Abstract
Introduction
Educational attainment is an important social determinant of health (SDOH) for cardiovascular disease (CVD). However, the association between educational attainment and all-cause and CVD mortality has not been longitudinally evaluated on a population-level in the US, especially in individuals with atherosclerotic cardiovascular disease (ASCVD). In this nationally representative study, we assessed the association between educational attainment and the risk of all-cause and cardiovascular (CVD) mortality in the general adult population and in adults with ASCVD in the US.
Methods
We used data from the 2006–2014 National Death Index-linked National Health Interview Survey for adults ≥ 18 years. We generated age-adjusted mortality rates (AAMR) by levels of educational attainment (< high school (HS), HS/General Education Development (GED), some college, and ≥ College) in the overall population and in adults with ASCVD. Cox proportional hazards models were used to examine the multivariable-adjusted associations between educational attainment and all-cause and CVD mortality.
Results
The sample comprised 210,853 participants (mean age 46.3), representing ~ 189 million adults annually, of which 8% had ASCVD. Overall, 14.7%, 27%, 20.3%, and 38% of the population had educational attainment < HS, HS/GED, Some College, and ≥ College, respectively. During a median follow-up of 4.5 years, all-cause age-adjusted mortality rates were 400.6 vs. 208.6 and 1446.7 vs. 984.0 for the total and ASCVD populations for < HS vs ≥ College education, respectively. CVD age adjusted mortality rates were 82.1 vs. 38.7 and 456.4 vs 279.5 for the total and ASCVD populations for < HS vs ≥ College education, respectively. In models adjusting for demographics and SDOH, < HS (reference = ≥ College) was associated with 40–50% increased risk of mortality in the total population and 20–40% increased risk of mortality in the ASCVD population, for both all-cause and CVD mortality. Further adjustment for traditional risk factors attenuated the associations but remained statistically significant for < HS in the overall population. Similar trends were seen across sociodemographic subgroups including age, sex, race/ethnicity, income, and insurance status.
Conclusions
Lower educational attainment is independently associated with increased risk of all-cause and CVD mortality in both the total and ASCVD populations, with the highest risk observed for individuals with < HS education. Future efforts to understand persistent disparities in CVD and all-cause mortality should pay close attention to the role of education, and include educational attainment as an independent predictor in mortality risk prediction algorithms.
Similar content being viewed by others
Introduction
Atherosclerotic cardiovascular disease (ASCVD) is the leading cause of death in the US [1]. While traditional risk factors for ASCVD have been extensively researched [2], socioeconomic and contextual factors which shape cardiovascular health – directly and indirectly – are less well studied [3]. Collectively, these factors are known as social determinants of health (SDOH) [3, 4]. Unfavorable SDOH have been shown to increase the risk of poor health outcomes – including CVD – with recent evidence suggesting that social disadvantage may increase the risk of all-cause mortality, independent of demographics or clinical risk factors [5].
Educational attainment is an important SDOH and a reliable measure of socioeconomic status. Lower educational attainment has a well-established association with higher risk of ASCVD [6,7,8,9] and is inversely associated with all-cause and cardiovascular disease (CVD) mortality, with higher educational attainment associated with lower mortality rates [10,11,12,13,14,15]. The magnitude of lower educational attainment or less than high school education has been associated with higher all-cause and cardiovascular mortality in several studies [16].
However, relatively little is known about the longitudinal impact of educational attainment on all-cause and CVD mortality specifically in the United States, particularly at the population level and using most contemporary data. Also, when evaluating the education-mortality association, prior studies typically performed a partial adjustment for confounders and sociodemographic factors and only a few assessed the potential mediation role of CVD risk factors, thereby preventing a full appreciation of the impact education has on mortality [5, 10,11,12,13,14,15]. Finally, few studies have evaluated these associations specifically among individuals with ASCVD [10,11,12], which remains the number one cause of death in the US.
Our aim was to conduct a large-scale, nationally representative study assessing the association between varying levels of educational attainment and all-cause and CVD mortality in the general US adult population, and specifically among individuals with ASCVD, over a 10-year period. We also aimed to assess these associations specifically across relevant sociodemographic subgroups.
Methods
Research design and study population
Our study included individuals ≥ 18 years of age from the 2006–2014 National Health Interview Survey (NHIS), an annual multistage survey conducted in the civilian non-institutionalized population of the United States. Details on survey design and information is available from https://www.cdc.gov/nchs/nhis/1997-2018.htm [17]. Data for adults who completed the surveys between 2006–2014 was linked to the National Death Index (NDI) through December 2015. The NDI is a centralized database of US death record information and includes detailed data on underlying cause of death. The following identifiers were used to link NDI to NHIS: social security number, first name, last name, father’s surname, month/day/year of birth, sex, race, state/country of birth, and residence [17]. We excluded individuals with missing data on NDI linkage (ineligible for NDI linkage), education, income, and other/unidentified racial/ethnic category.
Research ethics
This research does not contain Human Subjects. Due to the de-identified nature and public availability of NHIS data, this study was exempt from review by the institutional review board of Houston Methodist. No administrative approval was needed to access the raw data as it is publicly available. All data was anonymized prior to use in this study.
