Abstract
Background
National comprehensive smoke-free legislation has been found to decrease the incidence of several smoking-related diseases. In 2007, Denmark introduced a national smoking ban, which banned smoking indoor in workplaces and public places, although only partial restrictions were applied in certain settings. We examined the impact of the smoking ban on smoking-related diseases and whether this differed across socioeconomic groups.
Methods
Interrupted time series analyses of nationwide register data were performed using Poisson regression models to examine the differential impact of the smoking ban on monthly incidence rates of acute myocardial infarction, chronic obstructive pulmonary disease, and smoking-related cancers from 2002 to 2015. Immediate changes in incidence rates after the smoking ban and long-term changes in disease trends were estimated by comparing data from the pre- and post-ban period. Models were stratified by socioeconomic position.
Results
Overall, we found neither immediate changes in rates of acute myocardial infarction, chronic obstructive pulmonary disease, and smoking-related cancers following the smoking ban nor long-term post-ban changes in disease trends as compared to before the ban. Results did not differ across socioeconomic groups. A pronounced socioeconomic gradient in incidence rates was observed for all outcomes both before and after the smoking ban.
Conclusion
The national smoking ban was not associated with a lower incidence of smoking-related diseases in the post-ban period compared to pre-ban levels and no differences between socioeconomic groups were observed. Future tobacco control in Denmark should consider which measures most effectively target the low socioeconomic groups to decrease the current strong socioeconomic inequality in health.
Similar content being viewed by others
Background
Smoking is the single most important preventable cause of morbidity and premature mortality worldwide and is one of the most substantial global public health concerns [1]. Guided by international evidence of the negative health impacts of smoking and second-hand smoke (SHS) exposure, many countries have introduced national legislation to discourage smoking initiation, increase smoking cessation, and reduce SHS exposure [2, 3].
An important approach is the enactment of national smoking bans that restrict smoking in designated areas, including workplaces and public settings. The evidence is strong that comprehensive smoking bans are high-impact public health policies leading to reductions in adverse health outcomes in the general population [4, 5]. Previous studies in this field have mainly examined post-ban effects at population level [4, 6]. As any health benefits following a smoking ban may not be equivalent across population subgroups that differ in risk, incidence and burden of smoking-related morbidity, attention must also be given to the potential differential effect of smoking bans to prevent a widening of existing health disparities [6,7,8].
In most developed countries, smoking prevalence are particularly high in socioeconomic disadvantaged groups contributing to poorer health and higher mortality among those with lower socioeconomic position [9]. This manifests itself in a marked socioeconomic gradient in life expectancy [9, 10]. In Denmark, smoking displays large disparities and is strongly associated with lower socioeconomic position [11]. Further, smoking is one of the leading factors responsible for the socioeconomic inequality in health in the Danish population and smoking and alcohol have been identified as the main explanations for an increase in inequality in mortality observed from 1985 to 2009 [11, 12]. Although the smoking prevalence in the general population has decreased since 1970 to 19% in 2022, this has occurred at a slower pace among the lowest educated, thus increasing inequalities in smoking [13, 14]. In 2022, 22% of people with a primary school as the highest educational level were smoking daily in Denmark compared to only 8% among those with an advanced education [15]. This calls for tobacco control measures that strive to be effective in all socioeconomic groups.
In 2007, a national smoking ban was implemented prohibiting indoor smoking in public settings and workplaces. The ban was the most extensive tobacco control policy implemented at national level in Denmark at the time; however, several exemptions were made, resulting in only a partial coverage in specific premises such as small bars, one-man offices, and commercial vehicles [16]. The primary aim of the smoking ban was to protect non-smokers from the harmful effect of SHS exposure. Additionally, a reduction in population smoking prevalence and smoking intensity was anticipated.
While most previous studies have been examining the potential contribution of smoking bans to reduce socioeconomic inequalities in smoking behavior such as prevalence, cessation rates, and smoking intensity [1, 6, 17,18,19], less attention has been directed towards the differential impact on health outcomes. Existing research indicates greater post-ban reductions in mortality and hospital admissions for acute coronary events and chronic obstructive pulmonary disease (COPD) in socioeconomic disadvantaged groups [7], and in more deprived areas [20,21,22] compared with their socioeconomic counterparts. However, the evidence is limited, and findings are inconclusive. In this study we investigate whether the incidence of acute myocardial infarction (AMI), COPD, and smoking-related cancers differed across socioeconomic groups after the implementation of the Danish national smoking ban in 2007 compared to pre-ban levels.
