Abstract
Background
Paying attention to the health-related quality of life (HRQOL) of rural residents in poverty-stricken areas is an important part of China's poverty alleviation, but most studies on health-related quality of life have focused on rural residents, elderly individuals, and patients; evidence on the HRQOL of rural minority residents is limited. Thus, this study aimed to assess the HRQOL of rural Uighur residents in remote areas of Xinjiang, China, and determine its influencing factors to provide policy opinions for realizing a healthy China strategy.
Methods
A cross-sectional study was performed on 1019 Uighur residents in rural areas. The EQ-5D and self-administered questionnaires were used to assess HRQOL. We applied Tobit and binary logit regression models to analyse the factors influencing HRQOL among rural Uighur residents.
Results
The health utility index of the 1019 residents was − 0.197,1. The highest proportion of respondents reporting any problem was for mobility (57.5%), followed by usual activity (52.8%). Low levels of the five dimensions were related to age, smoking, sleep time, Daily intake of vegetables and fruit per capita. Gender, age, marital status, physical exercise, sleep duration, daily intake of cooking oil per capita, daily intake of fruit per capita, distance to the nearest medical institution, non-infectious chronic diseases (NCDs), self-rated health score, and participation in community activities were correlated with the health utility index of rural Uighur residents.
Conclusions
HRQOL was lower for rural Uyghur residents than for the general population. Improving health behavioural lifestyles and reducing the incidence of poverty (return to poverty) due to illness are effective means of promoting the health in Uyghur residents. The region must fulfil the health poverty alleviation policy and focus on vulnerable groups and low-income residents to improve the health, ability, opportunity, and confidence of this population to live well.
Similar content being viewed by others
Introduction
Health is essential for comprehensive human development and an important symbol of national wealth and prosperity. Since the implementation of the Health China 2030 plan and the Health Poverty Alleviation Project, Chinese residents’ health has improved significantly with life expectancy per capita reaching 77.3 years in 2019 and major health indicators generally ranking among the top in middle- and high-income countries [1]. Research on alleviating health poverty for the poor has shown positive progression. By the end of December 2019, the participation rate of the rural poor medical insurance had reached 99.99%, realising virtually complete insurance. More than 16 million poor people have received basic treatment and services. The rate of intra-county consultation for the poor has reached over 90%, and more than 9.97 million poor households have been lifted out of poverty due to illness [2].
While achieving positive results, relative poverty, low-income groups and disease characteristics also determine the long-term and arduous nature of the road of health poverty alleviation projects. Catastrophic disease is a major cause of rural poverty [3]. According to a statistical bulletin released by the National Bureau of Statistics of China, 44.1% of the rural poor are impoverished due to illness and 22.8% due to long-term chronic diseases (e.g. cardiovascular diseases) [4]. The intersection of poverty and illness is one of the main challenges plaguing the sick and poor and constitutes the focus and difficulty of governance for precise poverty-alleviation policies.
Xinjiang is located in western China, over 3000 km from Beijing, is the priority region for China's health poverty alleviation project [5]. The south of Xinjiang is the main battleground for China's poverty-eradication efforts and occupies a special position in the overall national strategy with core interests. Southern Xinjiang is predominantly Uyghur with per capita income lower than the national average [6], and relative poverty still exists. The health status of the rural population that has been lifted from poverty still requires long-term attention. Several studies have investigated mechanisms of physical and mental health of poor and low-income populations, but few have reported disease-related poverty and health-related quality of life (HRQOL) for low-income groups of ethnic minorities.
Regarded as a broad and multifaceted concept that usually reflects individuals' physical and mental health status, HRQOL has been widely used in clinical and public health research [7].
Health-related quality of life measurements are mainly assessed using generic and specific scales, European Quality of Life Five Dimension (EQ-5D) instrument was one of the most applicable measurements to assess HRQOL. Compared with other scales, EQ-5D instrument was more applicable for people in rural areas with low education status and it could provide a quantitative measure of health outcome [8]. It has five dimensions (mobility, self-care, usual activities, pain/discomfort, anxiety/depression, each with three response levels (EQ-5D-3L) and five response levels (EQ-5D-5L) [9]. Evidence shows that EQ-5D-5L can reduce the potential for ceiling effects and to address concerns about the sensitivity of the 3L version for detecting clinically important differences in HRQOL, therefore may be more useful for measuring population-level health status [10]. EQ-5D has good reliability and validity and has been widely used in measuring HRQOL in the Chinese population [11],and EQ-5D Chinese is generally recognized for its effectiveness in the Chinese population, and EQ-5D scores as one of the indicators of health-related quality of life of the population in the 5th National Health Service Survey [12].
