Abstract
Background
Immigrant women’s challenges in realizing sexual and reproductive health and rights (SRHR) are exacerbated by the lack of knowledge regarding how to tailor post-partum contraceptive services to their needs. Therefore, the overall aim of the IMPROVE-it project is to promote equity in SRHR through improvement of contraceptive services with and for immigrant women, and, thus, to strengthen women’s possibility to choose and initiate effective contraceptive methods post-partum.
Methods
This Quality Improvement Collaborative (QIC) on contraceptive services and use will combine a cluster randomized controlled trial (cRCT) with a process evaluation. The cRCT will be conducted at 28 maternal health clinics (MHCs) in Sweden, that are the clusters and unit of randomization, and include women attending regular post-partum visits within 16 weeks post birth. Utilizing the Breakthrough Series Collaborative model, the study’s intervention strategies include learning sessions, action periods, and workshops informed by joint learning, co-design, and evidence-based practices. The primary outcome, women’s choice of an effective contraceptive method within 16 weeks after giving birth, will be measured using the Swedish Pregnancy Register (SPR). Secondary outcomes regarding women’s experiences of contraceptive counselling, use and satisfaction of chosen contraceptive method will be evaluated using questionnaires completed by participating women at enrolment, 6 and 12 months post enrolment. The outcomes including readiness, motivation, competence and confidence will be measured through project documentation and questionnaires. The project’s primary outcome involving women’s choice of contraceptive method will be estimated by using a logistic regression analysis. A multivariate analysis will be performed to control for age, sociodemographic characteristics, and reproductive history. The process evaluation will be conducted using recordings from learning sessions, questionnaires aimed at participating midwives, intervention checklists and project documents.
Discussion
The intervention’s co-design activities will meaningfully include immigrants in implementation research and allow midwives to have a direct, immediate impact on improving patient care. This study will also provide evidence as to what extent, how and why the QIC was effective in post-partum contraceptive services.
Trial registration
NCT05521646, August 30, 2022.
Similar content being viewed by others
Introduction
Globally, as compared to native-born women, immigrant women across countries of all income groups report lower access to contraceptive services, accompanied by higher rates of unintended pregnancies and abortions [1,2,3,4]. A plethora of barriers to accessing contraceptive services exist for immigrants, such as language challenges, various cultural and religious beliefs, strict gender roles, social pressure and financial factors [5, 6]. Additionally, despite variation across immigrant populations, their family planning knowledge is generally low, causing misconceptions about contraceptive methods and limiting their possibilities to prevent unintended pregnancies [7,8,9].
Immigrants’ contraceptive decision making is further influenced by migration status, changes or instabilities in living conditions, and adaptation to resettlement communities [10,11,12]. While immigrants post resettlement might employ using contraceptives to regain financial and social stability, barriers to contraceptive services still exist [12,13,14,15].
With this said, there is a paucity of research regarding immigrants and post-partum contraception use. Ensuring access to effective post-partum contraception is fundamental when seeking to reduce inequities that immigrants face in SRHR, as it prevents unintended pregnancies, abortions and enables birthspacing [16]. A short interpregnancy interval (IPI) – less than 12 months – increases the risk of complications, e.g., preterm birth, low birthweight, stillbirth and neonatal death [17, 18]. Use of more effective post-partum contraception, such as long-acting reversible contraception (LARC) (i.e. intrauterine devices) and short-acting reversible contraception (SARC) (i.e. oral contraceptive pills), supports birth-spacing and prevents unintended pregnancies, abortions as well as pregnancy-related adverse events [19]. What little evidence exists regarding immigrants’ post-partum contraceptive use highlights that immigrant women are less likely to plan or attend post-partum clinic visits and use reliable contraception methods in a timely manner compared to non-immigrants, sometimes despite their interest [20,21,22].
The antenatal and post-partum period offers room for strengthening SRHR by improving contraceptive services. One focus of such improvement efforts can include double sessions of contraceptive counseling (CC), whereby sessions occur during both the antenatal and the post-partum period, as this has shown to increase contraceptive use after giving birth [23,24,25].
Additionally, offering information about contraceptive methods’ effectiveness and potential side effects can counteract patient-provider power imbalances that may hinder women’s choices of contraceptive methods [26]. For example, in Sweden, structured CC (“the LOWE model” using an educational video, an effectiveness chart, four key questions, and a box with contraceptive models) increased LARC choice, initiation and use, when controlled for migration background [27]. Immigrant women in Sweden have also expressed the importance of trust in CC encounters, especially since they perceive these as private matters [28].
High-quality post-partum CC—meaning that the HCP discusses what matters most to a patient in choosing a method—occurs less often among immigrant women, who are less likely to know where to seek such services, even if they are free of charge [29, 30]. Furthermore, the needs of immigrant women may be known by HCPs, but the womens’ knowledge and values may not be properly addressed [31]. HCPs express several challenges in communicating with immigrant women regarding SRHR including navigating cultural and religious differences and patients’ distrust in healthcare [31,32,33]. Overall, previous studies report several opportunities for improving underutilized SRHR services by interacting with immigrant women, taking into account their experiences, and adapting one’s practice to the situation at hand [34,35,36].
