Abstract
Background
Covid-19 vaccination is the main strategy to reduce SARS-CoV-2 transmission, mortality and morbidity. This study aimed to examine sociodemographic differences in Covid-19 vaccine uptake among all individuals invited for Covid-19 vaccination in Denmark.
Methods
This study was designed as a nationwide register-based cohort study. The study population included all Danish residents aged 12 years or above in Denmark between December 27, 2020 and October 20, 2021. Individuals who died during the study period before receiving an invitation for Covid-19 vaccination were excluded. Associations between sociodemographic factors and Covid-19 vaccination uptake were analyzed using logistic regression models adjusting for age, sex, immigration status, educational level, disposable income and history of SARS-CoV-2 infection.
Results
The study population included 5,164,558 individuals. The overall vaccination coverage was 87.1% by October 20, 2021. In the full adjusted logistic regression models, the highest ORs for non-vaccination were observed among individuals aged 12–24 years (OR: 8.99 (95% CI: 8.76–9.23)), descendants of non-western immigrants (OR: 5.26 (95% CI: 5.18–5.33)), individuals who never had a PCR-test performed (OR: 2.93 (95% CI: 2.90–2.96)), individuals with primary school as highest completed educational level (OR: 2.87 (95% CI: 2.83–2.91)) and individuals with disposable income < 33,605 EUR (OR: 3.72 (95% CI: 3.52–3.93)).
Conclusion
Overall, the Covid-19 vaccine uptake was high in Denmark. However, large sociodemographic differences in the vaccine uptake exist. The youngest age groups had the lowest vaccination coverage. Furthermore, the impact of the sociodemographic factors was more pronounced in the youngest age groups. The identified determinants may be used to design policies to help maximize the vaccination coverage.
Similar content being viewed by others
Background
A key challenge is to ensure sufficient vaccine uptake in the population to reduce SARS-CoV-2 transmission, mortality and morbidity from Covid-19 [1]. A national Covid-19 vaccination program was introduced in Denmark on 27 December 2020. The Danish Health Authority prioritized nursing home residents, individuals aged 85 years or above, vulnerable and frontline personnel first for vaccination followed by age groups younger than 85 years in decreasing order. By October 20, 2021, 87.1% of the Danish population invited for vaccination (individuals aged 12 years or above) had received at least the first Covid-19 vaccine dose. Understanding which sociodemographic, factors are associated with low vaccination coverage has major implications for designing policies that help maximize the vaccination coverage. Previous studies in this field of research have investigated attitudes and potential acceptance toward Covid-19 vaccination [2,3,4]. Showing clear sociodemographic differences in intention to accept a vaccine for Covid-19 with the intention being higher in those with higher income levels [3, 4] and higher education levels [2,3,4]. A Scottish study showed that white ethnicity was positively associated with vaccine acceptance compared with Black, Asian, and minority ethnic groups [4]. However, a study from the US showed that especially Asian and American Indian/Alaska Native racial groups were positively associated with Covid-19 vaccine acceptance compared to Black/African Americans [2]. Sociodemographic differences in actual Covid-19 vaccination uptake have only been examined in older adults [5,6,7]. These studies demonstrate that the greatest disparities in Covid-19 vaccine uptake were observed with younger age [7], male sex [5], lower income [5,6,7] and living alone [6, 7] certain religious groups [6] and between ethnic groups [5, 6]. It is important to examine associations between sociodemographic factors and Covid-19 vaccine uptake for all ages because other associations may exist in younger age groups. The aim of this study was to examine sociodemographic differences in Covid-19 vaccine uptake among all individuals invited for Covid-19 vaccination in Denmark.
Methods
Study design and population
The study was designed as a nationwide register-based cohort study. The study population included all residents invited for Covid-19 vaccination (individuals aged 12 years or above) in Denmark between December 27, 2020 and October 20, 2021. Individuals who died during the study period before receiving an invitation for Covid-19 vaccination were excluded.
