Abstract
Background
Previous studies have identified that socioeconomic status (SES) and obesity are associated with hypertension. However, their interaction on hypertension risk has not yet been assessed.
Methods
The study used data from 6,069 Tibetan residents in Chengguan District in Lhasa, the Chinese Tibetan autonomous region’s capital, based on a cohort study conducted from May 2018 to September 2019 in five provinces in southwest China. We used logistic regression models to assess the complex relations of SES and obesity with hypertension.
Results
Compared with individuals of high SES, low and moderate SES were positively associated with high risk of hypertension. SES and obesity have significant additive interaction on hypertension (general obesity by BMI: RERI = 1.33, P < 0.001; abdominal obesity by WC: RERI = 0.76, P < 0.001; abdominal obesity by WHtR: RERI = 0.96, P < 0.001). In people from the low and moderate SES segments, obesity was linked to an increased risk of hypertension, but the correlations were stronger in people from the moderate SES category. Compared with people of high SES and non obese, those with moderate SES and obesity had a higher risk of hypertension, and ORs were 4.38 (2.80, 6.84) for general obesity by BMI, 3.38 (2.05, 5.57) for abdominal obesity by WC, and 3.18 (1.57, 6.42) for abdominal obesity by WHtR.
Conclusion
There is an independent and additive interaction effect of obesity and SES on the risk of hypertension. People with obesity, especially those of moderate and low SES, should reduce weight and waist circumference, and pay more attention to blood pressure. Moreover, the government, health administration departments, and society should prioritize improving the socioeconomic status of the Tibetan population and addressing risk factors like obesity.
Similar content being viewed by others
Introduction
The development of society and the economy has led to an increased consumption of high-fat, high-sugar, and high-sodium foods among ethnic minorities in plateau areas. Tibet, also known as the “Third Pole,“ is situated in the southwest of the Qinghai-Tibet Plateau. With an average altitude exceeding 4,000 m, the region is characterized by a harsh climate, strong radiation, low pressure hypoxia, barren land, and a poor economic foundation [1]. Of the permanent population, 86.01% (3,137,901 individuals) adopt a high-fat and high-sodium diet [2]. Furthermore, according to China’s seventh population census in 2020, the percentage of individuals with a high school education or higher in Tibet is only 18.07%, significantly lower than the national average of 30.55%Footnote 1.This, combined with a lack of healthy lifestyle choices and health interventions, harsh natural environments with low oxygen and high altitude, and complex ethnic cultural traditions and customs, has created severe and complex health problems and behavioral risk factors [3, 4, 5]. A Chinese study found that overall health among people in the Tibet Autonomous Region is lower than that of individuals in other Chinese provinces [6]. Previous research has demonstrated that hypertension incidence in Tibet is higher than in other parts of China [7]. Furthermore, a systematic review indicated that the prevalence of hypertension in Tibetan residents increases by 2% for every 100 m increase in altitude [8]. In 2019, cardiovascular diseases (CVDs) were responsible for 46.74% and 44.26% of mortality in rural and urban areas of China, respectively [9]. Hypertension is a major risk factor for CVDs and a serious threat to human health [10]. As socioeconomic development, population aging, and urbanization accelerate, the prevalence of hypertension is increasing and has become a significant public health issue [11].
Socioeconomic status (SES) is a measure of an individual’s position in the class system, including factors such as education, income, occupation, wealth, and place of residence. SES widens health gradients between groups by providing health advantages [12, 13]. Previous studies have reported the presence of SES-health gradients and a meta-analysis found that individuals with the lowest SES in terms of income, occupation, and education had a higher prevalence of hypertension than those with the highest SES [14]. In an aging society with social stratification, individual health inequalities may tend to expand with age, known as cumulative disadvantage of health disparities. This kind of health disparity is evident in Tibet, which is sparsely populated and unevenly developed.
