Abstract
Objective
To evaluate the impact of Hurricanes Irma/Maria on diabetes incidence in Puerto Rico. Mortality increased substantially after the hurricanes, but morbidity was not assessed.
Methods
We recruited 364 participants from the San Juan Overweight Adults Longitudinal Study (SOALS) aged 40–65 years who completed a three-year follow-up and were free of diabetes. We conducted additional questionnaires 1.7–2.5 years after hurricanes. Glycosylated hemoglobin (HbA1c), fasting glucose and insulin were assessed at all three visits. We compared diabetes incidence between pre-hurricane visits and between visits spanning the hurricanes using Generalized Estimating Equation (GEE) adjusting for within person repeated measures, age, and body mass index (BMI).
Results
Diabetes incidence was significantly higher spanning the hurricanes than pre-hurricane (multivariate GEE model: IRR = 2.1; 95% CI: 1.4–3.1). There was a significantly higher increase spanning the hurricanes compared to pre-hurricanes for Homeostatic Model Assessment of Insulin Resistance (HOMA-IR) (median: 0.3 uIU/mL vs. 0.2 uIU/mL). HbA1c levels increased by 0.4% spanning the hurricanes.
Conclusion
Increases in diabetes incidence, HOMA-IR and HbA1c were higher spanning the hurricanes compared to the pre-hurricanes period. The increase in diabetes incidence remains significant after adjusting for age and BMI.
Similar content being viewed by others
Introduction
Prior studies suggest that hurricanes could lead to increased diabetes incidence and related complications, hospitalization, and mortality [1,2,3,4,5,6,7]. After natural disasters, anxiety, overeating, interruption of medications, and disruption of water supply and access to nutritious food could lead to glucose abnormalities; this in turn could lead to increased risk for diabetes and related comorbidities or complications and hospitalizations [1,2,3]. People with diabetes need to follow medical treatment and diet recommendations to manage their diabetes and keep their glucose and glycosylated hemoglobin (HbA1c) levels within an acceptable range. This might be more challenging after natural disasters. Also, insulin may be difficult to obtain after hurricanes, and difficult to store adequately during power outages, which could lead to poor control of diabetes.
In the week after Hurricane Sandy, the rate of diabetes diagnosis in the emergency room visits in New Jersey increased by 84% [1]. Patients with diabetes had more serious complications after hurricanes due to disrupted health care services and limited resources [4]. Moreover, the annual rate of death from diabetes in the 12 months following Hurricane Iniki in Kauai in 1992, was 2.6 (95% CI: 1.4–4.7) times higher than the median annual rate in 1987–1991 [5]. After the 2004 hurricane season in Florida, 5% of the indirect mortality from storm-related deaths were from diabetes [6].
Several studies have identified barriers that prevent people from preparing adequately for a natural disaster [8,9,10,11]. In 2012, a review suggested that only 30-40% of United States (US) residents had emergency supplies at any given time [9]. Low preparedness is common even in areas that have previously experienced natural disasters, such as hurricanes [10]. Exposure to natural disasters is a consistent predictor of individual adverse health outcomes, including the development or worsening of chronic diseases [12, 13]. It seems likely that high risk individuals without diabetes could experience impaired glucose metabolism, elevated HbA1c levels and increased risk for diabetes.
Puerto Rico (PR) is located in a hurricane prone area in the Caribbean and Atlantic basin. In September 2017, Hurricanes Irma and Maria impacted Puerto Rico leaving a large part of the population without power, water, and/or telecommunications for over six months in some areas, with disruption of primary health care services, and food supply. By December 2017, the PR government reported 64 attributed deaths to Hurricane Maria. However, in 2018 a study from George Washington University estimated 2,975 deaths, which was later accepted as the official death toll [14]. Diabetes is the third highest cause of death in Puerto Rico [15]. One recent study in the US Virgin Islands, found that the high rates of diabetes related morbidities after Hurricanes Irma and Maria were perceived to be due to the lack of availability of insulin [16]. The prevalence of diabetes in Puerto Rico was 15.5% (95% CI: 14.3-16.6%) in 2018 [17], compared to 10.5% in the general US population [18]. People who are less prepared may be more likely to have a health impact due to hurricanes [19], and may likely have increased risk for diabetes.
Despite the high burden of hurricanes and diabetes in Puerto Rico, the impact of hurricanes on diabetes incidence has not been assessed. US studies relating natural disasters and diabetes mostly focused on people with diabetes and did not evaluate diabetes incidence. This study prospectively evaluates the impact of Hurricanes Irma and Maria on diabetes incidence and management in Puerto Rico.