Data sources
Individual-based data from nationwide Danish registries were linked using the unique personal identification number collected from the Danish Civil Registration System (CRS) [8]. Information on sex, date of birth, immigration status, geographical region of residence, marital status and number of individuals in the household was obtained from CRS [8]. All administered Covid-19 vaccines are registered in the Danish Vaccination Registry (DVR) on an individual level, identified by the CRS number [9]. Information on educational level and disposable income were obtained from Statistics Denmark [10]. Information about previous SARS-CoV-2 infections (sample date and test results) was obtained from the Danish Microbiology Database (MiBa) [11]. MiBa is a national database containing real-time information on all microbiological laboratory test results from all clinical microbiology departments and private test centers. Information on chronic diseases within 5 years prior to study entry was obtained from the Danish National Patient Registry (DNPR) [12]. For each hospital contact, one primary and one or more optional secondary diagnoses are provided and coded according to the International Classification of Diseases, 10th revision (ICD-10) [12]. The ICD-10 codes used to define the included chronic diseases are shown in Supplementary (Table S2). The date of death for exclusion before invitation to Covid-19 vaccination was obtained from CRS [8]. All data were uploaded to Statistics Denmark for data management and analysis.
Outcome
The outcome in this study was having received at least one dose of a Covid-19 vaccine (BNT162b2 mRNA, mRNA-1273, ChAdOx1 or Ad26.COV2.S) between December 27, 2020 and 20 October, 2021.
Sociodemographic variables
The sociodemographic characteristics included in this study as predictors for non-vaccination were sex, age, immigration status, chronic diseases, infection status, educational level, disposable income, geographical region, marital status and living alone/not alone. Sex was defined as female or male. The age groups were divided into 12-15 years, 16–24 years, 25–34 years, 35–44 years, 45–54 years, 55–64 years, 65–74 years, 75–84 years and 85 years and above. Covid-19 vaccination was approved later for individuals aged 12–15 years (May 2021) [13]. Although the vaccine was approved for this age group while the vaccine roll-out was ongoing, the 12–15 years old were the last in Denmark to be invited for Covid-19 vaccination (July 2021). Therefore, we examined this age group separately. Immigration status was defined as Danish, immigrants of western descent, descendants of western immigrants, immigrants of non-western descent, descendants of non-western immigrants (see Supplementary, Table S1). Chronic diseases were defined as having at least one chronic disease or no chronic disease (see supplementary, Table S2). History of SARS-CoV-2 infection was defined as no history of SARS-CoV-2 infection before vaccination, history of SARS-CoV-2 infection before vaccination and never PCR-tested. The infections were diagnosed by PCR tests. The highest completed educational level was defined as master or Ph.D., bachelor, secondary school, vocational school and primary school. Disposable income was defined as 1,000,000 DDK or above (> 134,416 EUR), 700,000-999,999 DDK (94,091–134,416 EUR), 450,000-699,999 DDK (60,487 − 94,090 EUR), 250,000-449,999 DDK (33,605 − 60,486 EUR) and < 250,000 DDK (< 33,605 EUR). The income was converted to EUR to give a better perception. The exchange rate for 1 EUR was 7,44 DDK on February 2023 according to the central bank of Denmark. The majority of the population is represented in the lowest income group. However, we did not have information about the exact disposable income. Therefore, we were not able to create another division. The geographical region of residence was defined as Capital Region of Denmark, Region Zealand, Northern Denmark Region, Central Denmark Region and Region of Southern Denmark. Finally, marital status was defined as with a partner, divorced or widow/widower and unmarried) and living alone was defined as living alone and not living alone.
