Abstract
Background
The impact of starting HIV pre-exposure prophylaxis (PrEP) on diagnoses of sexually transmitted infections (STI) remains unclear. We used data from German HIV/STI Checkpoints collected from 01/2019 to 08/2021 to determine the impact of PrEP use on syphilis, gonorrhoea and chlamydia diagnoses.
Methods
We used self-reported data on demographics, sexual behaviour, testing and PrEP use, as well as lab-confirmed diagnoses from visits to HIV/STI Checkpoints in Germany. PrEP use was categorized as (1) never used; (2) intention to use; (3) former use; (4) current on-demand use; (5) daily use. In multivariate regression analyses (MRA) with gonorrhoea, chlamydia, and syphilis diagnoses as outcomes, we controlled for age, number of sexual partners, number of condomless anal intercourse (CAI) partners in the last six months, and testing recency.
Results
For the analysis, we included 9,219 visits for gonorrhoea and chlamydia testing and 11,199 visits for syphilis testing conducted at checkpoints from 01/2019 to 08/2021. MRA identified age (aOR 0.98; 95%CI 0.97–0.99), number of sexual partners in the past six months (aOR 4.90; 95%CI 2.53–9.52 for 11 + partners), and use of chemsex substances (aOR 1.62; 95%CI 1.32-2.00) as risk factors for gonorrhoea, while age (aOR 0.99; 95%CI 0.98-1.00), number of CAI partners (aOR 3.19; 95%CI 2.32–4.41 for 5 + partners), partner sorting (aOR 1.30; 95%CI 1.09–1.54), and use of chemsex substances (aOR 1.29; 95%CI 1.05–1.59) were risk factors for chlamydia infections. For syphilis, the number of CAI partners (aOR 3.19; 95%CI 1.60–6.34 for 5 + partners) was found to be the only significant risk factor. There was a strong association between PrEP use and the number of sexual partners (≤ 5 vs.>5: aOR 3.58; 95%CI 2.15–5.97 for daily PrEP use), the number of CAI partners in the past six months (≤ 1 vs.>1: aOR 3.70; 95%CI 2.15–6.37 for daily PrEP use), and the number of STI tests performed (suggesting higher testing frequency). Both outcomes were also related to partner sorting, chemsex, and selling sex.
Conclusions
Checkpoint visits reporting current PrEP use or intention to start PrEP correlated with eligibility criteria for PrEP, i.e. high partner numbers, inconsistent condom use during anal intercourse, and use of chemsex drugs. Use of HIV-specific prevention methods such as HIV serosorting, PrEP sorting, and viral load sorting was reported more frequently. (Daily) PrEP use was an independent risk factor for a chlamydia diagnosis only.
Similar content being viewed by others
Background
There are many, partly conflicting data on the impact of starting HIV pre-exposure prophylaxis (PrEP) on the diagnosis of sexually transmitted infections (STI). Even systematic reviews arrive at different conclusions [1,2,3,4,5,6]. Reasons for the diverging results could be, e.g., differences in the baseline STI risk between populations compared, insufficient controlling for increased STI screening frequency within PrEP programmes, aggregate vs. single infection outcome measures, or neglected change in STI diagnoses rates over time.
In Germany, testing is offered by primary care physicians, specialists, and local health departments. However, barriers to testing in primary care include (1) the lack of insurance coverage for STI screening for asymptomatic infections and (2) the requirement to disclose sexual risk behaviours in order to receive HIV/STI testing covered by health insurance. To improve access to queer-friendly HIV and STI testing, Checkpoints were established and managed by non-governmental organisations in Germany. Checkpoints are low-threshold community-based testing and counselling sites [7, 8].
