Abstract
Background
Postnatal care (PNC) is crucial for maternal and newborn health. Healthcare-seeking practices within the postpartum period help healthcare providers in early detection of complications related to childbirth and post-delivery period. This study aims to investigate trends of PNC utilization from 2006 to 2018, and to explore the effects of multi-level determinants of both maternal and newborn PNC in Pakistan.
Methods
Secondary data analysis of the last three waves of the nationally representative Pakistan Demographic and Health Surveys (PDHSs) was conducted Analysis was limited to all those women who had delivered a child during the last 5 years preceding each wave of PDHS Bivariate and multivariate logistic regression was applied to determine the association of maternal and newborn PNC utilization with multi-level determinants at individual, community, and institutional levels.
Results
In Pakistan, an upward linear trend in maternal PNC utilization was found, with an increase from 43.5 to 63.6% from 2006 to 2018. However, a non-linear trend was observed in newborn PNC utilization, with an upsurge from 20.6 to 50.5% from 2006 to 2013, nonetheless a decrease of 30.7% in 2018. Furthermore, the results highlighted that the likelihood of maternal and newborn PNC utilization was higher amongst older age women, who completed some years of schooling, were employed, had decision-making and emotional autonomy, had caesarean sections, and delivered at health facilities by skilled birth attendants. Multivariate analysis also revealed higher odds for women of older age, who had decision-making and emotional autonomy, and had caesarean section deliveries over the period of 2006–2018 for both maternal and newborn PNC utilization. Further, higher odds for maternal PNC utilization were found with parity and size of newborn, while less for ANC attendance and available means of transportation. Furthermore, increased odds were recorded for newborn PNC utilization with the number of children, ANC attendance, gender of child and mass media exposure from 2006 to 18.
Conclusion
A difference in maternal and newborn PNC utilization was found in Pakistan, attributed to multiple individual (socio-demographic and obstetrics), community, and institutional level determinants. Overall, findings suggest the need to promote the benefits of PNC for early diagnosis of postpartum complications and to plan effective public health interventions to enhance women’s access to healthcare facilities and skilled birth assistance to save mothers’ and newborns’ lives.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Background
Globally, approximately 810 women die every on average each day due to preventable causes related to pregnancy and childbirth [1]. The Maternal Mortality Ratio (MMR) is higher for the Asian region and even highest for the South Asian region, where almost one-fifth of the global maternal deaths occur. Similarly, neonatal deaths are also higher in Central and South Asia with 24 deaths per 1,000 live births [1].
The latest Pakistan Maternal Mortality Survey (2019) highlighted that although MMR has reduced from 276 deaths (as per 2006-07) to 186 deaths per 100,000 live births in the country, however, Pregnancy-Related Mortality Ratio (PRMR) is still higher with 255 deaths per 100,000 live births [2]. Further, the Newborn Mortality Rate (NMR) has also slowly reduced from 54 (as of 2006-07) to 41 deaths per 1,000 live births and the stillbirth rate to 31 pregnancy losses per 1,000 births in Pakistan [3]. Overall, statistics showed improvement over the period of time from 2006 to 07 to onwards, nonetheless, these are quite alarming, depicting that Pakistan is still lagging behind to achieve the Sustainable Development Goals (SDGs), ending preventable maternal and newborn deaths [4]. According to United Nations (UN), there is a dire need to address the issue of maternal and neonatal mortality as a top priority, reducing MMR to less than 70 deaths per 100,000 live births [2], and NMR to 12 deaths per 1,000 live births by 2030 [4].
A large strand of literature suggests preventing maternal and neonatal mortality, emphasizing skilled birth attendance, postnatal care facilities, provision, and access to modern contraception [4,5,6,7]. Evidence shows that most of the complications related to childbirth such as postpartum hemorrhage and various infections start instantly after birth, which put mothers’ and newborns’ health and lives at risk. These complications can be addressed by giving timely care to mothers and children in the period of postnatal care [7,8,9,10,11,12].
Postnatal care (PNC) is defined as care given during the first six weeks to the mother and her newborn, immediately after the birth of the placenta [13]. Literature suggests that the first 42 days after birth are very crucial, as the majority of maternal and neonatal deaths befalls during this period [14, 15]. Healthcare-seeking practices within the postpartum period help healthcare providers in early detection of complications related to childbirth and post-delivery period, enabling them to provide timely treatment to both mother and child to avoid any morbidity or mortality [14, 16]. In addition to saving mother and child from complications, PNC also provides opportunities for the new mothers to discuss their health-related issues, such as breastfeeding, required balanced nutrition, taking care of the child, and family planning [17].
Regardless of the importance of PNC for maternal and neonatal health, evidence revealed that most mothers and newborns do not obtain PNC from a skilled healthcare professional in developing countries [18, 19]. According to Pakistan Demographic Health Survey (PDHS) 2017-18, 36.4% of women and 69.3% of newborns did not receive PNC or a checkup by a health professional within six weeks after childbirth [20]. Further, there is also a disparity in terms of urban and rural areas of residence [20].
Pakistan, being a member state of the UN and signatory of SDGs, is committed to reducing maternal and newborn mortality rates to meet the UN target and address the issues of MMR and NMR. Predominantly, the SDGs are unmet due to maternal and neonatal deaths, and low-skilled birth assistance [21]. Therefore, it is imperative to provide skilled PNC to both mothers and newborns to ensure early diagnosis of complications for averting preventable maternal and neonatal deaths.
Given the context, there is limited research done on PNC in the country [22]. Although various studies have explored the maternal and newborn outcomes, particularly highlighting the significance of antenatal care and skilled birth assistance in Pakistan [23,24,25], there is a scarcity of research, examining trends of PNC for both mothers and newborns. Thus, bridging the gap in existing literature, this research article is aimed to examine trends of PNC utilization from 2006 to 2018 as well as explore the effects of multi-level determinants of both maternal and newborn PNC in Pakistan. This research is intended to unveil the trend of maternal and newborn PNC utilization from 2006 to 2018, examining the role of various underlying factors, contributing to and/or affecting the utilization of maternal and newborn PNC services at multi-levels, including individual (socio-demographics, obstetric), community and institutional levels.
Conceptual framework
Seeking guidance from the literature [26,27,28,29], the conceptual framework of this research encompasses multi-level hierarchical factors, affecting maternal and newborn PNC utilization in local cultural settings of Pakistan. These factors are related to access to maternal and newborn healthcare services, and the healthcare-seeking behavior of the respondents, along with community-level determinants. This research has conceptualized that maternal and newborn PNC utilization is linked with three levels of determinants, i.e. individual-level factors, community-level, and institutional-level factors. A list of explanatory variables for each factor has been selected based on Andersen’s health-seeking behavioral model [30,31,32,33,34].
The proposed conceptual framework accounts for individual women’s behavior, support from their families and community, as well as accessibility to maternal and newborn services in Pakistan. As illustrated in Fig. 1, the characteristics of the women and household factors (e.g., socio-demographic and obstetric) are considered as individual-level (level-1) predictors, whilst characteristics of the community are taken as group-level (level-2) predictors and facilities/institutional-level characteristics are grouped as level-3. This research conceptualizes that these three levels of predictors altogether contribute to maternal and newborn PNC utilization.