HRQOL is represented by health-rated quality weights (utilities) typically measured on a ‘0’ to ‘1’ scale where ‘0’ is defined as a health state equivalent to being dead and ‘1’ is full health [13], however, health utility values cannot be calculated directly. Therefore, a population-based preference trade-off time model is required to measure the results and convert them into health utility values for the population. In China, Liu et al. has developed a Chinese general population-based value set for EQ-5D health states, which is capable of converting health states measured by the EQ-5D-5L [14]. Nevertheless, the EQ-5D scale has a strong ceiling effect, i.e., most respondents report 'no problems' on all dimensions, and restricted range of health utility values. The Tobit model, introduced by TOBIN in 1958, is a restricted regression model characterized by the availability of the dependent variable in a "restricted" manner, hence the term "restricted dependent variable model", and is widely used in health scale evaluation and analysis of factors influencing quality of life [15].
Previous studies on HRQOL have focused on rural residents [16, 17] elderly individuals, and patients [16, 18]. Nevertheless, evidence of the HRQOL of rural minority residents is limited. Uyghurs, one of the major ethnic minorities in Xinjiang, have developed unique ethnic and regional dietary habits and cultural customs based on living conditions, production, and lifestyle, which affect the HRQOL of Uyghur residents to varying degrees and present characteristics different from those of other provinces or regions. Paying attention to the health-related quality of life (HRQOL) of rural residents in poverty-stricken areas is an important part of China's poverty alleviation. Therefore, this study aimed to describe the health status of rural Uyghur residents in remote areas of Xinjiang and explore the impacts of rural Uyghur residents’ HRQOL.
Methods
Data source and participants
A representative sample of rural Uyghur residents in Xinjiang was chosen as the research population for this study. July to August 2021, our group conducted a field survey in Tumushuk, Xinjiang Production and Construction Corps, China. A multi-stage whole-group random sampling method was used, divided into four stages. In the first stage, there are four cities in Southern Region of Xinjiang Production and Construction Corps according to the administrative division: the First Division (Alaer city), the Second Division (Tiemenguan city), the Third Division (Tumushuk city) and the Fourteenth Division (KunYu city). One of these cities was chosen at random which was Third Division (Tumushuk city). In the second stage, one of the seven corps in the Third Division (Tumushuk City), namely 53rd Corps, was randomly selected as the research area. In the third stage, 1, 2, 3 and 4 companies were randomly selected in whole groups based on the geographical location and population of the 53rd Regiment's companies as the sample areas. Finally, 4 companies were surveyed of all Uyghur residents. Since the 4 companies are Uyghur-inhabited areas and have similar dietary habits, cultural backgrounds, and lifestyles as Uyghurs in other rural areas of Xinjiang and follow the principle of randomization in the sampling process, so they can represent the rural Uyghur residents of Xinjiang.
The sample size of this research was determined based on the sample size formula (Eq. 1–1), δ is the allowable error, ɑ = 0.05, and P is the poverty incidence in the southern Xinjiang region in 2013 (29.1%) [2], when δ = 0.1, N = 400 × Q/P, the total sample size required for the study was about 976 cases, and the actual survey sample size was 1073 cases.
Face-to-face questionnaire interviews were used to investigate rural Uyghur residents’ health status. The surveyors were undergraduate nursing students familiar with the Uyghur language and Chinese. The questionnaire consisted of two sections: (1) a questionnaire on the personal situations of rural Uyghur residents and (2) the EQ-5D-5L scale. Respondents included in this study were required to meet the following criteria: (i) Uygur residents over 18 years old and have lived there for at least 6 months; (ii) had no missing values for the EQ-5D; and (iii)had no missing values for other variables included in the current analyses. Thus, a total of 1019 samples were included in the study, with a response rate of 95%. All participants signed informed consent. This study was approved by the Ethics Committee of the First Affiliated Hospital of Shihezi University School of Medicine (No. KJ2021-135–01).