Methods
This study is based on data from nationwide population-based registers. Separately for each outcome, a study population consisting of the entire Danish adult population (30 + years) from 2000 to 2015 was linked with individual outcome records from the Danish National Patient Register, which collects admission records from Danish hospitals since 1977 as well as outpatient and emergency room contacts since 1995 [23]. As we examined smoking-related diseases predominantly occurring in the adult population, the study population was restricted to include individuals over 30 years of age. Incident cases of disease occurring during the study period (primary or secondary diagnosis) were identified, and pre-hospital deaths were accounted for by retrieving cause-specific mortality data from the Danish Register of Causes of Death (underlying or contributory cause of death) [24]. Diagnoses were classified according to the International Classification of Disease, tenth revision (ICD10) (ICD8: 1977–1993). Through the Civil Registration System, we obtained information on sex and age [25]. Data was obtained at individual level and linked within and across years through the unique personal identification number (CPR), which residents in Denmark are legally required to be assigned at birth or immigration [25]. A study population were defined for each outcome separately and included individuals without a preceding diagnosis of the outcome in question, who were Danish residents 1 January 2002, at their 30 years birthday, or at immigration, whichever came last. Disease event, death of any cause, emigration, disappearance, or end of the study period whichever came first marked the end of follow up. Individuals were continuously included in the study population during the study period if they were eligible for inclusion. No re-entry was allowed. The study population was divided in age- and calendar-specific strata and subsequently aggregated in pre-defined age (1-year intervals), sex, calendar (monthly level), and socioeconomic groups.
Socioeconomic position
We included the highest achieved educational level measured in months as an indicator of socioeconomic position by retrieving information from the Population Education Register (PER), which contains annual individual-based information about all individuals attending an education in Denmark [26]. Educational level was grouped in three: low educational level, i.e., no education and primary school (≤ 9 years), medium educational level, i.e., high school or vocational school (10–12 years), and high educational level, which included university and other forms advanced education (≥ 13 years). Individuals with missing information were excluded from the analyses (corresponding to 4.6% of the AMI study population; 4.4% of the COPD study population, and 4.3% of the cancer study population).
Outcome
As most smoking-related morbidity arise from cardiovascular diseases (primarily AMI and stroke), respiratory diseases (primarily COPD), and cancers, three outcomes were included in the analyses: AMI (ICD8: 410; ICD10: I21) [27, 28], COPD (ICD8: 491–492; ICD10: J44) [29, 30], and smoking-related cancers defined as the first occurring diagnosis of cancer in bronchus and lung (ICD8: 162.1; ICD10: C34, D022), cancer in lip, mouth, oral cavity, and pharynx (ICD8: 140–149; ICD10: C00-C14, D000), and bladder cancer (ICD8: 188; ICD10: C67, D090). Analyses were conducted separately for each outcome.
Design
We used an interrupted time series design to quantify the immediate and long-term differential impact of the Danish smoking ban across socioeconomic groups. The time periods were centered around the time of enactment of the smoking ban on the 15 August 2007, thus defining a pre- and post-ban period to be compared. The immediate impact was expressed as changes in incidence rates occurring at the time the smoking ban was implemented, whereas changes in the slope of the disease trend in the post-ban period compared with pre-ban trends determined any long-term effects of the smoking ban [31, 32]. For all outcomes we applied a pre-ban period from 1 January 2002 to 31 August 2007. However, distinct post-ban periods were defined for each outcome due to different expectations of the lag between the time of implementation of the smoking ban and subsequent effects on incidence rates, caused by differences in latency periods between diseases. For AMI and COPD, immediate and fast-acting harmful pathological changes caused by smoking or SHS exposure have been observed even at low exposure levels and the risk for cardiovascular diseases has been suggested to decrease within a few years after the elimination of exposure [33,34,35,36,37]. In addition, previous studies have found declining admission rates in the general population within few years after the implementation of smoke-free regulations for both outcomes [30, 38]. Consequently, we included a post-ban period of 3.3. years for AMI (end of follow- up 31 December 2010) and 5.3 years for COPD (end of follow-up 31 December 2012). We acknowledge, that the long latency period for smoking-related cancers, which involve a complex process with a slow progression of disease, makes it more difficult to study causation between the implementation of the smoking ban and subsequent changes in incidence rates. However, due to the strong causal link between active smoking or SHS exposure and risk of cancer, we argue for the importance of examining cancer rates over time. Thus, for smoking-related cancers we included the longest possible follow-up period at the time of study (8.3-years) (end of follow up 31 December 2015).