Study exposure
Our exposure variable, self-reported educational attainment, was categorized as a 4-level ordinal variable: (1) no high school diploma (< HS), (2) HS diploma or general education development equivalent (HS/GED), (3) some college, and (4) at least one college degree (≥ college).
Ascertainment of baseline ASCVD
Respondents with an affirmative answer to at least one of the following items were deemed to have ASCVD: “Have you ever been told by a doctor or other health professional that you had coronary heart disease…angina or angina pectoris…a heart attack (also called a myocardial infarction) …a stroke?”. This information was used to define the ASCVD subpopulation as a binary “yes/no” variable.
Outcomes
Two outcomes of interest were evaluated: all-cause and CVD mortality. For decedents, mortality type (all-cause and CVD morality) was ascertained using death certificate records of the International Classification of Disease (ICD) codes for the primary cause of death. All-cause mortality was death due to any cause. CVD mortality was defined as death with CVD (I00-I09, I11, I13, I20-I51) as the primary cause of death.
Other relevant variables
Other study variables used in our analyses included age categories (18–39, 40–64, ≥ 65 years) [18, 19], sex (men, women), race/ethnicity (non-Hispanic White [NHW], non-Hispanic Black [NHB], and Hispanic), cardiovascular risk factors, family income (high, middle, low, and lowest income) and insurance type (uninsured, private insurance, or public insurance) these were included as covariates. Cardiovascular risk factors included hypertension, diabetes, obesity (body mass index ≥ 30 kg/m2), current smoking status, and insufficient physical activity. Insufficient physical activity included any of: < 150 min per week of moderate-intensity aerobic physical activity; < 75 min per week of vigorous-intensity aerobic physical activity, or < 150 min per week of moderate to vigorous-intensity aerobic physical activity. Family income was categorized based on the percentage of family income relative to the federal poverty limit from the US Census Bureau, i.e., high income (≥ 400%) of FPL, middle income (200%– < 400%), low income (125%– < 200%), and lowest income (< 125%) of FPL.
Statistical analysis
We reported the descriptive characteristics of the sample by educational attainment and compared the differences in these statistics with chi-squared tests. We generated weighted proportions of participant characteristics by levels of educational attainment to obtain nationally representative estimates.
We reported age-adjusted mortality rates (AAMR) per 100,000 person-years with 95% confidence intervals, by levels of educational attainment, using Poisson regression models. We examined two outcomes: all-cause and CVD mortality. First, we reported AAMRs for each mortality outcome in the total population. Second, we reported AAMRs in adults with ASCVD.
Kaplan–Meier survival curves were used to plot survival by levels of educational attainment during the 10 years of follow-up. Multivariable Cox proportional hazards models were used to examine the association between educational attainment and all-cause and CVD mortality separately in the total population and in adults with ASCVD. Four models were tested: Model 1: unadjusted; Model 2: adjusted for age, sex and race/ethnicity; Model 3: adjusted for Model 2 + insurance and income; Model 4: adjusted for Model 3 + traditional cardiovascular risk factors (hypertension, diabetes, obesity (body mass index ≥ 30 kg/m2), current smoking status, and insufficient physical activity).
Results
Our final sample consisted of 210,853 adults, representing 189 million annualized US adults. Descriptive characteristics of the study population are summarized in Table 1. Overall, 14.7%, 27%, 20.3%, and 38% of the population had < HS, HS/GED, some college, and ≥ college respectively. Participants with ≥ college degree were more likely to be female, non-Hispanic White, and have a lower burden of CVD risk factors than those with < HS education. Conversely, participants with < HS education were more likely to belong to families with low income and have no health insurance coverage.
Age-Adjusted Mortality Rates
AAMRs for all-cause and CVD mortality by educational attainment after a median follow-up duration of 4.5 years (IQR: 2.5–6.4) are presented in Fig. 1 (panels A and B) and Supplementary Table S3, Additional file 1. AAMRs increased with decreasing educational attainment in the total population (Fig. 1A) and the ASCVD population (Fig. 1B). All-cause and CVD AAMRs were approximately twofold higher for < HS vs. ≥ College in the total population and 1.5 to twofold higher in the ASCVD population. AAMRs for < HS vs. ≥ College in the total population were 400 vs. 209 and 82 vs. 39 per 100,000 person-years (PYs) for all-cause and CVD mortality, respectively. All-cause and CVD AAMRs for < HS vs. ≥ College were 1447 vs. 984 and 456 vs. 280 per 100,000 PY in the ASCVD population. The observed education-mortality patterns (i.e., increasing mortality rates with lower education attainment) were similar among individuals in the total and ASCVD population.
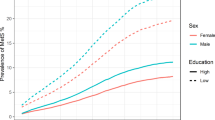
Findings from the Kaplan Meier analysis are shown in Fig. 2. We found a positive association between educational attainment and 10-year survival for all population subgroups and mortality types. Ten-year survival rates for < HS vs. ≥ College were 94% vs. 83% and 99% vs. 96%, respectively for all-cause and CVD mortality in the total population. Survival rates were the lowest in the ASCVD population for all-cause mortality for < HS vs. ≥ College (53% vs 75%).