Research design and methods
Study population
The Preparedness to Reduce Exposures and diseases Post-hurricanes and Augment Resilience (PREPARE) study was launched to longitudinally evaluate the impact of Hurricanes Irma and Maria on health in Puerto Rico, and to evaluate hurricane preparedness in this context. Diabetes was of key interest in PREPARE; the study design, population and methods are described in our prior publication [19].
PREPARE study was conducted among participants who were enrolled in a previous cohort study named San Juan Overweight Adults Longitudinal Study (SOALS). SOALS had pertinent pre-hurricane data from assessments conducted at baseline (2011 to 2013) and at three-year follow-up visits (2014 to 2016). SOALS recruited overweight/obese Hispanic adults aged 40 to 65 years, without diabetes mellitus (DM) and major conditions including cardiovascular disease. At baseline, participants reporting physician-diagnosed type 1 or type 2 diabetes, taking insulin or oral anti-hyperglycemic agents, or classified as having diabetes based on study assessments were excluded. At SOALS follow-up exam, participants reporting a diagnosis of diabetes, were given a medical referral and advice to consult their health care provider to seek a definitive diagnosis. We requested participants to send us a copy of their laboratory test results. If the diabetes was not confirmed, we invited the participant to undergo the oral glucose tolerance test and glucose assessments and classified their diabetes status based on study measures.
Participants who were considered free of diabetes at the follow-up visit and had previously consented to be contacted for future studies were potentially eligible for PREPARE study (N = 869). Since SOALS consisted of adults drawn primarily from San Juan and neighboring areas, and since the hurricane impact varied by location, we stratified the sampling by location to get better representation across Puerto Rico. We aimed to recruit 125 SOALS participants from three locations: the capital city (San Juan), the rest of the San Juan Metropolitan area (including Bayamón, Carolina, Cataño, Guaynabo and Trujillo Alto) and from municipalities of Puerto Rico outside of San Juan Metropolitan Area.
Procedures
Recruitment and post-hurricane data collection for PREPARE were conducted in a health clinic of the University between May 2019 and July 2020, 17–34 months after the hurricanes. After completing written informed consent, and confirmation of eligibility, trained interviewers conducted computer-aided interviews in Spanish using REDCap. We also assessed blood pressure, blood glucose and HbA1c levels, and anthropometric measures. Hence, we could compare measures across 3 timepoints (SOALS baseline, SOALS follow-up and PREPARE visit) and two time periods: (1) baseline to follow-up (pre-hurricanes: follow-up minus baseline; median 3.0 years) and (2) follow-up to PREPARE visits (spanning hurricanes: PREPARE minus follow-up; median 4.7 years).
The study was impacted due to a series of earthquakes that impacted Puerto Rico in January 2020, and the government mandated lockdown starting March 15, 2020 due to the COVID-19 pandemic. Due to this we decided to drop the visits for the 11 pending participants, hence, PREPARE study included a total of 364 participants.
Diabetes assessments in SOALS and PREPARE
For all visits, participants were asked to fast for 10 hours prior to their appointments, and through the last blood draw. For SOALS baseline and follow-up, blood samples were drawn at fasting, and after a 75 g oral glucose tolerance test (OGTT) at 30-mins, 1 and 2 hours. Only fasting blood was drawn in PREPARE for assessment of glucose, insulin and HbA1C. To compare diabetes prevalence and incidence measures, since OGTT was only assessed pre hurricanes, we used the fasting glucose and HbA1c measures to classify diabetes across all time points and time periods. We considered participants who had study assessed fasting glucose ≥ 126 mg/dl, or HbA1c > 6.5% (48 mmol/mol) as having diabetes. People were classified as having pre-diabetes if they had fasting glucose 100–126 mg/dl or HbA1c 5.7–6.5% (39–48 mmol/mol), or as having normal glycemia if all these values were below the mentioned thresholds for pre-diabetes [20]. Homeostatic Model Assessment of Insulin Resistance (HOMA-IR) was calculated using fasting values as [glucose (nmol/L) * insulin (µU/mL)/22.5] [21].
