of our study is the potential residual confounding due to smoking. Despite our efforts to control its effect by adjusting for its confounding effect in logistic regression analysis, it is possible that some confounding remains. Future studies may consider using matching based on smoking status or other methods to better control the confounding effect of smoking. This can help to improve the validity and reliability of the results. Another limitation of our study is the substantial differences in energy consumption and other micronutrient intakes between our case and control groups. While we attempted to account for these differences through adjustment, this method may not completely eliminate their effects. Additionally, our sample size was not large enough to support a stratified analysis based on energy intake levels. As such, the observed associations between dietary intakes and the outcome of interest may be influenced by these differences. Also, The HEI-2010 is an index based on dietary patterns in the USA and may not be applicable in other countries with different dietary habits. Nevertheless, the validity of the HEI-2010 index has been demonstrated in a previous study conducted in an Iranian population where it detected an association with the risk of breast cancer [66]. The case-control design of the study prevents us from drawing conclusions about causality due to selection and recall bias. Measurement errors may result in misclassification of study participants. Given the sample size of the current study, our findings should be generalized with caution.
Conclusion
In our case-control study, we found a significant inverse association between adherence to the HEI-2010 recommendations and the odds of developing COPD in a Middle Eastern population. This association remained significant even after adjusting for several confounding variables. To our knowledge, this is the first study to examine this association in a Middle Eastern region. While previous research has shown that healthy dietary habits can reduce the risk of developing COPD, our study supports these findings by demonstrating that adherence to the HEI-2010 guidelines is associated with a decreased likelihood of COPD. These results are consistent with other studies that have reported an inverse relationship between healthy dietary patterns and the incidence of COPD. Overall, our findings suggest that following a healthy diet, as recommended by the HEI-2010 guidelines, may play an important role in reducing the risk of COPD and improving lung function. Further research is needed to confirm these findings and to better understand the underlying mechanisms of this association.
Availability of data and materials
The datasets generated during and analyzed during the current study are not publicly available due to ethical concerns but are available from the corresponding author on reasonable request.
Abbreviations
- COPD:
-
Chronic obstructive pulmonary disease
- HEI-2010:
-
Healthy Eating index 2010
- SES:
-
Social economic status
- FFQ:
-
Food frequency questionnaire
- BMI:
-
Body mass index
- SCFA:
-
Short chain fatty acids
- TMAO:
-
Trimethylamine N-oxide
- PUFAs:
-
Polyunsaturated fatty acids
- MUFAs:
-
Monounsaturated fatty acids
- CI:
-
Confidence Interval
- OR:
-
Odd Ratio
- SD:
-
Standard Deviation
- ANOVA:
-
One-way analysis of variance
References
Organization WH. Chronic obstructive pulmonary disease (COPD). WHO fact sheet 2023. Available from: https://www.who.int/news-room/fact-sheets/detail/chronic-obstructive-pulmonary-disease-(copd).
Petty TL. The history of COPD. Int J Chronic Obstr Pulm Dis. 2006;1(1):3.
Vogelmeier CF, Criner GJ, Martinez FJ, Anzueto A, Barnes PJ, Bourbeau J, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease 2017 report. GOLD executive summary. Am J Respir Crit Care Med. 2017;195(5):557–82.
Blanco I, Diego I, Bueno P, Casas-Maldonado F, Miravitlles M. Geographic distribution of COPD prevalence in the world displayed by geographic information system maps. Eur Respir J. 2019;54(1):1900610.
Restrepo MI, Sibila O, Anzueto A. Pneumonia in patients with chronic obstructive pulmonary disease. Tuberc Respir Dis. 2018;81(3):187.
Raviv S, Hawkins KA, DeCamp MM Jr, Kalhan R. Lung cancer in chronic obstructive pulmonary disease: enhancing surgical options and outcomes. Am J Respir Crit Care Med. 2011;183(9):1138–46.
Perticone M, Maio R, Caroleo B, Suraci E, Corrao S, Sesti G, et al. COPD significantly increases cerebral and cardiovascular events in hypertensives. Sci Rep. 2021;11(1):7884.
Ford ES, Murphy LB, Khavjou O, Giles WH, Holt JB, Croft JB. Total and state-specific medical and absenteeism costs of COPD among adults aged 18 years in the United States for 2010 and projections through 2020. Chest. 2015;147(1):31–45.