Several quality improvement collaboratives (QICs) have been applied to improve obstetric, gynaecological and neonatal care, although many lacked close user engagement [37,38,39,40,41]. There is also promising evidence of how the umbrella of community-based participatory research (CBPR) and co-design methods are being employed to address health disparities and improve SRHR services for immigrants [42,43,44]. Co-design in healthcare involves HCPs, patients, caregivers, designers and researchers working together as equal partners to improve specified health outcomes and system efficiency [45]. Therefore, QICs based on the Breakthrough Series Collaborative model and co-design methods can help organizations to make and sustain measurable improvement according to patients needs, as well as stimulate joint learning and networking among HCPs [46].
In Sweden, a few small-scale QICs have demonstrated the importance and effectiveness of increasing user engagement. The evaluations of these QICs report positive results when seeking to improve access to or choice of effective methods in the context of abortion or post-partum care [40, 41, 47]. The lack of studies similar to these reflect how little evidence exists on how to combine QICs and co-design methods to improve immigrants’ post-partum contraceptive services.
Therefore, the overall aim of IMPROVE-it is to promote equity in SRHR through the improvement of contraceptive services and, thus, to strengthen women’s possibility to choose and initiate effective contraceptive methods post-partum. The hypothesis is that focusing on the following three evidence-based areas of change regarding contraceptive services:
-
1) developing tools to share information about contraceptive methods’ effectiveness,
-
2) developing approaches to providing CC and
-
3) improving access to contraceptive methods (Fig. 1) will lead to a significant increase in immigrant women’s choice and use of effective contraceptive methods.
Research questions
How does a Quality Improvement Collaborative (QIC) combined with co-design methodology influence immigrant women’s choice of effective post-partum contraception?
How and by what mechanisms does a QIC influence contraceptive services, and how does context affect the QIC efforts and outcomes?
Methods
Study design
The IMPROVE-it project will combine a cluster randomized controlled trial (cRCT) with a process evaluation to develop and study the in-depth effects of an intervention, a QIC, on contraceptive services and use. Harnessing QICs and co-design methods supported by National Quality Registers can ultimately help to close gaps between ordinary clinical practice and evidence-based guidelines [46, 48,49,50,51].
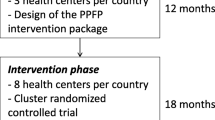
Figure 1shows the program theory of the project, which is based on a pilot study [47]. The project’s primary outcome is women´s choice of an effective contraceptive method within 16 weeks after giving birth. Effective contraception is defined as LARC (i.e. intrauterine devices and subdermal implants) and SARC (i.e. oral contraceptive pills, rings, patches, and injections).
Study setting
In 2021, 30% of newborn children in Sweden had a mother who was born outside of Sweden [52]. The foreign-born population in Sweden is heterogenous, with some of the most common countries of birth for persons born outside of Europe being: Syria, Somalia, Iraq and Afghanistan [53]. In this study, refugees and asylum seekers are considered immigrants (foreign-born persons). Post-partum clinic visit(s), including contraceptive services available to all residents as part of public health services, should be offered within 16 weeks post-partum [54]. Midwives are the main providers of post-partum care and also administer the majority of contraceptive methods [55]. This cRCT will be conducted at 28 MHCs in the regions of Jonkoping, Vastra Gotaland and Stockholm. In 2021, these 28 MHCs had between 1900–3300 pregnant women yearly [56]. All MHCs in Jonkoping (22 MHCs, 3812 births) and Stockholm (94 MCHs, 26 191 births) were invited to participate. In Vastra Gotaland (94 MCHs, 17 595 births), we invited selected clinics of sufficient cluster size.
Strategies used for recruitment
Managers at MHCs were contacted by co-authors EL or HK during 2019–2020 to inquire about their willingness to take part in the IMPROVE-it study. Due to the Covid-19 pandemic, the project’s commencement was postponed.
Initially, 29 MHCs accepted the invitation, finally 28 MHCs in three regions decided to participate. Informational meetings were held between the research team and the midwives at the MHCs during spring and fall 2021 before randomization was conducted.
Eligibility of MHCs and inclusion criteria
Inclusion criteria: MHCs in the previously described regions with > 100 registered pregnant women during 2021 were invited to participate in the cRCT.
Intervention clinics commit to register women’s choice of contraception in the Swedish Pregnancy Register (SPR) during the post-partum MHC visit and participate in the QIC for 12 months [56]. The control clinics commit to provide routine care and register consenting women’s choice of contraception in the SPR.
Self-administered questionnaire
Inclusion criteria: Women 18 years and above coming for post-partum visits within 16 weeks post birth (live birth).
Exclusion criteria: Women who do not anticipate becoming sexually active with a male partner within six months.