Multivariable-adjusted analyses
Results from multivariable regression are shown in Table 2. In models adjusted for age, sex, race/ethnicity, income, and insurance status (Model 3), participants with < HS had 1.4-fold (HR = 1.39; [95% CI 1.29, 1.50]) and 1.5-fold (HR = 1.51; 95% CI 1.26, 1.81) higher risk of all-cause and CVD mortality, in the total population, relative to those with ≥ College. Similar patterns were seen for the ASCVD population. In the ASCVD population, participants with < HS had 1.2-fold (HR = 1.21; 95% CI 1.06, 1.38) and 1.4-fold (HR = 1.38; 95% CI 1.04, 1.82) higher risk of all-cause and CVD mortality relative to those with ≥ College. Important to note, the education-mortality association was only statistically significant for < HS (compared to other educational attainment levels) for all-cause and CVD mortality in the ASCVD population and CVD mortality in the total population.
The education-mortality association was relatively stronger in the total population than the ASCVD population, with relatively higher HR for < HS (vs. ≥ College) for all-cause and CVD mortality. However, the education-mortality association was not statistically significant for other educational attainment levels in both the total and ASCVD populations. The observed association was attenuated after adjusting for CVD risk factors (Model 4) in the total population and was not statistically significant in the ASCVD population for < HS (vs. ≥ College).
Subgroup analyses
We found similar patterns of higher mortality risk with lower educational attainment across demographic groups (age, sex, and race/ethnicity) (Supplementary Tables S1-S2, Additional file 1). In the supplementary analyses, we consistently found higher mortality risk associated with lower educational attainment across age, sex and race/ethnicity strata. Consistent with prior literature, AAMRs were higher for males and NHB, compared to females and NHW/Hispanic, respectively. Overall, the observed association between educational attainment and mortality was relatively stronger in the non-elderly, females and NHB subgroups, compared to their counterparts.
Discussion
To our knowledge, this is the largest nationally representative study evaluating the longitudinal impact (approximately 10 years) of educational attainment on all-cause and CVD mortality in the general adult population and adults with ASCVD in the US. We also reported the education-mortality association across key sociodemographic subgroups including age, sex, and race/ethnicity strata. We observed an inverse relationship between educational attainment and risk of all-cause and CVD in both the total and ASCVD populations. Education < HS was associated with up to 1.2 to 1.5-fold higher risk of all mortality types compared to ≥ College for both total and ASCVD populations when adjusted for age, sex, race/ethnicity, income, and insurance status. Similar patterns were seen across age, sex, and race/ethnicity strata. Education < HS was associated with up to 1.4 to 1.5-fold and 1.2 to 1.4-fold higher risk of all mortality types compared to ≥ College in the total population and ASCVD population, respectively, when adjusted for insurance and income (Model 3). Upon further adjustment for CVD risk factors (Model 4), the education-mortality associations were attenuated in the total population and not statistically significant in the ASCVD population for all-cause and CVD mortality.
Education-mortality gradient: influential factors
Based on prior studies, lower educational attainment is associated with lower life expectancy and higher mortality [10,11,12,13,14,15], especially in those with ASCVD [7, 20]. However, the effect of educational attainment on mortality is multi-factorial. First, lower educational attainment is associated with lower health literacy [20,21,22,23]. Health literacy provides individuals a better understanding and utilization of public health and preventive CVD recommendations and has been associated with improved health behaviors. Better health literacy has been associated with health behaviors such as smoking cessation, healthy food consumption and greater adherence to dietary and physical activity guidelines, which lead to less health care demand and potentially better quality of life[20,21,22,23].Better health behaviors, especially reduction in smoking have been shown to improve all-cause and CVD mortality [20, 21]. Second, income and access to care are associated with educational attainment and mortality; those with higher income and educational attainment have better access to care and lower mortality rates [22]. Third, age and racial disparities may pose socioeconomic challenges in obtaining higher educational attainment and insurance and access to care (discussed below). There are other hypothesized mechanisms via which educational attainment may impact mortality that are poorly defined and require further investigation.
In our study, the education-mortality gradient was stronger in the total vs. the ASCVD population, with higher HRs at nearly each level of educational attainment in the former group when adjusting for age, sex, and race/ethnicity (Model 2). It is possible the education-mortality association was diminished in the presence of ASCVD as there is a higher risk at baseline independent of other factors, so that the influence of an upstream factor such as education is slightly diminished. After adjusting for insurance and income (Model 3), the gradient was more attenuated in the total population compared to the ASCVD population, suggesting educational attainment has a stronger impact on mortality in the ASCVD population vs. the total population. The education-mortality association was further diminished in the total population and not statistically significant in the ASCVD population after adjusting for CVD risk factors (Model 4). These results are expected as there may be a higher risk present at baseline independent of other factors in the ASCVD population vs the total population in addition to CVD risk factors being established clinical predictors of CVD [5, 6, 10]. Another factor that likely contributed to the confidence interval including the null value is the much smaller number of participants in this subgroup, which resulted in less statistical precision compared with the total population. Further investigation is needed to better understand the association of education attainment with mortality among individuals with established ASCVD, especially as it relates to preventive care (e.g., lifestyle interventions, medical therapies, access to healthcare) and overall comorbidity burden.