SES and obesity are well-known predictors of hypertension, and there is substantial evidence linking SES to traditional risk factors for hypertension such as health knowledge, behaviors, lifestyle, working conditions, medical care, income, and socio-psychological resources [15,16,17]. Studies on obesity have demonstrated that body fat distribution, particularly the accumulation of abdominal fat, is strongly associated with CVDs and is valuable in predicting the risk of CVDs [18]. While the relationship between SES, obesity, and hypertension is not new, it has received less attention in high-altitude regions with ethnic minorities. Furthermore, studies on hypertension and obesity among Tibetan residents in Tibet are relatively scarce.
There is a global debate on the predictive role of various obesity markers for hypertension development. Relying solely on a single obesity marker to predict hypertension may weaken the evidence’s strength. Moreover, current studies face several issues. First, although many studies have examined the relationship and pathways between obesity, hypertension, and SES, few have investigated how SES and obesity interact to cause hypertension. Second, earlier studies tended to use a single measure to reflect individuals’ overall SES level [19], indicating the need for a comprehensive SES index that can adequately reflect its effects on obesity and hypertension. Additionally, the lack of targeted studies on characteristic populations calls for further exploration of the relationship between SES, obesity, and hypertension in Tibetans.
This study aims to verify the association between SES, obesity, and hypertension in Tibetan residents to address the current research gap. The findings of this study can inform future research and aid in developing public health policies for similar high-altitude indigenous populations in China or other countries.
Methods
Study population
This study was conducted from May 2018 to September 2019 in five provinces of south-western regions of China. Data was collected primarily through electronic questionnaires and health examinations. Details of the study design, data collection, and methods were reported previously [20]. The ethics committee of Sichuan University (K2016038) approved this study. We obtained informed consent from all participants, and we conducted all methods in compliance with the relevant guidelines and regulations. The data used in this study was from the Chengguan District in Lhasa, the Chinese Tibetan autonomous region’s capital. For the current analyses, individuals missing data on any outcome, exposure, or adjusted variables were also disqualified, as were participants under the age of 18. In the end, 6069 people in all were used for the analyses.
Exposure
Based on previous studies, SES was measured using self-reported family income level, employment, education level, and health insurance gathered through questionnaires [21]. Each element was separated into three levels, with each level taking into account the sample size and practical interpretation. The family income level was categorized into < 20000yuan, 20000-59999yuan, and ≥ 60000yuan. Education was categorized into illiteracy, primary school, junior high school or higher. Occupation was categorized into upper (including administrative and management personnel, professional technical personnel, retirees), lower (including agricultural, forestry, animal husbandry and fishery workers; sales and service staff) and unemployment. Health insurance was categorized into medical insurance for urban population, new rural cooperative medical system, and no health insurance.
An overall SES variable based on family income level, employment, education level, and health insurance was developed using the latent class analysis. Using item-response probabilities, three latent classes were identified, representing high, moderate, and low SES [22]. Table S1 describes the indicators in models with different numbers of latent classes.
Participants’ height, waist circumference (WC), and weight were measured anthropometrically to determine obesity according to a standard protocol from the Working Group on Obesity [23]. Obesity was assessed by BMI, WC, and WHtR indicators. The cut-off values for the BMI, WC, and WHtR for obesity were 28.0 kg/m2 for both sexes, 90 cm for men and 85 cm for women, and 50.0% for both men and women, respectively [24,25,26].
Assessment of outcome and other covariates
Participants’ blood pressure (BP) was measured using electronic sphygmomanometers by trained medical personnel, according to the American Heart Association’s standardized protocol [27]. Diastolic BP (DBP) and systolic BP (SBP) were calculated based on the average of the three measurements. Hypertension was defined as having an average measured SBP≥140 mmHg or DPB≥90 mmHg or any use of antihypertensive medication (self-reported hypertension)[28].
