Abstract
Objective
To assess osteoarthritis (OA) patients’ preferences for pharmaceutical treatment via Adaptive Choice-Based Conjoint (ACBC) method.
Methods
A United Arab Emirates (UAE) based Patient and Public Involvement (PPI) group designed the ACBC questionnaire with 10 attributes and 34 levels. The questionnaire was developed using Sawtooth Software and analyzed through Hierarchical Bayesian (HB). Results were standardized using Z-score via SPSS.
Results
Study participants were 1030 OA patients, 83.6% aged 50 or older and 83.4% female. The avoidance of medication’s side effects accounted for 66% relative importance compared to 6% relative importance for the medication’s benefits. The “way of taking the medicine” attribute had the highest coefficient of variation (70%) and the four side effect attributes “risk of gastric ulcer, addiction, kidney and liver impairment, and heart attacks and strokes” had a coefficient of variation from 18 to 21%.
Conclusions
Arab OA patients are similar to other ethnic groups in trading-off benefits and side effects and consistently prioritizing the avoidance of medications’ side effects. Although the “Way of taking medicine” was the least important attribute it was associated with the highest variation amongst patients. OA patients also prefer prescribed medications to internet-purchased and over-the-counter options.
Similar content being viewed by others
Introduction
Osteoarthritis (OA) is a highly prevalent chronic joint disease, affecting 7% of the world population [1,2,3]. The treatment for OA includes non-pharmacological and pharmacological options, which focus on alleviating pain and stiffness and limiting functional loss [4]. Due to the long-term use of the pharmacological treatment and the adverse effects, surgical interventions such as joint replacement may be considered the last option [5, 6].
The assessment of patients’ preferences is a crucial aspect of healthcare systems worldwide [7]. Especially, in the management of non-urgent and non-fatal diseases, such as OA [8]. Appropriate elicitation of patients’ preferences for treatment and involving patients in the shared decision-making (SDM) process can improve disease management and patient adherence [9]. Furthermore, understanding patients’ preferences can aid in balancing the treatment’s benefits and risks [10, 11], and identifying choices of subpopulations with different risk tolerances [12]. Subsequently, the new treatment design and prescription could focus on those attributes that are highly important to the patients.
In Arabic-speaking countries, the burden of chronic diseases is increasing, but the consideration of patients’ opinions regarding treatment options is limited [13, 14]. This leads to the under-representation of patients’ needs and preferences in SDM [15, 16]. While studying patients’ preferences and SDM have been widely implemented in Europe and the United States (US) [17], they have recently acquired some attention in Arabic-speaking countries [18]. The studies examining patient preferences in Arabic countries have used the basic methods and general attributes related to health services assessment [13]. Furthermore, older Arabic patients and those with chronic health conditions prefer a paternalistic approach to their care [19]. This may be correlated to physicians’ perception of prioritizing evidence over SDM, sociocultural barriers, and the perception of patients’ unwillingness to take decisions regarding their health [20]. These concepts of patient preferences and SDM are important in countries such as the United Arab Emirates (UAE) where chronic diseases are highly prevalent, and patients are used to paternalistic approach in healthcare [20,21,22]. Although the UAE government is continuously aiming to improve the healthcare system [23], patient involvement in healthcare remains limited [24].
In OA settings, conjoint analysis (CA), discrete choice experiments (DCEs), best-worst scaling (BWS), and several other methods have been used to elicit patients’ preferences for treatments and understand the trade-offs [8, 25]. Adaptive Choice-Based Conjoint (ACBC) is the most recent and advanced CA technique used to quantify patients’ preferences [26]. The term “Adaptive” refers to the customization of choice tasks to the respondents’ preferred decision criteria [27]. Compared to the conventional methods, the ACBC can assess a large number of attributes (> 5 attributes) [28, 29]. This may help in limiting the extreme response behavior usually encountered in other CA techniques [29]. Additionally, ACBC can also provide information about the second-best options and the unacceptable features of the treatments [29]. However, the ACBC questionnaire takes a longer completion time than the conventional CA as it involves a higher number of attributes and levels [30]. This may cause respondents to be exhausted resulting in incomplete data [31]. Yet, better participants’ engagement while completing the ACBC questionnaire ensures a more accurate prediction of respondents’ choices behavior and may counter the longer completion time [32, 33]. Furthermore, the use of advanced methods such as ACBC can empower patients to discuss their preferences and needs with their physicians, thereby contributing to improved patient-centred care [34].
Despite its potential benefits, the utilization of ACBC in healthcare studies has been limited, especially in OA treatment preferences. Most studies that used ACBC in this context were conducted in the United Kingdom (UK) by Al-Omari and colleagues [26, 35,36,37], and have been performed in the English language. Al-Omari and colleagues reported that patients’ preferences for OA treatment are driven by avoidance of side effects [26, 36]. They also reported that ACBC is a feasible and useful tool to elicit patients’ preferences for OA treatment [36, 37]. However, one of the main limitations of their studies was related to the small sample size (n = 11–43) [26, 35,36,37].
To the best of our knowledge, there is no available literature on the use of the ACBC method in languages other than English. In turn, the few preference studies conducted were associated with small sample sizes. In light of these considerations, the aim of this study is to elicit patients’ preferences for pharmacological treatment for OA in a large sample of OA patients using a web-based Arabic version of the ACBC questionnaire. The primary research question asked in this study is “What drives patients’ preferences for pharmacological treatment among Arab OA patients?”. This will help in addressing the gap in the utilization of this method in non-English speaking populations and enhance patient-centred care in the UAE through a direct reflection of patients’ needs and preferences.