Statistical analysis
For each level of the sociodemographic variables numbers and proportions of vaccinated were calculated. In addition, stratified analyses presenting proportions vaccinated across sociodemographic variables were prepared to explore the combined effect of the different variables. Four logistic regression models were used to estimate odds ratio (OR) with 95% confidence intervals (95% CI) to explore the associations between each sociodemographic factor and non-vaccination. The first model was unadjusted. The second model was adjusting for age groups and sex. The third model was adjusting for age, sex, immigration status, educational level and disposable income. Finally, the fourth model was adjusting for age, sex, immigration status, educational level, disposable income and history of SARS-CoV-2 infection. Individuals were excluded from the logistic regression models if any information on the adjusting sociodemographic factors was missing (Fig. 1). This exclusion was done to guarantee that the same number of individuals were included in all four models to ensure that changes in the OR estimates were explained by adjustment and not differences in the included individuals. Coefficients and standard error (SE) from the logistic regression models were reported for educational level and disposable income to examine any collinearity (See supplementary, Table S3).
All analyses were performed using R statistical software version 2022.02.1.
Results
The study population for the descriptive statistics included 5,164,558 residents in Denmark invited for Covid-19 vaccination (12 years or above) and the study population for the logistic regression models included 4.887.387 individuals without missing values on the sociodemographic covariates used for adjustment (Fig. 1).
The oldest age groups were vaccinated in the early stage of the vaccination program from end of December 2020 until mid-April 2021 and reached a higher vaccination coverage than the younger age groups. All age groups have been invited for vaccination by July 2021 (Fig. 2).
Descriptive statistics
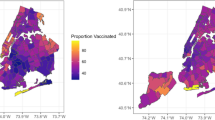
The mean age in the study population was 47 (SD: 20.7) years and 50.5% were women. By October 20, 2021, 87.1% of the study population had received at least the first dose of a Covid-19 vaccine. The vaccination coverage was similar among males and females. The vaccination coverage was lower among younger age groups: 12–15 years (70.0% vaccinated), 16–24 years (82.0% vaccinated), 25–34 years (75.7% vaccinated) and 35–44 years (84.1% vaccinated) (Table 1). Furthermore, individuals with other immigration status than Danish had lower vaccination coverage: immigrants of western descent (68.5% vaccinated), descendants of western immigrants (73.9% vaccinated), immigrants of non-western descent (73.9% vaccinated) and descendants of non-western immigrants (49.2% vaccinated). Lower vaccination coverage was also observed among individuals without chronic diseases (86.0% vaccinated), individuals with upper secondary school (85.0% vaccinated) or primary school (83.9% vaccinated) as highest completed educational level, disposable income < 33,605 EUR (85.0% vaccinated) and among individuals with history of SARS-CoV-2 infection before vaccination (79.5% vaccinated) and individuals who never had been PCR-tested (69.6% vaccinated). Vaccine uptake was lower among unmarried individuals (79.3% vaccinated). The vaccine uptake was 88.9% and 87.0% among individuals living alone and not living alone, respectively. The vaccination coverage was ranging between 85.5% and 88.7% across all five geographical regions (Table 1). Larger differences in vaccine uptake exist within sociodemographic factors across age groups and immigration status. Especially immigrants and descendants of immigrants aged 12–15 years, 16–34 years or 35–54 years had a lower vaccine uptake (Figs. 3, 4 and 5). Descendants of non-western immigrants aged 16–34 years with primary school as the highest educational level had a vaccine uptake of 41% whereas the vaccine uptake was 69% among descendants of non-western immigrants with master or Ph.D levels. However, the highest vaccine uptake within all educational levels in descendants of non-western immigrants is lower than the lowest vaccine uptake in Danish individuals regardless of educational level (Fig. 3). Among immigrants of western descent aged 16–34 years only 24% were vaccinated if they had history of SARS-CoV-2 infection whereas 74% were vaccinated if they had no history of SARS-CoV-2 infection.