The smoking status is a three-category variable (never, current, and former). Never smoking refers to individuals who have smoked fewer than 100 cigarettes in their lifetime. Current smoking was defined as having smoked more than 100 cigarettes in their lifetime, and former smoking was defined as having quit smoking for more than six months [29]. The Alcohol drinking status is a three-category variable (never, occasionally, and often). “Never drinking alcohol” means that the individual has never consumed any alcoholic beverages throughout their lifetime. Often drinking was defined as drinking alcohol more than two days per week on average over the past year, while occasional drinking was defined as drinking alcohol less than three days a week on average during the past year. The DASH score concentrated on seven different dietary categories, including fresh fruits and vegetables, legumes, whole grains, red and processed meat, dairy, and salt with a sodium content, and each category was given a score from 1 to 5 based on the quintile of the average food consumption [30, 31]. Physical activity comprehensively considered the occupation, transportation, household, and leisure time of participants [32]. Sleep disorders were assessed by early awakening, difficulty in falling asleep, drug-assisted sleep and poor sleep, and any positive one was defined as sleep disorder [33].
Statistical analysis
The basic characteristics of hypertensive and normotensive individuals were described using descriptive statistics. Continuous and categorical characteristic variables between normal and hypertensive subjects were reported as mean ± SD (The statistical test results show that the data presents a normal distribution) and numbers (percentages) and compared using the Student’s t-test and chi-squared test.
Multivariable logistic regression model was used to evaluate the association of SES and obesity on hypertension. Based on the previous literature [34], fully adjusted models including the following covariates: age, sex (male and female), smoking status (never, current, and former), alcohol status (never, occasionally, and often), physical activity, DASH score, sleep disorder (yes and no), and hypertension family history (yes, no, and not sure).
We conducted a stratified analysis by latent class of SES to explore associations of obesity with hypertension among adults in different socioeconomic subgroups. In this analysis, participants with normal weight served as the reference group, and we examined whether obesity was associated with an increased risk of hypertension in various SES categories.
We also included a product term for SES (low and high) and obesity (yes and no) to the model in order to quantify the additive and multiplicative interactions. The odds ratio (OR) with its 95% confidence interval (CI) of the product term was the measure of interaction on the multiplicative scale. We used the relative excess risk due to interaction (RERI) and its corresponding 95% CI as the measure of interaction on the additive scale.
We further divided people into six groups based on SES (low, moderate, and high) and obesity (yes or no) and computed ORs of hypertension in each group compared with those with high SES and normal weight in order to investigate the combined correlations.
We performed several sensitivity analyses. First, we additionally adjusted for diabetes to minimize the influence of multimorbidity. Second, we excluded those had any physician-diagnosed hypertension to test the accuracy of the effect estimates. Third, we used the higher cutoff point of BMI ≥30 (the recommendations of the World Health Organization) to test the stability of the results. R 4.0.2 (R Foundation for Statistical Computing) was used for the analyses, and statistical significance was declared if P values < 0.05.
Results
Population characteristics
Table 1 presents the general characteristics of the study population, including their average age of 46.97 years, with 60.70% being female. The population consisted of 6,069 participants, of which 381 (6.28%) had high SES, 1,556 (25.64%) had medium SES, and 4,132 (68.08%) had low SES. Hypertensive participants tended to be older, male, former smokers, frequent drinkers, less physically active, have a lower DASH score, lower SES level, a family history of hypertension, and experience sleep disorders. Moreover, the hypertensive participants had higher BMI, WC, and WHtR obesity indicators compared to the normotensive participants.
Association of SES and obesity with hypertension
Table 2 displays the ORs and 95% CIs for the association of obesity and SES with hypertension according to adjusted models. The results indicate a significant association between SES and hypertension, with an OR of 1.97 (1.51, 2.57) when participants of low SES were compared to those of high SES, after controlling for age, sex, smoking status, alcohol drinking status, physical activity, sleep disorder, DASH score, hypertension family history, and general obesity (by BMI). Positive associations were also observed between obesity indicators and hypertension, with ORs of 1.95 (1.67, 2.27), 1.92 (1.66, 2.21), and 2.12 (1.74, 2.58) for BMI, WC, and WHtR indicators, respectively. Sensitivity analyses produced identical results (see Table S2 and Table S3).