Midwives at intervention and control clinics will invite women to participate in the study, i.e. respond to a digital or printed paper questionnaire during the visit and be contacted for follow-up six and 12 months post enrolment. There is also the possibility to participate in a telephone interview with an interpreter. Additional information will be provided at the MHCs before prospective participants give their written, digital or verbal informed consent.
Data management
A safe web application (REDCap) for builing and managing questionnaires will be used to secure data storage [57]. The web application allows the women who wish to participate to register personal data such as name, social security number, address, email address and mobile number via a QR code. These personal data will be pseudonymised, and the research subjects will receive a study ID. Paper questionnaires will be manually entered into the REDCap database. Three of the researchers (SB, KEI and AW) will promote data quality (e.g., prevent double data entry and conduct range checks for data values).
The intervention – a QIC initiative
Midwives at the intervention clinics were invited to participate in the QIC initiative and gave their written consent to participate in the entire project. Midwives who joined the QIC after the first learning session (LS) were informed before participating in an LS. Through the consent process, participants agreed for LSs to be digitally recorded.
The intervention strategies presented at LSs will be applied at participating MHCs over nine months in 2022–2023 and follow those of the Breakthrough Series Collaborative model including [47]:
-
- Four remote digitally run and recorded learning sessions (LS) every third month.
-
- Action periods between every LS where participants apply learnings and evaluate changes in their MCH.
-
- Co-design workshops with members of the target population.
The LSs will be informed by joint learning, self-reflection, co-design and evidence-based practice. At each LS, midwives in the intervention group will participate in competency-enhancing activities, exchange experiences about counselling as well as analyze and interpret data from the SPR regarding women’s choice of contraceptive methods. They will also decide on improvement activities that they would like to test in clinical practice during the action periods by using Plan Do Study Act (PDSA) cycles [58, 59]. Through the LSs, HCPs will also practice self-reflection, which has been described as an important factor in a previous study when seeking to facilitate co-design of health and related services [60]. Such sessions will also contribute to building trusting relationships between providers of various regions, a context factor found crucial to the implementation of successful continuing midwifery care [61].
Throughout the intervention, representatives from immigrant communities will be invited to co-design workshops with researchers to share their experiences of contraceptive services post-partum and provide feedback on midwives’ improvement activities, such as the development of visual aids for counselling. Personas will also be developed during these workshops to enable midwives to best understand and design services to meet the diverse needs of their patients [62].
Defining outcomes and data collection methods
Reporting of the IMPROVE-it study results will follow the Standard Protocol Items for Clinical Trials (SPIRIT) [63, 64].
cRCT
The SPR will be used to retrieve the primary outcome, women’s choice of contraception, and covariates for evaluating social determinants such as age, sociodemographic characteristics and reproductive history. To evaluate secondary outcomes regarding participants’ satisfaction with the contraceptive counselling received, women attending the post-partum visit will complete a questionnaire that utilizes the Person-Centered Contraceptive Counseling Measure-scale (PCCC-scale) [65]. Participating women will also receive a follow-up questionnaire six and 12 months after the postpartum visit to evaluate their ongoing contraceptive use and satisfaction with the contraceptive method. In addition, the follow-up questionnaire will ask about unintended or planned pregnancy, induced abortion and miscarriages since the post-partum visit (Table 1).
The questionnaire will be completed digitally, manually on paper, or via telephone by interpreter amongst women who are illiterate or prefer this method. The printed paper questionnaire has been translated into the nine most common languages spoken by immigrants in Sweden. Participants will chose to receive follow-up text messages, e-mails or paper questionnaires at six and 12 month after the post-partum visit. Those who answered via telephone will be recalled. Several reminders/recalls will be performed.
The organizational outcomes including the MHCs’ and midwives’ readiness, motivation, competence and confidence will be measured through project documentation and a questionnaire (Table 1).
Power analysis and randomisation
The intraclass correlation coefficient (ICC) was set to 0.05 in the power analysis, equivalent to an observed ICC in a similar study [66]. To detect an anticipated 15 percentage point increase in choosing an effective contraceptive method (SARC/LARC) with 90% power at an α = 0.05 (i.e. the probability of rejecting a true null hypothesis), we needed to include at least 30 MHCs, each contributing an average of 100 participants (pregnant women). However, 28 (out of 52) agreed to participate in the study. This implies a statistical power of about 88% which was considered sufficient. The sample size calculations were performed using Stata version 17.0 [67]. No power calculations were performed for secondary outcomes.
The randomisation procedure followed a blocked cluster design. The MHCs (clusters) were first assigned to groups (blocks) based on their regional affiliation and size (number of visits by immigrant mothers in the past year), resulting in two blocks for Jonkoping and Stockholm and three blocks for Vastra Gotaland. Intervention and control status was then randomly assigned to clusters within each block.
Statistical analysis
The analysis population will consist of all women in the cRCT. Our primary goal is to estimate the effect of the QIC on choosing an effective contraceptive method using logistic regression analysis, relying on the randomization scheme to retrieve a causal estimate. We will also investigate whether the intervention effect varies by sociodemographic variables and reproductive history.