Statistical analyses
Descriptive characteristics of the study population stratified by sex, time-period, and educational level were calculated. For each educational level we estimated age- and sex-standardized incidence rates every three months of AMI, COPD, and smoking-related cancers (European population as standard).
To examine changes in incidence rates after the smoking ban across socioeconomic groups, Poisson regression models stratified by educational level were conducted for each outcome separately. As offset, a logarithmic transformation of the follow-up time was applied. Models were fitted to estimate three parameters of interest: the underlying secular disease trend assuming to continue unaffected in absence of the smoking ban; the level change occurring in the month after the smoking ban was introduced (September 2007), expressing the immediate impact of the ban; and the post-ban change in the disease trend, estimating any long-term impact of the smoking ban when compared to pre-ban trends. Models were adjusted for age, sex, and seasonal variations, which was constrained to be the same each year and based on calendar month. The final Poisson models were defined as:
where Y expresses the monthly incidence rate, β0 is the log-incidence rate at baseline for the outcome in question, β1, is the disease trend in the pre-ban period (continuous, linear predictor for time); β2, is the immediate level change in the rate following the implementation of the smoking ban (binary indicator variable with a value of zero in the pre-ban months and a value of 1 in the post-ban period), and β3, is the change in disease trend in the post-ban period compared to the pre-ban trend (interaction term between the linear predictor for time and the binary indicator). βx denotes the effects of the covariates.
Coefficients were exponentiated to derive incidence rate ratios (IRR) for presentation of results, and trend estimates were calculated as changes in rates every third year. Further, to examine changes in the socioeconomic gradient in incidence of AMI, COPD, and smoking related cancers pre- and post-ban, Poisson regression models accounting for the underlying secular trend, sex, age, and seasonality were performed. To account for overdispersion we applied a scale parameter in all models that allowed the variance to be bigger than the mean. Analyses were performed in SAS software (version 9.4) and figures were created in STATA (version 15.1).
Results
In both the low, medium, and high educational group, lower incidence rates of AMI were observed in the post-ban period compared to the pre-ban period for both men and women (Table 1). For COPD, lower post-ban rates, compared to pre-ban, were only observed among men with a medium educational level (pre-ban IR: 457.1, post-ban IR: 451.3) and women with a high educational level (pre-ban IR: 236.9, post-ban IR: 235.3), and for smoking-related cancers among men with a medium (pre-ban IR: 296.1, post-ban IR: 285.0) or high educational level (pre-ban IR: 218.3, post-ban IR: 196.9).
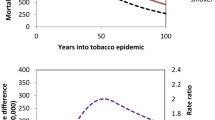
Declining age- and sex-standardized incidence rates for AMI were observed during the whole study period in the low, medium, and high educational group (Fig. 1). Incidence rates for COPD and smoking-related cancers appeared approximately constant in all educational groups during the study period. A socioeconomic gradient was observed for all outcomes during the whole study period with persistent higher incidence rates among the lowest educated group. Additionally, the difference between the socioeconomic groups appeared to be constant in the pre- and post-ban period for all outcomes. Seasonal variations were observed for AMI and COPD.
No consistent post-ban changes in the disease trend were found for AMI, COPD, and smoking-related cancers across educational groups (Table 2). For AMI, estimates indicated that the disease trend every third year declined to a slightly lesser extent following the implementation of the smoking ban among individuals with low (IRR: 1.03; 95% CI: 1.01–1.04) and medium educational level (IRR: 1.03; 95% CI: 1.02–1.05). Similarly, the COPD trend appeared to decline less steeply in the post-ban period among those with a low educational level (IRR: 1.02; 95% CI: 1.01–1.02). However, estimates and absolute differences were very small.
An immediate ten percent increase in incidence of COPD following the smoking ban was found among those with high educational level (IRR: 1.10; 95% CI: 1.03–1.17) (Table 2). Further, immediate increases of smoking-related cancers were observed in the medium (IRR: 1.06; 95% CI: 1.02–1.11) and high educational group (IRR: 1.09; 95% CI: 1.02–1.17). No immediate post-ban changes in rates were found for AMI.