At an individual level, the socio-demographic characteristics included women’s age, women’s and husband’s educational status and occupation, women’s decision-making and emotional autonomy, available means of transportation, and wealth quintile. The obstetric characteristics comprised women’s age at marriage and first birth, parity, number of living children, birth order, antenatal attendance, sex/gender of newborn, and size of the newborn at birth.
At the community level, multiple factors have been considered, such as regions/provinces, residential geographical classification, mass media exposure, visit of a field worker, and perceived difficulty of distance to the health facility, hindering access to medical care.
Lastly, institutional level characteristics included mode of delivery, place of delivery, and skilled birth assistance.
Methods
For this particular research, a secondary data analysis of the last three waves of the nationally representative and cross-sectional Pakistan Demographic and Health Surveys (PDHSs) was conducted. These include wave 2 (2006-07) [35], wave 3 (2012-13) [36] and wave 4 (2017-18) [37]. Since the data on PNC related variables was not collected during wave 1 (1990–1991) of PDHS [38], therefore, it is not part of the present study.
Under the international series of MEASURES DHS Program, the National Institute of Population Studies (NIPS) carried out PDHSs, about every five years to allow comparisons over time [35,36,37], with the exception from PDHS 1990-91. ICF International and the Pakistan Bureau of Statistics provided technical assistance for these surveys, whereas United States Agency for International Development provided financial assistance [35,36,37].
The PDHSs is a series of the largest representative and publicly available datasets at the household level, collected information of ever-married women of reproductive age between 15 and 49 years, including maternal and newborn PNC. Each of the PDHS waves applied a two-stage cluster random sampling design to interview married women of reproductive age (MWRAs) [35,36,37]. Primarily, urban and rural sampling units were selected, and secondly, eligible households with MWRAs were chosen for surveys [35,36,37]. During each wave of PDHS, data was collected by different field teams, each consisting of a supervisor, field editor, and four interviewers (1 male and 3 females). Further quality controllers, regional/provincial field coordinators, and core teams of NIPS and ICF supervised these field teams for quality assurance [35,36,37]. Concurrently with fieldwork, data processing, editing, and double data entry were also completed [35,36,37]. A set of questionnaires were used to collect data at community, household, and individual (women and men) levels during each wave of PDHS. This particular research used a standard women questionnaire for secondary data analysis, administered to MWRAs (aged 15–49 years), through a face-to-face method [35,36,37]. This women’s questionnaire also comprised of questions regarding obstetric care including maternal and newborn PNC [35,36,37]. Overall, the response rate for each wave of PDHS ranged from 93 to 94.5% [35,36,37].
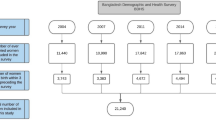
A sample of 10,023, 13,558 and 12,364 ever MWRAs were interviewed for PDHS 2006-07, 2012-13 and 2017-18 respectively [35,36,37]. However, this analysis is limited to all those women, who had delivered a child during the last 5 years preceding each wave of PDHS from 2006 to 2018, considering the research objectives. Thus, it yielded sample size 5,677, 7,446 and 6,711 women for PDHS 2006-07, 2012-13 and 2017-18 respectively [35,36,37], as shown in Fig. 2.
Variables
Outcome variables
There are two outcome variables for this research, i.e. maternal PNC and newborn PNC utilization. Maternal PNC utilization represents those ever MWRAs who gave birth during the five years preceding each wave of the PDHSs and utilized PNC after childbirth. Maternal PNC utilization was derived from the following questions: “Anyone checked respondent before discharge/delivery?” and “Anyone checked respondent after discharge/delivery?” The women, who received PNC services were coded as ‘yes’, while those women, who didn’t receive PNC were coded as ‘no’.
Another outcome variable is newborn PNC utilization within the last 2 months, which was also coded into binary responses, i.e. ‘yes and no’.
Explanatory variables
Considering the datasets of PDHS, the multi-level explanatory variables were organized into three hierarchical levels. The characteristics of the women and household factors were considered as individual-level (level-1) predictors, whilst characteristics of the community were taken as group-level (level-2) predictors and facilities/institutional level characteristics were grouped as level-3. Following are the details of each level:
-
1)
Individual-level characteristics.
The individual level (women and household) characteristics include socio-demographic and obstetric-related variables. The socio-demographic characteristics include women’s age in years (15–24 years, 25–34 years, 35 years and above), women’s and husband’s educational status (no formal schooling, up to 5 years of schooling, 6–10 years of schooling, more than 10 years of schooling), women’s and husband’s occupation (not working/unemployed, professional/clerical/sales & services, agriculture, manual or household worker). The available means of transportation for the household were coded into the binary category, i.e. no vehicle or own vehicle. Here, own vehicle indicates the availability of a bicycle, motorcycle/scooter, or car/truck at the household level, capable to transport mothers. The composite index of household amenities was grouped into five wealth quintiles (poorest, poorer, middle, richer, and richest).
Women’s domestic decision-making autonomy and emotional autonomy were also key predictors at the individual level. Women’s domestic decision-making autonomy measures the overall contribution of women in household decisions, such as spending one’s own and husbands’ earnings, making large household purchases, visiting family or relatives, and making decisions for healthcare. These were inferred from the following questions: i) “who (in your family) usually decides how to spend your earnings?”, ii) “who usually decides on making large household purchases?”, iii) “who usually decides on your visits to family or relatives?”, iv) “who usually decides on your healthcare?” and v) “who usually decides what to do with your husband/partner’s earnings?”. Possible responses to the first four questions were: respondent alone, husband/partner alone, respondent and husband/partner jointly, respondent and other person, someone else, family elders, or others. Nonetheless, for the last question regarding the decision of husband/partner’s earnings, an option of husband/partner does not bring in any money was also added along with other possible responses. For this research, all the responses to the above decision-making questions were dichotomized into one of two categories: whether the woman has ‘a say at all’ (either alone or jointly with the husband/partner or other person) was coded as ‘yes’ or whether she has ‘no say at all’ was coded as ‘no’ (in the case, when husband/partner, family elders or someone else makes the decision). This dichotomization of decision-making autonomy (yes/no) is consistent with the previous research work done using the DHS data [39, 40]. Based upon these five binary household decision-making indicator questions, a score of decision-making was computed for each woman, ranging from 0 to 5, where 0 showed ‘no say or autonomy’ and 1–5 reflected ‘say in any of the five household decisions or yes autonomy’. Cronbach’s alpha (α) for autonomy in domestic decision-making was found 0.88, 0.92, and 0.91 for PDHS 2006-07, 2012-13, and 2017-18 respectively, showing higher internal consistency.
Women’s emotional autonomy was assessed, using their attitudes against women violence.