Sorli-Aguilar M, Martin-Lujan F, Flores-Mateo G, Arija-Val V, Basora-Gallisa J, Sola-Alberich R. Dietary patterns are associated with lung function among spanish smokers without respiratory disease. BMC Pulm Med. 2016;16(1):162.
Varraso R, Willett WC, Camargo CA Jr. Prospective study of dietary fiber and risk of chronic obstructive pulmonary disease among US women and men. Am J Epidemiol. 2010;171(7):776–84.
Kaluza J, Larsson SC, Orsini N, Linden A, Wolk A. Fruit and vegetable consumption and risk of COPD: a prospective cohort study of men. Thorax. 2017;72(6):500–9.
Varraso R, Barr RG, Willett WC, Speizer FE, Camargo CA Jr. Fish intake and risk of chronic obstructive pulmonary disease in 2 large US cohorts–. Am J Clin Nutr. 2014;101(2):354–61.
DeSalvo KB, Olson R, Casavale KO. Dietary guidelines for Americans. JAMA. 2016;315(5):457–8.
Guo X, Warden B, Paeratakul S, Bray G. Healthy eating index and obesity. Eur J Clin Nutr. 2004;58(12):1580–6.
Wu P-Y, Lin M-Y, Tsai P-S. Alternate healthy eating index and risk of depression: a meta-analysis and systemematic review. Nutr Neurosci. 2020;23(2):101–9.
Schwingshackl L, Bogensberger B, Hoffmann G. Diet quality as assessed by the healthy eating index, alternate healthy eating index, dietary approaches to stop hypertension score, and health outcomes: an updated systematic review and meta-analysis of cohort studies. J Acad Nutr Dietetics. 2018;118(1):74–100 (e11).
Onvani S, Haghighatdoost F, Surkan P, Larijani B, Azadbakht L. Adherence to the healthy eating Index and Alternative Healthy Eating Index dietary patterns and mortality from all causes, cardiovascular disease and cancer: a meta-analysis of observational studies. J Hum Nutr Dietetics. 2017;30(2):216–26.
Shaheen S, Jameson K, Syddall H, Sayer AA, Dennison E, Cooper C, et al. The relationship of dietary patterns with adult lung function and COPD. Eur Respir J. 2010;36(2):277–84.
Varraso R, Fung TT, Barr RG, Hu FB, Willett W, Camargo CA Jr. Prospective study of dietary patterns and chronic obstructive pulmonary disease among US women. Am J Clin Nutr. 2007;86(2):488–95.
Varraso R, Fung TT, Hu FB, Willett W, Camargo CA. Prospective study of dietary patterns and chronic obstructive pulmonary disease among US men. Thorax. 2007;62(9):786–91.
Varraso R, Chiuve SE, Fung TT, Barr RG, Hu FB, Willett WC, et al. Alternate healthy eating Index 2010 and risk of chronic obstructive pulmonary disease among US women and men: prospective study. BMJ. 2015;350:h286.
Ducharme-Smith K, Mora-Garcia G, de Castro Mendes F, Ruiz-Diaz MS, Moreira A, Villegas R, et al. Lung function, COPD and alternative healthy eating index in US adults. ERJ Open Res. 2021;7(4):00927–2020.
Varraso R, Chiuve S, Fung T, Barr G, Hu F, Willett W, Camargo C. Prospective cohort study of the alternate healthy eating index-2010 and risk of chronic obstructive pulmonary disease in US women and men. Eur Respir J. 2013;42:P1561.
Wen J, Gu S, Wang X, Qi X. Associations of adherence to the DASH diet and the Mediterranean diet with chronic obstructive pulmonary disease among US adults. Front Nutr. 2023;10:10.
Yu W, Pan L, Cao W, Lv J, Guo Y, Pei P, et al. Dietary patterns and risk of Chronic Obstructive Pulmonary Disease among chinese adults: an 11-year prospective study. Nutrients. 2022;14(5):996.
Malmir H, Onvani S, Ardestani ME, Feizi A, Azadbakht L, Esmaillzadeh A. Adherence to low carbohydrate diet in relation to chronic obstructive pulmonary disease. Front Nutr. 2021;8:690880.
Miller V, Webb P, Cudhea F, Shi P, Zhang J, Reedy J, et al. Global dietary quality in 185 countries from 1990 to 2018 show wide differences by nation, age, education, and urbanicity. Nat Food. 2022;3(9):694–702.