Clear socioeconomic gradients in incidence of AMI, COPD, and smoking-related cancers were observed in both the pre- and post-ban period (Table 3). In the pre-ban period, the incidence rate of AMI was 72% higher among the low educated compared to those with high educational levels (IRR: 1.72, 95%CI: 1.67–1.77). Similar socioeconomic gradients were observed for COPD (2.45, 95%CI: 2.39–2.52) and smoking-related cancers (1.74, 95%CI: 1.68–1.80). The incidence rate ratios did not change in the post-ban period for any outcomes.
Discussion
In this nationwide study including the entire Danish adult population, no differential impact of the Danish national smoking ban from 2007 on incidence of AMI, COPD, and smoking-related cancers was found across socioeconomic groups. Neither immediate changes in incidence rates nor long-term changes in the disease trend were observed for any outcomes in the years after the smoking ban compared to pre-ban levels. The social gradient observed in the pre-ban period continued at the same level post-ban.
Overall, previous studies examining the contribution of smoking bans to reduce socioeconomic inequalities have primarily focused on post-ban changes in smoking behavior, such as smoking prevalence, SHS exposure, and cessation rates [6, 17, 39, 40]. Two systematic reviews found insufficient evidence that restrictions in workplaces and public places are more effective in reducing smoking in higher socioeconomic groups [6, 17]. Hill et al. found higher workplace SHS exposure among socioeconomic disadvantaged groups, but no clear evidence of how smoking restrictions affect this gradient since studies have failed to demonstrate differential effects [6]. In addition, no educational differences in successful smoking cessation were observed after a smoking ban in the hospitality industry in the Netherlands [40]. Lastly, Federico et al. suggested that the immediate 1.6% decrease in smoking prevalence and 4.5% increase in smoking cessation following the Italian smoking ban, which was observed only among low educated women, subsequently reversed over time [41].
Previous studies examining the differential impact of smoking bans on smoking-related morbidity are limited. Contrary to the present findings, a study examining COPD admissions following two succeeding smoking bans in Spain suggested greater declines of COPD in provinces with lower levels of socioeconomic development [21]. Further, Cesaroni et al. observed reductions in acute coronary events in the population of Rome after smoking was banned in all public places, with the largest reduction among those living in low socioeconomic census blocks [22]. Socioeconomic differences were also found in mortality of ischemic heart disease and COPD following the national Irish smoking ban, where health benefits were concentrated among the most disadvantaged groups [7].
We did not find any differential effects across socioeconomic groups, which might be explained by differences between countries in standards of living, available health care systems as well as population smoking rates. Another explanation may be that the Danish smoking ban was considerably less comprehensive than those implemented in other countries [16, 42]. Previous studies have shown that comprehensive smoking bans are more effective in reducing several adverse health outcomes such as AMI, COPD, and lung cancer compared to partial bans [29, 43, 44]. Further, comprehensive bans have been found to enhance public support and compliance with regulations and are associated with more quit-attempts and subsequent quit-success compared to partial bans [45, 46]. The Danish smoking ban comprised several exemptions such as allowing smoking in bars under 40m2 where no food is served, in one-man offices, in commercial vehicles, and in mental health care services [16]. This has probably influenced the lack of a measurable impact of the ban.
Two main pathways may link smoking bans to declines in disease rates, including directly reduce SHS exposure and indirectly reduce smoking prevalence by encourage quitting and prevent initiation [47]. Previous research demonstrates that comprehensive smoking bans are effective in reducing SHS exposure, while inconsistent evidence exists for smoking prevalence [4].
The smoking prevalence in Denmark has steadily decreased with approximately one percentage point each year from 2000 to 2012 where a stagnation followed [48]. Thus, no accelerated decrease in the smoking prevalence occurred in the years after the smoking ban [28, 49]. The exposure to SHS in workplaces, educational institutions, and public settings declined in the years preceding the smoking ban and continued to decrease post-ban [49]. A survey from 2009 showed that self-reported daily SHS exposure in workplaces and educational institutions decreased substantially from 27% in 2004 and 21% in 2006 to 5% in 2009 [49]. We found no changes in disease trends post-ban in any socioeconomic groups, thus the reduction in SHS exposure following the smoking ban is not reflected in our findings. Further, attributing the decrease in SHS exposure solely to the implementation of the smoking ban must be done with caution.