PrEP for HIV was officially approved in Germany in 2016, but access remained severely restricted due to prohibitively high drug costs and lack of health insurance coverage until October 2017, when a drastic price cut for a generic PrEP version greatly increased PrEP affordability [9]. Since September 2019, check-ups, medical advice, HIV/STI testing and the actual PrEP prescription are covered by the statutory health insurance system in Germany, provided the prescribing physician is licensed to prescribe PrEP [10]. Until September 2019, HIV/STI Checkpoints in Germany were a low-cost alternative for HIV and STI testing for PrEP users compared to the primary care system. After September 2019, Checkpoints remain a low-cost alternative for PrEP users with private health insurance and co-pay, for PrEP users without health insurance, and for PrEP users with access barriers to licensed PrEP prescribers, as well as for PrEP users who are insured but do not wish to disclose PrEP use to their health insurance provider.
We used observational data from HIV/STI Checkpoints collected in Germany from 01/2019 to 08/2021 to determine the association between PrEP use and the diagnosis of an infection with syphilis, gonorrhoea and/or chlamydia.
Methods
We used biobehavioural data routinely collected at consultation visits in HIV/STI Checkpoints in Germany from 01/2019 to 08/2021. At each visit, a voluntary and anonymous questionnaire is self-administered on a tablet. Laboratory test results are subsequently added to the questionnaire, resulting in an anonymous bio-behavioural dataset of Checkpoint visits. Individual participant data cannot be matched to prior visits. Questions include demographics (month and year of birth, country of birth, country of residence, level of education, employment status, as well as gender, sexual orientation and relationship status), sexual behaviour (number, gender and type of partners in the last 6 months; condom and PrEP use), substance use when having sex and type of substances used, place and recency of previous HIV and STI tests, hepatitis vaccination status, self-assessed risk estimate for HIV infection, reasons for testing, and reasons for not using condoms. Questionnaires cannot be linked to individuals but represent the total number of consultations, i.e. a person might have filled out more than one questionnaire. The subgroup of self-identified heterosexual clients was excluded from this analysis because PrEP use was very infrequent (< 1%) in this client subgroup. Ethic board approval was granted by the Ethics Review Board of the Berlin Medical Association (Eth-61/21).
Based on answers to questions on reasons for testing and on PrEP use since the previous HIV test, we constructed a secondary variable to categorize (1) no PrEP use; (2) intention to use PrEP; (3) former PrEP use; (4) current on-demand PrEP use; and (5) daily PrEP use (see Additional File 1).
We used uni- and multivariate regression analyses with a diagnosis of gonorrhoea, chlamydia and syphilis as outcome while controlling for age, number of sexual partners in the last six months, and the number of condomless anal intercourse (CAI) partners in the last six months, and using the type of PrEP used as explanatory variable. Further variables included in the models as surrogate markers for distinct sexual networks and their potential impact were receiving money for sexual services, a combined variable that includes HIV serosorting, PrEP sorting, or viral load sorting as reasons for not using condoms named ‘partner sorting’ (see Additional File 1), and reporting the use of chemsex drugs in the context of recent sexual encounters.
The multivariate logistic regression models were constructed with stepwise forward variable selection for variables significant in univariate analysis. We included three variables (age, region of birth, partner sorting) in the syphilis model which were not significant in univariate analysis for better comparability with the gonorrhoea and chlamydia models. Missing values were included as a separate category if appropriate, except for age, which was included as a continuous variable.
In Germany, Checkpoints in general do not provide treatment but refer clients with an STI diagnosis to a physician. Most clients are aware of this fact, thus clients with symptoms would seek treatment directly. It is for this reason that clients in Checkpoints generally present without signs or symptoms of an STI. Data on symptoms are therefore not collected. Gonorrhoea and chlamydia diagnoses are based on positive nucleic acid amplification test results. Most gonorrhoea/chlamydia testing in checkpoints is conducted on pooled specimens, hence it is not possible to determine whether one or multiple sites were affected. A syphilis diagnosis was based on serological lab test results. We defined syphilis as “active” when the test results were in line with a recommendation to treat.