Methods
An Arabic version of the ACBC questionnaire was developed to investigate patients’ preferences when choosing drug treatments for OA. The treatment options were described by a set of attributes, further specified by levels set for each attribute.
Patients and public involvement
In the previous studies conducted by Al-Omari and colleagues [26, 35], the patient and public involvement (PPI) groups were involved in the design of the ACBC questionnaire and the selection of attributes and levels [26].
Since this study was conducted in the UAE, some modifications to the content of the ACBC questionnaire were made to adjust to the cultural and linguistic differences. In the absence of structured PPI groups in the UAE, the researchers formed a group of twenty OA volunteer participants from the public. The volunteers representing both genders (12 females, 8 males), different age groups (25 to 68 years), educational levels (uneducated to master’s degree) and Arab origins (UAE, Jordan, Lebanon, Syria, and Egypt) completed the ACBC questionnaire. The questionnaire web link was sent by email to each participant followed by another email providing the username and password. For validation purposes, participants were then informed of their individual patient preference results and asked if these results were consistent with their stated preferences. All participants confirmed that the ACBC technique predicted their preferences as they intended when they completed the questionnaire. For standardization purposes, each participant was contacted by phone to provide feedback regarding the content and feasibility of using the questionnaire with Arabic OA patients. Subsequently, a few minor amendments to the language of the content were suggested and integrated into the final version of the ACBC questionnaire.
Participants and settings
A cross-sectional study was conducted on OA patients recruited from the rheumatology and orthopedics clinics at one of the hospitals in the United Arab Emirates, Abu Dhabi between January and June 2022. Adult patients 18 years of age and older, suffering from joint pain, and having a diagnosis of OA from their physicians were recruited. Patients who have acute or chronic illnesses that may contribute to their joint pain other than OA (e.g., osteoporosis, rheumatoid arthritis, septic arthritis, lupus, bursitis, joint injuries) were excluded from this study.
The traditional sample size calculation methods cannot be applied to CA studies for practical reasons [38, 39]. Therefore, there is still no consensus regarding the appropriate sample size for CA studies. A recent systematic review of CA studies indicated that it depends on factors such as the number of subgroup analyses, scenarios, and conjoint tasks [40]. However, it is suggested that the sample size for a CA study should not be less than 300 for one group analysis [41]. Furthermore, reducing the sampling and measurement error in CA studies could be achieved by designing high-quality conjoint tasks and collecting more data from each respondent [40, 41]. Taking into consideration that this study conducted one sample group analysis, it aimed to recruit a minimum of 300 participants.
ACBC questionnaire
The ACBC questionnaire was developed using Sawtooth Software Lighthouse Studio version 9.13.1. The first screen introduces the participants to the content of the questionnaire (See supplemental Fig. 1). The next set of screens is related to the participants’ demographics and OA medical history (See supplemental Figs. 2–12). The ACBC task starts after the demographics questions and consists of three sections. The first section is “Build Your Own” which presents a complete list of all the attributes and levels and asks the participants to choose their most preferred level for each attribute (See supplemental Fig. 13). The second section is the “screening section” which consists of multiple scenarios generated by the software and customized based on the participant’s previous answers (See Supplemental Fig. 14) and the ‘must have’ and ‘unacceptable’ questions to customize scenarios matching the individual participant preferences (See supplemental Figs. 15 and 16). The final task consists of choice-based questions where participants can choose their preferred scenario from three sets of scenarios (See supplemental Fig. 17).
Since the Sawtooth software is mainly adapted to the English language, the questionnaire had to be translated into the Arabic language by modifying some of the built-in codes with the assistance of a software developer as recommended by the technical team of Sawtooth Software. Primarily, the questionnaire was developed in English language then translated to Arabic by one of the researchers and reviewed by the lead researcher. The Arabic version of the questionnaire was then reviewed by five native Arabic speakers to confirm the language’s accuracy. The rheumatology and orthopaedics healthcare team also reviewed the Arabic version of the questionnaire before piloting with the PPI.
Defining attributes and levels
The factors that may directly affect patients’ preferences regarding the pharmaceutical treatment of OA were identified as the attributes and levels. The selection of these attributes and levels was based on a previously published systematic review, comprehensive discussion with the PPI group, a previously conducted ACBC feasibility study, and discussions with the physicians, pharmacists of the rheumatology department as well as research methodologists and PPI coordinators.
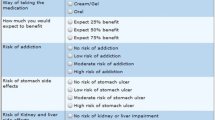
The original pilot study conducted in the United Kingdom (UK) by Al-Omari and colleagues included eight attributes and 28 levels and recruited 11 participants [35]. The “treatment benefit” attribute was split into “mobility improvement” and “pain reduction” resulting in a total of nine attributes and 31 levels and recruited 43 participants in the following study [26]. This current study has a total number of 10 attributes and 34 levels after including the ‘cost’ attribute, since the variation in insurance coverage among UAE patients may affect their preferences for treatment. A full list of the attributes and levels is presented in supplemental Fig. 13. Comprehensive details about the criteria for including the attributes and levels are discussed in previously published studies by Al-Omari and colleagues [26, 40, 42].