Smoking bans may also influence smoking behavior through a decrease in the social acceptability of smoking and changes in social norms [50,51,52]. In the years prior to the ban, public information announcing the impending changes, brought out an extensive media attention on the Danish smoking legislation, which increased the negative public awareness on smoking [28, 53]. In addition, individual-level interventions such as smoking cessation programs or voluntary workplace regulations were introduced throughout Denmark in these years. Two years before the enactment, 35% had introduced local smoking regulations totally banning indoor smoking in workplaces and educational institutions [49]. This increased to 48% in 2006 and 67% in 2007. Thus, a considerable part of the Danish population was already covered by local smoking restrictions at the time of the national smoking ban. The influence of these contextual factors associated with the smoking ban may have limited the direct measurable impact of the ban.
Limitations of this study include the expected time from onset of the smoking ban to manifestation of disease, which vary between diseases and in people with different magnitudes of risk. Especially, the latency period for smoking-related cancers is quite extensive. Thus, the results related to smoking-related cancers are considered preliminary. Including a longer follow-up period could have considered the possible slow responsiveness to behavioral changes among smokers caused by smoking addiction. However, increasing the period for each outcome would induce uncertainties about whether any changes in disease rates could be linked to the implementation of the smoking ban. We do not believe that a increasing the length of the post-ban period would change the findings.
This study has several strengths. First, the study is based on high quality data from nationwide registers, which enabled the inclusion of a large sample size providing great statistical power to the analyses. Combined with the detailed individual-level linkage between registers, we were able to detect even small variations in disease trends. The linkage to the RCD allowed us to include acute fatal events outside hospital, which provided a more complete measure of disease incidence. As the registers are continuously updated, thus providing many data points over time, the pre-ban trend was estimated with precision, and long follow up periods were applied. Further, because all residents in Denmark are entitled to publicly financed healthcare and we included the whole Danish adult population, the risk of selection bias was eliminated. In the analysis, we accounted for seasonality and the underlying secular disease trend which strengthened the findings.
We defined socioeconomic position as the individual highest achieved education. Research suggests that education represents a valid indicator of socioeconomic position as it often determines future employment and income and is relatively stable over an adult life span [54, 55]. Through the PER we were able to quantify the measurement comparatively accurate.
Overall, national health targets stand little chance of being reached without specific attention to the health of the socioeconomic disadvantaged groups [10]. Tobacco control policies may have considerable potential to reduce smoking inequalities, especially those targeting pricing on tobacco products, tobacco advertising, and subsidized smoking cessation services [18]. Preferably, implementing multiple policies as a part of a comprehensive tobacco control approach could be prioritized as initiatives individually may affect different sociodemographic groups. Understanding these nuances is important for creating more robust tobacco control policies beneficial for all population subgroups.
Conclusion
We found no evidence of a differential impact of the national smoking ban from 2007 on three smoking-related diseases in the Danish adult population. Neither immediate nor long-term changes in incidence of any outcome were observed post-ban compared to pre-ban levels across socioeconomic groups. Future tobacco control measures in Denmark should consider which measures most effectively targets low socioeconomic groups to decrease the current strong socioeconomic inequality in health.
Availability of data and materials
Data used in this study are available upon request to Statistics Denmark.
Abbreviations
- SHS:
-
Second-hand smoke
- COPD:
-
Chronic obstructive pulmonary disease
- AMI:
-
Acute myocardial infarction
- ICD:
-
International Classification of Disease
- PER:
-
Population Education Register
References
Brown T, Platt S, Amos A. Equity impact of population-level interventions and policies to reduce smoking in adults: a systematic review. Drug Alcohol Depend. 2014;138:7–16.
Catalano MA, Gilleskie DB. Impacts of local public smoking bans on smoking behaviors and tobacco smoke exposure. Health Econ. 2021;30(8):1719–44.
Feliu A, Filippidis FT, Joossens L, Amalia B, Tigova O, Martínez C, et al. The association between tobacco control policy implementation and country-level socioeconomic factors in 31 European countries. Sci Rep. 2021;11(1):8912.
Frazer K, Callinan JE, McHugh J, van Baarsel S, Clarke A, Doherty K, et al. Legislative smoking bans for reducing harms from secondhand smoke exposure, smoking prevalence and tobacco consumption. The Cochrane database of systematic reviews. 2016;2:CD005992.
Hoffman SJ, Tan C. Overview of systematic reviews on the health-related effects of government tobacco control policies. BMC Public Health. 2015;15:744.