Trends in demographic subgroups: age, sex, and race/ethnicity
The educational-mortality association was consistent across various sociodemographic subgroups. In the total population, there was a higher risk of all-cause mortality for ages < 40 vs. ≥ 40 after adjusting for SDOH and CVD risk factors (Supplementary Tables S1-S2, Models 3–4, Additional file 1). In the ASCVD population, many of these associations were not statistically significant after adjusting for SDOH and CVD risk factors (Supplementary Tables S1-S2, Models 3–4, Additional file 1).
Population level mortality risk assessments traditionally focus on established risk factors such as clinical indicators of physical and mental health without due attention to key “upstream” SDOH such as educational attainment. Age and associated mortality risk factors such as medical comorbidities, genetics, and cumulative psychosocial stress may alter the effects of educational attainment in late life [24,25,26,27,28]. Further, higher educational attainment is strongly predictive of stable employment, which may improve access to care such as via employer-sponsored health coverage; lower educational attainment and stable employment may restrict access to care and increase the risk of adverse health outcomes including mortality. These effects may be blunted after the age of 65 [29], given access to Medicare and other public benefit programs. Therefore, once accounting for SDOH and CVD risk factors, the education-mortality risk is blunted in ages < 40 in the total population. Unlike ages < 40, which had very few CVD events [30], ages > 65 were observed to have a statistically significant CVD mortality risk in the ASCVD population after adjusting for CVD risk factors, which is expected given multi-morbidity with advanced age and CVD risk factors being clinical predictors of CVD [31].
Regarding sex, the education-mortality association was similar for both men and women in the total population for all-cause and CVD mortality for < HS vs. ≥ College when adjusting for SDOH and CVD risk factors (Supplementary Tables S1-S2, Model 3–4, Additional file 1). However, the impact of educational attainment on all-cause and CVD mortality was relatively more robust in women vs. men in the ASCVD population after adjusting for SDOH and CVD risk factors (Supplementary Table S1-S2, Model 3–4, Additional file 1). Sex differences in education-mortality association may be explained by sex-related risk factors such as pregnancy or hormonal influences, which may affect CV physiology [32, 33] and variable health behaviors, screening practices, and presentations of ASCVD in men and women that may alter diagnosis and management, contributing to adverse CVD outcomes in women [34,35,36,37].”
Similarly, we found a higher mortality risk for non-Hispanic Black compared to other racial/ethnic groups (Supplementary Table S1-S2, Model 2, Additional file 1), consistent with prior studies [37,38,39]. However, after adjusting for SDOH (Model 3), this risk is comparable to NHW. These findings reflect the persistent social adversity faced by racial/ethnic minority populations, suggesting educational attainment may be driven by or contributes to a ‘cumulative’ social burden in explaining the adverse outcomes experienced by the non-Hispanic Black population. Some mechanisms for these disparities may include disproportionate impact of adverse SDOH, including neighborhood disadvantage, housing/overall economic instability, and structural racism such as redlining policies and other forms of racial/ethnic discrimination on socially vulnerable populations, which may restrict access to opportunities for educational attainment and potentially worsen the negative impact of low educational attainment on mortality via increased risk of established CV risk factors such as obesity, diabetes, hypertension and others [40, 41]. Additionally, racial differences between non-Hispanic Black and other races extend to CVD therapies, including treatment of hypertension, coronary artery disease, arrhythmias, and heart failure [42]. As seen in the primary analyses, adjustment for income and insurance in adjusted models attenuated the observed sociodemographic disparities in mortality considerably, further highlighting the importance of cumulative SDOH burden in explaining health disparities by individual socioeconomic predictors. Future studies should focus on further understanding the race-education-mortality association and elucidating the impact of structural inequities such as lack of access to education for racial/ethnic minority subgroups.
Potential approaches to reduce the education-mortality gradient
The factors mentioned above merit further investigation as their effect on the education-mortality association may be unique. These cumulative results necessitate upstream interventions, which can help improve midstream determinants over time to improve educational attainment and reduce mortality rates. Upstream interventions include social reform and public health policies to 1) improve educational attainment by targeting key demographics and SDOH burden to improve CVD and mortality and 2) reduce high risk health behaviors (smoking, drinking, etc.). These interventions will ultimately heighten educational attainment as an important social determinant of mortality and inform evidence-based CVD risk stratification and prevention strategies. Improving access to education by supporting schools and colleges serving socioeconomically disadvantaged subgroups can reduce dropout rates and improve graduation rates, bridging the societal gap in educational attainment with subsequent economic and health outcomes. Therefore, it is important to have policies supporting socially vulnerable communities to facilitate access to education through direct/indirect financial support and incentivizing higher educational attainment with easy access to loans/repayment policies. An example of an upstream intervention includes the 2015 Every Student Succeeds Act, establishing accountability of schools towards creating equitable educational attainment in the United States. While the impact of this bill on educational attainment is yet to be seen, it highlights current policies that can potentially narrow the education-mortality gap [43]. Additionally, there are several programs that support historically black colleges and universities in improving student retention in underserved communities. Examples include the United Negro College Fund and Thurgood Marshall College Fund that provides financial assistance to students, academic/career support services, and institutional development resources [44].