Questionnaire validation
For validation purposes, three researchers completed the ACBC questionnaire independently assuming two different characters of participants with extreme preference profiles. At the beginning of the task, investigators were provided with documents explaining the profiles regarding specific pharmacological treatment preferences. The main question this task wanted to address was: Given a clear set of preferences, starting from a different random starting point (which is how the ACBC questionnaire works to get started on each occasion), and with different observers armed with these preferences, would we get the same outcome? The answer to this question was “yes”; the ACBC method produced the same outcome for all researchers independently, which matched the set of preferred levels for the extreme preference profiles.
Data collection
Posters about the study were distributed at the reception of the rheumatology and orthopedics clinics. Two full-time research associates collected the data in the clinics during the period from January until June 2022. Patients who showed interest in participating in the study were directly assisted by the researchers. An information sheet explaining the aim of the study and a consent form was given to each participant. All participants were allowed to raise any inquiries or concerns related to the study with the researchers. The recruited participants were accompanied to a private room to ensure information privacy and patients’ comfort. Touch screen Microsoft pads were provided to the participants to complete the ACBC questionnaire. Participants were given the opportunity to complete the questionnaire independently or be assisted by the researchers during the waiting time for their clinic visit.
Data analysis
SPSS (version 22.0) was used to analyze the descriptive statistics. The categorical variables were presented in frequencies and percentages while the mean and the standard deviation (SD) were used for continuous variables. The lighthouse studio built-in Hierarchical Bayesian (HB) analysis was used to estimate the relative importance of the attributes and the part-worth (utilities) of the levels. Utilities are estimated through the maximum likelihood of each level [43, 44]. The ACBC HB estimate individual-level utility coefficients and aggregate preference distribution with individual choices by repeating the estimation and borrowing estimates of population-level means and covariance [41, 45,46,47,48]. This estimation assumes that respondents answer using an additive process consistent with the multinomial logit rule [43, 44, 49]. The level with the highest utility is the most favourable. The actual utility value given to each level is arbitrarily assigned and the levels’ utilities in each attribute are summed to zero. Therefore, the utility numbers represent the order of the levels and do not have a specific quantitative interpretation. Furthermore, the utility value of one level cannot be compared with the value of another level in another attribute because the ACBC utilities are measured on an interval, rather than a ratio, scale. Therefore, the Z score was used to standardize utility values across all attributes. The relative importance of the attributes is ratio-scaled and relative. The sums of the relative importance of all attributes add up to 100%. A higher relative importance represents a greater impact on patient’s preferences.
Results
Patients’ characteristics
One thousand and thirty OA patients completed the online ACBC questionnaire. Approximately 83% of the participants were females. Approximately 33% and 34% were aged 50–59 and 60–69 years, respectively, and only 0.6% were 20–29 years old. The dominant mother tongue language was Arabic (98.7%) since the majority of the study participants originated from UAE (89.5%). The majority of the participants (75.4%) were either uneducated (35.9%) or had school education (39.5%) and only 1% had a doctoral degree. Approximately 66% of the patients were unemployed whereas the minority were either part-time workers or students (0.6%) (See Table 1).
Patients’ OA-associated characteristics
Largely participants suffer from OA in one type of joint (63.4%) and approximately 10.4% had OA in three or more types of joints. The most affected joint by OA was the knee (83.8%) and the least affected joint was the elbow (3.6%). Most patients reported suffering from OA for less than 5 years (38%), while 26.5% of patients reported suffering from OA for more than 10 years. OA joint pain extremely affected the normal life in 28.4% of the patients, whereas 5% reported a normal life not being affected by joint pain. Most patients (53.1%) selected physiotherapy and exercise as their preferred treatment for OA, while 15.9% selected surgical intervention (See Table 2).
The relative importance of the attributes
The relative importance (RI) is measured in percentage to determine the relative contribution of different attributes for a given profile. In this case, RI is applied to assess the relative contribution of the attributes for OA treatment. The higher the value of the RI, the more important the attribute. The “Risk of kidney and liver impairment” was the most important attribute (RI = 18.54%), followed by the “Availability” (RI = 18.10%). The least important attribute was the “Way of taking medicine” (RI = 1.78%). The combined RI of the two benefits attributes (mobility improvement and pain reduction) was 6.34% and the combined RI of the four risk attributes (heart attacks and strokes, kidney and liver impairment, addiction, and gastric ulcer) was 65.91%. The highest SD of RI was 7.08 for the “Availability”, whereas the lowest SD was 1.24 for the “Way of taking the medicine” (See Fig. 1). The coefficient of variation (CV) for each attribute was obtained by calculating the ratio of the SD to the mean (represented by the relative importance). The CV provides a better understanding of the relative variability amongst the participant in favouring a particular attribute. The higher the value of CV for an attribute, the greater the variation between responses favouring this attribute. The “Way of taking the medicine” attribute had the highest variation (CV = 0.70) whereas the “Risk of addiction” attribute had the lowest variation (CV = 0.18) (See Table 3).