Interaction and joint analysis of SES and obesity with hypertension
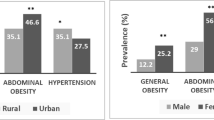
A significant additive interaction between SES and obesity (general obesity by BMI, abdominal obesity by WC and WHtR) on hypertension was found, but there was no significant multiplicative interaction (P > 0.05). For instance, when comparing participants of low SES to those of high SES, the RERI was 1.33 (0.53, 2.12), indicating a relative excess risk of 1.33 due to the additive interaction (see Fig. 1).
All models adjusted for age, sex, smoking status, alcohol drinking status, physical activity, sleep disorder, DASH score and hypertension family history.
Multiplicative interaction was evaluated using hazard ratios for the product term between obesity (yes v no) and SES (low v high), and the multiplicative interaction was statistically significant when its confidence interval did not include 1. Additive interaction was evaluated using relative excess risk due to interaction (RERI) between obesity (yes v no) and SES (low v high), and the additive interaction was statistically significant when its confidence interval did not include 0.
The study found that individuals in the low and moderate SES groups had an increased risk of hypertension linked to obesity, with the correlations being stronger in the moderate SES group. For instance, the ORs for hypertension among individuals with general obesity by BMI compared to normal weight were 1.24 (0.73, 2.13) for those in the high SES group, 2.50 (1.77, 3.54) for those in the moderate SES group, and 1.94 (1.62, 2.32) for those in the low SES group (Fig. 1).
Figure 2 illustrated the combined association of SES and obesity with hypertension. The results showed that adults with moderate SES and obesity had a higher risk of developing hypertension than those with high SES and no obesity, with ORs of 4.38 (2.80, 6.84) for general obesity by BMI, 3.38 (2.05, 5.57) for abdominal obesity by WC, and 3.18 (1.57, 6.42) for abdominal obesity by WHtR (Fig. 2).
All models adjusted for age, sex, smoking status, alcohol drinking status, physical activity, sleep disorder, DASH score and hypertension family history.
Discussion
An independent and additional interaction effect of obesity and SES on hypertension was observed. Positive associations were found between lower SES and hypertension, with stronger correlations of obesity with hypertension among those of moderate SES. The highest risks of hypertension were observed in people with moderate SES and obesity. This is the first study to examine the interaction associations of three types of obesity and overall SES with hypertension.
In previous studies, a single variable such as income, occupation, or education level was typically used to represent SES at the individual level. Studies investigating the relationship between SES and hypertension have reported mixed results, with some finding a positive association [35, 36] and others reporting a negative association [37, 38]. A population-based cohort study conducted in rural South-Central Uganda found that hypertension was more prevalent among those with higher SES [37], while a study of 76 low- and middle-income countries (LMICs) found that hypertension was more common among adults in the lowest socioeconomic classes as LMICs developed economically [36]. The discrepancy in findings across previous studies may be due to a variety of factors, including socioeconomic inequality and social patterns of behavior that contribute to risk factors [39]. For example, evidence suggests that individuals of low SES in LMICs are more likely to use tobacco and alcohol and to consume a less healthy diet, while individuals of high SES tend to be more physically inactive [40]. Additionally, most studies have investigated only a single socioeconomic factor, but different socioeconomic factors represent various aspects of SES or social class and should not be simply interchanged with one another [19]. Our study found a positive association between low and moderate SES and a higher risk of hypertension compared to participants of high SES. The relatively low levels of economic and educational development in Tibet are important factors that impact the prevention and treatment of hypertension.
Our study found a positive correlation between hypertension and all three types of obesity indicators, which is consistent with previous research [41,42,43]. The prevalence of obesity and associated disorders is increasing worldwide, with adipose storage accounting for 60% of hypertension cases [44]. The relationship between obesity and hypertension is complex and multifactorial, involving genetics, environment, sympathetic nervous system activity, renal function, and insulin resistance [45]. In Tibet, the cold climate has led to a diet high in fat, sodium, and protein, and low in sugar and cellulose, with staples such as yak beef, milk residue, ghee, and sweet tea [46]. This diet may contribute to the dual threat of obesity and hypertension among Tibetans.