These results prompt the following questions: 1) how can existing, predominantly clinical risk prediction algorithms be remodeled for improved mortality prediction using educational attainment?, 2) how does educational attainment interact with other SDOH such as income, healthcare/barriers to care, neighborhood environment, and community/social context such as social support mechanisms to impact mortality risk?, and 3) from a policy standpoint, are there evidence-based interventions aiding the US population in mitigating the education-mortality gap? Based on the existing AHA/ACC guidelines for preventative cardiology [45], educational attainment is not a targeted SDOH for CVD; however, we hope this study attracts greater attention towards the education-mortality relationship in the ASCVD population. Our results may inform future interventions targeting educational attainment in CVD prevention frameworks – both from a health literacy standpoint and via greater advocacy efforts for increased access to educational attainment to improve population cardiovascular health.
Strengths
This study is the most recent, large-scale, longitudinal assessment of the association between educational attainment and all-cause and CVD mortality using a disaggregated 4-level educational attainment variable. Ours is the one of the few population-based, national studies to report the risk of both all-cause and CVD mortality associated with varying levels of educational attainment in the general US adult population, and in adults with ASCVD. Other major strengths include a large sample size with statistically robust estimates, longitudinal analysis of the educational attainment effect over a 10-year follow up period, a disaggregated 4-level educational attainment variable, and the analyses stratified by major sociodemographic factors (age, sex, and race/ethnicity) and other SDOH (insurance and income).
Limitations
Our study is not without limitations. Other racial/ethnic subgroups (Asian, native Americans, etc.) were not included in the analysis given small available sample sizes and potentially underpowered and non-representative mortality analyses (especially for CVD mortality) for these population subgroups in the NHIS database. Additionally, while higher risk of mortality is associated with lower educational attainment with regional/geographic variation [46, 47], assessment of regional variation in the education-mortality gradient was outside the scope of our study. Given the self-reported nature of the data, there is potential for under-reporting and misclassification. The prevalence of low educational attainment is likely to be under-estimated, potentially resulting in a bias of our estimates towards the null. Despite these expected limitations of survey datasets, the NHIS remains a reliable source of information on the health of the non-institutionalized US population and has been used extensively in social epidemiology and health outcomes research previously [48, 49]. However, the NDI has been previously shown to overrepresent CVD mortality [50]. Despite this limitation, the NDI remains the most reliable source of information for mortality for large national studies such as the NHIS and National Health and Nutrition Examination Survey (NHANES). Lastly, these results do not provide causal mechanisms for the relationship between educational attainment and mortality but indicate pathways to be investigated in future studies.
Conclusions
Lower educational attainment is strongly associated with all-cause and CVD mortality in the total and ASCVD populations in the US. Despite some variation, the impact of low educational attainment on mortality risk is seen consistently across sociodemographic strata. Our study suggests that enhanced upstream interventions to improve access to high quality education in the US may have a significant impact on life expectancy. Future efforts to understand persistent disparities in CVD and all-cause mortality should pay close attention to the role of education, and include educational attainment as an independent predictor in mortality risk prediction algorithms.
Availability of data and materials
The datasets generated and analyzed during the current study are available in the National Health Institute (https://www.cdc.gov/nchs/nhis/data-questionnaires-documentation.htm).
Abbreviations
- AAMR:
-
Age-adjusted mortality rates
- ASCVD:
-
Atherosclerotic cardiovascular disease
- CVD:
-
Cardiovascular disease
- ICD:
-
International Classification of Disease
- NDI:
-
National Death Index
- NHIS:
-
National Health Interview Survey
References
Tsao CW, Aday AW, Almarzooq ZI, et al. Heart disease and stroke statistics—2022 update: a report from the american heart association. Circulation. 2022;145(8):e153-639. https://doi.org/10.1161/cir.0000000000001052.
Roth GA, Mensah GA, Johnson CO, et al. Global burden of cardiovascular diseases and risk factors, 1990–2019: update from the GBD 2019 study. J Am Coll Cardiol. 2021;77(15):1958–9. https://doi.org/10.1016/j.jacc.2020.11.010. J Am Coll Cardiol. 2020;76(25):2982-3021.
Havranek EP. American heart association council on quality of care and outcomes research, council on epidemiology and prevention, council on cardiovascular and stroke nursing, council on lifestyle and cardiometabolic health, and stroke council. Social determinants of risk and outcomes for cardiovascular disease: a scientific statement from the American heart association. Circulation. 2015;132(9):873–98. https://doi.org/10.1161/CIR.0000000000000228.
Commission on Social Determinants of Health. Closing the gap in a generation: health equity through action on the social determinants of health: final report of the Commission on Social Determinants of Health. 2008. https://www.who.int/social_determinants/thecommission/finalreport/en/. Accessed 30 Nov 2019.
Javed Z, Valero-Elizondo J, Khan SU, et al. cumulative social disadvantage and all-cause mortality in the United States: findings from a national study. Popul Health Manag. 2022;25(6):789–97. https://doi.org/10.1089/pop.2022.0184.
Rosengren A, et al. Socioeconomic status and risk of cardiovascular disease in 20 low-income, middle-income, and high-income countries: the Prospective Urban Rural Epidemiologic (PURE) study. Lancet Glob Health. 2019;7(6):e748–60. https://doi.org/10.1016/S2214-109X(19)30045-2. Epub 2019 Apr 23 PMID: 31028013.