We also constructed two multivariate regression models to identify factors associated with the numbers of sex partners and the number of CAI partners. Both models used binarized outcomes: up to 5 partners or more than 5 different sex partners in the last 6 months and up to 1 partner or more than 1 partner with CAI in the last 6 months.
Clients filled out anonymous online questionnaires prior to their consultations on tablets provided at each Checkpoint. Laboratory test results were entered by Checkpoint staff or volunteers post hoc. We analysed data in Stata 17™ (StataCorp, College Station, Texas, USA).
Results
The analysis of 11,228 Checkpoint visits from 01.01.2019 through 31.08.2021 showed that not using PrEP or not answering the question whether PrEP was used was with 72% the most common answer (see Additional File 1). Bearing in mind that returning clients could have provided a questionnaire at each visit, an interest in starting PrEP was disclosed on more than 10% of questionnaires while current PrEP use was reported on more than 16% of questionnaires (Table 1).
Matched with 9,239 tests results for gonorrhoea, 9,247 for chlamydia, and 11,228 for syphilis, the most prevalent infections were chlamydia and gonorrhoea with 11.2–11.8% during visits of current PrEP users, followed by visits of former PrEP users with 8.5% and 10.4% respectively. Syphilis was also more frequently diagnosed during visits of current PrEP users, with 2.7% in daily and 3.0% in on-demand use. The number of tests for gonorrhoea/chlamydia and syphilis, and the number and proportion of diagnoses are shown in Table 1.
Factors associated with the diagnosis of gonorrhoea in the multivariate model were primarily the number of sex partners in the last 6 months and age (2.4% risk reduction per additional year of age). Other factors independently associated with a gonorrhoea diagnosis were 5 or more CAI partners in the last 6 months or a missing response to this question, the intention to use PrEP, the use of chemsex drugs with recent sex partners, a previous STI test in the last 6 months, and the following regions of origin: European countries other than Germany, South America, Australia and New Zealand. Borderline significant (0.05 < p < 0.09) were the following factors: having had CAI with 1 to 5 partners in the last 6 months,, and any current PrEP use (see Table 2).
Factors associated with the diagnosis of a chlamydia infection were primarily the number of CAI partners in the last 6 months and age (1.4% risk reduction per additional year of age). Other factors independently associated with a chlamydia diagnosis were having had more than 10 different sex partners in the last 6 months, daily PrEP use, reporting not to use condoms based on information about HIV serostatus, PrEP use or undetectable viral load of the partner, the use of chemsex drugs with recent sex partners, and having been born in Asia. A recent STI test in the last 3 months and a last STI test more than 6 months ago were both associated with a lower probability of a chlamydia diagnosis (see Table 3).
Factors associated with an acute syphilis diagnosis were primarily the number of CAI partners in the last 6 months (see Table 4).
The following factors were associated with higher numbers of sex partners (i.e. more than 5) in the last 6 months: ever PrEP use or the intention to use PrEP; receiving money for providing sexual services; the use of chemsex drugs; reporting not to use condoms based on information about HIV serostatus, PrEP use or undetectable viral load of the partner; a recent STI test; and having been born in the following regions: European countries other than Germany, Eastern Mediterranean, Central or South America, Australia or New Zealand. Compared to not using PrEP, taking PrEP for less than 6 months was associated with a lower probability for high partner numbers (see Table 5).
Associated with more than one CAI partners in the last 6 months were ever PrEP use or the intention to use PrEP; receiving money for providing sexual services; the use of chemsex drugs; reporting not to use condoms based on information about HIV serostatus, PrEP use or undetectable viral load of the partner; an STI test within the last 3 months; and – compared to having been born in Germany – all other regions of origin except for Australia and New Zealand. Taking PrEP for more than 12 months was associated with a higher probability of more than 1 CAI partner in the last 6 months (see Table 5).