Women’s agreement or disagreement represents their emotional autonomy [40]. It was inferred through the following five situations when sometimes a husband, being annoyed or angered, is justified in hitting or beating his wife: i) “if she goes out without telling husband?”, ii) “if she neglects the children?”, iii) “if she argues with husband?”, iv) “if she refuses to have sex with husband?” and v) “if she burns the food?”. Possible responses for each question were yes, no, and don’t know. For this research, yes and don’t know responses were given 0 scores, while no was scored as 1. Thus, a score ranged 0–5 was computed and dichotomized using the mean value. Thus, mothers, who had a score between 1 to 5 were categorized as ‘having emotional autonomy (disagree with wife-beating circumstances)’ and 0 scores indicated as ‘no emotional autonomy (agree with wife-beating situations). Cronbach Alpha (α) for emotional autonomy was found 0.913 and 0.908 for PDHS 2012-13 and PDHS 2017-18, indicating high reliability. It is pertinent to mention here that data against these variables were not collected during PDHS 2006-07 [35].
The obstetric characteristics included women’s age at marriage (< 20 years, 20 years and above), women’s age at first birth (< 20 years, 20 years and above), parity (1–2 children, 3–4 children, 5 children or above), number of living children (0, 1–2, 3–4, 5 or above), birth order (1, 2–3, 4–5, 6 or more), antenatal attendance (less than 4 visits or no visit, at least 4 visits or more), sex/gender of the newborn (female, male), and size of the newborn at birth (large, average, small).
-
2)
Community-level characteristics.
At community level, predictors encompassed regions/provinces (Punjab, Sindh, Baluchistan, Khyber Pakhtunkhwa, Gilgit Baltistan, Islamabad, FATA), respondents’ residential geographical classification (urban, rural), mass media exposure to radio, TV, newspaper (yes, no), and visit of the fieldworker, e.g., Lady Health Worker (LHW) in past 12 months (yes, no). DHS also measured the respondents’ perceived difficulty of distance to the health facility, hindering their access to medical care (problem, not a problem). It is pertinent to mention here that data against respondents’ mass media exposure and perceived difficulty of distance is not available for PDHS 2006-07 [35].
-
3)
Institutional-level characteristics.
The characteristics at the institutional level consisted of the mode of delivery (vaginal, caesarean section), place of delivery (either at home or public and private hospital/facility), and skilled birth assistance (no, yes). Here, Skilled Birth Assistance (SBA) referred to skilled health professionals, e.g., doctors, nurses, midwives, or Lady Health Visitors (LHVs).
Data analysis
For data analysis, IBM Statistical Package for Social Sciences (SPSS) version 21 was used and sampling weights were applied. Analysis was conducted at three levels, i.e. univariate, bivariate and multivariate. Firstly, univariate descriptive analysis was performed and presented, using frequencies and percentages. Secondly, cross-tabulation and chi-square test of association (p-value) was conducted, where a p-value ≤ 0.05 was found statistically significant. Lastly, bivariate and multivariate logistic regression was applied to determine the association of maternal and newborn PNC utilization with multi-level determinants at the individual, community, and institutional levels. During bivariate and multivariate regression analysis, odds ratios (ORs) and adjusted odds ratios (AOR) at 95% confidence intervals (CI) were calculated, separately for maternal and newborn PNC utilization. Multivariable logistic regression analysis was carried out after adjusting the visit of fieldworkers (e.g., LHWs) as a constant/fixed variable to obtain the AOR and 95%CI for both maternal and newborn PNC utilization. Further, variance inflation factor (VIF) – a measure to assess multicollinearity was also calculated before multivariate regression, which was reported as > 10 and acceptable [41].
Results
Sample characteristics at individual level
Table 1 indicated the individual level (socio-demographic and obstetric) characteristics of MWRAs (15–49 years), who gave birth during 5 years preceding the last three waves of PDHSs from 2006 to 2018. Here, wave 2 represents PDHS 2006-07, wave 3 indicates PDHS 2012-13, and wave 4 highlights PDHS 2017-18.
Table 1 showed that the majority of the MWRAs were aged between 25 and 34 years (52%, 54.2%, and 55.5%) and had not attained formal schooling (64.6%, 55.8%, and 47.9%), however, their husbands had completed 6–10 years of schooling, i.e. 33.7%, 34.3%, and 35.2%. in the last three waves respectively. A common trend was seen in terms of employment during the last three waves of PDHS, where a large number of MWRAs were found unemployed (71%, 72.2%, and 82.4%), while their husbands were mostly employed and working as manual/household workers (40.8%, 49.8%, and 47.7%). Further, mostly MWRAs belonged to the poorest wealth quintile (22.7%, 22.8%, and 21.5%), nonetheless, confirmed the availability of own vehicles for transportation (52.1%, 53.3%, and 65.2%).
With regards to autonomy, relevant data was not collected during PDHS 2006-07. Hence, analysis informed that a substantial proportion of the MWRAs (71.7% and 66%) had domestic decision-making autonomy, whereas 56.2% and 56.3% MWRAs had no emotional autonomy in waves 3 and 4 of PDHS respectively.
Regarding obstetric characteristics of MWRAs in the last three waves, most of the women were married at a younger age, i.e. <20 years (75.1%, 71.7%, and 64.4%). However, a slight variation was observed in women’s age at first birth, as 54.1% of women gave birth at < 20 years in wave 2, while 20 years and above (50.5% and 54.2%) gave birth in wave 3 and 4. More than one-third of MWRAs had 1–2 children ever born (35.2%, 38.7%, and 41%) and similarly 1–2 living children (37.7%, 42.3%, and 43.9%). Further analysis revealed that most of the women had either availed less than 4 antenatal visits or no visit (71.2% and 63.4%) in wave 2 and wave 3 respectively, nonetheless availed at least 4 visits or more (58.9%) in wave 4, showing an increase in antenatal care utilization over time. Furthermore, the majority of MWRAs had 2–3 birth orders (33.8%, 36.4%, and 38.3%), male newborns (54.1%, 51.9%, and 50.7%) with an average size (44.8%, 73%, and 72.7%) in all three waves of PDHS.
Characteristics at community and institutional level
Table 2 indicated community and institutional level characteristics of MWRAs (aged 15–49 years), who gave birth in the last 5 years preceding PDHSs from 2006 to 2018.
For community-level characteristics, a higher number of women were found from Punjab (56.1%, 56.1%, and 51.5%), and belonged to rural areas (69.8%, 69.9%, and 66.5%). The majority of the MWRAs had exposure to mass media (70.6% and 63.4%) and reported that distance to health facilities was not a problem (59.9% and 54.9%) from wave 3 and 4 respectively. Further, most of the MWRAs (73%) in wave 2 reported that they were not visited by the field workers, e.g., LHWs, nonetheless, an increase in the number of women attended by LHWs (56.8% and 61.8%) was observed in wave 3 and 4.
Regarding institutional level characteristics, a shift from home-based deliveries to hospital-based deliveries was observed from wave 2 to wave 4. Analysis showed that the majority of MWRAs reported that they had a vaginal delivery (91.5%, 84.3%, and 75.9%), however, mostly delivered at home (62.8%), without any SBA (58.1%) in wave 2. Contrary, a higher number of MWRAs were delivered at health facilities/hospitals (51.7% and 68.8%) by SBA (55.4% and 72%) in wave 3 and 4 respectively.
Maternal and newborn PNC related characteristics
Table 3 highlighted respondents’ characteristics related to maternal and newborn PNC utilization within the first 2 months from 2006 to 2018. Analysis reveals that the trend of maternal and newborn PNC utilization has changed over time from 2006 to 2018, as exhibited in Fig. 3.