Statistical methods
People with missing data for key variables were excluded or dropped from the pertinent analyses. Descriptive analyses were performed using PREPARE data. To assess the pre-hurricanes diabetes incidence rate (IR), we included 968 eligible participants without diabetes at baseline who completed the SOALS follow-up. For the incidence rate spanning the hurricanes, three participants who reported diabetes in the post-hurricanes visit but did not have study measures consistent with diabetes were excluded from this analysis. Since we excluded people who developed diabetes prior to each time point for incidence measures, the participants varied across the two time-points. Hence we computed adjusted incidence rate ratio (IRR) using a generalized estimating equation (GEE) model adjusting for within person repeated measures and key potential time varying confounders, age and body mass index (BMI) [22]. We also evaluated crude incidence rate within subgroups of income and education using survival analysis to see any differences in diabetes development across these subgroups.
Changes in fasting glucose, HOMA-IR and HbA1c were computed in the same 364 people for the two time periods. Normality of the changes were evaluated using Shapiro-Wilk test. Since the evaluated measures were not normally distributed, Wilcoxon signed-rank tests were conducted to compare changes in these measures across the two time periods. Since the effect of the hurricanes on HOMA-IR and HbA1c may vary across gender, education, income, and location, we used Wilcoxon rank-sum test to evaluate whether changes in HOMA-IR, and HbA1c levels spanning the hurricanes were different across subgroups defined by these factors. A significance level of ≤ 0.05 was used in all analyses. We used Stata software version 16.1 to conduct statistical analyses, and R-Studio for the figures.
Results
The mean age at the time of PREPARE visit was 58.7 years (SD = 6.8) and 76.9% were women (Table 1). Over half of the participants (51.9%) reported a family income of $20,000 or more, while 73.9% had higher than high school education; 42.0% were employed and 39.3% were retired/disabled. Almost half (47.8%) the participants were classified as having pre-diabetes prior to the hurricanes, and 66.4% at the time of the post-hurricane visit.
Between the pre-hurricanes visits, there were 61 new diabetes cases (IR = 2.1 per 100 person-years; 95% CI: 1.7, 2.8), compared to 44 new cases spanning the hurricanes (IR = 6.7 per 100 person-years; 95% CI: 5.0–9.0), which translates to IRR of 3.1 per 100 person-years; 95% CI: 2.1–4.7 (Table 2). Incidence rate ratio (IRR) comparing the incidence rates before and spanning the hurricanes adjusted for within person repeated measures using GEE was 2.0 (95% CI: 1.4–2.8), and additionally adjusting for age and BMI was 2.1 (95% CI: 1.4–3.1).
Participants reporting annual family income below $20,000 had higher incidence spanning the hurricanes (IR = 7.6 per 100 person-years; 95% CI: 5.1–11.3) compared to those with higher income (IR = 5.9 per 100 person-years; 95% CI: 3.8–9.1) (Table 3). Similarly, participants with high school or less education (IR = 7.4 per 100 person-years; 95% CI: 4.3–12.7) had higher incidence spanning the hurricanes compared to those with higher education (IR = 6.5 per 100 person-years; 95% CI: 4.5–9.2). Participants with a family income below $20,000 had an IRR of 4.2 (95% CI: 2.3–7.8) comparing the incidence rates before and spanning the hurricanes, while participants with higher income had lower IRR 2.4 (95% CI: 1.3–4.2). For participants with high school or less education, IRR comparing the incidence rates before and spanning the hurricanes was also higher (IRR = 3.5; 95% CI: 1.8–6.6), than for participants with higher education (IRR = 2.4; 95% CI: 1.1–6.1).
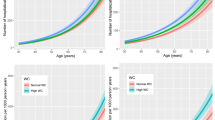
There was a significant increase in the changes between pre-hurricanes visits to changes between visits spanning the hurricanes for HOMA-IR (p = 0.05) and HbA1c levels (p < 0.001) (Fig. 1). HOMA-IR levels increased more spanning the hurricanes (median 0.3 uIU/mL), compared to pre-hurricane (0.2 uIU/mL). HbA1c levels decreased by 0.2% (median) between the pre-hurricane visits and increased by 0.4% spanning the hurricanes. Changes in fasting glucose levels remained similar (5.0 mg/dL) across the two time periods. Females had a significantly higher increase in HbA1c (median increase = 0.4%) spanning the hurricanes compared to males (median increase = 0.3%). Similarly, HOMA-IR levels increased significantly more in females (median increase = 0.3) than in males (median increase = 0.03). HOMA-IR and HbA1c changes spanning the hurricanes were similar across subgroups defined by education, location, and income (not shown in tables).