Discussion
Our analyses confirmed that PrEP users and Checkpoint clients with the intention to use PrEP met sexual risk criteria for PrEP eligibility such as higher partner numbers, inconsistent or no condom use for anal intercourse, and chemsex substance use. They were also more likely to use HIV-specific prevention methods such as HIV serosorting, PrEP sorting, and viral load sorting.
Beyond these shared characteristics, there were noticeable differences regarding factors associated with the diagnosis of specific bacterial STIs. For a gonorrhoea diagnosis, there was an almost linear relationship with the number of sex partners and the number of CAI partners in the last six months, suggesting that not only CAI but also a range of other sexual practices contribute to the sexual transmission of gonococci [11,12,13,14,15]. From our data, we were unable to determine whether the number of partners increases or condom use declines after initiating PrEP. The association of both findings with the length of PrEP use would be compatible with either explanation, but might also be due to a cohort effect of earlier initiation of PrEP use by MSM with higher partner numbers and less consistent condom use. However, other observations from longitudinal data on PrEP use also suggest that condom use declines and partner numbers moderately increase [1, 5, 16,17,18]. Contrastingly, it appears that primarily the lack of condom use for anal intercourse contributes to an increased transmission risk of chlamydia and syphilis. This is consistent with the finding that pharyngeal chlamydia infections are rare [19], and that (painless) primary and secondary syphilis lesions remain more often undetected in the rectum than in the mouth or on the genitals.
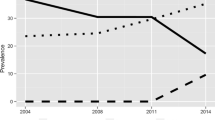
The strong association in univariate analysis of STI diagnoses with current PrEP use and intention to use PrEP is losing significance in multivariate analysis and could be credited to higher numbers of sexual partners, respectively CAI partners. The remaining associations might be explained by sexual network effects or by testing effects. Persons taking PrEP for example may form sexual networks with other persons taking PrEP or being successfully treated for HIV. The association of shorter testing recency with higher probability of a gonorrhoea diagnosis might either be related to the association between shorter testing intervals with higher partner numbers or it may represent a paradoxical effect of frequent screening and treatment of asymptomatic infections. The association of the shorter testing interval with partner numbers has been controlled for in our analysis. The paradoxical association of frequent screening and treatment of asymptomatic infections with more self-reported bacterial STIs might be due to the arrested immunity hypothesis, i.e. a reduction in lasting immunity due to treatment leading to an increased susceptibility for reinfection [20]. This association has also been observed in a sample comparing prevalence in European MSM between 2010 and 2017 [21].
In general, we would expect a stronger association between testing frequency and diagnosis of gonorrhoea and chlamydia, but the association cannot be confirmed because we can only look at data from visits and not from individual client histories and cannot discern differences in STI testing frequencies.
The different patterns of STI infections by region of origin are not readily accounted for by the numbers of sex partner or the number of CAI partners, and point to the need for more research into migration-associated vulnerabilities and behavioural diversity of migrants from different regions.
Limitations
Due to a lack of a unique identifier, we cannot identify individuals and their repeat visits. People at higher risk for an STI might be over-represented because they are more likely to be on PrEP and/or visit Checkpoints more frequently. Overall, 73% of daily PrEP users have been tested for STIs within the last 3 months while only 11% of non-PrEP users have done so. Nevertheless, we can compare the risk of having acquired an STI since the last STI testing between PrEP users and non-PrEP users. Untreated asymptomatic gonorrhoea usually clears within 3 months; infections would therefore not accumulate with longer testing intervals, and very few, if any checkpoint clients are testing more frequently than every three months. Thus, our comparison between PrEP users and non-PrEP users regarding the risk of acquisition of gonorrhoea may not be substantially biased by higher testing frequencies. Compared to gonorrhoea, infections with chlamydia take longer to clear and thus chlamydia cases may accumulate with longer testing intervals [22,23,24,25]. This may increase the probability to detect chlamydia among checkpoint clients with longer testing intervals, thus this may weaken the association with PrEP use. As for syphilis, a diagnosis is usually based on the detection of long-lasting antibodies. Titres decline after successful treatment and are boosted by re-infection. Compared to non-PrEP users, testing PrEP users more frequently for syphilis would result in earlier detection and treatment. In the absence of a documented treatment history, it may be difficult to discern whether an infection is new and untreated or a successfully treated re-infection because both can show elevated titres. Thus, for syphilis the impact of more frequent checkpoint visits on associations in the MRA is the least predictable among the three STIs. To summarize, the prevalence of infections among checkpoint clients is biased by different testing intervals, which should be considered when interpreting the associations found with PrEP use.