Hill S, Amos A, Clifford D, Platt S. Impact of tobacco control interventions on socioeconomic inequalities in smoking: review of the evidence. Tob Control. 2014;23(e2):e89-97.
Stallings-Smith S, Goodman P, Kabir Z, Clancy L, Zeka A. Socioeconomic differentials in the immediate mortality effects of the national Irish smoking ban. PLoS ONE. 2014;9(6): e98617.
Fagan P, King G, Lawrence D, Petrucci SA, Robinson RG, Banks D, et al. Eliminating tobacco-related health disparities: directions for future research. Am J Public Health. 2004;94(2):211–7.
Hiscock R, Bauld L, Amos A, Fidler JA, Munafò M. Socioeconomic status and smoking: a review. Ann N Y Acad Sci. 2012;1248:107–23.
Whitehead M, Dahlgren G. Concepts and principles for tackling social inequities in health: Levelling up Part 1. Regional Office for Europe: World Health Organization; 2007.
Udensen CH, Skaarup C, Petersen MNS, Ersboll AK. Social inequality in health and morbidity. The development in Denmark during the period 2010–2017 [In Danish: Social Ulighed i sundhed og sygdom. Udviklingen i Danmark i perioden 2010–2017]. The National Institute of Public Health, University of Southern Denmark, for The Danish Health Authority; 2020: Copenhagen, Denmark. Available from: https://www.sst.dk/da/udgivelser/2020/social-ulighed-i-sundhed-og-sygdom.
Koch MB, Diderichsen F, Gronbaek M, Juel K. What is the association of smoking and alcohol use with the increase in social inequality in mortality in Denmark? A nationwide register-based study. BMJ Open. 2015;5(5): e006588.
Koch MB, Davidsen M, Juel K. Social inequality in health, illness and well-being 2010 and the development since 1987 [In Danish: Social ulighed i sundhed, sygelighed og trivsel 2010 og udviklingen siden 1987]. National Institute of Public Health, University of Southern Denmark; 2012: Copenhagen, Denmark. Available from: https://www.sdu.dk/da/sif/rapporter/2012/social_ulighed_i_sundhed.
Clemmensen KK, Lynge E, Clemmensen IH. Nationwide tobacco surveys and sales data in Denmark from 1920 to 2010. Dan Med J. 2012;59(6):A4448.
Jarlstrup NS, Pedersen MT, Bast LS. Smoking habits in the Danish population 2022. The National Institute of Public Health, University of Southern Denmark, for The Danish Health Authority; 2023: Copenhagen, Denmark. Available from: https://www.sst.dk/da/udgivelser/2023/danskernes-rygevaner-2022.
Ministry of the Interior and Health of Denmark. ‘The Smoke-Free Environment Act’ [In Danish: Lov om røgfri miljøer]. Regulation no. 512, 06/06/2007. Available from: https://www.retsinformation.dk/eli/lta/2007/512.
Thomas S, Fayter D, Misso K, Ogilvie D, Petticrew M, Sowden A, et al. Population tobacco control interventions and their effects on social inequalities in smoking: systematic review. Tob Control. 2008;17(4):230–7.
Giskes K, Kunst AE, Ariza C, Benach J, Borrell C, Helmert U, et al. Applying an equity lens to tobacco-control policies and their uptake in six Western-European countries. J Public Health Policy. 2007;28(2):261–80.
Schaap MM, Kunst AE, Leinsalu M, Regidor E, Ekholm O, Dzurova D, et al. Effect of nationwide tobacco control policies on smoking cessation in high and low educated groups in 18 European countries. Tob Control. 2008;17(4):248–55.
Liu A, Guzman Castillo M, Capewell S, Lucy J, O’Flaherty M. Reduction in myocardial infarction admissions in Liverpool after the smoking ban: potential socioeconomic implications for policymaking. BMJ Open. 2013;3(11): e003307.
Galan I, Simon L, Boldo E, Ortiz C, Fernandez-Cuenca R, Linares C, et al. Changes in hospitalizations for chronic respiratory diseases after two successive smoking bans in Spain. PLoS ONE. 2017;12(5): e0177979.
Cesaroni G, Forastiere F, Agabiti N, Valente P, Zuccaro P, Perucci CA. Effect of the Italian smoking ban on population rates of acute coronary events. Circulation. 2008;117(9):1183–8.
Schmidt M, Schmidt SA, Sandegaard JL, Ehrenstein V, Pedersen L, Sorensen HT. The Danish National Patient Registry: a review of content, data quality, and research potential. Clin Epidemiol. 2015;7:449–90.