Discussion
Prior studies had documented the impact of natural disasters on patient with diabetes. A recent study after Hurricanes Irma and Maria in the US Virgin Islands [16] reported that physicians and medical record staff perceived higher rates of diabetes-related morbidities. The same study also found a significant increase in the percentage of patients’ visits for endocrine, nutritional, and metabolic diseases; more than half of the visits were attributable to diabetes or related illnesses. Previous studies have found that people with diabetes needed support in the week after disasters due to increased risk of myocardial infarction [23]. In the aftermath of Hurricane Katrina, one of the main concerns for people with diabetes was obtaining insulin/medication and appropriate care for their condition. However, the impact of natural disasters on diabetes incidence is an understudy topic. According to the Behavioral Risk Factor Surveillance System (BRFSS), the prevalence of diabetes in Puerto Rico, for 2019, was 16.7% (95% CI: 15.6-17.8%), which is 1.2% higher than in 2018 [17]. To our knowledge, this is the first study to report a significant increase in diabetes incidence after a natural disaster and to highlight diabetes incidence after natural disasters in PR - a US territory prone to hurricanes with a majority Latino population and high federal poverty rate.
Changes in fasting glucose and HOMA-IR spanning the hurricanes were significantly higher than changes between the pre-hurricane visits. HbA1c increased more spanning hurricanes compared to earlier. The average time between the pre-hurricane visits was 3.0 years (SD = 0.25), whereas it was 4.7 years (SD = 0.46) between the visit spanning the hurricanes. However, the difference in the incidence rates cannot be attributed to the difference in the two time periods since the incidence rate ratio considers the time in the denominator. Considering that the higher incidence persisted after adjusting for age and BMI, the incidence may likely have increased due to the impact of the hurricanes. This is supported by the fact that participants with less income and education had higher increase in diabetes incidence spanning the hurricanes despite having lower pre-hurricanes incidence compared to participants with higher income and education. Since we compared glucose abnormalities across time points within the same individuals, results from these comparisons are also unlikely to be confounded. Our data is not representative of the whole Puerto Rican population which may affect generalizability. However, the associations are still likely to be valid.
Literature has usually focused on natural disasters and the impact on patients with diabetes [4, 6, 7]. However, given our findings of increase in diabetes incidence after the hurricanes, it is important to consider that high-risk people may likely further increase their risk of developing diabetes after hurricanes due to a combination of factors such as lack of water, power, nutritious foods, physical and mental stress. Tanaka and colleagues found that the high amount of stress after a hurricane activates the body’s “fight-or-flight” system for longer periods of time, which can lead to the development of diabetes [24]. Social determinants of health like income and education can also have an effect in the population’s health, as after natural disasters low-income people tend to have a higher impact. Our results showed that the incidence rate of participants with lower income and educational attainment increased significantly after the hurricanes demonstrating that social economic disparities resulted in higher risk for developing diabetes.
Detrimental changes in diet due to hurricanes could also have contributed to increased risk for diabetes. In the aftermath of the hurricanes in Puerto Rico, most (41%) of the food received at a federal distribution center were snacks and sweets [25]. Only 13% of the food was fruits, 4% vegetables, 13% proteins and 7% grains; 46% of these foods were high in sodium, saturated fat or added sugar [25]. In PREPARE, long-term diet changes were similar among people who had diabetes, pre-diabetes or normoglycemia before the hurricanes. No associations were found between long-term diet changes post-hurricanes and the changes in HbA1c spanning the hurricanes. In one study, HbA1c and fasting insulin levels rose significantly post-hurricanes [7]; however, we did not find any studies evaluating HOMA-IR or fasting glucose after hurricanes.
Our results suggest that the incidence of diabetes may have increased in Puerto Rico following Hurricanes Irma and Maria. The results were adjusted for age, suggesting that the increase in diabetes incidence spanning the hurricanes was beyond the expected increase in diabetes incidence due to aging. These findings have high public health relevance, as high-risk adults, those with lower socio-economic resources and people with pre-diabetes should take additional preparedness measures for natural disasters to sustain healthy levels of HbA1c. After a natural disaster the medical attention is often concentrated in treating acute injury and illness, leaving fewer resources to prioritize chronic conditions prevention and management. In 2007, the Disaster Response Task Force from the American Diabetes Association released a statement on Emergency and Disaster Preparedness, which contained a guide for people with diabetes [26]. A similar guide is needed for patients at high-risk of diabetes, which can incorporate recommendations such as storing nutritious food options that have a long shelf-life, staying well hydrated, and stress management skills to prevent the development of diabetes and its complications. The relevance of these findings also can extend globally and add to existing evidence that natural disasters could have a detrimental impact on the population’s health and increase social disparities. Additional research and global efforts are needed to further understand the impact of diabetes incidence after natural disaster.