Results from logistic regression models
The unadjusted logistic regression models showed that male sex was associated with an OR of 1.14 (95% CI: 1.13–1.14) for non-vaccination compared to females. The OR estimate was slightly lower after full adjustment (model 4) (Table 2). The highest OR for non-vaccination was observed among individuals aged 12–15 years, 16–24 years, 25–34 years and 35–44 years compared to individuals aged 85 years or above. Large differences in the OR estimates for the associations between age groups and non-vaccination was observed before and after adjustment for sociodemographic covariates. In the unadjusted model, OR was 5.20 (95% CI: 5.07–5.33) for individuals aged 25–34 years and 3.04 (95% CI: 3.00-3.12) for individuals aged 35–44 years. In the full adjusted model (model 4) the OR estimates increased to 8.99 (95% CI: 8.76–9.23) for individuals aged 25–34 years and 6.09 (95% CI: 5.94–6.26) for individuals aged 35–44 years (Table 2). Immigrants of western and non-western descent and descendants of western and non-western immigrants had higher ORs of non-vaccination compared to Danish. The highest OR was observed among descendants of non-western immigrants with an OR of 10.38 (95% CI: 10.24–10.51) in the unadjusted model and 5.26 (95% CI: 5.18–5.33) in the full adjusted model (model 4) (Table 2). The OR estimates for the associations between immigrants of western and non-western descent and descendants of western immigrants and non-vaccination were similar before and after adjustments. Disposable income <33,605 EUR was associated with the highest OR of non-vaccination. The unadjusted model showed an OR of 6.29 (95% CI: 5.97–6.64) and the full adjusted model (model 4) showed an OR of 3.72 (95% CI: 3.52–3.93) compared to income above 134,416 EUR (Table 2). Smaller differences in the OR estimates between the models before and after adjustment was observed for history of SARS-CoV-2 infection and educational level. In the full adjusted model (model 4) vocational education was associated with an OR of 2.25 (95% CI: 2.22–2.28) and primary school was associated with an OR of 2.87 (95% CI: 2.83–2.91) for non-vaccination compared to master or Ph.D. level (Table 2). In the adjusted model (model 3), OR was 2.91 (95% CI: 2.88–2.93) for individuals with history of SARS-CoV-2 infection before vaccination and 2.93 (95% CI: 2.90–2.96) for individuals who had never been PCR tested compared to individuals with no history of SARS-CoV-2 infection before vaccination (Table 2). The SE were unchanged when including sociodemographic variables, which indicates that the educational level and income variable are not collinear (Table S3).
Discussion
This study contributed with new insights into the understanding of the sociodemographic complexity in Covid-19 vaccine uptake, showing marked differences in the uptake not only between, but also within sociodemographic groups. Non-vaccination was most pronounced among individuals of younger age, immigrants or descendants, individuals with low educational level, low income, history of SARS-CoV-2 infection and never PCR-tested. However, the impact of educational level, disposable income and history of SARS-CoV-2 infection was more pronounced in the youngest age groups 12–15, 16–34 and 35–54 years of age. Previous studies have only examined sociodemographic differences in Covid-19 vaccination uptake among older adults [5,6,7] whereas our study contributes with evidence of sociodemographic differences in vaccine uptake among both children and adults. However, a Swedish register-based cross-sectional study of adults aged 60 years or above showed that younger age (60–74 years compared to ≥ 75 years), low income and living alone were associated with non-vaccination [7], which is similar to our findings. Their results showed that low income was associated with an OR of 2.16 (95% CI: 2.10–2.23) for non-vaccination compared to medium/high income. High-income countries and low-middle-income countries of birth were associated with ORs of 2.15 (95% CI: 2.07–2.23) and 3.86 (3.71-4.00) for non-vaccination compared to Sweden as country of birth. Living alone was associated with an OR of 1.64 (95% CI: 1.59–1.68) for non-vaccination compared to not living alone. Furthermore, the Swedish study also observed a higher proportion of non-vaccinated individuals among those with history of Covid-19. A Danish study has demonstrated that previously infected individuals also benefit from COVID-19 vaccination [14], which underlines the importance that results from these studies are taken into account when designing future policies to increase vaccination uptake in these groups. Studies from England and Wales have shown marked differences in Covid-19 vaccine uptake between ethnic groups [5, 6]. These associations are consistent with our findings. Although, the ethnic groups are not necessarily similar to immigrants and descendants in Denmark in terms of country of origin or religious affiliation. Qualitative research is needed to examine underlying explanations for non-vaccination in the identified populations with low vaccine uptake. Promoting vaccine uptake among the identified populations with low vaccine uptake should include targeted multilingual campaigns and specific outreach strategies.