Utilities (part-worth) of the levels of attributes
The most preferred scenario for OA treatment for all participants combined was a prescribed medication applied topically as cream or gel, as needed, provides 75% mobility improvement and 75% pain reduction, has no risk of any of the associated side effects, and is fully covered by the insurance. The value of the interval utility for each attribute reflects how likely the participants are willing to trade-off a level against another level within the same attribute. The larger value of the utility interval indicates that participants are less likely to trade-off these levels against each other. The easiest levels to trade-off against each other are the levels with the smallest utility interval within each attribute. For example, the availability utilities for “Prescription drug”, “Over-the-counter drug” and “Internet purchase” are 135.9, -64.0, and -71.9, respectively. Therefore, moving from “Prescription drug” to “Over-the-counter drug” and “Over-the-counter drug” to “Internet purchase” would result in interval losses of 199.9 and 7.9. This indicates that it is easier for patients to trade-off over-the-counter with the internet purchase drug than trading-off prescribed medication with any other level. Moreover, the patients’ most preferred level for all risk attributes is the “No” risk. Moving from “No” to “low” toward “moderate” and then “high” risk for all risk attributes, the interval of utilities is gradually reduced. For example, the risk of addiction utility interval between (“No” and “Low”), (“Low” and “Moderate”), and (“Moderate” and “High”) are 107.1, 29.7, and 22.2, respectively. This shows that for the risk of addiction, it is easier for patients to trade-off “High” with “Moderate” risk (utility interval 22.2) than trading off “Low” risk with “No” risk (utility interval 107.2). For the “cost” attribute, a drug “fully covered by the insurance” is the most preferred option for the participants (utility mean 27.5). However, moving from “Fully covered” to “Partially covered” to “Not covered” drugs would result in 36.8 and 8.9 interval losses, respectively. This means that concerning the cost of the OA treatment, patients would probably accept to trade-off between a “Partially covered” and “Not covered” drug (utility mean 8.9) which is not the case if they are asked to trade-off between a “Fully covered” and a “Partially covered” drug (utility mean 36.8) (See Table 4). However, the utility scores for each level are arbitrarily given by the software. Therefore, these scores have been standardized using the z-score to have a mean of 0. Consequently, the utilities of levels across all different attributes would be comparable and potential trade-offs between levels within attributes could be identified. The most preferred level for a selected attribute is reflected through a positive utility score (see Fig. 2).
Discussion
To the best of our knowledge, this is the first application of ACBC in healthcare settings in a language other than English and the first study to elicit patients’ preferences regarding pharmaceutical treatment for OA in the Arab region.
This study recruited 1,030 OA patients suffering from OA in at least one joint. The study investigated their preferences for pharmaceutical treatment using an ACBC questionnaire involving 34 levels of 10 medication attributes. The vast majority of participants were females (83%) and over 50 years of age. This is consistent with previous studies confirming the higher prevalence of OA in females [50,51,52]. However, 83% is higher than the prevalence reported in previous literature. This may indicate that women are more engaged and interested in participating in this type of study. According to Rigby et al., female patients have a greater preference for acquiring information and understanding medications [53]. Therefore, females are usually more interested than males in physicians’ attention and listening regarding their treatment and health [54, 55]. The older age of the study population may be correlated with the increasing OA cases in patients aged 60 years and above in the Middle East [56,57,58]. The Prevalence of Rheumatic Diseases and Osteoporosis (PRO) in Dubai study reported that Emirati patients between 41–60 years of age were at increased risk for developing knee OA [59]. Furthermore, the participation of higher older females in our study might be correlated to the severity of OA. A meta-analysis regarding sex differences in OA reported that females ≥ 55 years tended to have more severe knee OA than males [52]. Most of the participants reported that joint pain is extremely affecting their normal life. Yet, participants mainly selected physiotherapy and exercise as their preferred choice of treatment and surgical interventions as the least preferred. Previous studies suggested that physiotherapy and exercise decreased pain, increased health-related quality of life, and delayed surgical interventions [60]. Therefore, this may suggest that OA patients are familiar with OA treatment options and able to make informed decisions about their preferences.
In our study, the combined four side effects attributes accounted for nearly 66% relative importance, while the combined two benefit attributes accounted for just over 6% relative importance. This is consistent with previous research in terms of the importance of side effects attributes preferences for the pharmaceutical treatment of OA [8, 26]. Patients’ preferences and adherence to medications were also seen to be affected by the presence of associated adverse events even if the available drugs were of equal benefit, especially in elderly patients. Precisely, the results of our ACBC study confirm that OA patients’ choice of medication is driven by patients’ avoidance of possible side effects and suggest that there is no difference between Arab OA patients and other ethnic groups in trading-off benefits and side effects. Interestingly, the “Way of taking medicine” attribute was associated with the highest coefficient of variation (0.70) despite its low relative importance (1.78%) compared to all other attributes. Therefore, the dispersion of participants’ preferences regarding the way of taking the medicine may be related to comorbidities, changes in cognitive, motor, and sensory functions which are highly encountered in older people [61]. This also highlights the importance of understanding patients’ preferences details and not focusing only on the most and least important attributes. Therefore, these findings support the crucial value of matching patients’ preferences to treatment recommendations [62]. For example, increased satisfaction with treatment and health-related quality of life have been encountered when patients’ preferences for treatment attributes were incorporated [63]. In turn, a mismatch between physicians’ and patients’ preferences may result in patients’ dissatisfaction, which may impact negatively on patients’ adherence to the recommended treatments [64]. However, the four side effects attributes had a closely similar coefficient of variation (ranging between 0.18 and 0.21). This indicates that OA patients are consistently prioritizing the avoidance of medications’ side effects.