Data Availability
The datasets generated and/or analyzed during the current study are not publicly available as the grant just ended in 2021 and the primary manuscripts are still in progress, but the data are available from the corresponding author on reasonable request.
Abbreviations
- BMI:
-
Body mass index
- BRFSS:
-
Behavioral Risk Factor Surveillance System
- GEE:
-
Generalized Estimating Equation
- HbA1c:
-
Glycosylated hemoglobin
- HOMA-IR:
-
Homeostatic Model Assessment of Insulin Resistance
- IR:
-
Incidence Rate
- IRR:
-
Incidence Rate Ratio
- PR:
-
Puerto Rico
- PREPARE:
-
Preparedness to Reduce Exposures and diseases Post-hurricanes and Augment Resilience
- OGTT:
-
Oral glucose tolerance test
- SOALS:
-
San Juan Overweight Adults Longitudinal Study
- CI:
-
Confidence interval
References
Velez-Valle EM, Shendell D, Echeverria S, Santorelli M. Type II diabetes emergency room visits associated with Hurricane Sandy in New Jersey: implications for preparedness. J Environ Health. 2016;79(2):30–7.
Guha-Sapir D, van Panhuis WG, Lagoutte J. Short communication: patterns of chronic and acute diseases after natural disasters - a study from the International Committee of the Red Cross field hospital in Banda Aceh after the 2004 Indian Ocean tsunami. Trop Med Int Health. 2007;12(11):1338–41.
Kaufman FR, Devgan S. An increase in newly onset IDDM admissions following the Los Angeles earthquake. Diabetes Care. 1995;18(3):422.
Fonseca VA, Smith H, Kuhadiya N, Leger SM, Yau CL, Reynolds K, Shi L, McDuffie RH, Thethi T, John-Kalarickal J. Impact of a natural disaster on diabetes: exacerbation of disparities and long-term consequences. Diabetes Care. 2009;32(9):1632–8.
Hendrickson LA, Vogt RL. Mortality of Kauai residents in the 12-month period following Hurricane Iniki. Am J Epidemiol. 1996;144(2):188–91.
McKinney N, Houser C, Meyer-Arendt K. Direct and indirect mortality in Florida during the 2004 hurricane season. Int J Biometeorol. 2011;55(4):533–46.
Miller AC, Arquilla B. Chronic diseases and natural hazards: impact of disasters on diabetic, renal, and cardiac patients. Prehosp Disaster Med. 2008;23(2):185.
Ablah E, Konda K, Kelley CL. Factors predicting individual emergency preparedness: a multi-state analysis of 2006 BRFSS data. Biosecurity and bioterrorism: biodefense strategy, practice, and science 2009, 7(3):317-330.
Levac J, Toal-Sullivan D, OSullivan TL. Household emergency preparedness: a literature review. J Community Health. 2012;37(3):725–33.
Kapucu N. Culture of preparedness: household disaster preparedness.Disaster Prevention and Management: An International Journal2008.
Kohn S, Eaton JL, Feroz S, Bainbridge AA, Hoolachan J, Barnett DJ. Personal disaster preparedness: an integrative review of the literature. Disaster Med Pub Health Prep. 2012;6(3):217–31.
Raker EJ, Zacher M, Lowe SR. Lessons from Hurricane Katrina for predicting the indirect health consequences of the COVID-19 pandemic. Proceedings of the National Academy of Sciences 2020, 117(23):12595-12597.
Norris FH, Sherrieb K, Galea S. Prevalence and consequences of disaster-related illness and injury from Hurricane Ike. Rehabil Psychol. 2010;55(3):221.
Santos-Burgoa C, Goldman A, Andrade E, Barrett N, Colon-Ramos U, Edberg M, Garcia-Meza A, Goldman L, Roess A, Sandberg J. Ascertainment of the estimated excess mortality from hurricane Maria in Puerto Rico. 2018.
Annual Vital Statistics Report: Deaths, years 2015 and 2016. [http://www.salud.gov.pr/Estadisticas-Registros-y-Publicaciones/Pages/Estadisticas-Vitales.aspx] Accessed 05 March 2021.
Chowdhury MAB, Fiore AJ, Cohen SA, Wheatley C, Wheatley B, Balakrishnan MP, Chami M, Scieszka L, Drabin M, Roberts KA, et al. Health Impact of Hurricanes Irma and Maria on St Thomas and St John, US Virgin Islands, 2017-2018. Am J Public Health. 2019;109(12):1725–32.