Process evaluation
The process evaluation started during the planning phase of the cRCT. Chosen improvement activities tested during action periods within three evidence-based areas of change, as well as the process itself, will be evaluated (Fig. 2). The study will use both quantitative and qualitative research methods to evaluate the QIC initiative in-depth and aims to discover which actions were carried out, what worked where, and how and why (or why not) an impact occurred.
According to Moore et al. the process evaluation will be divided into three areas for which data will be collected [68]:
-
1. The process of the QIC––to describe what is being applied, we will study and document the preparation phase of the QIC initiative, as well as ongoing activities throughout the cRCT, emerging changes in implementation and experiences of the intervention.
-
2. Mechanisms of impact––to examine how the delivered QIC produced change at the intervention clinics, we will document the evidence-based changes tested, and evaluate their impact on women’s choices, as well as identify what components work and how, including the immigrant women’s contribution in coproducing the contraceptive services.
-
3. Context–– to examine how the context affects the QIC’s implementation and outcomes, we will document how this varies across contexts, and how the intervention is delivered in the various county councils and MHCs. We will also evaluate social processes and different organizational circumstances that enable QICs as well as the target-population’s involvement.
Quantitative data collection and analysis
To assess fidelity (quality) and dose of codesigned contraceptive services delivered (quantity), a survey will be used at each LS (every third month) that collects data on components of the intervention which have been tested at each MHC. Midwives will also be asked to complete a questionnaire regarding their experiences of evidence-based changes tested at the MHCs. To assess mechanisms of impact, the participating midwives will be asked to fill in a questionnaire on their competence and confidence in providing contraceptive counselling before and after the intervention. Additional data might also be collected as the project will use an emerging design (Table 1).
Qualitative data collection
During each phase of the QIC, project documents will be collected including recordings from the LSs, field notes from phone meetings and e-mail conversations. Additionally, a checklist will be used for regular follow-up briefings with coordinators at each MHC. These tools aim to capture contextual factors (such as staff rotatation, work load, motivation, management, etc.) facilitating or hindering the QIC intervention at the various MHCs as well as potential unintended outcomes (Table 1).
Analysis
Quantitative data will be reported as medians and frequencies for the evidence-based changes made at MHCs. Qualitative thematic analysis will be employed to the qualitative data[69].
Discussion
Many health promotion and prevention studies have been carried out to improve SRHR services. Immigrants have collaborated on several health-related studies but have rarely been involved in all stages of the research process, especially the later implementation phases [42, 70]. Therefore, IMPROVE-it is designed to engage immigrants in the research process, especially in the intervention implementation phase, where representatives from immigrant communities will provide feedback on suggested improvement activities during co-design workshops.
The project will also bring forward women’s voices in that it will invite them to participate in a self-administered questionnaire regarding their choice of contraceptive method and satisfaction during CC at the post-partum visit. Importantly, to accommodate immigrant women’s views especially, we have translated the questionnaires into nine languages. Moreover, women who are illiterate will have the opportunity to participate and report their experiences via telephone with an interpreter. Data from the registers and potentially the self-administered questionnaire will be fed back to the midwives during the LSs as part of the QIC intervention.
Furthermore, the intervention includes co-design activities, including LSs created together with representatives from the target population that will use personas developed from focus group discussion data. This will enable HCPs to self-reflect and engage with immigrant women’s lived experiences of post-partum contraceptive services. Other co-design activities, such as workshops, will enable representatives from immigrant communities to provide feedback on suggested improvement activities regarding three evidence-based areas of change. To better understand the process of how the QIC is perceived, IMPROVE-it will evaluate organizational outcomes such as midwives’ confidence and competence. Ultimately, this intervention allows HCPs to have a direct impact on improving patient care by applying immediate changes to their practice that may be sustained over time.
However, a key limitation of the study is that it may be difficult to capture exactly how the intervention is delivered in the various health services regions and MHCs, since we have to rely on midwives self-reports of tested changes. To overcome this difficulty, we will triangulate our data by also collecting such information via coordinators and LS questionnaires.
Previous case studies reporting on QICs show positive results when seeking to improve access to or choice of effective methods in the context of abortion or post-partum care [40, 41, 47]. Yet, there is still limited evidence regarding to what extent, how and why a QIC is effective and what factors influence a QIC in these healthcare contexts, due to a general lack of understanding on the role of context, mechanisms of change and critical components of success [71,72,73]. This lack of understanding is especially problematic given the lack of SRHR intervention studies including immigrant women, as we know that their contraceptive use is generally low [1,2,3,4].
A challenge of IMPROVE-it will be to evaluate which components have had which effect, but the process evaluation will enable an in-depth analysis of these issues. By using the design of a cRCT, the study also offers the potential to distinguish between varying influences of overlapping improvement activities.
Availability of data and materials
The dataset generated and/or analysed during the current study is not publicly available due to restrictions from the ethics review board, but it can be made available to qualified researchers upon request, after approval from the ethics board. EL should be contacted to request the data.