Our study confirmed that all three types of obesity indicators were associated with higher risks of hypertension among participants with moderate and low SES. Additionally, we found significant additive interactions, with those with moderate SES showing a stronger link between obesity and hypertension. These findings emphasize the importance of weight loss and waist circumference reduction, particularly for those with moderate SES. Few studies have examined the interaction between SES and obesity on the risk of hypertension. One study conducted in Peru showed that education level was an effect modifier of the association between BMI and both SBP and DBP [47]. The socioeconomic distribution of the most significant non-communicable disease risk factors may be related to the biological mechanism of the interaction between SES, obesity, and hypertension [40], and this interaction may also be affected by the plateau environment and Tibetan dietary habits. Compared to people with low SES, those with moderate SES may be more likely to consume a high-fat diet, while those with low SES tend to be more physically active [48]. These are important influencing factors for the prevalence of hypertension. These findings underscore the need for weight loss and waist circumference reduction, particularly for those with moderate SES. To fully understand the intricate interactions between SES, obesity, and hypertension, further research is still required.
This is the first study reporting a significant additive interaction between SES and obesity on the risk of hypertension. An overall SES variable was created to assess the complex relationships between SES, obesity, and hypertension. However, several limitations should be acknowledged. First, measurement errors were inevitable due to self-reported socioeconomic information and hypertension based on a single blood pressure measurement(It needs to be noted that we conducted a separate analysis of participants who had already been diagnosed with hypertension, which demonstrated the stability of our results.). Second, despite accounting for important covariates in the analysis, the possibility of reverse causation and residual confounding (e.g., ambient air pollution [34]) cannot be fully eliminated. Third, the use of a BMI cutoff of 28 kg/m2 for obesity classification does not align with much of the international evidence, including the recommendations of the World Health Organization (30 kg/m2), which limits the extrapolation of results to some extent. Fourth, the cross-sectional design restricts the estimation of causal interpretations.
Conclusion
Lower SES was positively associated with hypertension in our study. The highest risk of hypertension was observed in individuals with moderate SES and obesity, with stronger correlations between obesity and hypertension seen in this group. We found an independent and additive interaction effect of obesity and SES on the risk of hypertension. Thus, people with obesity, particularly those with moderate and low SES, should focus on reducing weight and waist circumference, and pay close attention to their blood pressure. Additionally, we recommend strengthening the adaptability of health education to the language and daily life of Tibetan residents, which can be achieved through the widespread dissemination of health knowledge, promotion of healthy lifestyles. Furthermore, the health administration departments should focus on deepening the management of chronic diseases and encouraging the signing of family doctor contracts to enhance their healthcare.
Data Availability
Due to property rights protection, the data sets created and analyzed during the current study are not publically accessible, however they are available from the corresponding author upon justifiable request.
References
Wu T. The Qinghai-Tibetan plateau: how high do Tibetans live? High Alt Med Biol. 2001;2(4):489–99.
Li K, Zhang Q, Cai H, He R, Nima Q, Li Y, Suolang D, Cidan Z, Wangqing P, Zhao X, et al. Association of Tibetan Habitual Food and Metabolic Syndrome among Tibetan People in China: a cross-sectional study. Front Nutr. 2022;9:888317.
Aryal N, Weatherall M, Bhatta YK, Mann S. Blood pressure and hypertension in adults permanently living at high Altitude: a systematic review and Meta-analysis. High Alt Med Biol. 2016;17(3):185–93.
Zheng CY, Wang ZW, Chen Z, Zhang LF, Wang X, Dong Y, Nie JY, Wang JL, Shao L, Tian Y. [Association between the types of obesity and the 10-year-coronary heart disease risk, in Tibet Autonomous Region and Xinjiang Uygur Autonomous Region]. Zhonghua Liu Xing Bing Xue Za Zhi. 2017;38(6):721–6.