Ritchie H, Rosado P, Roser M. "Diet Compositions". Published online at OurWorldInData.org. 2023. Retrieved from: https://ourworldindata.org/diet-compositions. [Online Resource]
Popkin BM, Adair LS, Ng SW. Global nutrition transition and the pandemic of obesity in developing countries. Nutr Rev. 2012;70(1):3–21.
Azzam A. Is the world converging to a ‘Western diet’? Public Health Nutr. 2021;24(2):309–17.
Abdullah A, Husten C. Promotion of smoking cessation in developing countries: a framework for urgent public health interventions. Thorax. 2004;59(7):623–30.
Hoffman DJ. Upper limits in developing countries: warning against too much in lands of too little. J Am Coll Nutr. 2004;23(sup6):610S-615S.
Mannucci PM, Franchini M. Health effects of ambient air pollution in developing countries. Int J Environ Res Public Health. 2017;14(9):1048.
Fernández-Villar A, Represas-Represas C, Mouronte-Roibás C, Ramos-Hernández C, Priegue-Carrera A, Fernández-García S, et al. Reliability and usefulness of spirometry performed during admission for COPD exacerbation. PLoS ONE. 2018;13(3):e0194983.
Rothman KJ, Greenland S, Lash TL. Modern epidemiology (Vol. 3). Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins; 2008.
Esfahani FH, Asghari G, Mirmiran P, Azizi F. Reproducibility and relative validity of food group intake in a food frequency questionnaire developed for the Tehran lipid and glucose study. J Epidemiol. 2010;20(2):150–8.
Ghafarpour M, Houshiar-Rad A, Kianfar H. The manual for household measures, cooking yields factors and edible portion of food. Tehran: Keshavarzi Press; 1999.
Haytowitz D, Lemar L, Pehrsson P, Exler J, Patterson K, Thomas R, et al. USDA national nutrient database for standard reference, release 24. Washington, DC, USA: US Department of Agriculture; 2011.
Orta J. Nutritionist IV for Windows. J Am Diet Assoc. 1994;94(8):936–8.
Guenther PM, Casavale KO, Reedy J, Kirkpatrick SI, Hiza HA, Kuczynski KJ, et al. Update of the healthy eating index: HEI-2010. J Acad Nutr Dietetics. 2013;113(4):569–80.
Des Jardins T, Burton GG. Clinical Manifestations & Assessment of Respiratory Disease-E-Book. Elsevier Health Sciences; 2023.
Pauwels RA, Buist AS, Calverley PM, Jenkins CR, Hurd SS. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: NHLBI/WHO Global Initiative for Chronic Obstructive Lung Disease (GOLD) workshop summary. Am J Respir Crit Care Med. 2001;163(5):1256–76.
Celli BR, MacNee W, Agusti A, Anzueto A, Berg B, Buist AS, et al. Standards for the diagnosis and treatment of patients with COPD: a summary of the ATS/ERS position paper. Eur Respir J. 2004;23(6):932–46.
Mahler DA, Weinberg DH, Wells CK, Feinstein AR. The measurement of dyspnea: contents, interobserver agreement, and physiologic correlates of two new clinical indexes. Chest. 1984;85(6):751–8.
Hallal PC, Victora CG. Reliability and validity of the international physical activity questionnaire (IPAQ). Med Sci Sports Exerc. 2004;36(3):556.
Booth M. Assessment of physical activity: an international perspective. Res Q Exerc Sport. 2000;71(sup2):114–20.
Willis GB. Questionnaire pretesting. The SAGE handbook of survey methodology. 2016;24:359–81.
Venkatesan P. GOLD COPD report: 2023 update. The Lancet Respiratory Medicine. 2023;11(1):18.
Steinemann N, Grize L, Pons M, Rothe T, Stolz D, Turk A, et al. Associations between dietary patterns and post-bronchodilation lung function in the SAPALDIA Cohort. Respiration. 2018;95:454–63.
Neelakantan N, Koh W-P, Yuan J-M, van Dam RM. Diet-quality indexes are associated with a lower risk of cardiovascular, respiratory, and all-cause mortality among chinese adults. J Nutr. 2018;148(8):1323–32.
Butler LM, Koh W-P, Lee H-P, Tseng M, Yu MC, London SJ. Prospective study of dietary patterns and persistent cough with phlegm among chinese Singaporeans. Am J Respir Crit Care Med. 2006;173(3):264–70.