Surprisingly, the “Availability” attribute accounted for 18.10% relative importance (the second most important of all ten attributes). This is much higher than previously reported in the UK by Al-Omari and colleagues (11.6–12.7%) [26], indicating that patients preferred “prescribed medication” more in the UAE than in the UK. This could be due to the addition of the “Cost” attribute in this study which may have made OA patients consider the “Availability” attribute more often, especially since the “Cost” attribute was the sixth most important after the availability and side effects. The availability and cost are interlinked, as the patients will not be able to have the cost covered by the insurance if it is not prescribed by the physician. Furthermore, the use of prescription drugs was seen to be correlated with the patients’ level of education where self-medication was more encountered in younger educated individuals rather than elderly ones [65]. This finding may be extrapolated in our study since most patients were uneducated or had received a limited education. Frequency and way of taking the medication are as important as mobility improvement and pain reduction; these four attributes combined accounted for 11.84% relative importance. Our findings endorse the importance of availability attribute alongside the side effects to patients making decisions about their OA medication options.
In practice, it has been hypothesized that improved medications’ adherence may have a greater influence on the population’s health in comparison to improvements in medical therapies [66]. Several studies in chronic conditions have also correlated poor adherence to an increased risk of hospitalization and overall costs [67]. At an individual level, assessing OA patients’ concerns about treatments, and involving them in treatment decision-making may improve medication adherence and effectiveness [40]. Therefore, improving the understanding of patients’ preferences for OA treatment is of great importance [68]. This explains the necessity of patients’ preferences about treatments to make final treatment decisions [69]. The use of ACBC helps in determining patients’ preferences, allowing healthcare professionals to better understand individual patients’ needs and tailor treatment plans accordingly. This may be particularly significant in Arab countries such as UAE, which have sufficient resources to provide a clinical care model similar to the Western countries [70].
Despite its strengths, this study has some limitations. Anticipating that ACBC is potentially a complicated task for some participants with a limited educational level and computer literacy, the participants were supported by the research associates while completing the ACBC questionnaire. The results may differ if the ACBC questionnaire was completed by the participants without support, as the presence of the researcher may have encouraged participants to complete the task. Despite the large number of recruited participants, our study was conducted in a single healthcare centre, which may limit the generalizability of the findings. Another limitation is that the data related to the associative correlation between patients’ comorbidities other than OA and patients’ preferences to take or avoid was not collected. Therefore, some of the patient’s preferences may not be entirely related to OA. Futuristic studies are needed to clarify the directions of these associations. However, the ACBC questionnaire focused on treatment related to joint pain caused by OA. Moreover, the number of patients approached and those who rejected to participate could not be established. Therefore, we were not able to evaluate the response rate.
Conclusion
This study marks a significant step forward in the application of an Arabic version of the ACBC questionnaire as a preference-based research method involving patients in healthcare decision-making in the UAE. Arab OA patients are similar to other ethnic groups in trading-off benefits and side effects and consistently prioritizing the avoidance of medications’ side effects. Although the “Way of taking medicine” was the least important attribute it was associated with the highest variation amongst patients. OA patients also prefer prescribed medications to internet-purchased and over-the-counter options.
Availability of data and materials
The datasets generated and/or analysed during the current study are not publicly available due to further ongoing structured research projects. However, data are available from the corresponding author on reasonable request.
Abbreviations
- ACBC:
-
Adaptive Choice-Based Conjoint
- BWS:
-
Best-Worst Scaling
- CV:
-
Coefficient of Variation
- CA:
-
Conjoint analysis
- DCEs:
-
Discrete Choice Experiments
- HB:
-
Hierarchical Bayesian
- OA:
-
Osteoarthritis
- PPI:
-
Patient and Public Involvement
- RI:
-
Relative Importance
- SD:
-
Standard Deviation
- UAE:
-
United Arab Emirates
- UK:
-
United Kingdom
- US:
-
United States
References
Leifer VP, Katz JN, Losina E. The burden of OA-health services and economics. Osteoarthritis Cartilage. 2022;30(1):10–6.
Mahendira L, Jones C, Papachristos A, Waddell J, Rubin L. Comparative clinical and cost analysis between surgical and non-surgical intervention for knee osteoarthritis. Int Orthop. 2020;44(1):77–83.
Thysen S, Luyten FP, Lories RJU. Targets, models and challenges in osteoarthritis research. Dis Model Mech. 2015;8(1):17–30.
Hermann W, Lambova S, Muller-Ladner U. Current treatment options for osteoarthritis. Curr Rheumatol Rev. 2018;14(2):108–16.
Al-Saleh JA, Albelooshi AA, Salti AA, Farghaly M, Ghorab AM, Linga S, et al. Burden, treatment patterns and unmet needs of osteoarthritis in Dubai: a retrospective analysis of the Dubai Real-World Claims Database. Rheumatol Ther. 2022;9(1):151–74.
Cross M, Smith E, Hoy D, Nolte S, Ackerman I, Fransen M, et al. The global burden of hip and knee osteoarthritis: estimates from the Global Burden of Disease 2010 study. Ann Rheum Dis. 2014;73(7):1323–30.
People-centred health care: a policy framework. WHO Regional Office for the Western Pacific; 2007. https://www.who.int/publications-detail-redirect/9789290613176. Accessed 11 July 2023.
Hiligsmann M, Pinto D, Dennison E, Al-Daghri N, Beaudart C, Branco J, Bruyère O, et al. Patients’ preferences for osteoarthritis treatment: the value of stated-preference studies. Aging Clin Exp Res. 2019;31(1):1–3.
Brennan PF, Strombom I. Improving health care by understanding patient preferences: the role of computer technology. J Am Med Inform Assoc. 1998;5(3):257–62.
Vennedey V, Derman SH, Hiligsmann M, Civello D, Schwalm A, Seidl A, et al. Patients’ preferences in periodontal disease treatment elicited alongside an IQWiG benefit assessment: a feasibility study. Patient Prefer Adherence. 2018;12:2437–47.