Bilo G, Caravita S, Torlasco C, Parati G. Blood pressure at high altitude: physiology and clinical implications. Kardiol Pol. 2019;77(6):596–603.
Su JT, Zhang YM, Wang P, Du J, Wei ZH. [Comparative analysis of comprehensive health status among 31 provinces in China and 134 countries (regions) in 2015]. Zhonghua Yu Fang Yi Xue Za Zhi. 2020;54(2):165–8.
Sun SF. Epidemiology of hypertension on the Tibetan Plateau. Hum Biol. 1986;58(4):507–15.
Mingji C, Onakpoya IJ, Perera R, Ward AM, Heneghan CJ. Relationship between altitude and the prevalence of hypertension in Tibet: a systematic review. Heart. 2015;101(13):1054–60.
Report on Cardiovascular Health and Diseases in China. 2021: An Updated Summary. Biomed Environ Sci 2022, 35(7):573–603.
Lin KC, Tsao HM, Chen CH, Chou P. Hypertension was the major risk factor leading to development of cardiovascular diseases among men with hyperuricemia. J Rheumatol. 2004;31(6):1152–8.
Ruilope LM, Nunes Filho ACB, Nadruz W Jr, Rosales R, Verdejo-Paris FF. Obesity and hypertension in Latin America: current perspectives. Hipertens Riesgo Vasc. 2018;35(2):70–6.
McEniry M, Samper-Ternent R, Flórez CE, Pardo R, Cano-Gutierrez C. Patterns of SES Health Disparities among older adults in three Upper Middle- and two high-income countries. J Gerontol B Psychol Sci Soc Sci. 2019;74(6):e25–e37.
Smith KV, Goldman N. Socioeconomic differences in health among older adults in Mexico. Soc Sci Med. 2007;65(7):1372–85.
Leng B, Jin Y, Li G, Chen L, Jin N. Socioeconomic status and hypertension: a meta-analysis. J Hypertens. 2015;33(2):221–9.
Wu X, Wang Z. Role of Socioeconomic Status in Hypertension among Chinese Middle-Aged and Elderly Individuals. Int J Hypertens 2019, 2019:6956023.
Bijani M, Parvizi S, Dehghan A, Sedigh-Rahimabadi M, Rostami-Chijan M, Kazemi M, Naghizadeh MM, Ghaemi A, Homayounfar R, Farjam M. Investigating the prevalence of hypertension and its associated risk factors in a population-based study: Fasa PERSIAN COHORT data. BMC Cardiovasc Disord. 2020;20(1):503.
Cutler DM, Lleras-Muney A. Understanding differences in health behaviors by education. J Health Econ. 2010;29(1):1–28.
Koenen M, Hill MA, Cohen P, Sowers JR. Obesity, adipose tissue and vascular dysfunction. Circ Res. 2021;128(7):951–68.
Zhang YB, Chen C, Pan XF, Guo J, Li Y, Franco OH, Liu G, Pan A. Associations of healthy lifestyle and socioeconomic status with mortality and incident cardiovascular disease: two prospective cohort studies. BMJ. 2021;373:n604.
Zhao X, Hong F, Yin J, Tang W, Zhang G, Liang X, Li J, Cui C, Li X. Cohort Profile: the China multi-ethnic cohort (CMEC) study. Int J Epidemiol. 2021;50(3):721–721l.
Quaglia A, Lillini R, Mamo C, Ivaldi E, Vercelli M. Socio-economic inequalities: a review of methodological issues and the relationships with cancer survival. Crit Rev Oncol Hematol. 2013;85(3):266–77.
Sepriano A, Ramiro S, van der Heijde D, van Gaalen F, Hoonhout P, Molto A, Saraux A, Ramonda R, Dougados M, Landewé R. What is axial spondyloarthritis? A latent class and transition analysis in the SPACE and DESIR cohorts. Ann Rheum Dis. 2020;79(3):324–31.
Chen C, Lu FC. The guidelines for prevention and control of overweight and obesity in chinese adults. Biomed Environ Sci. 2004;17 Suppl:1–36.