HRQOL measurement
EQ-5D scale is the most internationally used measurement of health-related quality of life in the population and is suitable for measuring health status in disadvantaged areas and in areas with low levels of education [19]. Research has shown that the EQ-5D has good reliability and validity for assessing health-related quality of life in the general population or in people with medical conditions [20, 21]. The EQ-5D-5L scale is an optimized version of the EQ-5D-3L scale, which has fewer ceiling effects and limitations [22]. In the research, the Cronbacha's α coefficient of EQ-5D-5L scale was 0.848, indicating good reliability, which could be used to measure health-related quality of life of the rural Uygur residents. Therefore, this research uses the EQ-5D-5L as a measure of health-related quality of life for rural Uyghur residents.
The EQ-5D-5L scale consists of two parts:(1) five dimensions of mobility, self-care, usual activity, pain/discomfort, and anxiety/depression, which have five levels of response from no problems (code 1) to extreme problems (code 5), and (2) the EQ visual analogue scale, which can be used to assess the self-rated health of respondents using a 100-mm scale with a score ranging from 0 (the worst health you can imagine) to 100 (the best health you can imagine) [23].
Groups and variables
Low- and non-low-income groups were divided according to the 2020 Xinjiang Rural Minimum Livelihood Security standard of RMB 4,100 per person per year [24]. Dependent variables were mobility, self-care, usual activity, pain/discomfort, and depression/anxiety on the health utility index. Other variables were (1) demographic characteristics (age, gender, marital status, occupation, household size, and income, (2) healthy lifestyle behaviours (smoking, alcohol consumption, physical activity, daily intake of cooking oil per capita, daily intake of fruit per capita, daily intake of vegetables per capita, and sleep duration), (3) health service accessibility (distance to the nearest medical facility), (4) health status (body mass index(BMI), self-rated health score, Non-communicable chronic diseases(NCDs), hospitalisation, two-week visit), and (5) social support (who to live with and community involvement).
Statistical analysis
Data were analysed using Stata version 12.0 and SPSS version 26.0. First, the demographic characteristics of the Uyghur population and the distribution of the EQ-5D for different subgroups were described. Continuous variables were presented as means, standard deviations, medians, and interquartile ranges, and categorical variables were presented as absolute numbers and frequencies. Second, the chi-square, t-test, and rank-sum tests were used to assess differences in the characteristics of residents in the low- and non-low-income groups and the distribution of each dimension of the EQ-5D. Third, the Wilcoxon test was used for binary variables in the single-factor analysis, and the Kruskal–Wallis H test was used for multiple categorical variables. The range of values of health utility values as dependent variables is subject to limited, therefore the tobit model was used to analyse. And binary logistic regression models were used to explore the factors of the five dimensions of the EQ-5D. The significance level was set at P < 0.05.
Results
Participant characteristics
Of the 1019 respondents, 58.2% were female, the average age was 43.7 years, 61.5% had an education level of elementary school or less, and the median BMI was 24.5 kg/cm2. There were 375 people in the low-income group and 644 in the non-low-income group, and the self-rated health score was slightly lower in the low-income group (7.45 ± 1.74) than in the non-low-income group (7.63 ± 2.02). Age (P = 0.004), household size (P = 0.002), occupation (P = 0.03), sleep duration (P = 0.034), daily cooking oil intake per capita (P = 0.005), daily vegetable intake per capita (P = 0.005), distance to the nearest health facility (P = 0.005), self-rated health score (P = 0.03), and those who lived with others were statistically significant between the two groups (P = 0.038); differences were statistically significant. Table 1 shows respondents’ characteristics.
EQ-5D distribution and health utility index in different groups
As shown in Table 2, the range of the health utility index for the 1019 respondents was (− 0.197, 1). Of the respondents, 52.8%, 49.2%, 57.5%, 42.3%, and 30.8% had problems with mobility, self-care, usual activity, pain/discomfort, and depression/anxiety, respectively. More respondents had more problems with their usual activities, mobility, and less problems with depression/anxiety. We compared the low-income group with the non-low-income group, and the differences were statistically significant in the self-care (P = 0.027) and usual activity (P = 0.023) dimensions. However, the health utility indices for the low-income (− 0.182, 1) and non-low-income (− 0.197, 1) groups and the difference between the two groups (P = 0.251) was not statistically significant.