Hollin IL, Peay HL, Apkon SD, Bridges JFP. Patient-centered benefit-risk assessment in duchenne muscular dystrophy. Muscle Nerve. 2017;55(5):626–34.
van Overbeeke E, Janssens R, Whichello C, SchölinBywall K, Sharpe J, Nikolenko N, et al. Design, conduct, and use of patient preference studies in the medical product life cycle: a multi-method study. Front Pharmacol. 2019;3(10):1395.
Eapen V, Ghubash R. Help-seeking for mental health problems of children: preferences and attitudes in the United Arab Emirates. Psychol Rep. 2004;94(2):663–7.
Hajat C, Harrison O, Shather Z. A profile and approach to chronic disease in Abu Dhabi. Global Health. 2012;8(1):18.
Obeidat R. Decision-making preferences of Jordanian women diagnosed with breast cancer. Support Care Cancer. 2015;23(8):2281–5.
van den Muijsenbergh ME, Lagro-Janssen TA. Urinary incontinence in Moroccan and Turkish women: a qualitative study on impact and preferences for treatment. Br J Gen Pract. 2006;56(533):945–9.
Chachoua L, Dabbous M, François C, Dussart C, Aballéa S, Toumi M. Use of patient preference information in benefit-risk assessment, health technology assessment, and pricing and reimbursement decisions: a systematic literature review of attempts and initiatives. Front Med (Lausanne). 2020;26(7):543046.
Alzubaidi H, Hussein A, Namara KM, Scholl I. Psychometric properties of the Arabic version of the 9-item Shared Decision-Making Questionnaire: the entire process from translation to validation. BMJ Open. 2019;9(4):e026672.
AlHaqwi AI, AlDrees TM, AlRumayyan A, AlFarhan AI, Alotaibi SS, AlKhashan HI, et al. Shared clinical decision making: a Saudi Arabian perspective. SMJ. 2015;36(12):1472–6.
Alzubaidi H, Samorinha C, Saidawi W, Hussein A, Saddik B, Scholl I. Preference for shared decision-making among Arabic-speaking people with chronic diseases: a cross-sectional study. BMJ Open. 2022;12(4):e058084.
Paulo MS, Loney T, Lapão LV. The primary health care in the emirate of Abu Dhabi: are they aligned with the chronic care model elements? BMC Health Serv Res. 2017;17(1):725.
Alameddine M, AlGurg R, Otaki F, Alsheikh-Ali AA. Physicians’ perspective on shared decision-making in Dubai: a cross-sectional study. Hum Resour Health. 2020;18(1):33.
Bodolica V, Spraggon M, Shahid A. Strategic adaptation to environmental jolts: an analysis of corporate resilience in the property development sector in Dubai. Middle East J Manag. 2018;1(5):1.
Bodolica V, Spraggon M. Toward patient-centered care and inclusive health-care governance: a review of patient empowerment in the UAE. Public Health. 2019;169:114–24.
Egbrink M oude, IJzerman M. The value of quantitative patient preferences in regulatory benefit-risk assessment. J Mark Access Health Policy. 2014;2. https://doi.org/10.3402/jmahp.v2.22761.
Al-Omari B, McMeekin P. Patients’ preferences regarding osteoarthritis medications: an adaptive choice-based conjoint analysis study. Patient Prefer Adherence. 2020;22(14):2501–15.
Cunningham CE, Deal K, Chen Y. Adaptive choice-based conjoint analysis. Patient. 2010;3(4):257–73.
Eggers F, Sattler H. Preference measurement with conjoint analysis. Overview of state-of-the-art approaches and recent developments. NIM Mark Intell Rev. 2011;3(1):36–47.
Brand BM, Baier D. Adaptive CBC: are the benefits justifying its additional efforts compared to CBC? 2020.
Orme BK. Fine-tuning CBC and adaptive CBC questionnaires. Sequim: Sawtooth Software; 2009. https://sawtoothsoftware.com/resources/technical-papers/fine-tuning-cbc-and-adaptive-cbc-questionnaires. Accessed 2009.
Webb EJD, Meads D, Eskyte I, King N, Dracup N, Chataway J, et al. A systematic review of discrete-choice experiments and conjoint analysis studies in people with multiple sclerosis. Patient. 2018;11(4):391–402.
Yu J, Goos P, Vandebroek M. Individually adapted sequential Bayesian conjoint-choice designs in the presence of consumer heterogeneity. Int J Res Mark. 2011;28(4):378–88.
Jervis SM, Ennis JM, Drake MA. A comparison of adaptive choice-based conjoint and choice-based conjoint to determine key choice attributes of sour cream with limited sample size. J Sens Stud. 2012;27(6):451–62.
Krumholz HM. Informed consent to promote patient-centered care. JAMA. 2010;303(12):1190–1.
Al-Omari B. Patient preferences for the pharmacological treatment of osteoarthritis using adaptive choice-based conjoint (ACBC) analysis: a pilot study. Eur J Pers Cent Healthc. 2017;5(2):220–4.
Al-Omari B, Sim J, Croft P, Frisher M. Generating individual patient preferences for the treatment of osteoarthritis using Adaptive Choice-Based Conjoint (ACBC) analysis. Rheumatol Ther. 2017;4(1):167–82.
Al-Omari B, Farhat J, Shraim M. The role of web-based adaptive choice-based conjoint analysis technology in eliciting patients’ preferences for osteoarthritis treatment. Int J Environ Res Public Health. 2023;14(20):3364.