The majority of respondents informed that they had not availed both maternal PNC (56.5%) and newborn PNC (79.4%) in wave 2, nevertheless, a gradual increase in the proportions of maternal PNC utilization (60.3% and 63.6%) was recorded in wave 3 and 4 respectively, showing an upward trend in maternal PNC utilization. In the case of newborn PNC utilization, a dip was observed, where more than half of the respondents reported that their newborns were checked (50.5%) in wave 3, while 69.3% were not checked after delivery in wave 4, highlighting a downward trend in newborn PNC.
Further, amongst those who availed PNC utilization, the majority availed PNC within the first 24 h (90.1%, 81.5%, and 59.1%), by skilled birth attendants (62.1%, 80%, and 90.6%). Furthermore, a large number of the women reported that their first PNC checkup took place at home (91.3%) in wave 2, nevertheless mostly visited a health facility for their first PNC checkup (78.5% and 79%) during wave 3 and 4 of PDHS.
Relationship of maternal and newborn PNC utilization with multi-level determinants
Table 4 indicated an association between maternal as well as newborn PNC utilization with individual-level characteristics of MWRAs aged 15–49 years. The results of chi-square showed a statistically significant relationship (p ≤ 0.05) of maternal and newborn PNC utilization with women’s and husband’s education status, women’s occupation, and wealth quintile in the last three waves of PDHS. Further, a strong statistical association between PNC utilization and decision-making, emotional autonomy and available means of transportation was also seen during 3 and 4 waves of PDHS. Furthermore, results of maternal and newborn PNC utilization showed a statistical significance with women’s age and husband’s occupation in varied waves of PDHS.
Findings highlighted an upward trend of maternal PNC utilization over the period of time, along with a strong association, particularly with women’s older age, higher years of schooling, professional/clerical/sales & services occupation, availability of transportation, and richest wealth quintile, whereas newborn PNC highlighted statistical significance with women’s and their husband’s higher years of schooling across last three waves of PDHS. Results also informed a substantial difference in patterns of newborn PNC utilization with women’s occupations across three waves. Results revealed that a large number of women having decision-making autonomy, nonetheless, without any emotional autonomy received maternal PNC in waves 3 and 4. Contrarily, a considerable variation along with low uptake of newborn PNC utilization was observed with women’s decision-making and emotional autonomy.
With respect to obstetric characteristics, a statistically significant association of maternal and newborn PNC utilization was found with women’s age at marriage, parity, number of living children, antenatal attendance and birth order in the last three waves of PDHS (2006–2018). Nonetheless, a significant relationship of maternal and newborn PNC utilization was also observed with women’s age at first birth, sex/gender and size of the newborn.
Table 5 showed a statistically significant relationship (p ≤ 0.05) between various community-level characteristics with maternal and newborn PNC utilization. Findings informed that majority of the women from Sindh (60.6%, 67.6%, and 75.6%), residing in urban areas (57.8%, 74.4%, and 76.8%) and visited by LHWs (47.5%, 65.2%, and 68.1%) availed maternal PNC utilization. Similar pattern was seen for newborn PNC, where majority of the women living in an urban area (26.4%, 58.3%, and 36.9%), particularly from Sindh province (34.2% and 40.4%) in waves 2 and 4, and Punjab province (58.1%) in wave 3 availed newborn PNC services. Further, those women, who had exposure to mass media and had not faced any difficulty accessing the facility also utilized maternal and newborn PNC during wave 3 and 4 of PDHS. Regarding institutional level characteristics, results highlighted that majority of the women, who had caesarean sections and delivered at health facilities by skilled birth attendants had a strong statistical association with maternal and newborn PNC utilization.
Bivariate logistic regression of maternal and newborn PNC utilization with multi-level determinants
Table 6 and 4.2 showed the bivariate analysis of maternal and newborn PNC utilization with multi-level determinants at the individual, community, and institutional levels of women of reproductive age 15–49 years, who gave birth during 5 years preceding PDHSs (2006–2018). Overall, the findings of maternal PNC utilization showed that women aged 35 years and above, who attained more than 10 years of schooling, served in professional/clerical/sales & services, and their husbands also had above 10 years of schooling, and were employed as professional/clerical/ sales & services, owned a vehicle for transportation and belonged to the richest wealth quintile were more likely to avail maternal PNC services in all three waves of PDHS. More specifically, maternal PNC utilization increased with the increase in age (OR: 0.66, 0.79, and 0.83), with a higher level of education (OR: 5.39, 9.42, and 6.78), in the category of professional/clerical/sales & services (OR: 1.73, 2.16, and 1.83) and with the increase in wealth quintile (OR: 4.18, 6.86, and 7.42) in all three waves. Additionally, those women, who had decision-making and emotional autonomy had more probability of maternal PNC utilization during waves 3 and 4.
Similar to the above, findings highlighted that probability to avail newborn PNC services augmented with the increase in women age (OR: 0.65), who attained 6–10 years of schooling (OR: 2.07) in wave 2, while more than 10 years of schooling in wave 3 and 4 (OR: 4.13 and 1.97), as well as their husbands also had more than 10 years of schooling (OR: 2.53, 2.61, and 1.43) across three waves of PDHS. Further, the odds of newborn PNC utilization were found higher amongst women serving as professional/clerical/sales & services (OR: 1.35 and 1.47) in waves 3 and 4, and their husbands also working in the same category (OR: 1.89, 2.31, and 0.86) and belonged to richest wealth quintile (OR: 2.35, 3.59, and 1.68) in all three waves of PDHS.
With reference to obstetric characteristics, results also revealed that maternal PNC utilization was found associated with women’s age at marriage and first birth, number of living children, antenatal attendance, birth order, sex/gender of newborn, and size of the newborn at birth. Further data suggested that maternal PNC utilization was higher among women having 1–2 children (OR: 1.69, 2.20, and 2.43) and large size of newborns at birth (OR: 1.19, 1.55, and 1.69) in the last three waves of PDHS. Moreover, results informed that newborn PNC utilization was associated with women age at marriage, the number of living children, antenatal attendance, and birth order. Further data highlighted that odds of newborn PNC utilization were found higher among women having 1–2 children (OR: 1.31, 1.54, and 1.71) in all three waves of PDHS.
Furthermore, Table 7 revealed that women from Sindh were more likely to avail maternal and newborn PNC utilization as compared to other provinces in all three waves. Also, an increased PNC utilization was found in all three waves amongst women residing in urban areas, visited by LHWs, had caesarean section, and delivered at hospital/facility by skilled birth attendants for both mothers and newborn.
Multivariate logistic regression of maternal PNC utilization with individual, community, and institutional level characteristics
Table 8 exhibited multivariate logistic regression of maternal PNC utilization with individual, community, and institutional level characteristics of women of reproductive age 15–49 years, who gave birth during 5 years preceding PDHSs (2006–2018). While interpreting the results of multivariate logistic regression, one may consider that multivariate analysis was conducted to obtain AOR after controlling for visits of field workers (LHWs). Further, VIF was calculated before multivariate regression to assess multicollinearity, which was found > 10.