Baldi I, Costa G, Foltran F, et al. Effect of educational attainment on incidence and mortality for ischemic heart and cerebrovascular diseases: a systematic review and trend estimation. Int J Cardiol. 2013;168(5):4959–63.
Meara ER, Richards S, Cutler DM. The gap gets bigger: changes in mortality and life expectancy, by education, 1981-2000. Health Aff (Millwood). 2008;27:350–60. https://doi.org/10.1377/hlthaff.27.2.350.
Hamad R, Nguyen TT, Bhattacharya J, Glymour MM, Rehkopf DH. Educational attainment and cardiovascular disease in the United States: a quasi-experimental instrumental variables analysis. PLoS Med. 2019;16(6):e1002834. https://doi.org/10.1371/journal.pmed.1002834. Published 2019 Jun 25.
Kubota Y, Heiss G, MacLehose RF, Roetker NS, Folsom AR. Association of educational attainment with lifetime risk of cardiovascular disease: the atherosclerosis risk in communities study. JAMA Intern Med. 2017;177:1165–72.
Kelli HM, Mehta A, Tahhan AS, et al. low educational attainment is a predictor of adverse outcomes in patients with coronary artery disease. J Am Heart Assoc. 2019;8(17):e013165. https://doi.org/10.1161/jaha.119.013165.
Choi AI, Weekley CC, Chen S-C, et al. Association of educational attainment with chronic disease and mortality: the Kidney Early Evaluation Program (KEEP). Am J Kidney Dis. 2011;58(2):228–34. https://doi.org/10.1053/j.ajkd.2011.02.388.
Sasson I. Diverging trends in cause-specific mortality and life years lost by educational attainment: evidence from United states vital statistics data, 1990–2010. PLoS One. 2016;11(10):e0163412. https://doi.org/10.1371/journal.pone.0163412. Published 2016 Oct 4.
Montez JK, Hummer RA, Hayward MD. Educational attainment and adult mortality in the United States: a systematic analysis of functional form. Demography. 2012;49(1):315–36. https://doi.org/10.1007/s13524-011-0082-8.
Hummer RA, Hernandez EM. The effect of educational attainment on adult mortality in the United States. Popul Bull. 2013;68(1):1–16.
Byhoff E, Hamati MC, Power R, Burgard SA, Chopra V. Increasing educational attainment and mortality reduction: a systematic review and taxonomy. BMC Public Health. 2017;17(1):719. https://doi.org/10.1186/s12889-017-4754-1. Published 2017 Sep 18.
Centers for Disease Control and Prevention. The Linkage of National Center for Health Statistics Survey Data to the National Death Index – 2019 Linked Mortality File (LMF): Linkage Methodology and Analytic Considerations. Published July 8, 2021. Accessed 1 Aug 20201. https://www.cdc.gov/nchs/data/datalinkage/2019NDI-Linkage-Methods-and-Analytic-Considerations-508.pdf
Okunrintemi V, Tibuakuu M, Virani SS, et al. Sex differences in the age of diagnosis for cardiovascular disease and its risk factors among US adults: trends from 2008 to 2017, the Medical Expenditure Panel Survey. J Am Heart Assoc. 2020;9(24):e018764. https://doi.org/10.1161/JAHA.120.018764.
Alam MT, Echeverria SE, DuPont-Reyes MJ, et al. Educational Attainment and Prevalence of Cardiovascular Health (Life’s Simple 7) in Asian Americans. Int J Environ Res Public Health. 2021;18(4):1480. https://doi.org/10.3390/ijerph18041480. Published 2021 Feb 4.
Rogers RG, Hummer RA, Everett BG. Educational differentials in US adult mortality: an examination of mediating factors. Soc Sci Res. 2013;42(2):465–81. https://doi.org/10.1016/j.ssresearch.2012.09.003.
Tan JP, Cheng KKF, Siah RC. A systematic review and meta-analysis on the effectiveness of education on medication adherence for patients with hypertension, hyperlipidaemia and diabetes. J Adv Nurs. 2019;75(11):2478–94.
Loucks EB, Gilman SE, Howe CJ, et al. Education and coronary heart disease risk: potential mechanisms such as literacy, perceived constraints, and depressive symptoms. Health Educ Behav. 2015;42(3):370–9. https://doi.org/10.1177/1090198114560020.
Grossman M. On the concept of Health Capital and the demand for Health. J Polit Econ. 1972;80(2):223–55. https://doi.org/10.7312/gros17812-004.
Kann L, McManus T, Harris WA, Shanklin SL, Flint KH, Queen B, Lowry R, Chyen D, Whittle L, Thornton J, Lim C, Bradford D, Yamakawa Y, Leon M, Brener N, Ethier KA. Youth risk behavior surveillance - United States, 2017. MMWR Surveill Summ. 2018;67(8):1–114. https://doi.org/10.15585/mmwr.ss6708a1.PMID:29902162;PMCID:PMC6002027.
Abraham G, Havulinna AS, Bhalala OG, Byars SG, De Livera AM, Yetukuri L, Tikkanen E, Perola M, Schunkert H, Sijbrands EJ, et al. Genomic prediction of coronary heart disease. Eur Heart J. 2016;37:3267–78.
Slopen N, Goodman E, Koenen KC, Kubzansky LD. Socioeconomic and other social stressors and biomarkers of cardiometabolic risk in youth: a systematic review of less studied risk factors. PLoS ONE. 2013;8:e64418.