Single-factor analysis
We conducted univariate analyses of the factors influencing the health utility index, except for income (P = 0.251), physical activity (P = 0.295), daily vegetable intake per capita (P = 0.341), and daily fruit intake per capita (P = 0.246), which did not pass the statistical tests; the remaining variables were statistically significant. Table 3 provides additional information.
Factors influencing HRQOL among rural Uyghur residents
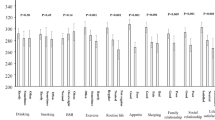
Mobility, self-care, usual activity, pain/discomfort, and depression/anxiety were set as the dependent variables in the binary logistic models. Table 4 presents the results. Women were most likely to have problems with mobility (OR = 0.365, 95% CI = 0.245,0.543), self-care (OR = 0.513, 95% CI = 0.347,0.757), and pain/discomfort (OR = 0.596, 95% CI = 0.407,0.874). Health status decreased with age, and self-reported health in the five dimensions of the EQ-5D was poor. Furthermore, healthy behavioural lifestyles were significantly associated with EQ-5D distribution status. Daily intake of vegetables per capita and daily intake of fruits per capita were related to usual activity (OR = 1.002, 95% CI = 1.000,1.004; OR = 1.001, 95% CI = 1.000,1.002) and depression/anxiety (OR = 0.998, 95% CI = 0.995,1.000; OR = 0.999, 95% CI = 0.998,1.000). Last, residents suffering from NCDs had health issues in mobility (OR = 2.520, 95% CI = 1.589,3.998), self-care (OR = 2.745, 95%CI = 1.761,4.277), usual activity (OR = 2.103,95% CI = 1.355,3.266), and pain/discomfort (OR = 2.789, 95%CI = 1.849,4.205). Residents with low self-rated health scores were more likely to be unhealthy in terms of self-care (OR = 0.656, 95% CI = 0.590,0.730), usual activity (OR = 0.670, 95% CI = 0.603,0.744) and pain/discomfort (OR = 0.676, 95% CI = 0.610,0.748). Residents who did not participate in community activities had health problems according to the five dimensions of the EQ-5D
Table 4 presents the results of the Tobit regression model. We found that gender (coef. = − 0.0948, 95% CI = − 0.1403, − 0.0493), age (coef. = − 0.0031 95% CI = − 0.0049, − 0.0013), married (coef. = − 0.0125, 95% CI = − 0.2168, − 0.0342), divorced/death of a spouse (coef. = − 0.1903, 95% CI = − 0.3111, − 0.0694), exercise (coef. = 0.0971, 95% CI = 0.0543,0.1399), sleep time from 7 to 9 h (coef. = 0.1382, 95% CI = 0.0711,0.2053), daily intake of fruits per capita (coef. = − 0.0001, 95% CI = − 0.0002,0), daily intake of oil per capita (coef. = − 0.0006, 95% CI = − 0.0012,0), distance to the nearest medical facility of 2–4 km (coef. = 0.047, 95% CI = 0.0045,0.0895), distance to the nearest medical facility of > 4 km (coef. = 0.1426, 95% CI = 0.0833, − 0.2019), NCDs (coef. = 0.1576, 95% CI = 0.1059,0.2093), self-rated health scores (coef. = 0.0852, 95% CI = 0.0737,0.0968), and participation in community activities (coef. = − 0.1991, 95% CI = − 0.2530, − 0.1452) were statistically significant, and these variables correlated with the health utility index of rural Uyghur residents.
Discussion
Health utility index and EQ-5D distribution of rural Uighur residents
This study demonstrated that the health utility index of rural Uighur residents (− 0.197, 1) was lower than that of Urban and Rural Residents in Shaanxi (− 0.149, 1) [25]. A higher proportion of respondents had problems with Mobility (52.8%) and Usual Activity (57.5%), physical health is relatively poor. It is due to the poor climatic conditions in the area where the inhabitants live and the high consumption of fatty foods, which similar to the research of the HRQOL of Ethnic Minorities in Yunnan Province [26]. In addition, rural Uyghur residents consume less vegetables, have less awareness of health literacy, lack better body management and physical exercise, leading to obesity, less range of mobility and ability to usual activity [27]. We found that rural Uyghurs had fewer problems with depression and anxiety (69.2%). This might be explained by the Uyghur population's positive attitude toward life, a strong sense of self-sufficiency, and the simple cultural concept of ‘cheerfulness and contentment’, which was influenced by the unique culture [28], thus reducing the incidence of mental illness among them. The EQ-5D distribution showed that the low-income group had a higher rate of problems in the three dimensions of mobility, self-care, and usual activity than the non-low-income group, but the differences in health utility index between the two groups were not statistically significant, and differences in usual activity and self-care were statistically significant. Activity limitations due to illness and poor self-care may be the main factors influencing HRQOL in the local population.