Results (Table 8) informed a significant association of maternal PNC utilization with women’s age of 35 years and above (AOR = 0.46, 95% CI: 0.26–0.82) in wave 2, who attained education up to 5 years of schooling (AOR = 1.38, 95% CI: 1.00-1.94; AOR = 0.70, 95% CI: 0.55–0.88) in waves 2 and 3 respectively, and were employed in agriculture (AOR = 0.79, 95% CI: 0.62-1.00) and manual/household jobs (AOR = 0.76, 95% CI: 0.59–0.98) in wave 3, and their husbands employed as professional/clerical/sales & services (AOR = 4.57, 95% CI: 1.23–16.99) and manual/household jobs (AOR = 3.95, 95% CI: 1.07–14.57) in wave 4. Further, a higher likelihood of maternal PNC was found with availability of own vehicle for transportation (AOR = 0.79, 95% CI: 0.66–0.95; AOR = 1.28, 95% CI: 1.02–1.61) in waves 3 and 4, and richest wealth quintile in wave 4 (AOR = 1.69, 95% CI: 1.08–2.92). Women’s decision-making autonomy (AOR = 0.79, 95% CI: 0.66–0.95; AOR = 1.28, 95% CI: 1.02–1.61) in waves 3 and 4, and emotional autonomy jobs (AOR = 0.77, 95% CI: 0.62–0.95) in wave 4 was also significantly associated with maternal PNC utilization.
Multivariate analysis revealed that maternal PNC utilization showed a strong association with the obstetric characteristics in some waves, such as parity in wave 4, number of living children in waves 3 and 4, and the average size of the newborn at birth in waves 3 and 4. Only the antenatal attendance was found significant with maternal PNC utilization (AOR = 2.23, 95% CI: 1.63–3.03; AOR = 1.69, 95% CI: 1.39–2.05; AOR = 1.23, 95% CI: 1.00-1.52) across all waves of PDHS.
At the community level characteristics, regions/provinces, and perceived difficulty to access the distant health facility highlighted a significant association with maternal PNC utilization during multivariate analysis. More specifically, perceived difficulty was found significant in wave 3, while some of the regions/provinces had a strong association across all waves of PDHS. Further, nearly all characteristics of the institutional level (e.g., mode of delivery, skilled birth assistance) significantly predicted the maternal PNC utilization across waves of PDHS, except for a place of delivery.
Multivariate logistic regression of newborn PNC utilization with individual, community, and institutional level characteristics
Table 9 informed multivariate logistic regression findings of newborn PNC utilization with individual, community, and institutional level characteristics of women of reproductive age 15–49 years, who gave birth during 5 years preceding PDHSs (2006–2018), after adjusting the visits of field workers (LHWs).
Findings of multivariate analysis revealed that those mother, who aged 35 years and above (AOR = 1.84, 95% CI: 1.14–2.97) in wave 3, attained 6–10 years of schooling (AOR = 0.76, 95% CI: 0.59–0.99) in wave 4, serving as professional/clerical/sales & services (AOR = 1.67, 95% CI: 1.19–2.37) in wave 3 and manual/households jobs (AOR = 1.55, 95% CI: 1.16–2.06) in wave 4, belonged to middle wealth quintile (AOR = 0.69, 95% CI: 0.48-1.00) in wave 3 and had both decision-making (AOR = 1.56, 95% CI: 1.28–1.90) and emotional autonomy (AOR = 1.23, 95% CI: 1.03–1.47) in wave 4 are more likely to avail newborn PNC utilization in Pakistan.
Regarding obstetric characteristics, the multivariate analysis highlighted that the mothers gave first birth at the age of 20 years and above (AOR = 0.55, 95% CI: 0.35–0.88) in wave 3, having living children in wave 4, had male newborns (AOR = 1.28, 95% CI: 1.09–1.49) in wave 4 with large size (AOR = 0.59, 95% CI: 0.38–0.91) in wave 3 had more probability to avail newborn PNC services. Findings showed that antenatal attendance with at least 4 visits or more had a strong association with newborn PNC utilization (AOR = 1.73, 95% CI: 1.09–2.74; AOR = 1,19, 95% CI: 1.09–1.44) in waves 2 and 4 respectively.
With reference to community-level characteristics, results showed that women from Sindh province across all three waves of PDHS (AOR 4.81, 95% CI: 1.47–15.70; AOR 5.28, 95% CI: 1.61–17.29; AOR 3.61, 95% CI: 1.53–8.51), while Punjab in last two waves, i.e. wave 3 and 4 (AOR = 4.28, 95% CI: 1.33–13.77) (AOR = 2.30, 95% CI: 1.09–5.35) had higher newborn PNC utilization. Further, those mothers, who had exposure to mass media (AOR = 1.29, 95% CI: 1.05–1.59) in wave 4 and had no perceived difficulty in accessing distant healthcare facilities (AOR = 1.29, 95% CI: 1.01–1.66) in wave 3 are more likely to avail newborn PNC utilization.
Lastly, multivariate analysis with institutional level characteristics informed that newborn PNC utilization had a strong association with mode of delivery (AOR = 2.55, 95% CI: 1.71–3.81; AOR = 2.23, 95% CI:1.83–2.72) in waves 3 and 4, skilled birth assistance (AOR = 1.76, 95% CI: 1.09–3.32; AOR = 2.39, 95% CI: 1.39–4.09) in wave 2 and 3, and place of delivery (AOR = 0.27, 95% CI: 0.18–0.40) in wave 4 of PDHS.
Discussion
The topic of PNC utilization is of great significance, as it provides a window of opportunity to avert maternal and newborn mortality. The present study is aimed to analyze the trend of multi-level determinants i.e. individual (socio-demographic and obstetric), community, and institutional level determinants, influencing the maternal and newborn PNC utilization among women of reproductive age 15–49 years in Pakistan across the last three waves of PDHS, from 2006 to 2018. This research is an attempt to bridge the gap in existing literature, documenting the maternal and newborn PNC utilization with three hierarchal level determinants at individual, community, and institutional levels to highlight the maternal and newborn health issues in Pakistan.
The research revealed an upward trend in maternal PNC utilization, with an increase from 43.5 to 63.6% from 2006 to 2018 in Pakistan, which highlights the continued efforts of the government at large and the contribution of community-level healthcare providers in particular. Contrary, a dip was observed in newborn PNC utilization in the country, with an upsurge from 20.6 to 50.5% from 2006 to 2013, nonetheless 30.7% in 2018. The decrease in newborn PNC utilization is alarming, that may be attributed to various geographical and health inequalities [42]. Also, it highlights that newborn PNC is the least consulted area due to a lack of awareness amongst mothers [43], and requires immediate attention.
Findings informed that maternal and newborn PNC utilization had a strong association with individual-level socio-demographic characteristics. Particularly, it was found higher amongst older age women, who completed at least basic years of schooling, were employed in various occupations, and had decision-making and emotional autonomy in varied waves of PDHS. These findings related to women’s age, education, and occupation are consistent with the studies conducted in Malawi [44], Nigeria [45], Bangladesh [46, 47], and India [48]. Moreover, the women who had women’s decision-making and emotional autonomy were more likely to utilize PNC services, which also corresponds to the preceding research [44, 49, 50]. A variation between maternal and newborn PNC utilization with some key socio-demographic characteristics was also seen, where the availability of own vehicle for transportation, household wealth quintile, and spouse occupation had a statistically significant relationship with maternal PNC utilization, nonetheless insignificant relationship with newborn PNC utilization. These results are somehow similar to studies carried out in Gondar (Ethiopia), Swaziland (North Africa), and Nepal [50,51,52]. Arguably, women with improved education, economic status, and empowerment are more capable to seek and afford healthcare services, in contrast to others [53].