The observed differences between sociodemographic factors also exist for seasonal influenza, pneumococcal and herpes zoster vaccine uptake [15, 16]. In addition to the importance of sociodemographic factors, a Danish study demonstrated the importance of health communication [17]. The results showed that vaccine acceptance increased when individuals were exposed to transparent positive communication and transparent neutral communication. Whereas transparent negative communication and vague communication decrease vaccine acceptance [17]. These are both important factors when planning future vaccination campaigns.
Strengths and limitations
The strengths of this study consist of including all residents in Denmark invited for Covid-19 vaccination. Furthermore, data are register-based with high quality and completeness, resulting in few missing data.
We were able to include information on several sociodemographic characteristics. However, some factors were categorized into broad categories. This may have caused some of the finer differences in non-vaccination between groups to remain undetected. Furthermore, other unmeasured factors such as religion, attitude towards vaccination and trust in health authorities may also be important factors for the vaccine uptake. We identified several characteristics of non-vaccination. However, it may be difficult to identify individuals with e.g. low educational level, low disposable income or history of SARS-CoV-2 infection. Further research should identify more specific characteristics such as occupation to identify individuals with low vaccine uptake and to plan interventions or campaigns for these groups. Due to the data delivery processes, data availability only extends to October 20, 2021, and we are unable to assess if vaccination rates in certain groups indeed increased over time after this date.
In conclusion, the results demonstrated large sociodemographic differences in Covid-19 vaccination uptake, especially in the younger age groups, which have not previously been included in this field of research. Promoting vaccine uptake should include targeted multilingual campaigns and specific outreach strategies.
Data availability
The data that support the findings of this study are available from Statistics Denmark, the Danish Data Protection Agency and Danish Health and Medicines Authority but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of from Statistics Denmark, the Danish Data Protection Agency and Danish Health and Medicines Authority.
References
Strategy to Achieve Global Covid-19 Vaccination by mid-2022.
Malik AA, McFadden SM, Elharake J, Omer SB. Determinants of COVID-19 vaccine acceptance in the US. EClinicalMedicine. 2020;26:100495.
Lazarus JV, Ratzan SC, Palayew A, Gostin LO, Larson HJ, Rabin K, et al. A global survey of potential acceptance of a COVID-19 vaccine. Nat Med. 2021;27(2):225–8.
Williams L, Flowers P, McLeod J, Young D, Rollins L, The Catalyst Project T. Social Patterning and Stability of Intention to Accept a COVID-19 Vaccine in Scotland: Will Those Most at Risk Accept a Vaccine? Vaccines (Basel). 2021;9(1).
Perry M, Akbari A, Cottrell S, Gravenor MB, Roberts R, Lyons RA, et al. Inequalities in coverage of COVID-19 vaccination: a population register based cross-sectional study in Wales, UK. Vaccine. 2021;39(42):6256–61.
Nafilyan V, Dolby T, Razieh C, Gaughan CH, Morgan J, Ayoubkhani D, et al. Sociodemographic inequality in COVID-19 vaccination coverage among elderly adults in England: a national linked data study. BMJ Open. 2021;11(7):e053402.