Association between poverty and HRQOL of the residents
We found that the health utility index was (− 0.182, 1) of low-income groups and (− 0.197, 1) of non-low-income groups. Non-low-income residents had higher mobility, self-care, usual activity, and health utility index scores than those in the low-income group, it could be found that the health status of the low-income group is lower than that of the high-income group, indicating that health has a significant positive effect on the overall evaluation of poor residents [29]. Income was statistically significant only in the ‘Depression/Anxiety’ dimension among EQ-5D but not a factor affecting health utility value of residents in the tobit models. For all respondents, higher incomes were associated with better mental and self-rated health scores, For the low-income group, their poor economic conditions, higher psychological burden and stress levels [30], inadequate knowledge and awareness of mental health, less access to mental health services led to vulnerability to depression/anxiety. The government should pay attention to the health status of people living with poverty and illness, the sense of access in the pursuit of a better life and think about how to give this group of people the ability, opportunity and confidence to live happily from the level of policy formulation and implementation.
Determinant factors of quality of life in rural Uyghur residents
Several factors affect the health status of rural Uyghur residents in remote western areas. First, sex, age, marital status, and family size affected the health status of rural Uyghur residents in remote western areas, which is consistent with previous studies [31]. Physical function tends to decline with age. The older the participants, the more health problems reported on the EQ-5D. Marital status and household size also affected the health status of rural Uyghur residents with married residents having better health than those who were divorced or widowed. This might be because Uyghur residents had developed an ethnically distinctive family culture over the course of their long, productive lives. Culture based on the values of ‘respect for the elderly’, ‘love for each other, ‘and ‘filial piety’ [6] had a subtle influence on their way of life.
Second, health behaviour and lifestyle informed the health status of rural Uyghur residents. The average daily intake of vegetables for rural Uighurs was 100 g, lower than the normal level for Chinese residents, and the daily intake of edible oil was 55.6 g, much higher than the recommended daily intake of 25–30 g of edible oil for adults in the Dietary Guidelines for Chinese Residents, it is similar to the dietary habits of ethnic minorities in the farming and pastoral areas of Qinghai [32]. It was explained that Uyghur residents tend to eat high-calorie foods, such as pasta, grilled rice, naan, beef, and mutton. However, a diet high in carbohydrates and low in vegetables can lead to overweight and obesity. The BMI of the residents was in the overweight range of 24.5 kg/cm2. Moreover, physical activity affected the health status of rural Uyghur residents with 67.5% of respondents not practising physical activity. Hence, residents in the area are recommended to promote beneficial changes in their health status by consuming less high-calorie and high-fat food and more vitamin-rich food, such as vegetables and fruits; performing sensible exercise; and engaging in healthy behavioural lifestyles [33].
Last, having chronic illness, hospitalisation within six months, distance to the nearest health facility, self-rated health scores, and social support affected the HRQOL of rural Uyghur residents, which is consistent with a study on quality of life profile of general Vietnamese population [34]. Vietnamese population has Lower HRQOL composite scores were related to have chronic diseases, and multiple health issues and using health service. Similarly, in our research, the Tobit regression model showed that NCDs were an impact factor on the health utility index of rural Uyghur residents. NCDs involve high rates of disability and mortality and are typically associated with a wide range of complications, imposing a heavy financial burden. The prevalence of NCDs among Uyghur residents was 25.3%, slightly higher than the 24.5% in the Fifth National Health Service Survey [35] and lower than the 39.32% prevalence among the low-income population [36]. The study found that residents with chronic conditions had problems with mobility, self-care, usual activity, and pain/discomfort, yet the prevalence of chronic conditions was lower than that in similar studies. This suggests that the implementation of pro-poor health policies and NCD prevention strategies had a significant impact. This demonstrates that the health poverty alleviation policy and NCD prevention strategies have had a significant impact. Policymakers target health policies to improve the HRQOL of low-income individuals according to local population characteristics [37]. Tobit regression models also showed that the distance to the nearest health facility and self-rated health scores affected the low health utility index of Uyghur residents, which is similar with evaluation of quality of life among Dong Elderly Population in Guizhou province, accessibility of health services is their HRQOL factors [38]. Low-income people with chronic illnesses are eager to access health services, and the Company Health Office or Community Health Centre still needs to focus on low-income people [39], popularising knowledge about the prevention and treatment of NCDs, enhancing self-care awareness, changing poor lifestyles [40], and improving the HRQOL of low-income Uyghur residents.