References
Usta J, Taleb R, El Harakeh S, El Kheir R, Jbahi M, Dassouki S, et al. Predictors of Contraception Use Among Syrian Refugees in Lebanon: Results from a Cross-Sectional Study. Matern Child Health J. 2021;25(4):684–93.
Ackerson K, Zielinski R. Factors influencing use of family planning in women living in crisis affected areas of Sub-Saharan Africa: A review of the literature. Midwifery. 2017;54:35–60.
Omland G, Ruths S, Diaz E. Use of hormonal contraceptives among immigrant and native women in Norway: data from the Norwegian Prescription Database. BJOG Int J Obstet Gynaecol. 2014;121(10):1221–8.
Väisänen H, Koponen P, Gissler M, Kontula O. Contraceptive use among migrant women with a history of induced abortion in Finland. Eur J Contracept Reprod Health Care Off J Eur Soc Contracept. 2018;23(4):274–81.
Khin YP, Nawa N, Fujiwara T, Surkan PJ. Access to contraceptive services among Myanmar women living in Japan: A qualitative study. Contraception. 2021;104(5):538–46.
Gele AA, Musse FK, Shrestha M, Qureshi S. Barriers and facilitators to contraceptive use among Somali immigrant women in Oslo: A qualitative study. PLoS ONE. 2020;15(3):e0229916.
Gümüş Şekerci Y, Aydın Yıldırım T. The knowledge, attitudes and behaviours of Syrian refugee women towards family planning: Sample of Hatay. Int J Nurs Pract John Wiley Sons Inc 2020;26(4):1–12.
Zhang Y, McCoy EE, Scego R, Phillips W, Godfrey E. A Qualitative Exploration of Somali Refugee Women’s Experiences with Family Planning in the U.S. J Immigr Minor Health. 2020;22(1):66–73.
Che Y, Dusabe-Richards E, Wu S, Jiang Y, Dong X, Li J, et al. A qualitative exploration of perceptions and experiences of contraceptive use, abortion and post-abortion family planning services (PAFP) in three provinces in China. BMC Womens Health. 2017;17(1):113.
Ngum Chi Watts MC, Liamputtong P, Carolan M. Contraception knowledge and attitudes: truths and myths among African Australian teenage mothers in Greater Melbourne, Australia. J Clin Nurs. 2014;23(15–16):2131–41.
Agbemenu K, Volpe EM, Dyer E. Reproductive health decision-making among US-dwelling Somali Bantu refugee women: A qualitative study. J Clin Nurs. 2018;27(17–18):3355–62.
Degni F, Koivusilta L, Ojanlatva A. Attitudes towards and perceptions about contraceptive use among married refugee women of Somali descent living in Finland. Eur J Contracept Reprod Health Care Off J Eur Soc Contracept. 2006;11(3):190–6.
Royer PA, Olson LM, Jackson B, Weber LS, Gawron L, Sanders JN, et al. ‘In Africa, There Was No Family Planning. Every Year You Just Give Birth’: Family Planning Knowledge, Attitudes, and Practices Among Somali and Congolese Refugee Women After Resettlement to the United States. Qual Health Res. 2020;30(3):391–408.
Soin KS, Beldowski K, Bates E, Garcia KP, Naik S, Plumb E, et al. Attitudes Towards Family Planning among Bhutanese, Burmese, and Iraqi Refugee Women: A Qualitative Study. Hawaii J Health Soc Welf. 2020;79(6 Suppl 2):70–7.
Chalmiers MA, Karaki F, Muriki M, Mody SK, Chen A, Thiel de Bocanegra H. Refugee women’s experiences with contraceptive care after resettlement in high-income countries: A critical interpretive synthesis. Contraception. 2022;108:7–18.
World Health Organization, United States. Agency for International Development. Programming strategies for postpartum family planning [Internet]. Stratégies de programmation pour la planification familiale du post-partum. Geneva: World Health Organization; 2013. Available from: https://apps.who.int/iris/handle/10665/93680. Cited 30 Nov 2022.
Smith GCS, Pell JP, Dobbie R. Interpregnancy interval and risk of preterm birth and neonatal death: retrospective cohort study. BMJ. 2003;327(7410):313.
Conde-Agudelo A, Rosas-Bermúdez A, Kafury-Goeta AC. Birth Spacing and Risk of Adverse Perinatal OutcomesA Meta-analysis. JAMA. 2006;295(15):1809–23.
Trussell J, Henry N, Hassan F, Prezioso A, Law A, Filonenko A. Burden of unintended pregnancy in the United States: potential savings with increased use of long-acting reversible contraception. Contraception. 2013;87(2):154–61.
Cope AG, Mara KC, Weaver AL, Casey PM. Postpartum Contraception Usage Among Somali Women in Olmsted County. Minnesota Obstet Gynecol. 2019;133(4):762–9.
Funkhouser S, Bullard KA, Hersh AR, Greiner KS, Rodriguez MI. Postpartum Care Utilization Among Emergency Medicaid Recipients. J Immigr Minor Health. 2021;23(5):1121–5.