Helweg-Larsen K. The Danish Register of Causes of Death. Scandinavian journal of public health. 2011;39(7 Suppl):26–9.
Pedersen CB. The Danish Civil Registration System. Scandinavian journal of public health. 2011;39(7 Suppl):22–5.
Jensen VM, Rasmussen AW. Danish Education Registers. Scandinavian journal of public health. 2011;39(7 Suppl):91–4.
Gaudreau K, Sanford CJ, Cheverie C, McClure C. The effect of a smoking ban on hospitalization rates for cardiovascular and respiratory conditions in Prince Edward Island, Canada. PLoS ONE. 2013;8(3): e56102.
Christensen TM, Moller L, Jorgensen T, Pisinger C. The impact of the Danish smoking ban on hospital admissions for acute myocardial infarction. Eur J Prev Cardiol. 2014;21(1):65–73.
Hahn EJ, Rayens MK, Adkins S, Simpson N, Frazier S, Mannino DM. Fewer Hospitalizations for Chronic Obstructive Pulmonary Disease in Communities With Smoke-Free Public Policies. Am J Public Health. 2014;104(6):1059–65.
Rando-Matos Y, Pons-Vigués M, López MJ, Córdoba R, Ballve-Moreno JL, Puigdomènech-Puig E, et al. Smokefree legislation effects on respiratory and sensory disorders: A systematic review and meta-analysis. PloS one. 2017;12(7):e0181035-e.
Wagner AK, Soumerai SB, Zhang F, Ross-Degnan D. Segmented regression analysis of interrupted time series studies in medication use research. J Clin Pharm Ther. 2002;27(4):299–309.
Bernal JL, Cummins S, Gasparrini A. Interrupted time series regression for the evaluation of public health interventions: a tutorial. Int J Epidemiol. 2017;46(1):348–55.
IARC Handbooks of Cancer Prevention, Tobacco Control, Vol. 13: Evaluating the effectiveness of smoke-free policies. 2009: Lyon, France. Available from: https://www.iarc.who.int/wp-content/uploads/2018/07/handbook13.pdf.
Barnoya J, Glantz SA. Cardiovascular effects of secondhand smoke: nearly as large as smoking. Circulation. 2005;111(20):2684–98.
Flouris AD, Koutedakis Y. Immediate and short-term consequences of secondhand smoke exposure on the respiratory system. Curr Opin Pulm Med. 2011;17(2):110–5.
Duncan MS, Freiberg MS, Greevy RA Jr, Kundu S, Vasan RS, Tindle HA. Association of Smoking Cessation With Subsequent Risk of Cardiovascular Disease. JAMA. 2019;322(7):642–50.
Bullen C. Impact of tobacco smoking and smoking cessation on cardiovascular risk and disease. Expert Rev Cardiovasc Ther. 2008;6(6):883–95.
Tan CE, Glantz SA. Association between smoke-free legislation and hospitalizations for cardiac, cerebrovascular, and respiratory diseases: a meta-analysis. Circulation. 2012;126(18):2177–83.
Main C, Thomas S, Ogilvie D, Stirk L, Petticrew M, Whitehead M, et al. Population tobacco control interventions and their effects on social inequalities in smoking: placing an equity lens on existing systematic reviews. BMC Public Health. 2008;8:178.
Nagelhout GE, Crone MR, van den Putte B, Willemsen MC, Fong GT, de Vries H. Age and educational inequalities in smoking cessation due to three population-level tobacco control interventions: findings from the International Tobacco Control (ITC) Netherlands Survey. Health Educ Res. 2013;28(1):83–91.
Federico B, Mackenbach JP, Eikemo TA, Kunst AE. Impact of the 2005 smoke-free policy in Italy on prevalence, cessation and intensity of smoking in the overall population and by educational group. Addiction. 2012;107(9):1677–86.
European Commission. Smoke-free environments [Available from: https://ec.europa.eu/health/tobacco/smoke-free-environments_en].
Hahn EJ, Rayens MK, Wiggins AT, Gan W, Brown HM, Mullett TW. Lung cancer incidence and the strength of municipal smoke-free ordinances. Cancer. 2018;124(2):374–80.
Jones MR, Barnoya J, Stranges S, Losonczy L, Navas-Acien A. Cardiovascular Events Following Smoke-Free Legislations: An Updated Systematic Review and Meta-Analysis. Curr Environ Health Rep. 2014;1(3):239–49.