A strong association between PNC utilization and women’s obstetric characteristics was observed, particularly with women’s age at first birth, parity, the number of living children, antenatal attendance with at least 4 visits, and sex and size of the newborn. These results are similar to previous studies [54,55,56], where women who gave birth at age of 25–34 years, had a smaller number of children, with at least 4 antenatal visits, and had male newborns were more likely to avail PNC utilization for themselves and their newborns [57].
Upon analyzing the relationship between newborn PNC utilization and community-level characteristics, the study showed that women living in various regions/provinces of Pakistan (e.g., Sindh & Punjab), who had no perceived difficulty in accessing healthcare facilities to seek medical care were more likely to avail both maternal and newborn PNC utilization. Further, a strong association between exposure to mass media and newborn PNC utilization was also observed, highlighting the significant role of mass media in raising awareness. These findings are also comparable to the previous research, informing that mothers belonged to the developed areas, and had access to mass media as well as health facilities are more advantageous to avail PNC services [58,59,60].
Regarding institutional level determinants, the study revealed that mode of delivery, skilled birth assistance, and place of delivery in some waves showed a statistically significant relationship with maternal and newborn PNC utilization. These findings informed that births assisted by skilled birth attendants, preferably caesarean section and at health facilities are more likely to receive PNC services. These results are similar to the previous studies [61,62,63,64,65,66,67] and also highlight that skilled personnel educate and encourage mothers regarding the significance of PNC. Nonetheless, it is pertinent to mention that PDHS does not collect data on the types of services received during PNC, therefore additional research would be required in this area to develop a more thorough understanding.
Policy implications
This research suggests multiple policy implications to improve the maternal and newborn PNC utilization in Pakistan. Considering the significance of PNC, this research contributes to expand the policies, particularly ensuring PNC as a critical component of continuum of care, denoting it as a ‘fourth trimester’, instead of a single encounter. This fourth trimester must be indispensable to deliver quality services and support according to the women’ needs, including pre-emptive guidance during pregnancy and development of a postpartum care plan, implementation of comprehensive postpartum visit schedule, and counseling women with pregnancies complicated by preterm birth, gestational diabetes, or hypertensive disorders to control future pregnancies. The results may be helpful for policymakers to include specific implementation strategies directly related to the maternal and newborn survival with defined timelines and releases of appropriate funding for enhancing community access to PNC services. This could be done through establishing and strengthening Emergency Obstetric and Newborn Care (EmONC) centers with equitable geographical distribution and referral support.
Another policy implication highlights to design clearly defined mechanisms and astringent monitoring and evaluation system to gauge effective implementation of strategies and achievement of outcome targets. This could be done through enhancing inter-sectoral collaboration with clearly identified roles and responsibilities of key stakeholders. This research also informs to improve access to health education for girls and women, increasing their social support, and promoting parenting responsibilities for maximizing the benefits of PNC utilization.
Conclusion
The research concluded that there is a difference in maternal and newborn PNC utilization in Pakistan, which is influenced by multiple individual (socio-demographic and obstetrics), community, and institutional level determinants. Overall, an upward trend in maternal PNC, nonetheless, a downward trend in newborn PNC utilization is evident from the analysis of the last three waves of PDHS from 2006 to 2018, which requires immediate attention. There is a need to promote the benefits of PNC for early diagnosis of postpartum complications, and for saving mothers’ and newborns’ lives.
The research recommends a national-level mass media campaign for health promotion and awareness-raising, preferably in regional languages, and focusing on PNC’s importance, as part of a continuum of care during pregnancy. An active engagement of social media channels can be more beneficial in the present scenario to reach a maximum audience for health promotion. This research also advocates strategizing effective public health interventions to enhance women’s access to healthcare facilities and skilled healthcare providers for childbirth and related PNC services. More specifically, the role of healthcare providers is of utmost importance in health education and counseling for PNC services. Emphasis should be given to educationally and economically marginalized mothers, particularly, those living in remote communities, where PNC utilization is comparatively low.
Data availability
The present study used raw data of four waves from PDHS. The DHS Program is authorized to distribute free-of-cost and unrestricted survey data files for academic research with registration only. This dataset is available on the DHS website and may be accessed on the following link https://dhsprogram.com/data/available-datasets.cfm by registering as a DHS user. DHS holds country-specific datasets and is widely used for secondary data analysis across the globe.
Abbreviations
- AOR:
-
Adjusted odds ratio
- CI:
-
Confidence interval
- LHW:
-
Lady Health Worker
- MMR:
-
Maternal Mortality Ratio
- MWRA:
-
Married women of reproductive age
- NIPS:
-
National Institute of Population Studies
- OR:
-
Odds ratio
- PDHS:
-
Pakistan Demographic and Health Survey
- PNC:
-
Postnatal care
- SBA:
-
Skilled Birth Attendant
- SDG:
-
Sustainable Development Goals
- SPSS:
-
Statistical Package for Social Sciences
- UN:
-
United Nations
- VID:
-
Variance inflation factor
References
World Health Organization. Maternal mortality. 2019. https://www.who.int/news-room/fact-sheets/detail/maternal-mortality. Accessed 20 August 2022.
World Health Organization. Newborns: improving survival and well-being. 2020. https://www.who.int/news-room/fact-sheets/detail/newborns-reducing-mortality. Accessed 20 August 2022.
UNICEF. Child survival and the SDGs. 2021. https://data.unicef.org/topic/child-survival/child-survival-sdgs/. Accessed 20 August 2022.
National Institute of Population Studies (NIPS) [Pakistan] and ICF. Pakistan maternal mortality Survey 2019: Key Indicators Report. Islamabad, Pakistan, and Rockville. Maryland, USA: NIPS and ICF; 2020.
Hafeez A, Zaka N, Ahmad I, Shahzad K, Improving, Maternal. Newborn and Child Health Outcomes in a Decade, Pakistan Report 2020. 2021. https://www.countdown2030.org/wp-content/uploads/2021/02/Pakistan-CD-report-2020.pdf. Accessed 20 August 2022.
Naseem S, Khattak UK, Ghazanfar H, Irfan A. Maternal health status in terms of utilisation of antenatal, natal and postnatal services in a Peri urban setting of Islamabad: a community based survey. J Pak Med Assoc. 2017;67(8):1186–91.
Titaley CR, Dibley MJ, Roberts CL. Factors associated with non-utilisation of postnatal care services in Indonesia. J Epidemiol Community Health. 2009;63(10):827–31.
Syed U, Asiruddin S, Helal MS, Mannan II, Murray J. Immediate and early postnatal care for mothers and newborns in rural Bangladesh. J Health Popul Nutr. 2006;24(4):508.