Spetz M, Lundberg L, Nwaru C, Li H, Santosa A, Leach S, et al. The social patterning of Covid-19 vaccine uptake in older adults: a register-based cross-sectional study in Sweden. Lancet Reg Health Eur. 2022;15:100331.
Schmidt M, Pedersen L, Sørensen HT. The danish Civil Registration System as a tool in epidemiology. Eur J Epidemiol. 2014;29(8):541–9.
Grove Krause T, Jakobsen S, Haarh M, Mølbak K. The Danish vaccination register.Euro Surveill. 2012;17(17).
Thygesen L. The register-based system of demographic and social statistics in Denmark. Stat J UN Econ Comm Eur. 1995;12(1):49–55.
Schønning K, Dessau RB, Jensen TG, Thorsen NM, Wiuff C, Nielsen L, et al. Electronic reporting of diagnostic laboratory test results from all healthcare sectors is a cornerstone of national preparedness and control of COVID-19 in Denmark. Apmis. 2021;129(7):438–51.
Schmidt M, Schmidt SA, Sandegaard JL, Ehrenstein V, Pedersen L, Sørensen HT. The danish National Patient Registry: a review of content, data quality, and research potential. Clin Epidemiol. 2015;7:449–90.
First COVID-19 vaccine approved for children aged 12 to 15 in EU: European Medicines Agency; 2021 [cited 2023 January 31]. Available from: https://www.ema.europa.eu/en/news/first-covid-19-vaccine-approved-children-aged-12-15-eu.
Nielsen KF, Moustsen-Helms IR, Schelde AB, Gram MA, Emborg H-D, Nielsen J et al. Vaccine effectiveness against SARS-CoV-2 reinfection during periods of Alpha (B.1.1.7), Delta (B.1.617.2) or Omicron (B.1.1.529) dominance: A Danish nationwide study. medRxiv. 2022:2022.06.01.22275858.
Jain A, van Hoek AJ, Boccia D, Thomas SL. Lower vaccine uptake amongst older individuals living alone: a systematic review and meta-analysis of social determinants of vaccine uptake. Vaccine. 2017;35(18):2315–28.
La EM, Trantham L, Kurosky SK, Odom D, Aris E, Hogea C. An analysis of factors associated with influenza, pneumoccocal, tdap, and herpes zoster vaccine uptake in the US adult population and corresponding inter-state variability. Hum Vaccin Immunother. 2018;14(2):430–41.
Petersen MB, Bor A, Jørgensen F, Lindholt MF. Transparent communication about negative features of COVID-19 vaccines decreases acceptance but increases trust. Proc Natl Acad Sci U S A. 2021;118:29.
Bekendtgørelse af sundhedsloven. : The Danish Ministry of Health; [cited 2022 September 9]. Available from: https://www.retsinformation.dk/eli/lta/2019/903.
Acknowledgements
The authors are grateful to the Danish Health Data Authority for their help in defining the population. We would also like to thank the Department of Data Integration and Analysis at Statens Serum Institut for data management.
Funding
Not applicable as neither Statens Serum Institut nor any authors received funding for this study.
Author information
Authors and Affiliations
Contributions
Mie Agermose Gram and Hanne-Dorthe Emborg wrote the main manuscript text. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This article has been prepared on the basis of a study carried out as part of a task imposed on Statens Serum Institut according to the national legislation as specified in the Danish Health Care Act (Sundhedsloven § 222) [18]. The need for ethics approval and informed consent is therefore deemed unnecessary according to national legislation, cf. implementing decree, act no. 1338 of 2020-09-01 on research ethics review of health research projects. The article only contains aggregated results and no personal data. The article is therefore not covered by the European General Data Protection Regulation.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Gram, M.A., Moustsen-Helms, I.R., Valentiner-Branth, P. et al. Sociodemographic differences in Covid-19 vaccine uptake in Denmark: a nationwide register-based cohort study. BMC Public Health 23, 391 (2023). https://doi.org/10.1186/s12889-023-15301-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-023-15301-x