BRFSS Prevalence & Trends Data. [https://www.cdc.gov/brfss/brfssprevalence/] Accessed 05 March 2021.
Statistics About Diabetes. [https://www.diabetes.org/resources/statistics/statistics-about-diabetes] Accessed 08 October 2020.
Joshipura K, Martínez-Lozano M, Ríos-Jiménez PI, Camacho-Monclova DM, Alvarado-González C, Lowe SR. Preparedness, hurricanes Irma and Maria, and impact on health in Puerto Rico International Journal of Disaster Risk Reduction 2022, 67.
Understanding A1C Diagnosis. [https://diabetes.org/diabetes/a1c/diagnosis] Accessed 08 October 2020.
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28(7):412–9.
Kautzky-Willer A, Harreiter J, Pacini G. Sex and gender differences in risk, pathophysiology and complications of type 2 diabetes Mellitus. Endocr Rev. 2016;37(3):278–316.
Lee DC, Gupta VK, Carr BG, Malik S, Ferguson B, Wall SP, Smith SW, Goldfrank LR. Acute post-disaster medical needs of patients with diabetes: emergency department use in New York City by diabetic adults after Hurricane Sandy. BMJ Open Diabetes Res Care. 2016;4(1):e000248.
Tanaka M, Imai J, Satoh M, Hashimoto T, Izumi T, Sawada S, Uno K, Hasegawa Y, Kaneko K, Yamada T, et al. Impacts of the Great East Japan Earthquake on diabetic patients. J Diabetes Investig. 2015;6(5):577–86.
Colon-Ramos U, Roess AA, Robien K, Marghella PD, Waldman RJ, Merrigan KA. Foods distributed during Federal Disaster Relief response in Puerto Rico after Hurricane Maria did not fully Meet Federal Nutrition Recommendations. J Acad Nutr Diet. 2019;119(11):1903–15.
Disaster Response Task F. American Diabetes Association Statement on Emergency and Disaster preparedness: a report of the disaster response Task Force. Diabetes Care. 2007;30(9):2395–8.
Acknowledgements
The authors acknowledge Sarah Lowe, Jeanpaul Fernández, Dahianira Camacho, Paula Ríos, Omar Acevedo, Gabriela Morales, Fabiana De La Matta, Eduardo Rodríguez, Coralys Ortiz, Karla Perez, Ibanaliz Santoni, Angel Aguayo, Kiany Serrano, Fabiola Morales, Radamés Revilla, Dr. Karen Martínez, Dr. Hilton Franqui Rivera, Dr. Ángel López Candales, the PRCTRC laboratory and nursing personnel and COSSMA staff and volunteers Anna B. Flores Rolón, Isolina Miranda Sotillo, Dr. Diomarie Martínez Reyes, Dr. Héctor O. Santos Reyes, Lic. Norma Antomattei Velázquez, José Antonio Santiago Vázquez, Charlynne De Jesús Ramos, Héctor R. Álvarez Vázquez, Krystal M. Morales López, Daraishka M. Pérez Caraballo, Gedaliz Leon Ortolaza, Idaliz Ortiz De Villate, Nataly A. Delgado Hernández, Jaisy Vega, and Valerie Molina.
Funding
Research reported in this publication was supported by the National Institute on Minority Health and Health Disparities Grants R21MD013666, U54MD007587, U54MD007600 and 1U54GM133807-01A1, and the National Institute of Dental and Craniofacial Research Grant R01DE020111.
Author information
Authors and Affiliations
Contributions
Dr. Kaumudi Joshipura is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. M.M.L. contributed to the data analyses plan, conducted the data analyses, prepared the figure and tables, and wrote the initial draft of the manuscript. K.J. conceived and designed the study, obtained funding, and contributed to analyses plan and interpretation. C.N coordinated and contributed to the data collection and interpretation. G.A.G. contributed to data collection and interpretation. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All methods were carried out in accordance with relevant guidelines and regulations in the Declaration of Helsinki pertaining to research involving human participants. Informed consent was obtained from all the participants. The study was approved by the University of Puerto Rico Medical Sciences Campus Institutional Review Board.
Consent for publication
Not Applicable.
Competing interests
The authors have no competing interests to declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Martínez-Lozano, M., Noboa, C., Alvarado-González, G. et al. Hurricanes Irma and Maria and Diabetes incidence in Puerto Rico. BMC Public Health 23, 1019 (2023). https://doi.org/10.1186/s12889-023-15542-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-023-15542-w