Regarding chlamydia testing, there was no subtyping conducted to identify serotypes L1-L3. Due to a relatively high prevalence of lymphogranuloma venereum infections (LGV) among MSM from Germany diagnosed with HIV [26] and reduced HIV serosorting among PrEP users, the prevalence of LGV among PrEP users in Germany may be currently increasing.
Conclusion
Our analysis suggests that the higher STI prevalence detected during visits by PrEP users compared to non-users is due to (1) more frequent screening in general, (2) higher partner numbers in the case of gonorrhoea and (3) more condomless anal intercourse in the case of chlamydia and syphilis. Initiating PrEP might increase the acquisition of these STIs should PrEP users have sex with more partners and/or reduce condom use for anal intercourse. Since our data are cross-sectional, we are unable to discern this further.
Data Availability
The dataset used for this analysis has been obtained from the German Checkpoint Collaborative Group (GCCG) under a data transfer agreement that prohibits sharing the dataset publicly. The dataset or aggregated data could be made available from the corresponding author on reasonable request.
References
Beymer MR, DeVost MA, Weiss RE, Dierst-Davies R, Shover CL, Landovitz RJ, Beniasians C, Talan AJ, Flynn RP, Krysiak R, et al. Does HIV pre-exposure prophylaxis use lead to a higher incidence of sexually transmitted infections? A case-crossover study of men who have sex with men in Los Angeles, California. Sex Transm Infect. 2018;94(6):457–62.
Coudray M, Kiplagat S, Saumell F, Madhivanan P. Sexually transmitted infections among high-risk populations that use treatment as prevention or pre-exposure prophylaxis: a protocol for a systematic review. BMJ open. 2019;9(12):e032054.
Freeborn K, Portillo CJ. Does pre-exposure prophylaxis for HIV prevention in men who have sex with men change risk behaviour? A systematic review. J Clin Nurs. 2018;27(17–18):3254–65.
Ong JJ, Baggaley RC, Wi TE, Tucker JD, Fu H, Smith MK, Rafael S, Anglade V, Falconer J, Ofori-Asenso R, et al. Global epidemiologic characteristics of sexually transmitted infections among individuals using preexposure Prophylaxis for the Prevention of HIV infection: a systematic review and Meta-analysis. JAMA Netw open. 2019;2(12):e1917134.
Traeger MW, Schroeder SE, Wright EJ, Hellard ME, Cornelisse VJ, Doyle JS, Stoové MA. Effects of Pre-exposure Prophylaxis for the Prevention of Human Immunodeficiency Virus infection on sexual risk behavior in men who have sex with men: a systematic review and Meta-analysis. Clin Infect diseases: official publication Infect Dis Soc Am. 2018;67(5):676–86.
Chou R, Evans C, Hoverman A, Sun C, Dana T, Bougatsos C, Grusing S, Korthuis PT. U.S. Preventive Services Task Force evidence Syntheses, formerly systematic evidence reviews. Pre-Exposure Prophylaxis for the Prevention of HIV infection: a systematic review for the US Preventive Services Task Force. edn. Rockville (MD): Agency for Healthcare Research and Quality (US); 2019.