Gogia S, Sachdev HS. Home visits by community health workers to prevent neonatal deaths in developing countries: a systematic review. Bull World Health Organ. 2010;88:658–66.
Kirkwood BR, Manu A, ten Asbroek AH, Soremekun S, Weobong B, Gyan T, et al. Effect of the Newhints home-visits intervention on neonatal mortality rate and care practices in Ghana: a cluster randomised controlled trial. Lancet. 2013;381(9884):2184–92.
Alemayeh H, Assefa H, Adama Y. Prevalence and factors associated with post natal care utilization in Abi-Adi Town, Tigray, Ethiopia: a cross sectional study. IJPBSF Int J Pharm Biol Sci Fundamentals. 2014;8(1):23–35.
Wang W, Hong R. The continuum of care for maternal and newborn health in Cambodia: where are the gaps and why? A population-based study. Lancet. 2013;381:145.
World Health Organization. Technical Consultation on Postpartum and postnatal care: Department of making pregnancy safer. Geneva: World Health Organization; 2008.
CSA-Ethiopia. International: Ethiopia Demographic and Health Survey 2011. Maryland, USA.: Central Statistical Agency of Ethiopia and ICF International Addis Ababa, Ethiopia and Calverton; 2012.
Wudineh KG, Nigusie AA, Gesese SS, Tesu AA, Beyene FY. Postnatal care service utilization and associated factors among women who gave birth in Debretabour town, North West Ethiopia: a community-based cross-sectional study. BMC Pregnancy Childbirth. 2018;18:508.
Singh K, Brodish P, Haney E. Postnatal care by provider type and neonatal death in sub-saharan Africa: a multilevel analysis. BMC Public Health. 2014;14:941.
Lawn JE, Mwansa-Kambafwile J, Horta BL, Barros FC, Cousens S. ‘Kangaroo mother care’ to prevent neonatal deaths due to preterm birth complications. Int J Epidemiol. 2010;39(Suppl1):i144–54.
Lawn J, Kerber K. Opportunities for Africa’s newborns: practical data, policy and programmatic support for newborn care in Africa. Cape Town: Partnership for Maternal, Newborn and Child Health; 2006.
World Health Organization. WHO recommendations on postnatal care of the mother and newborn. Geneva: World Health Organization; 2014.
National Institute of Population Studies, Pakistan. (2019). Pakistan Demographic and Health Survey 2017-18.
Adnan M, Mahmood H, Hassan M, Humayun A. Maternal health care expenditure among women in rural areas of Pakistan.Annals of King Edward Medical University2017;23(2).
Yunus A, Iqbal S, Munawar R, Zakar R, Mushtaq SK, Sadaf F, Usman A. Determinants of postnatal care services utilization in Pakistan-insights from Pakistan Demographic and Health Survey (PDHS) 2006-07. Middle-East J Sci Res. 2013;18(10):1440–7.
Pasha O, Saleem S, Ali S, Goudar SS, Garces A, Esamai F, Patel A, Chomba E, Althabe F, Moore JL, Harrison M, Berrueta MB, Hambidge K, Krebs NF, Hibberd PL, Carlo WA, Kodkany B, Derman RJ, Liechty EA, Koso-Thomas M, et al. Maternal and newborn outcomes in Pakistan compared to other low and middle income countries in the Global Network’s maternal Newborn Health Registry: an active, community-based, pregnancy surveillance mechanism. Reproductive Health. 2015;12(Suppl 2):15.
Iqbal S, Maqsood S, Zakar R, Zakar MZ, Fischer F. Continuum of care in maternal, newborn and child health in Pakistan: analysis of trends and determinants from 2006 to 2012. BMC Health Serv Res. 2017;17:189.
Mcnojia SZ, Saleem S, Feroz A, Khan KS, Naqvi F, Tikmani SS, McClure EM, Siddiqi S, Goldenberg RL. Exploring women and traditional birth attendants’ perceptions and experiences of stillbirths in district Thatta, Sindh, Pakistan: a qualitative study. Reproductive Health. 2020;17(1):3.
Huda TM, Chowdhury M, El Arifeen S, Dibley MJ. Individual and community level factors associated with health facility delivery: a cross sectional multilevel analysis in Bangladesh. PLoS ONE. 2019;14(2):e0211113.
Adedokun ST, Adekanmbi VT, Uthman OA, Lilford RJ. Contextual factors associated with health care service utilization for children with acute childhood illnesses in Nigeria. PLoS ONE. 2017;12(3):e0173578.
Mezmur M, Navaneetham K, Letamo G, Bariagaber H. Individual, household and contextual factors associated with skilled delivery care in Ethiopia: evidence from ethiopian demographic and health surveys. PLoS ONE. 2017;12(9):e0184688.
Teshale AB, Tesema GA, Yeshaw Y, Tesema AK, Alem AZ, Liyew AM. Individual and community level factors associated with delayed first postnatal care attendance among reproductive age group women in Ethiopia. BMC Pregnancy Childbirth. 2021;21:22.
Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995;36(1):1–10.
Andersen RM, Rice TH, Kominski GF. Changing the US health care system: key issues in health services policy and management. John Wiley & Sons; 2011.
Andersen R, Newman JF. Societal and individual determinants of medical care utilization in the United States. Milbank Meml Fund Q Health Soc. 1973;51(1):95–124.
Andersen R. A behavioral model of families’ use of health services. A behavioral model of families’ use of health services. Chicago: Center for Health Administration Studies; 1968.
Andersen RM. National health surveys and the behavioral model of health services use. Med Care. 2008;46(7):647–53.
National Institute of Population Studies (NIPS). Pakistan Demographic and Health Survey (PDHS) 2006–07. Maryland: Macro International Inc.; 2007.
National Institute of Population Studies (NIPS). Pakistan Demographic and Health Survey (PDHS) 2012–13. Maryland: Macro International Inc.; 2013.
National Institute of Population Studies (NIPS). Pakistan Demographic and Health Survey (PDHS) 2017–18. Maryland: Macro International Inc.; 2018.
National Institute of Population Studies (NIPS). Pakistan Demographic and Health Survey (PDHS) 1990–91. Maryland: Macro International Inc.; 1991.
Antai D. Controlling behavior, power relations within intimate relationships and intimate partner physical and sexual violence against women in Nigeria. BMC Public Health. 2011;11:511.
Iqbal S, Maqsood S, Zafar A, Zakar R, Zakar MZ, Fischer F. Determinants of overall knowledge of and attitudes towards HIV/AIDS transmission among ever-married women in Pakistan: evidence from the Demographic and Health Survey 2012–13. BMC Public Health. 2019;19:793.
Hair JF Jr, Anderson RE, Tatham RL, Black WC. Multivariate Data Analysis. New York: Macmillan; 1995.
Saira A, Wilson LA, Ezeh KO, Lim D, Osuagwu UL, Agho KE. Factors associated with non-utilization of postnatal care among newborns in the first 2 days after birth in Pakistan: a nationwide cross-sectional study. Global Health Action. 2021;14(1):1973714.
Sultana N, Shaikh BT. Low utilization of postnatal care: searching the window of opportunity to save mothers and newborns lives in Islamabad capital territory, Pakistan. BMC Res Notes. 2015;8:645.