This study enriches the research on the HRQOL of ethnic minority populations, especially the quality of life of Uyghur populations in remote areas. It provides information for governments, policymakers, and medical institutions to reduce health inequities and improve the health status of the population. This study has various advantages. First, a sufficient sample of residents and well-trained staff with standardised tools made the results more authentic and convincing. Second, the analysis of five different dimensions can identify the factors affecting HRQOL in a more specific manner.
Nevertheless, this study has some limitations. The study was cross-sectional and could not determine the causal relationship between HRQOL and influencing factors. More common diseases were integrated into NCDs, and there was no separate exploration of NCDs; thus, the diverse effects of different diseases might have been neglected.
Conclusion
The HRQOL of the rural Uyghur residents was lower than that of the general population. Various factors affecting HRQOL include sex, age, marital status, physical activity, sleep time, daily fruit intake per capita, daily cooking oil intake per capita, NCD, self-rated health score, and participation in social activities. Thus, first, relevant organisations should continue to pay more attention to vulnerable groups such as women, elderly individuals, and low-income groups in the current poverty-alleviation policy and conduct appropriate health education for them [41]. Second, the Uighur population should change their poor dietary habits, reduce their intake of high-fat foods, and increase their intake of vitamin-rich foods such as vegetables and fruits. Finally, this study aimed to enhance the prevention and control of chronic diseases in the low-income Uyghur population. The region should pursue health poverty alleviation policies and focus on sick, low-income residents to improve the health, ability, opportunity, and confidence of this population to live well.
Availability of data and materials
The datasets used during the current study are available from the corresponding author on reasonable request. The Chinese questionnaire copy may be requested from the authors.
Change history
08 May 2023
Editor’s Note: Concerns have been raised about the ethics approval and informed consent procedures related to the research reported in this paper. Editorial action will be taken as appropriate once an investigation of the concerns is complete and all parties have been given an opportunity to respond in full.
25 August 2023
This article has been retracted. Please see the Retraction Notice for more detail: https://doi.org/10.1186/s12889-023-16559-x
Abbreviations
- HRQOL:
-
Health-rated quality of life
- BMI:
-
Body mass index
- NCDs:
-
Non-communicable chronic diseases
References
Average life expectancy is 77.3 years: China’s main health indicators rank among the top among middle- and high-income countries. 2020. http://www.gov.cn/xinwen/2020-10/14/content_5551367.htm. Accessed 23 Jan 2022.
Health poverty alleviation—overcoming difficulties—poverty alleviation exhibition. In: People’s daily online. 2022. http://fpzg.cpad.gov.cn/429463/429470/429503/index.html. Accessed 10 Feb 2023.
Wu CJ. Policy optimization for public health insurance-based on perspective of combatting illness-led poverty risk in whole life-cycle. Chin Public Admin. 2016;11:94–100.
Wang P. Health poverty alleviation projects will be implemented to prevent poor rural people from falling into poverty due to illness and returning to poverty. 2022. http://www.nhc.gov.cn/xcs/2017hydt/201703/399de486b5e044a89dfed9e8c1ff596e.shtml. Accessed 23 Jan 2022.
He D, et al. Research report on health poverty alleviation in China. Beijing: People’s Publishing House; 2019.
Wang M, He B, Wang Y, et al. Depression among low-income female Muslim Uyghur and Kazakh informal caregivers of disabled elders in Far Western China: influence on the caregivers’ burden and the disabled elders’ quality of life. PLOS One. 2016;11:e0156382. https://doi.org/10.1371/journal.pone.0156382.