Potter JE, Hubert C, White K. The Availability and Use of Postpartum LARC in Mexico and Among Hispanics in the United States. Matern Child Health J. 2017;21(9):1744–52.
Yee L, Simon M. Urban minority women’s perceptions of and preferences for postpartum contraceptive counseling. J Midwifery Womens Health. 2011;56(1):54–60.
Cameron ST, Craig A, Sim J, Gallimore A, Cowan S, Dundas K, et al. Feasibility and acceptability of introducing routine antenatal contraceptive counselling and provision of contraception after delivery: the APPLES pilot evaluation. BJOG Int J Obstet Gynaecol. 2017;124(13):2009–15.
Cavallaro FL, Benova L, Owolabi OO, Ali M. A systematic review of the effectiveness of counselling strategies for modern contraceptive methods: what works and what doesn’t? BMJ Sex Reprod Health. 2020;46(4):254–69.
Reyes-Martí L, Rubio-Rico L, Ortega-Sanz L, Raigal-Aran L, de la Flor-López M, Roca-Biosca A, et al. Contraceptive counselling experiences in Spain in the process of creating a web-based contraceptive decision support tool: a qualitative study. Reprod Health. 2021;18(1):1–17.
EmtellIwarsson K, Larsson EC, Bizjak I, Envall N, Kopp Kallner H, Gemzell-Danielsson K. Long-acting reversible contraception and satisfaction with structured contraceptive counselling among non-migrant, foreign-born migrant and second-generation migrant women: evidence from a cluster randomised controlled trial (the LOWE trial) in Sweden. BMJ Sex Reprod Health. 2022;48(2):128–36.
Kolak M, Löfgren C, Hansson SR, Rubertsson C, Agardh A. Immigrant women’s perspectives on contraceptive counselling provided by midwives in Sweden - a qualitative study. Sex Reprod Health Matters. 2022;30(1):2111796.
Coleman-Minahan K, Potter JE. Quality of postpartum contraceptive counseling and changes in contraceptive method preferences(). Contraception. 2019;100(6):492–7.
Åkerman E, Larsson EC, Essén B, Westerling R. A missed opportunity? Lack of knowledge about sexual and reproductive health services among immigrant women in Sweden. Sex Reprod Healthc. 2019;19:64–70.
Larsson EC, Fried S, Essén B, Klingberg-Allvin M. Equitable abortion care - A challenge for health care providers. Experiences from abortion care encounters with immigrant women in Stockholm, Sweden. Sex Reprod Healthc Off J Swed Assoc Midwives. 2016;10:14–8.
Newbold KB, Willinsky J. Providing family planning and reproductive healthcare to Canadian immigrants: perceptions of healthcare providers. Cult Health Sex. 2009;11(4):369–82.
Degni F, Suominen S, Essén B, El Ansari W, Vehviläinen-Julkunen K. Communication and Cultural Issues in Providing Reproductive Health Care to Immigrant Women: Health Care Providers’ Experiences in Meeting Somali Women Living in Finland...[corrected] [published erratum appears in J IMMIGRANT MINORITY HEALTH 2012; 04(2):344]. J Immigr Minor Health. 2012 Apr;14(2):330–43.
Walker SH, Hooks C, Blake D. The views of postnatal women and midwives on midwives providing contraceptive advice and methods: a mixed method concurrent study. BMC Pregnancy Childbirth. 2021;21(1):411.
Otero-Garcia L, Goicolea I, Gea-Sánchez M, Sanz-Barbero B. Access to and use of sexual and reproductive health services provided by midwives among rural immigrant women in Spain: midwives’ perspectives. Glob Health Action. 2013;8(6):22645.
Kolak M, Jensen C, Johansson M. Midwives’ experiences of providing contraception counselling to immigrant women. Sex Reprod Healthc Off J Swed Assoc Midwives. 2017;12:100–6.
Magge H, Nahimana E, Mugunga JC, Nkikabahizi F, Tadiri E, Sayinzoga F, et al. The All Babies Count Initiative: Impact of a Health System Improvement Approach on Neonatal Care and Outcomes in Rwanda. Glob Health Sci Pract. 2020;8(3):505–17.
Nahimana E, Magge H, Bizimana F, Nyishime M, Lively CT, Gilbert H, et al. Sustainability Assessment of a District-Wide Quality Improvement on Newborn Care Program in Rural Rwanda: A Mixed-Method Study. Ann Glob Health. 2021;87(1):40.
Madeira AD, Rangen CM, Avery MD. Design and Implementation of a Group Prenatal Care Model for Somali Women at a Low-Resource Health Clinic. Nurs Womens Health. 2019;23(3):224–33.
Kilander H, Brynhildsen J, Alehagen S, Fagerkrantz A, Thor J. Collaboratively seeking to improve contraceptive counselling at the time of an abortion: a case study of quality improvement efforts in Sweden. BMJ Sex Reprod Health. 2019;45(3):190–9.