Schink SB, Schafberger A, Tappe M, Marcus U, Teststellenprojekt. : Bericht 2015/2016: Robert Koch-Institut; 2019. https://edoc.rki.de/bitstream/handle/176904/5896/Teststellenbericht_2015_2016.pdf.
Schink SB, Schafberger A, Tappe M, Marcus U. Gemeinsames Teststellenprojekt 2017: Robert Koch-Institut; 2019. https://edoc.rki.de/bitstream/handle/176904/5895/Teststellenbericht_2017.pdf.
PrEP-Info [https://www.koelsche-blister.de/index.php/prep/allgemeines], last accessed 04.04.2023.
Bundesgesundheitsministerium. Schnellere Termine, mehr Sprechstunden, bessere Angebote für gesetzlich Versicherte. In: Terminservice- und Versorgungsgesetz (TSVG Terminservice- und Versorgungsgesetz). https://www.bundesgesundheitsministerium.de/terminservice-und-versorgungsgesetz.html; 2019, Last accessed 04.04.2023.
Chow EP, Fairley CK. The role of saliva in gonorrhoea and chlamydia transmission to extragenital sites among men who have sex with men: new insights into transmission. J Int AIDS Soc. 2019;22(Suppl 6):e25354.
Schmidt AJ, Rasi M, Esson C, Christinet V, Ritzler M, Lung T, Hauser CV, Stöckle M, Jouinot F, Lehner A, et al. The Swiss STAR trial - an evaluation of target groups for sexually transmitted infection screening in the sub-sample of men. Swiss Med Wkly. 2020;150:w20392.
van der Veer B, Hoebe C, Dukers-Muijrers N, van Alphen LB, Wolffs PFG. Men and Women Have Similar Neisseria gonorrhoeae Bacterial Loads: a Comparison of Three Anatomical Sites.Journal of clinical microbiology2020, 58(11).
Bamberger DM, Graham G, Dennis L, Gerkovich MM. Extragenital Gonorrhea and Chlamydia among Men and Women according to type of sexual exposure. Sex Transm Dis. 2019;46(5):329–34.
Hook EW 3rd, Bernstein K. Kissing, saliva exchange, and transmission of Neisseria gonorrhoeae. Lancet Infect Dis. 2019;19(10):e367–9.
Chapin-Bardales J, Johnson Jones ML, Kirkcaldy RD, Bernstein KT, Paz-Bailey G, Phillips C, Papp JR, Raymond HF, Opoku J, Braunstein SL et al. Pre-exposure Prophylaxis Use and Detected Sexually Transmitted Infections Among Men Who Have Sex With Men in the United States-National HIV Behavioral Surveillance, 5 US Cities, 2017. Journal of acquired immune deficiency syndromes (1999) 2020, 85(4):430–435.
Nguyen VK, Greenwald ZR, Trottier H, Cadieux M, Goyette A, Beauchemin M, Charest L, Longpré D, Lavoie S, Tossa HG, et al. Incidence of sexually transmitted infections before and after preexposure prophylaxis for HIV. Aids. 2018;32(4):523–30.
Morgan E, Dyar C, Newcomb ME, D’Aquila RT, Mustanski B. PrEP use and sexually transmitted infections are not Associated longitudinally in a Cohort Study of Young Men who have sex with men and Transgender Women in Chicago. AIDS Behav. 2020;24(5):1334–41.
van Liere GAFS, Hoebe CJPA, Dukers-Muijrers NHTM. Evaluation of the anatomical site distribution of chlamydia and gonorrhoea in men who have sex with men and in high-risk women by routine testing: cross-sectional study revealing missed opportunities for treatment strategies. Sex Transm Infect. 2014;90(1):58–60.
Brunham RC, Rekart ML. The arrested immunity hypothesis and the epidemiology of chlamydia control. Sex Transm Dis. 2008;35(1):53–4.