Sang S, Kang N, Liao W, et al. The influencing factors of health-related quality of life among rural hypertensive individuals: a cross-sectional study. Health Qual Life Outcomes. 2021;19:244. https://doi.org/10.1186/s12955-021-01879-6.
Cunillera O, Tresserras R, Rajmil L, et al. Discriminative capacity of the EQ-5D, SF-6D, and SF-12 as measures of health status in population health survey. Qual Life Res. 2010;19(6):853–64. https://doi.org/10.1007/s11136-010-9639-z.
Herdman M, Gudex C, Lloyd A, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res. 2011;20(10):1727–36. https://doi.org/10.1007/s11136-011-9903-x.
Subramaniam M, Abdin E, Poon LY, et al. EQ-5D as a measure of programme outcome: Results from the Singapore early psychosis intervention programme. Psychiatry Res. 2014;215:46–51.
Wang H, Patrick D, Edwards T, et al. Validation of the EQ-5D in a general population sample in urban China. Qual Life Res. 2012;21:155–60.
Health N, Center FPCSI. 2013 The fifth national health service survey analysis report. Beijing: Peking Union Medical College Press; 2015.
McCaffrey N, Kaambwa B, Currow DC, et al. Health-related quality of life measured using the EQ-5D-5L: South Australian population norms. Health Qual Life Outcomes. 2016;14(1):133.
Luo N, Liu G, Li M, et al. Estimating an EQ-5D-5L Value Set for China. Value Health. 2017;20(4):662–9. https://doi.org/10.1016/j.jval.2016.11.016.
Niao W. Health-related quality of life and its influencing factors a among residents over 65 years old in Henan Province. Zhengzhou: Zhengzhou University; 2017.
Zhang Y, Zhou Z, Gao J, et al. Health-related quality of life and its influencing factors for patients with hypertension: evidence from the urban and rural areas of Shaanxi Province, China. BMC Health Serv Res. 2016;16; https://doi.org/10.1186/s12913-016-1536-x.
Lu Y, Wang N, Chen Y, et al. Health-related quality of life in type-2 diabetes patients: a cross-sectional study in East China. BMC Endocr Disord. 2017;17:38. https://doi.org/10.1186/s12902-017-0187-1.
Liao W, Liu X, Kang N, et al. Independent and combined effects of sleep quality and night sleep duration on health-related quality of life in rural areas: a large-scale cross-sectional study. Health Qual Life Outcomes. 2022;20:31. https://doi.org/10.1186/s12955-022-01936-8.
Zhou T, Guan HJ, Liu GG, et al. Comparison analysis on the EQ-5D-5L and the EQ-5D-3L for general population in China. Chin Health Econ. 2016;35:17–20.
Li MH, Luo N. Introduction to the Chinese version of the European five dimensional health scale (EQ-5D). China J Pharm Econ. 2009;1:49–57. https://doi.org/10.3969/j.issn.1673-5846.2009.01.007.
Wang H, Kindig DA, Mullahy J, et al. The production of Chinese health related quality of life as measured by EQ-5D in Beijing, China. World Economic Papers. 2006;1:37–53. https://doi.org/10.3969/j.issn.0488-6364.2006.01.004.
Teni FS, Gerdtham U, Leidl R, et al. Inequality and heterogeneity in health-related quality of life: findings based on a large sample of cross-sectional EQ-5D-5L data from the Swedish general population. Qual Life Res. 2022;31(3):697–712. https://doi.org/10.1007/s11136-021-02982-3.
Cheng KJG, Rivera AS, Miguel RTDP, Lam HY. A cross-sectional study on the determinants of health-related quality of life in the Philippines using the EQ-5D-5L. Qual Life Res. 2021;30:2137–47. https://doi.org/10.1007/s11136-021-02799-0.
The People’s Government of Xinjiang Uygur Autonomous Region of China. Xinjiang raised the subsistence allowance for urban and rural residents to ensure the basic livelihood of people in need. 2020.
Zhou ZL, Zhou ZY, Li D, et al. Analyzing the health-related quality of life of urban and rural residents in Shaanxi: estimation based on the EQ-5D value sets. Chin Health Econ. 2015;34:13–6.
Sang SP. The study of health-related quality of life and its impact factors on people in minority areas.[D]. Wuhan: Wuhan University; 2014.