Kilander H, Brynhildsen J, Alehagen S, Thor J. Examining the pace of change in contraceptive practices in abortion services - a follow-up case study of a quality improvement collaborative. BMC Health Serv Res. 2020;20(1):948.
Vaughn L, Jacquez F, Lindquist-Grantz R, Parsons A, Melink K. Immigrants as Research Partners: A Review of Immigrants in Community-Based Participatory Research (CBPR). J Immigr Minor Health. 2017;19(6):1457–68.
Wallerstein NB, Duran B. Using Community-Based Participatory Research to Address Health Disparities. Health Promot Pract. 2006;7(3):312–23.
Goodwin L, Skrybant M, Kenyon S. Involving and engaging pregnant women in maternity-related research: reflections on an innovative approach. Res Involv Engagem. 2021;7(1):90.
Ward ME, De Brún A, Beirne D, Conway C, Cunningham U, English A, et al. Using Co-Design to Develop a Collective Leadership Intervention for Healthcare Teams to Improve Safety Culture. Int J Environ Res Public Health. 2018;15(6):1182.
Kilo CM. A framework for collaborative improvement: lessons from the Institute for Healthcare Improvement’s Breakthrough Series. Qual Manag Health Care. 1998;6(4):1–13.
Kilander H, Weinryb M, Vikström M, Petersson K, Larsson EC. Developing contraceptive services for immigrant women postpartum - a case study of a quality improvement collaborative in Sweden. BMC Health Serv Res. 2022;22(1):556.
Batalden M, Batalden P, Margolis P, Seid M, Armstrong G, Opipari-Arrigan L, et al. Coproduction of healthcare service. BMJ Qual Saf. 2016;25:509–17.
Bate P, Robert G. Experience-based design: from redesigning the system around the patient to co-designing services with the patient. Qual Saf Health Care. 2006;15(5):307–10.
Peterson A, Gudbjornsdottir S, Lofgren UB, Schioler L, Bojestig M, Thor J, et al. Collaboratively improving diabetes Care in Sweden Using a National Quality Register: successes and challenges-a case study. Qual Manag Health Care. 2015;24(4):212–21.
Peterson A, Hanberger L, Akesson K, Bojestig M, AnderssonGare B, Samuelsson U. Improved results in paediatric diabetes care using a quality registry in an improvement collaborative: a case study in Sweden. PLoS ONE. 2014;9(5):e97875.
The Statistics Authority: Births and deaths by gender and country of birth 1970–2021 and projection 2022–2070. https://www.scb.se/hitta-statistik/statistik-efter-amne/befolkning/befolkningsframskrivningar/befolkningsframskrivningar/pong/tabell-och-diagram/fodda-och-doda-efter-kon-och-fodelseland-samt-framskrivning/#:~:text=I%20takt%20med%20att%20det,barnen%20en%20utrikes%20f%C3%B6dd%20mamma. Accessed 21 Feb 2023.
The Statistics Authority: Uppväxtvillkor för barn med utländsk bakgrund. https://www.scb.se/contentassets/ed22f1c0a03e4ee199bad44cc32162e0/le0102_2020a01_br_be51br2003.pdf. Accessed 21 Feb 2023.
Swedish gynaecologists and obstetricians within the Swedish Medical Association: Maternal health care, Sexual and Reproductive health. 2008, revised 2016. https://www.sfog.se/natupplaga/ARG76web4a328b70-0d76-474e-840e-31f70a89eae9.pdf. Accessed 25 Feb 2023.
The Swedish medical products agency: Anticonception-treatment recommendation. 2014;25(2):14–28. https://www.lakemedelsverket.se/sv/behandling-och-forskrivning/behandlingsrekommendationer/sok-behandlingsrekommendationer/preventivmetoder-for-antikonception--behandlingsrekommendation. Accessed 25 Feb 2023.
Graviditetsregistret: Statistics of the Pregnancy Registry. 2021. https://www.medscinet.com/gr/resultat.aspx. Accessed 25 Feb 2023.
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–81.
Langley GJ, Moen R, Nolan KM, Nolan TW, Norman CL, Provost LP. The improvement guide : a practical approach to enhancing organizational performance. 2nd ed. San Francisco: Jossey-Bass; 2009.
Berwick DM. A primer on leading the improvement of systems. BMJ. 1996;312(7031):619–22.
Radl-Karimi C, Nicolaisen A, Sodemann M, Batalden P, von Plessen C. Under what circumstances can immigrant patients and healthcare professionals co-produce health? - an interpretive scoping review. Int J Qual Stud Health Well-being. 2020;15(1):1838052.
McInnes RJ, Aitken-Arbuckle A, Lake S, Hollins Martin C, MacArthur J. Implementing continuity of midwife carer - just a friendly face? A realist evaluation. BMC Health Serv Res. 2020;20(1):304.