Shah NS, Lloyd-Jones DM, Kandula NR, Huffman MD, Capewell S, O’Flaherty M, Kershaw KN, Carnethon MR, Khan SS. Adverse trends in premature cardiometabolic mortality in the United States, 1999 to 2018. J Am Heart Assoc. 2020;9(23):e018213. https://doi.org/10.1161/JAHA.120.018213. Epub 2020 Nov 23. PMID: 33222597; PMCID: PMC7763768.
Chen Y, Freedman ND, Albert PS, Huxley RR, Shiels MS, Withrow DR, Spillane S, Powell-Wiley TM, Berrington de González A. Association of cardiovascular disease with premature mortality in the United States. JAMA Cardiol. 2019;4(12):1230–8. https://doi.org/10.1001/jamacardio.2019.3891. Erratum in: JAMA Cardiol. 2019 Dec 1;4(12):1301. PMID: 31617863; PMCID: PMC6802055.
Krumholz HM, Nuti SV, Downing NS, Normand SL, Wang Y. Mortality, hospitalizations, and expenditures for the medicare population aged 65 years or older, 1999–2013. JAMA. 2015;314(4):355–65. https://doi.org/10.1001/jama.2015.8035. Erratum.In:JAMA.2015Aug25;314(8):837.PMID:26219053;PMCID:PMC5459402.
Centers for Disease Control and Prevention, National Center for Health Statistics. National Vital Statistics System, Mortality 1999–2020 on CDC WONDER Online Database, released in 2021. Data are from the Multiple Cause of Death Files, 1999–2020, as compiled from data provided by the 57 vital statistics jurisdictions through the Vital Statistics Cooperative Program. Accessed at http://wonder.cdc.gov/ucd-icd10.html on Feb 28, 2023 5:12:22 PM
Forman DE, Maurer MS, Boyd C, et al. Multimorbidity in older adults with cardiovascular disease. J Am Coll Cardiol. 2018;71(19):2149–61. https://doi.org/10.1016/j.jacc.2018.03.022.
Iorga A, Cunningham CM, Moazeni S, Ruffenach G, Umar S, Eghbali M. The protective role of estrogen and estrogen receptors in cardiovascular disease and the controversial use of estrogen therapy. Biol Sex Differ. 2017;8(1):33. https://doi.org/10.1186/s13293-017-0152-8. PMID:29065927;PMCID:PMC5655818.
Shufelt CL, Pacheco C, Tweet MS, Miller VM. Sex-Specific Physiology and Cardiovascular Disease. Adv Exp Med Biol. 2018;1065:433–54. https://doi.org/10.1007/978-3-319-77932-4_27.
Bugiardini R, Ricci B, Cenko E, Vasiljevic Z, Kedev S, Davidovic G, Zdravkovic M, Miličić D, Dilic M, Manfrini O, Koller A, Badimon L. Delayed care and mortality among women and men with myocardial infarction. J Am Heart Assoc. 2017;6(8):e005968. https://doi.org/10.1161/JAHA.117.005968. PMID: 28862963; PMCID: PMC5586439.
Ladwig KH, Fang X, Wolf K, Hoschar S, Albarqouni L, Ronel J, Meinertz T, Spieler D, Laugwitz KL, Schunkert H. Comparison of Delay Times Between Symptom Onset of an Acute ST-elevation Myocardial Infarction and Hospital Arrival in Men and Women <65 Years Versus ≥65 Years of Age: Findings From the Multicenter Munich Examination of Delay in Patients Experiencing Acute Myocardial Infarction (MEDEA) Study. Am J Cardiol. 2017;120(12):2128–2134. doi: https://doi.org/10.1016/j.amjcard.2017.09.005. Epub 2017 Sep 18. PMID: 29122276.
Ski CF, King-Shier K, Thompson DR. Women are dying unnecessarily from cardiovascular disease. Am Heart J. 2020;230:63–5.
Lee C, Park S, Boylan JM. Cardiovascular health at the intersection of race and gender: identifying life-course processes to reduce health disparities. Kelley J, ed. J Gerontol Series B. 2021;76(6):1127–39.
Roy B, Kiefe CI, Jacobs DR, Goff DC, Lloyd-Jones D, Shikany JM, Reis JP, Gordon-Larsen P, Lewis CE. Education, race/ethnicity, and causes of premature mortality among middle-aged adults in 4 US Urban Communities: results From CARDIA, 1985–2017. Am J Public Health. 2020;110(4):530–6. https://doi.org/10.2105/AJPH.2019.305506. Epub 2020 Feb 20. PMID: 32078342; PMCID: PMC7067110.
Heart Disease and African Americans. Office of Minority Health. https://minorityhealth.hhs.gov/omh/browse.aspx?lvl=4&lvlid=19. Published 2021. Accessed 10 Aug 2021.
Williams DR, Lawrence Davis BA. Racism and health: evidence and needed research. Annu Rev Public Health. 2019;40(1):105–25. https://doi.org/10.1146/annurev-publhealth-040218-043750.
Kyalwazi AN, Loccoh EC, Brewer LC, et al. Disparities in cardiovascular mortality between black and white adults in the United States, 1999 to 2019. Circulation. 2022;146(3):211–28. https://doi.org/10.1161/CIRCULATIONAHA.122.060199.