Sagawa J, Kabagenyi A, Turyasingura G, Mwale SE. Determinants of postnatal care service utilization among mothers of Mangochi district, Malawi: a community-based cross-sectional study. BMC Pregnancy Childbirth. 2021;21:591.
Babalola S, Fatusi A. Determinants of use of maternal health services in Nigeria-looking beyond individual and household factors. BMC Pregnancy Childbirth. 2009;9:43.
Aziz S, Basit A, Sultana S, Homer CS, Vogel JP. Inequalities in women’s utilization of postnatal care services in Bangladesh from 2004 to 2017. Sci Rep. 2022;12(1):2747.
Mosiur Rahman M, Haque SE, Sarwar Zahan M. Factors affecting the utilisation of postpartum care among young mothers in Bangladesh. Health Soc Care Commun. 2011;19(2):138–47.
Singh R, Neogi SB, Hazra A, Irani L, Ruducha J, Ahmad D, et al. Utilization of maternal health services and its determinants: a cross-sectional study among women in rural Uttar Pradesh, India. J Health Popul Nutr. 2019;38(1):13.
Phiri PWC, Rattanapan C, Mongkolchati A. Determinants of postnatal service utilisation among mothers in rural settings of Malawi. Health Soc Care Commun. 2015;23(5):493–501.
Khanal V, Adhikari M, Karkee R, Gavidia T. Factors associated with the utilisation of postnatal care services among the mothers of Nepal: analysis of Nepal Demographic and Health Survey 2011. BMC Women’s Health. 2014;14:19.
Worku AG, Yalew AW, Afework MF. Factors affecting the utilization of skilled maternal care in Northwest Ethiopia: a multilevel analysis. BMC Int Health Hum Rights. 2013;13:20.
Tsawe M, Moto A, Netshivhera T, Ralesego L, Nyathi C, Susuman AS. Factors influencing the use of maternal healthcare services and childhood immunization in Swaziland. Int J Equity Health. 2015;14:32.
Tiruneh FN, Chuang KY, Chuang YC. Women’s autonomy and maternal healthcare service utilization in Ethiopia. BMC Health Serv Res. 2017;17:718.
Chungu C, Makasa M, Chola M, Jacobs CN. Place of delivery associated with postnatal care utilization among childbearing women in Zambia. Front Public Health. 2018;6:94.
Teklehaymanot A, Niguse D, Tesfay A. Early postnatal care service utilization and associated factors among mothers who gave birth in the last 12 months in Aseko district, Arsi zone, south East Ethiopia in 2016. J Women’s Heal Care 2017;6.
Izudi J, Akwang GD, Amongin D. Early postnatal care use by postpartum mothers in Mundri East County, South Sudan. BMC Health Serv Res. 2017;17:442.
Islam MA, Barna SD. Concise title: maternal health service utilization. Clin Epidemiol Global Health. 2020;8(4):1236–41.
Bwalya BB, Mulenga MC, Mulenga JN. Factors associated with postnatal care for newborns in Zambia: analysis of the 2013-14 Zambia Demographic and Health Survey. BMC Pregnancy Childbirth. 2017;17:418.
Singh A, Yadav A, Singh A. Utilization of postnatal care for newborns and its association with neonatal mortality in India: an analytical appraisal. BMC Pregnancy Childbirth. 2012;12:33.
Mumtaz Z, Salway S, Shanner L, Zaman S, Laing L. Addressing disparities in maternal health care in Pakistan: gender, class and exclusion. BMC Pregnancy Childbirth. 2012;12:80.
Ahinkorah BO, Seidu AA, Budu E, Armah-Ansah EK, Agbaglo E, Adu C, et al. Factors Associated with utilization of postnatal care services in Mali, West Africa. Int J Translational Med Res Public Health. 2021;5(1):23–32.
Gabrysch S, Campbell OM. Still too far to walk: literature review of the determinants of delivery service use. BMC Pregnancy Childbirth. 2009;9:34.
Say L, Raine R. A systematic review of inequalities in the use of maternal health care in developing countries: examining the scale of the problem and the importance of context. Bull World Health Organ. 2007;85:812–9.
Stephenson R, Matthews Z. Maternal health-care service use among rural-urban migrants in Mumbai, India. Asia-Pacific Popul J. 2004;19(1):39–60.
Rwabufigiri BN, Mukamurigo J, Thomson DR, Hedt-Gautier BL, Semasaka JPS. Factors associated with postnatal care utilisation in Rwanda: a secondary analysis of 2010 Demographic and Health Survey data. BMC Pregnancy Childbirth. 2016;16:122.
Kebede SA, Weldesenbet AB, Tusa BS. Determinants of Postnatal Care and Timing of the First Postnatal Care for Newborns in Ethiopia: Further Analysis of 2019 Ethiopian Demographic and Health Survey. 2021
Neupane S, Doku D. Utilization of postnatal care among nepalese women. Matern Child Health J. 2013;17(10):1922–30.
Acknowledgements
Not applicable.
Funding
This research received no supporting funds from any funding agency in the public, commercial, or not-for-profit sector.
Author information
Authors and Affiliations
Contributions
SI and RZ conceptualized the study. SI led the analysis, interpretation of the study findings, and manuscript writing. SM, RZ and FF contributed to data analysis and revised the manuscript critically for important intellectual content. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
No ethical approval was needed for this study, because it is based on secondary data taken from four waves of PDHS. For primary data collection, ethical approvals were obtained: The ICF Institutional Review Board (132989.<0.010.PK.DHS.01) and the National Bioethics Committee of Pakistan (4–87/NBC-285/17/1438) reviewed and approved PDHS 2017-18. The Institutional Review Board of ICF Macro reviewed and approved the MEASURE Demographic and Health Surveys Project Phase III. The PDHS 2012-13 is categorized under that approval (31406.0<0.012.12). The Institutional Review Board of Macro International, Inc. reviewed and approved the MEASURE Demographic and Health Surveys Project Phase II. The PDHS 2006-07 is categorized under that approval. The Institutional Review Board of Macro International, Inc. reviewed and approved the MEASURE Demographic and Health Surveys + Project, which includes the PDHS 1990-9. Written informed consent was obtained from participants or from legally authorized representatives in case of minors.
The DHS Program maintains ethical standards and ethical reviews to protect the privacy of respondents and household members for all DHS. Furthermore, all questionnaires and procedures for DHS were reviewed and approved by ICF Institutional Review Board (IRB) to comply with the U.S. Department of Health and Human Services regulations for the protection of human subjects (45 CFR 46), as well as by country-specific IRB to ensure compliance of the survey with local laws and norms. You may kindly refer to the following link: https://dhsprogram.com/Methodology/Protecting-the-Privacy-of-DHS-Survey-Respondents.cfm.
All procedures were taken in respect of the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare no conflict of interest. RZ and FF serve on the Editorial Board of BMC Public Health as Associate Editors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Iqbal, S., Maqsood, S., Zakar, R. et al. Trend analysis of multi-level determinants of maternal and newborn postnatal care utilization in Pakistan from 2006 to 2018: Evidence from Pakistan Demographic and Health Surveys. BMC Public Health 23, 642 (2023). https://doi.org/10.1186/s12889-023-15286-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-023-15286-7