Ali P, Rogers M. Use of Personas and Participative Methods When Researching with Hard-to-Reach Groups. In: Hinsliff-Smith K, McGarry J, Ali P, editors. Arts Based Health Care Research: A Multidisciplinary Perspective [Internet]. Cham: Springer International Publishing; 2022:41–50. Available from: https://doi.org/10.1007/978-3-030-94423-0_4
Chan AW, Tetzlaff JM, Altman DG, Laupacis A, Gøtzsche PC, Krleža-Jerić K, et al. SPIRIT 2013 Statement: Defining Standard Protocol Items for Clinical Trials. Ann Intern Med. 2013;158(3):200–7.
Chan AW, Tetzlaff JM, Gøtzsche PC, Altman DG, Mann H, Berlin JA, et al. SPIRIT 2013 explanation and elaboration: guidance for protocols of clinical trials. BMJ. 2013;9(346):e7586.
Dehlendorf C, Henderson JT, Vittinghoff E, Steinauer J, Hessler DJC. Development of a patient-reported measure of the interpersonal quality of family planning care. Contraception. 2018;97(1):34–40.
EmtellIwarsson K, Envall N, Bizjak I, Bring J, Kopp Kallner H, Gemzell-Danielsson K. Increasing uptake of long-acting reversible contraception with structured contraceptive counselling: cluster randomised controlled trial (the LOWE trial). BJOG. 2021;128(9):1546–54.
StataCorp. Stata Statistical Software: Release 17. College Station, TX: StataCorp LLC; 2021.
Moore GF, Audrey S, Barker M, Bond L, Bonell C, Hardeman W, et al. Process evaluation of complex interventions: Medical Research Council guidance. BMJ. 2015;19(350):h1258.
Braun V, Clarke V. Thematic analysis : a practical guide. Los Angeles: SAGE; 2022.
Filler T, Benipal PK, Torabi N, Minhas RS. A chair at the table: a scoping review of the participation of refugees in community-based participatory research in healthcare. Glob Health. 2021;17(1):103.
Wells S, Tamir O, Gray J, Naidoo D, Bekhit M, Goldmann D. Are quality improvement collaboratives effective? A systematic review BMJ Qual Saf. 2018;27(3):226–40.
Schouten LMT, Hulscher MEJL, van Everdingen JJE, Huijsman R, Grol RPTM. Evidence for the impact of quality improvement collaboratives: systematic review. BMJ. 2008;336(7659):1491–4.
Zamboni K, Baker U, Tyagi M, Schellenberg J, Hill Z, Hanson C. How and under what circumstances do quality improvement collaboratives lead to better outcomes? A systematic review. Implement Sci. 2020;15(1):27.
Acknowledgements
The authors wish to thank Prof. Glenn Robert, King’s College London for constructive support in developing the co-design methodology.
Funding
Open access funding provided by Karolinska Institute. This study was funded by grants from Forte (reference number 2021–00261) and The Swedish Research Council (reference number 2020–01121). The funders had no role in the study design, data collection or analysis, the decision to publish or preparation of the manuscript. Forte is a Swedish research council for health, working life, welfare and a government agency under the Swedish Ministry of Health and Social Affairs. Forte is the major funder for this project.
Author information
Authors and Affiliations
Contributions
EL, HK, KGD, JT, KP, GB designed the project. RS, HK, EL, SB, GB, AW, KP, KGD, KEI participated in protocol writing. All authors reviewed the manuscript. All authors read and approved the final version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study is conducted in keeping with the principles for research ethics according to the Helsinki Declaration, including written informed consent by all participants and protection of the integrity and dignity of individuals. The study was approved by the Regional Ethical Review Committee in Sweden. The reference number is 2021–05962-01.
Consent for publication
Not applicable.
Competing interests
HK reports consulting fees from Bayer AB and Campus Pharma for giving lectures or running educational events. KEI reports payment or honoraria for presentation from Bayer AB and for travel support for presentation at conference from RemovAid AS.KGD reports consulting fees from Bayer, MSD, Organon, Gedeon Richter, Mithra, Exeltis, MedinCell, Cirqle, Natural Cycles, Exelgyn, Campus Pharma, HRA-Pharma; payment or honoraria for lectures, presentations, speakers bureaus, manuscript writing or educational events from Bayer, MSD, Organon, Gedeon Richter, Mithra, Exeltis, Exelgyn, Campus Pharma; participation on a Data Safety Monitoring Board or Advisory Board: Gedeon Richter, Bayer; leadership or fiduciary role in other board, society, committee or advocacy group, paid or unpaid: FIGO, WHO HRP/SRH, ESC, FIAPAC, FSRH/RCOG UK, Population Council.The other co-authors have stated that they have no conflicts of interest in connection with this manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kilander, H., Sorcher, R., Berglundh, S. et al. IMplementing best practice post-partum contraceptive services through a quality imPROVEment initiative for and with immigrant women in Sweden (IMPROVE it): a protocol for a cluster randomised control trial with a process evaluation. BMC Public Health 23, 806 (2023). https://doi.org/10.1186/s12889-023-15776-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-023-15776-8