Ratcliffe J, Buxton M, McGarry T, Sheldon R, Chancellor J. Patients’ preferences for characteristics associated with treatments for osteoarthritis. Rheumatology. 2004;43(3):337–45.
de Bekker-Grob EW, Donkers B, Jonker MF, Stolk EA. Sample size requirements for discrete-choice experiments in healthcare: a practical guide. Patient. 2015;8(5):373–84.
Al-Omari B, McMeekin P, Bate A. Systematic review of studies using conjoint analysis techniques to investigate patients’ preferences regarding osteoarthritis treatment. Patient Prefer Adherence. 2021;3(15):197–211.
Orme BK. Getting Started with Conjoint Analysis: Strategies for Product Design and Pricing Research. 1st ed. New York: Research Publishers, LLC; 2006.
Al-Omari B, Sim J, Croft P, Frisher M. Patient preferences for the pharmacological treatment of osteoarthritis: a feasibility study using adaptive choice-based conjoint analysis (ACBCA). Eur J Pers Cent Healthc. 2015;3(2):253–60.
The Adaptive Choice-Based Conjoint (ACBC). Utah: Sawtooth Software; 2014. https://sawtoothsoftware.com/resources/technical-papers/acbc-technical-paper. Accessed Feb 2014.
Chapman C, Alford J, Johnson C, Weidemann R, Lahav M. CBC vs. ACBC: comparing results with real product selection. Sequim: Sawtooth Software Conference Proceedings; 2009. https://sawtoothsoftware.com/resources/technical-papers/cbc-vs-acbc-comparing-results-with-real-product-selection. Accessed 1 Jan 2009.
Louviere JJ, Street D, Burgess L, Wasi N, Islam T, Marley AAJ. Modeling the choices of individual decision-makers by combining efficient choice experiment designs with extra preference information. J Choice Model. 2008;1(1):128–64.
Toubia O, Hauser JR, Simester DI. Polyhedral methods for adaptive choice-based conjoint analysis. J Mark Res. 2004;41(1):116–31.
Allenby G, Fennell G, Huber J, Eagle T, Gilbride T, Horsky D, et al. Adjusting choice models to better predict market behavior. Market Lett. 2005;16(3):197–208.
Johnson RM, Orme BK. A new approach to adaptive CBC. In: Sawtooth software conference. 2007. p. 85.
Glossary of Terms, Sawtooth software. 2023. https://sawtoothsoftware.com/resources/knowledge-base/general-issues/glossary-of-terms. Accessed 10 July 2023.
Plotnikoff R, Karunamuni N, Lytvyak E, Penfold C, Schopflocher D, Imayama I, et al. Osteoarthritis prevalence and modifiable factors: a population study. BMC Public Health. 2015;15(1):1195.
Blagojevic M, Jinks C, Jeffery A, Jordan KP. Risk factors for onset of osteoarthritis of the knee in older adults: a systematic review and meta-analysis. Osteoarthritis Cartilage. 2010;18(1):24–33.
Srikanth VK, Fryer JL, Zhai G, Winzenberg TM, Hosmer D, Jones G. A meta-analysis of sex differences prevalence, incidence and severity of osteoarthritis. Osteoarthritis Cartilage. 2005;13(9):769–81.
Rigby D, Vass C, Payne K. Opening the “Black Box”: an overview of methods to investigate the decision-making process in choice-based surveys. Patient. 2020;13(1):31–41.
Alraddadi KS, Al-Adwani F, Taher ZA, Al-Mansour M, Khan M. Factors influencing patients’ preferences for their treating physician. Saudi Med J. 2020;41(8):866–73.
Erdem S, Thompson C. Prioritising health service innovation investments using public preferences: a discrete choice experiment. BMC Health Serv Res. 2014;28(14):360.
Naeem SM, Jahan F, Siddiqui MA, Khan MM. Pattern of morbidity among elders attending general practice: health needs assessment of geriatric patients in Oman. Geriatric Care. 2018. https://doi.org/10.4081/gc.2018.7774.
Ahmed A, Rigi A, Kokash FE, Samad OA, Shaikh RB. Arthritis among Patients Attending GMC Hospital, Ajman, UAE: A cross sectional survey. Gulf Medical University: Proceedings. 2014;5(6):52–9.
Al-Modeer MA, Hassanien NS, Jabloun CM. Profile of morbidity among elderly at home health care service in Southern Saudi Arabia. J Family Community Med. 2013;20(1):53–7.
Al Saleh J, Sayed ME, Monsef N, Darwish E. The prevalence and the determinants of musculoskeletal diseases in Emiratis attending primary health care clinics in Dubai. Oman Med J. 2016;31(2):117–23.
Jönsson T, Ekvall Hansson E, Thorstensson CA, Eek F, Bergman P, Dahlberg LE. The effect of education and supervised exercise on physical activity, pain, quality of life and self-efficacy - an intervention study with a reference group. BMC Musculoskelet Disord. 2018;19(1):198.
Chait MM. Gastroesophageal reflux disease: Important considerations for the older patients. World J Gastrointest Endosc. 2010;2(12):388–96.
Robinson JH, Callister LC, Berry JA, Dearing KA. Patient-centered care and adherence: definitions and applications to improve outcomes. J Am Acad Nurse Pract. 2008;20(12):600–7.
Lecluse LLA, TuteinNolthenius JLE, Bos JD, Spuls PI. Patient preferences and satisfaction with systemic therapies for psoriasis: an area to be explored. Br J Dermatol. 2009;160(6):1340–3.