Brigham EP, Steffen LM, London SJ, Boyce D, Diette GB, Hansel NN, et al. Diet pattern and respiratory morbidity in the atherosclerosis risk in communities study. Ann Am Thorac Soc. 2018;15(6):675–82.
McKeever TM, Lewis SA, Cassano PA, Ocke M, Burney P, Britton J, et al. Patterns of dietary intake and relation to respiratory disease, forced expiratory volume in 1 s, and decline in 5-y forced expiratory volume. Am J Clin Nutr. 2010;92(2):408–15.
Yazdanpanah L, Paknahad Z, Moosavi AJ, Maracy MR, Zaker MM. The relationship between different diet quality indices and severity of airflow obstruction among COPD patients. Med J Islamic Repub Iran. 2016;30:380.
Sarraf-Zadegan N, Boshtam M, Shahrokhi S, Naderi GA, Asgary S, Shahparian M, et al. Tobacco use among iranian men, women and adolescents. Eur J Public Health. 2004;14(1):76–8.
Rahman I, Adcock I. Oxidative stress and redox regulation of lung inflammation in COPD. Eur Respir J. 2006;28(1):219–42.
Scoditti E, Massaro M, Garbarino S, Toraldo DM. Role of diet in chronic obstructive pulmonary disease prevention and treatment. Nutrients. 2019;11(6):1357.
De Filippis F, Pellegrini N, Vannini L, Jeffery IB, La Storia A, Laghi L, et al. High-level adherence to a Mediterranean diet beneficially impacts the gut microbiota and associated metabolome. Gut. 2016;65(11):1812–21.
Trompette A, Gollwitzer ES, Yadava K, Sichelstiel AK, Sprenger N, Ngom-Bru C, et al. Gut microbiota metabolism of dietary fiber influences allergic airway disease and hematopoiesis. Nat Med. 2014;20(2):159–66.
Ottiger M, Nickler M, Steuer C, Bernasconi L, Huber A, Christ-Crain M, et al. Gut, microbiota-dependent trimethylamine-N-oxide is associated with long-term all-cause mortality in patients with exacerbated chronic obstructive pulmonary disease. Nutrition. 2018;45:135–41 (e1).
Budden KF, Gellatly SL, Wood DL, Cooper MA, Morrison M, Hugenholtz P, et al. Emerging pathogenic links between microbiota and the gut–lung axis. Nat Rev Microbiol. 2017;15(1):55–63.
Ghorbani P, Santhakumar P, Hu Q, Djiadeu P, Wolever TM, Palaniyar N, et al. Short-chain fatty acids affect cystic fibrosis airway inflammation and bacterial growth. Eur Respir J. 2015;46(4):1033–45.
Liu Q, Tian X, Maruyama D, Arjomandi M, Prakash A. Lung immune tone via gut-lung axis: gut-derived LPS and short-chain fatty acids’ immunometabolic regulation of lung IL-1β, FFAR2, and FFAR3 expression. Am J Physiol-Lung Cell Mol Physiol. 2021;321(1):L65–78.
Richards LB, Li M, Folkerts G, Henricks PA, Garssen J, van Esch BC. Butyrate and propionate restore the cytokine and house dust mite compromised barrier function of human bronchial airway epithelial cells. Int J Mol Sci. 2020;22(1): 65.
Tatsuta M, Kan-o K, Ishii Y, Yamamoto N, Ogawa T, Fukuyama S, et al. Effects of cigarette smoke on barrier function and tight junction proteins in the bronchial epithelium: protective role of cathelicidin LL-37. Respir Res. 2019;20:1–14.
Ghosn B, Benisi-Kohansal S, Ebrahimpour-Koujan S, Azadbakht L, Esmaillzadeh A. Association between healthy lifestyle score and breast cancer. Nutr J. 2020;19(1):1–11.
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
BG and AE contributed to idea conception, design, statistical analyses, data interpretation and manuscript drafting. SO, MEA, AF and LA contributed in data collection and interpretation. AE supervised the study. All authors approved the final manuscript for submission.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving research study participants were approved by the Research Council and Ethical Committee of the School of Nutrition and Food Science, Isfahan University of Medical Sciences, Isfahan, Iran (ethical code: 393881). Written informed consent was attained from all subjects/patients.
Consent for publication
NA.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ghosn, B., Onvani, S., Ardestani, M.E. et al. The association between diet quality and chronic obstructive pulmonary disease: a case-control study. BMC Public Health 23, 2071 (2023). https://doi.org/10.1186/s12889-023-16586-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-023-16586-8