Marcus U, Mirandola M, Schink SB, Gios L, Schmidt AJ. Changes in the prevalence of self-reported sexually transmitted bacterial infections from 2010 and 2017 in two large european samples of men having sex with men-is it time to re-evaluate STI-screening as a control strategy? PLoS ONE. 2021;16(3):e0248582.
Barbee LA, Khosropour CM, Soge OO, Hughes JP, Haglund M, Yeung W, Golden MR. The natural history of rectal Gonococcal and Chlamydial Infections: the ExGen Study. Clinical Infectious Diseases; 2021;74(9):1549–1556.
Barbee LA, Soge OO, Khosropour CM, Haglund M, Yeung W, Hughes JP, Golden MR. The Duration of Pharyngeal Gonorrhea: A Natural History Study. Clinical Infectious Diseases 2020;73(4):575–582.
Chow EP, Camilleri S, Ward C, Huffam S, Chen MY, Bradshaw CS, Fairley CK. Duration of gonorrhoea and chlamydia infection at the pharynx and rectum among men who have sex with men: a systematic review. Sex Health. 2016;13(3):199–204.
Chow EPF, Vodstrcil LA, Williamson DA, Maddaford K, Hocking JS, Ashcroft M, De Petra V, Bradshaw CS, Fairley CK. Incidence and duration of incident oropharyngeal gonorrhoea and chlamydia infections among men who have sex with men: prospective cohort study. Sex Transm Infect. 2021;97(6):452–7.
Hoffmann C. Lymphogranuloma venereum: Renaissance eines Erregers. Dtsch Arztebl International. 2017;114(17):11.
Acknowledgements
The data used for this analysis have been collected by the German Checkpoint Collaborative Group (GCCG). The following members of the GCCG contributed data for this analysis (in the order of number of client visits in 2019–2021): Checkpoint Berlin; Mann-O-Meter, Berlin; Sub München; Checkpoint Freiburg; Checkpoint Nürnberg; Aidshilfe Berlin; Aidshilfe Düsseldorf; Aidshilfe Saarbrücken; Fixpunkt Berlin; KOSI.MA, Mannheim; Pluspunkt Berlin; Hein & Fiete, Hamburg; Checkpoint Hannover; Checkpoint Konstanz; Checkpoint Regensburg (Oberpfalz); Aidshilfe Ulm; Rat & Tat Potsdam; Rat & Tat Cottbus; Checkpoint Augsburg; Aidshilfe Potsdam; Aidshilfe Tübingen-Reutlingen. The GCCG is coordinated by Deutsche Aidshilfe Berlin.
We thank all Checkpoint clients for answering questionnaires at their visits and Checkpoint staff and volunteers for supporting data collection and entering test results in the database.
Funding
Open Access funding enabled and organized by Projekt DEAL. The work of the GCCG has been financially supported by the MAC AIDS Fund, MSD Sharp and Dohme, and ViiV Healthcare. No specific funding was obtained for this study. SBS received funding from the German Ministry of Health in the context of the PrEP evaluation project EVE-PrEP. The German Ministry of Health had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
The analysis was conceived and conducted by UM, SBS prepared the dataset and double-checked the analysis, CW contributed to data sampling. The first draft was written by UM, and all authors contributed to, have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethic board approval for this analysis was granted from the Ethics Review Board of the Berlin Medical Association on Oct. 05, 2021 (Eth-61/21). All methods were carried out in accordance with relevant guidelines and regulations. Informed consent was obtained from all subjects.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Additional File 1
: Variables based on questionnaire items (detailed description of PrEP use and partner sorting variables)
Additional Table 1
: Absolute numbers for checkpoint visits from 01/2019 to 08/2021 for the categories and sub-categories included in multivariate regression analyses
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Marcus, U., Schink, S.B. & Weber, C. HIV pre-exposure prophylaxis and diagnoses of sexually transmitted infections – observational data from German checkpoints, 01/2019–08/2021. BMC Public Health 23, 661 (2023). https://doi.org/10.1186/s12889-023-15570-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-023-15570-6