Karnati SA, Wee A, Shirke MM, Harky A. Racial disparities and cardiovascular disease: one size fits all approach? J Card Surg. 2020;35(12):3530–8.
Every Student Succeeds Act, 20 U.S.C. § 6301; (2015). https://www.congress.gov/bill/114th-congress/senatebill/1177.
The White House. FACT SHEET: State-by-State Analysis of Record $2.7 Billion American Rescue Plan Investment in Historically Black Colleges and Universities. The White House. Published March 7, 2022. Accessed 28 Feb 2023. https://www.whitehouse.gov/briefing-room/statements-releases/2022/03/07/fact-sheet-state-by-state-analysis-of-record-2-7-billion-american-rescue-plan-investment-in-historically-black-colleges-and-universities/
Arnett DK, Blumenthal RS, Albert MA, et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;140(11):e596–646. https://doi.org/10.1161/cir.0000000000000678.
Roth GA, et al. Trends and patterns of geographic variation in cardiovascular mortality among US counties, 1980-2014. Jama. 2017;317(19):1976–92.
Miller CE, Vasan RS. The southern rural health and mortality penalty: a review of regional health inequities in the United States. Soc Sci Med. 2021;268:113443.
Cheng YJ, Imperatore G, Geiss LS, et al. Trends and disparities in cardiovascular mortality among U.S. Adults with and without self-reported diabetes, 1988–2015. Diabetes Care. 2018;41(11):2306–15.
Lee H, Singh GK. Psychological distress and heart disease mortality in the United States: results from the 1997–2014 NHIS-NDI record linkage study. Int J MCH AIDS. 2020;9(3):260–73.
Olubowale OT, Safford MM, Brown TM, et al. Comparison of expert adjudicated coronary heart disease and cardiovascular disease mortality with the national death index: results from the Reasons for Geographic And Racial Differences in Stroke (REGARDS) Study. J Am Heart Assoc. 2017;6(5):e004966. https://doi.org/10.1161/jaha.116.004966.
Acknowledgements
Najah Khan is a Burroughs Wellcome Fund Scholar in the Texas A&M University Academy of Physician Scientists, supported in part by a BWF Physician Scientist Institutional Award
Funding
No sources of funding were used in creating this manuscript.
Author information
Authors and Affiliations
Contributions
N.K. contributed to the writing and editing of this manuscript. ZJ and IAH contributed to implementing the statistical analysis and editing of this manuscript. All authors reviewed the final manuscript for content feedback and editing of the manuscript. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable. This study was exempt from review by the institutional review board of Houston Methodist as it does not contain Human Subjects research and is de-identified and publicly available NHIS data. No administrative approval was needed to access the raw data as it is publicly available. All data was anonymized prior to use in this study.
Consent for publication
Not applicable.
Competing interests
Dr. Nasir is on the advisory board of Amgen, Novartis, Medicine Company, and his research is partly supported by the Jerold B. Katz Academy of Translational Research.
Dr. Virani is receiving grant funding from Department of Veterans Affairs, NIH, World Heart Federation, Tahir and Jooma Family and is an Associate Editor for Innovations for the American College of Cardiology.
Dr. Hyder’s research is funded by several donors and organizations including United States National Institutes of Health, World Bank, and the World Health Organization.
Dr. Najah Khan has no competing financial interests, her research is supported by the Burroughs Wellcome Fund.
Dr. Zulqarnain Javed has no competing financial and non-financial interests to disclose.
Dr. Acquah has no competing financial and non-financial interests to disclose.
Dr. Hagan has no competing financial and non-financial interests to disclose.
Dr. Madiha Khan has no competing financial and non-financial interests to disclose.
Dr. Valero-Elizondo has no competing financial and non-financial interests to disclose.
Dr. Chang has no competing financial and non-financial interests to disclose.
Dr. Umair Javed has no competing financial and non-financial interests to disclose.
Dr. Taha has no competing financial and non-financial interests to disclose.
Dr. Blaha has no competing financial and non-financial interests to disclose.
Dr. Sharma has no competing financial and non-financial interests to disclose.
Dr. Blankstein has no competing financial and non-financial interests to disclose.
Dr. Gulati has no competing financial and non-financial interests to disclose.
Dr. Mossialos has no competing financial and non-financial interests to disclose.
Dr. Cainzos Achirica has no competing financial and non-financial interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
This supplementary file contains additional tables that relate to educational attainment and risk of mortality and age-adjusted mortality rates for the total and ASCVD populations. S1. Total Population: Education and Risk of Mortality, by age, sex, and race/ethnicity from the National Health Interview Survey, 2006-2014. S2. ASCVD Population: Education and Risk of Mortality, by age, sex, and race/ethnicity from the National Health Interview Survey, 2006-2014. S3. Age-adjusted Mortality Rate (per 100,000) for the Total and ASCVD populations by All-Cause and CVD Mortality.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Khan, N., Javed, Z., Acquah, I. et al. Low educational attainment is associated with higher all-cause and cardiovascular mortality in the United States adult population. BMC Public Health 23, 900 (2023). https://doi.org/10.1186/s12889-023-15621-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-023-15621-y