Mons U, Nagelhout GE, Guignard R, McNeill A, van den Putte B, Willemsen MC, et al. Comprehensive smoke-free policies attract more support from smokers in Europe than partial policies. Eur J Public Health. 2012;22(Suppl 1):10–6.
Nagelhout GE, de Vries H, Boudreau C, Allwright S, McNeill A, van den Putte B, et al. Comparative impact of smoke-free legislation on smoking cessation in three European countries. Eur J Public Health. 2012;22 Suppl 1(Suppl 1):4–9.
Xiao H, Zhang H, Wang D, Shen C, Xu Z, Zhang Y, et al. Impact of smoke-free legislation on acute myocardial infarction and stroke mortality: Tianjin, China, 2007–2015. Tob Control. 2020;29:61–67.
Hoffmann SH, Schramm S, Jarlstrup NS, Christensen AI. Surveillance of smoking habits in the Danish population - The trend from 1994 to 2017 [In Danish: Danskernes Rygevaner - Udviklingen fra 1994 til 2017]. Copenhagen: The National Institute of Public Health, The Danish Health Authority; 2018.
Aarestrup AK, Due TD, Juel K. Evaluation of The Smoke-Free Environment Act [In Danish: Evaluering af loven om røgfri miljøer - lov nr. 512 af 6. juni 2007]. The National Institute of Public Health, University of Southern Denmark; 2009: Copenhagen, Denmark. Available from: https://www.cancer.dk/dyn/resources/File/file/7/5837/1475670015/evaluering-af-loven-om-roegfri-miljoeer.pdf.
Brown A, Moodie C, Hastings G. A longitudinal study of policy effect (smoke-free legislation) on smoking norms: ITC Scotland/United Kingdom. Nicotine & tobacco research : official journal of the Society for Research on Nicotine and Tobacco. 2009;11(8):924–32.
Lagerweij NA, Kuipers MAG, Schreuders M, Grard A, Mlinarić M, Richter M, et al. The visibility of smoking in Europe and its relationship with youth’s positive beliefs about smoking. Int J Public Health. 2019;64(9):1335–44.
Rees VW. The promise - and pitfalls - of smoke-free policy adoption. Isr J Health Policy Res. 2019;8(1):41.
Pisinger C, Jørgensen T, Toft U. A multifactorial approach to explaining the stagnation in national smoking rates. Dan Med J. 2018;65(2):A5448
Lynch JW, Kaplan G. Socioeconomic Position. In: Berkman LFKI, editor. Social Epidemiology. 1st ed. Oxford: Oxford University Press; 2000. p. 13–35.
Krieger N, Williams DR, Moss NE. Measuring Social Class in US Public Health Research: Concepts, Methodologies, and Guidelines. Annu Rev Public Health. 1997;18(1):341–78.
Thygesen LC, Daasnes C, Thaulow I, Bronnum-Hansen H. Introduction to Danish (nationwide) registers on health and social issues: structure, access, legislation, and archiving. Scandinavian journal of public health. 2011;39(7 Suppl):12–6.
Acknowledgements
Not applicable.
Funding
Open access funding provided by University Library of Southern Denmark This work was supported by the Danish Foundation TrygFonden. The funding organization had no influence on the design and conduct of the study, analysis, interpretation of results, preparation, review, or approval of the manuscript.
Author information
Authors and Affiliations
Contributions
NJ and JT contributed to the conception and design of the study. NJ and JT acquired the data. NJ, JT, and LT designed the analytical strategy and completed the analyses. All authors interpreted the findings. NJ wrote first draft of the manuscript. JT, LT, CP, JV, and MG critically revised the manuscript for important intellectual content. All authors contributed and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
According to Danish legislation, register-based studies not including human biological material do not require approval by committees on biomedical research ethics [56]. This study was approved by SDU Research & Innovation Organization (journal no. 16/49148) who examines and approves all scientific and statistical projects at the University of Southern Denmark according to the Danish Data Protection Regulation since 2016.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Jarlstrup, N.S., Thygesen, L.C., Pisinger, C. et al. Trends in smoking-related diseases by socioeconomic position following a national smoking ban in 2007: a nationwide study in the Danish population. BMC Public Health 23, 1648 (2023). https://doi.org/10.1186/s12889-023-16456-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-023-16456-3