Hou X, Lu J, Weng J, Ji L, Shan Z, Liu J, Tian H, Ji Q, Zhu D, Ge J, et al. Impact of waist circumference and body mass index on risk of cardiometabolic disorder and cardiovascular disease in chinese adults: a national diabetes and metabolic disorders survey. PLoS ONE. 2013;8(3):e57319.
Song WF, Zhong XN, Luo R, Wang YH, Li YQ, Tian KC. [Utility of waist-to-height ratio in detecting central obesity and related adverse cardiovascular risk among normal weight adults]. Zhonghua Yu Fang Yi Xue Za Zhi. 2010;44(12):1102–5.
Zhou BF. Predictive values of body mass index and waist circumference for risk factors of certain related diseases in chinese adults–study on optimal cut-off points of body mass index and waist circumference in chinese adults. Biomed Environ Sci. 2002;15(1):83–96.
Perloff D, Grim C, Flack J, Frohlich ED, Hill M, McDonald M, Morgenstern BZ. Human blood pressure determination by sphygmomanometry. Circulation. 1993;88(5 Pt 1):2460–70.
Zhang Y, Wang Y, Chen Y, Zhou J, Xu L, Xu K, Wang N, Fu C, Liu T. Associations of dietary patterns and risk of hypertension in Southwest China: a prospective cohort study. Int J Environ Res Public Health 2021, 18(23).
Pärna K, Ringmets I, Siida S. Self-rated health and smoking among physicians and general population with higher education in Estonia: results from cross-sectional studies in 2002 and 2014. Arch Public Health. 2019;77:49.
Eilat-Adar S, Sinai T, Yosefy C, Henkin Y. Nutritional recommendations for cardiovascular disease prevention. Nutrients. 2013;5(9):3646–83.
Chiu S, Bergeron N, Williams PT, Bray GA, Sutherland B, Krauss RM. Comparison of the DASH (Dietary Approaches to stop hypertension) diet and a higher-fat DASH diet on blood pressure and lipids and lipoproteins: a randomized controlled trial. Am J Clin Nutr. 2016;103(2):341–7.
Ainsworth BE, Haskell WL, Herrmann SD, Meckes N, Bassett DR Jr, Tudor-Locke C, Greer JL, Vezina J, Whitt-Glover MC, Leon AS. 2011 Compendium of Physical Activities: a second update of codes and MET values. Med Sci Sports Exerc. 2011;43(8):1575–81.
Li Y, Nima Q, Yu B, Xiao X, Zeng P, Suolang D, He R, Ciren Z, Wangqing P, Laba C, et al. Determinants of self-rated health among an older tibetan population in a chinese plateau area: analysis based on the conceptual framework for determinants of health. BMC Public Health. 2021;21(1):489.
Xu H, Guo B, Qian W, Ciren Z, Guo W, Zeng Q, Mao D, Xiao X, Wu J, Wang X, et al. Dietary Pattern and Long-Term Effects of Particulate Matter on blood pressure: a large cross-sectional study in chinese adults. Hypertension. 2021;78(1):184–94.
McDoom MM, Palta P, Vart P, Juraschek SP, Kucharska-Newton A, Diez Roux AV, Coresh J. Late life socioeconomic status and hypertension in an aging cohort: the atherosclerosis risk in Communities Study. J Hypertens. 2018;36(6):1382–90.
Kirschbaum TK, Sudharsanan N, Manne-Goehler J, De Neve JW, Lemp JM, Theilmann M, Marcus ME, Ebert C, Chen S, Yoosefi M, et al. The Association of Socioeconomic Status with Hypertension in 76 low- and Middle-Income Countries. J Am Coll Cardiol. 2022;80(8):804–17.
Mustapha A, Ssekasanvu J, Chen I, Grabowski MK, Ssekubugu R, Kigozi G, Reynolds SJ, Gray RH, Wawer MJ, Kagaayi J, et al. Hypertension and socioeconomic status in South Central Uganda: a Population-Based Cohort Study. Glob Heart. 2022;17(1):3.