Su Tianyuan, Zhuang Wei, Zhang Qiqi, et al. Study on health-rated quality of life of Xinjiang residents based in the EQ-5D health scale integral system. J Xinjiang Med Univ. 2020;43(01):106–9+114.
Li XH, Gong CT, Zheng KL, et al. The quality of life and its influencing factors of Uygur ethnic group’s elderly people in Xinjiang. Chin Gen Pract. 2014;17:1884–8.
Ren Tian, Hu Jin-liang, Huang Mao-juan. overty, disease and health poverty alleviation policy: Based on quality of life evaluation for the poor residents. Chin J Health Policy. 2018;11(05):61–4.
Yang JL, Li XJ, Mao L, et al. Factors associated with depression in middle-aged and the elderly with hypertension. Chinese Prev Med. 2021;22(11):827–32.
Zhang C, Cheng XY, Zhou Q, et al. Study on health-related quality of life and associated factors of rural population with different income levels in central and Western China. Chin Health Econ. 2020;39:22–6.
Zong-fang LU, Lai WEI, Chong-yu CHEN, et al. Study on HRQoL of elderly patients with chronic disease in agricultural and pastoral areas of Qinghai Province based on EQ-5D scale. Medicine and. 2021;34(11):11–5. https://doi.org/10.13723/j.yxysh.2021.11.003.
Steptoe A, Perkins-Porras L, Hilton S, et al. Quality of life and self-rated health in relation to changes in fruit and vegetable intake and in plasma vitamins C and E in a randomised trial of behavioural and nutritional education counselling. Br J Nutr. 2004;92:177–84. https://doi.org/10.1079/BJN20041177.
Nguyen LH, Tran BX, Le Hoang QN, et al. Quality of life profile of general Vietnamese population using EQ-5D-5L. Health Qual Life Outcomes. 2017;15(1):199. https://doi.org/10.1186/s12955-017-0771-0.PMID:29020996;PMCID:PMC5637080.
National Health and Family Planning Commission Statistical Information Center. Peking Union Medical College Press, 2015; 2013 The fifth national health service survey analysis report [M].
Zhang XY, Yan J, Liu JJ, et al. Status of health-related quality of life and its influencing factors of residents in Jiangxi Province based on Tobit regression. Med Soc. 2021;34:15–9.
Wang J, Dong JY, Shen C, et al. Study on health-related quality of life base on EQ-5D among middle-aged and the elderly in a poor country in Jiangsu Province. Chin J Soc Med. 2022;39:38–42.
Shao-hui Z, Yang H, Lei-lei L, et al. Evaluation of Quality of Life Among Dong Elderly Population in Guizhou Province. Med Soc. 2021;34(01):65-71. https://doi.org/10.13723/j.yxysh.2021.01.014.
Li HM, Gao Y, Mao Q, et al. Health status and utilization of health services in low-income people. Chin Gen Pract. 2020;23:2576–81.
Liu Q, Zhang GS, Su M, et al. Analysis of health cost of low-income population in Urumqi. China Health Ind. 2017;14:151–2.
Dou WJ, Han ZY, Song KM, et al. Research on health related quality of life and its influencing factors among rural residents in Shandong Province. Chin J Gen Pract. 2017;15:911–4.
Acknowledgements
We sincerely thank all the interviewers and respondents who participated in the field survey. Thanks to the people who have supported this research work.
Funding
This study was funded by Shihezi University Youth Innovative Top Talent Project (No. CXBJ202005).
Author information
Authors and Affiliations
Contributions
JXD was responsible for the article conception and design, result analysis and paper writing; XJL was responsible for the feasibility analysis and revision of the article, JLY and RF were responsible for the data collection and collation, JXD and XJL were responsible for the quality control and review of the article, and XJL is responsible for the overall supervision and management of the article.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was conducted in accordance with the Declaration of Helsinki. And this study was approved by the Ethics Committee of the First Affiliated Hospital of Shihezi University School of Medicine (No. KJ2021-135-01). All of the participants provided their written informed consent prior to the start of the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article has been retracted. Please see the retraction notice for more detail:https://doi.org/10.1186/s12889-023-16559-x
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Dong, J., Li, X., Fan, R. et al. RETRACTED ARTICLE: Health-related quality of life among ethnic minority residents in remote Western China: a cross-sectional study. BMC Public Health 23, 638 (2023). https://doi.org/10.1186/s12889-023-15544-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-023-15544-8