Vogel BA, Helmes AW, Hasenburg A. Concordance between patients’ desired and actual decision-making roles in breast cancer care. Psychooncology. 2008;17(2):182–9.
Ansari M, Alanazi A, Moin A. Consumers’ awareness, attitude and associated factors towards self-medication in Hail, Saudi Arabia. Bourgeois D, editor. PLoS One. 2020;15(4):e0232322.
Haynes RB, McDonald H, Garg AX, Montague P. Interventions for helping patients to follow prescriptions for medications. Cochrane Database Syst Rev. 2002;(2):CD000011. https://doi.org/10.1002/14651858.CD000011.
Boye KS, Curtis SE, Lage MJ, Garcia-Perez LE. Associations between adherence and outcomes among older, type 2 diabetes patients: evidence from a Medicare Supplemental database. PPA. 2016;16(10):1573–81.
Nicolson PJA, Holden MA. Patient Preferences and Osteoarthritis Care: What Do We Know About What Patients Want from Osteoarthritis Treatment? Curr Treat Options in Rheum. 2023;9:120–31.
Rivero-Santana A, Perestelo-Perez L, Perez-Ramos J, Gonzalez-Lorenzo M, Serrano-Aguilar P. Treatment Preferences in Patients with Knee or Hip Osteoarthritis: An Overview. In: Osteoarthritis - Diagnosis, Treatment and Surgery. InTech; 2012. https://doi.org/10.5772/26343.
Margolis SA. Patient satisfaction with primary health care services in the United Arab Emirates. Int J Qual Health Care. 2003;15(3):241–9.
Acknowledgements
The authors would like to thank Khalifa University of Science, Technology & Research and Healthpoint Hospital for their support of this research project. Special thanks to Ms. Mai Ershaid for contributing to the data collection and entering, and Mr. Feras Joudeh and Ms. Asmaa Al Menhali for their support in the patients’ recruitment and hospital electronic data.
Funding
This research project was funded by Khalifa University of Science and Technology (Reference number: 8474000267). The funder was not involved in the design and conduct of the study; collection, analysis, and interpretation of the data; drafting, review, or approval of the manuscript; and the decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
Conception and design: B.A. Methodology: B.A., J.F. Acquisition of data: B.A., J.F. Software: B.A., J.F. Validation: B.A., J.F. Formal analysis, B.A., and J.F.; Investigation: B.A., J.F., M.K., H.G., Z.A., S.H., A.A. Resources, B.A. Data curation, B.A., J.F. Drafting of the manuscript: B.A., J.F. Critical revision of the manuscript: B.A., J.F. M.K, H.G, Z.A., S.H., A.A. Statistical analysis: B.A., J.F. Provision of study patient: B.A., J.F. M.K, H.G, Z.A., S.H., A.A. Obtaining funding: B.A. Administrative, technical, or logistic support: B.A., J.F. Supervision: B.A. Others: All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This research was approved by the Institutional Review Board of Khalifa University of Science and Technology (Reference number: H20-023) and the Healthpoint Research Ethics Committee (Reference number: MF2467-2020-4). All data collections and analyses were anonymous and performed in accordance with the Declaration of Helsinki. Informed consent was obtained from all subjects in this study.
Consent for publication
Not applicable. This manuscript does not include any details relating to an individual person.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplemental figure 1.
An example of the first screen of the ACBC questionnaire (The first screen of the ACBC questionnaire briefly introduces the participants to the content of the questionnaire. This introductory part helps the participants to know what to expect and what kind of questions and tasks are requested from them throughout the whole ACBC questionnaire). Supplemental figure 2. An example of patients’ demographics question (age). Supplemental figure 3. An example of patients’ demographics question (gender). Supplemental figure 4. An example of patients’ demographics question (country of origin). Supplemental figure 5. An example of patients’ demographics question (native language). Supplemental figure 6. An example of patients’ demographics question (education). Supplemental figure 7. An example of patients’ demographics question (employment). Supplemental figure 8. An example of OA medical history question (duration of OA). Supplemental figure 9. An example of OA medical history question (level of pain). Supplemental figure 10. An example of OA medical history question (site of OA). Supplemental figure 11. An example of OA medical history question (preferred treatment). Supplemental figure 12. An example of OA medical history question (current treatment). Supplemental figure 13. An example of the Build Your Own (BYO) questions (In the BYO section, participants can choose their preferred treatment characteristics through the listed attributes and their levels). Supplemental figure 14. An example of the screening questions (The screening section presents multiple scenarios for participants. For each scenario, participants are asked to select if the offered treatment characteristics are a “Possibility” or “Not a possibility’ to consider). Supplemental figure 15. An example of the “must have” questions (The “Must have” questions allow participants to specify the most important characteristic that needs to be always present in their treatment scenario). Supplemental figure 16. An example of the “Unacceptable” questions (The “Unacceptable” questions allow participants to specify the least important characteristic which is not considered if present in their treatment scenario). Supplemental figure 17. An example of the choice-task questions. The choice-task questions allow participants to choose their most preferred treatment option among multiple scenarios.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Al-Omari, B., Farhat, J., Khan, M. et al. Exploring patient treatment decision making for osteoarthritis in the UAE: a cross-sectional adaptive choice-based conjoint study. BMC Public Health 23, 1542 (2023). https://doi.org/10.1186/s12889-023-16490-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-023-16490-1