Kibria GMA, Hashan MR, Hossain MM, Zaman SB, Stennett CA. Clustering of hypertension, diabetes and overweight/obesity according to socioeconomic status among bangladeshi adults. J Biosoc Sci. 2021;53(2):157–66.
Stringhini S, Bovet P. Socioeconomic status and risk factors for non-communicable diseases in low-income and lower-middle-income countries. Lancet Glob Health. 2017;5(3):e230–1.
Allen L, Williams J, Townsend N, Mikkelsen B, Roberts N, Foster C, Wickramasinghe K. Socioeconomic status and non-communicable disease behavioural risk factors in low-income and lower-middle-income countries: a systematic review. Lancet Glob Health. 2017;5(3):e277–89.
Nurdiantami Y, Watanabe K, Tanaka E, Pradono J, Anme T. Association of general and central obesity with hypertension. Clin Nutr. 2018;37(4):1259–63.
Tanaka M. Improving obesity and blood pressure. Hypertens Res. 2020;43(2):79–89.
Zhao Y, Wang L, Xue B, Wang Y. Associations between general and central obesity and hypertension among children: the childhood obesity study in China Mega-Cities. Sci Rep. 2017;7(1):16895.
Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, Mullany EC, Biryukov S, Abbafati C, Abera SF, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the global burden of Disease Study 2013. Lancet. 2014;384(9945):766–81.
Seravalle G, Grassi G. Obesity and hypertension. Pharmacol Res. 2017;122:1–7.
Shen Y, Chang C, Zhang J, Jiang Y, Ni B, Wang Y. Prevalence and risk factors associated with hypertension and prehypertension in a working population at high altitude in China: a cross-sectional study. Environ Health Prev Med. 2017;22(1):19.
Bernabe-Ortiz A, Carrillo-Larco RM, Miranda JJ. Association between body mass index and blood pressure levels across socio-demographic groups and geographical settings: analysis of pooled data in Peru. PeerJ. 2021;9:e11307.
Vu THL, Bui TTQ, Nguyen TKN, Hoang VM. Adverse influence of multilevel socioeconomic status on physical activity: results from a national survey in Vietnam. BMC Public Health. 2020;20(1):561.
Acknowledgements
The authors are extremely grateful to the National Key Research and Development Program of China (Grant No. 2017YFC0907302, 2017YFC0907305) for the financial support and to the peer reviewers whose insightful comments and suggestions significantly improved the quality of the manuscript.
Funding
This work was supported by the National Key Research and Development Program of China (Grant No. 2017YFC0907302), the Natural Science Foundation of Tibet Autonomous Region (Grant No. XZ202101ZR0103G, XZ2019ZR G-142).
Author information
Authors and Affiliations
Contributions
Conceptualization, Y.L., J.L., and Q.N.; Data curation, Y.L., Q.N.; Formal analysis, Y.L.; Investigation, Y.L.; Methodology, Y.L.; Project administration, Y.L.; Writing—original draft, Y.L., J.L.; Writing—review & editing, Y.L., J.L., and Q.N. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the ethics committee of Sichuan University (K2016038). Informed consent was obtained from all participants, and all methods were performed in accordance with the relevant guidelines and regulations. The records of participants were anonymized and deidentified before analysis.
Consent for publication
Not applicable.
Competing interests
The authors declare no conflicts of interest.
Financial support
This work was supported by the National Key Research and Development Program of China (Grant No. 2017YFC0907302, 2017YFC0907305) Ethics approval and consent to participate This study was approved by the ethics committee of Sichuan University (K2016038). Informed consent was obtained from all participants, and all methods were performed in accordance with the relevant guidelines and regulations. The records of participants were anonymized and deidentified before analysis.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Li, Y., Li, J. & Nima, Q. Associations of socioeconomic status and obesity with hypertension in tibetan adults in a Chinese plateau area. BMC Public Health 23, 1840 (2023). https://doi.org/10.1186/s12889-023-15864-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-023-15864-9