Abstract
Background
Accelerating declines in tuberculosis (TB) incidence is paramount for achieving global goals set for 2030 by the Sustainable Development Goals and the End TB Strategy. The aim of this study was to identify key country-level social determinants of national TB incidence trends.
Methods
This longitudinal ecological study used country-level data extracted from online databases from the period 2005–2015. We used multivariable Poisson regression models allowing for distinct within- and between-country effects to estimate associations between national TB incidence rates and 13 social determinants of health. The analysis was stratified by country income status.
Results
The study sample included 48 low- and lower-middle-income countries (LLMICs) and 68 high- and upper-middle income countries (HUMICs), with a total of 528 and 748 observations between 2005–2015, respectively. National TB incidence rates declined in 108/116 countries between 2005–2015, with an average drop of 12.95% in LLMICs and 14.09% in HUMICs. Between LLMICs, higher Human Development Index (HDI), social protection spending, TB case detection, and TB treatment success were associated with lower TB incidence. Higher prevalence of HIV/AIDS was associated with higher TB incidence. Within LLMICs, increases in HDI over time were associated with lower TB incidence rates. Between HUMICs, higher HDI, health spending, and diabetes prevalence were associated with lower TB incidence, whereas higher prevalence of HIV/AIDS and alcohol-use were associated with higher TB incidence. Within HUMICs, increases in HIV/AIDS and diabetes prevalence over time were associated with higher TB incidence.
Conclusions
In LLMICs, TB incidence rates remain highest in countries with low human development, social protection spending and TB programme performance, and high rates of HIV/AIDS. Strengthening human development is likely to accelerate declines in TB incidence. In HUMICs, TB incidence rates remain highest in countries with low human development, health spending and diabetes prevalence, and high rates of HIV/AIDS and alcohol use. Here, slowing rising rates of HIV/AIDS and diabetes is likely to accelerate declines in TB incidence.
Similar content being viewed by others
Background
Tuberculosis (TB) remains the world’s biggest infectious killer, claiming an estimated 1.6 million global deaths in 2021 [1]. The World Health Organization’s (WHO) End TB Strategy aims to achieve an 80% drop in new cases of TB and 90% reduction in TB mortality by 2030 [2]. However, progress remains well short of what is necessary to achieve these goals [1, 2]. Global estimates updated to reflect disruptions to essential TB services during COVID-19 estimate that TB incidence increased by 3.6% for the first time in decades between 2020 and 2021 [1].
Action on poverty and associated risk factors is expected to play an important role in accelerating the decline in TB incidence and has been integrated as a central paradigm of the End TB Strategy [2, 3]. TB disease disproportionately affects poor and marginalised populations [4] and is strongly associated with living or working in an environment with high TB prevalence [5, 6], overcrowding [7], poor ventilation [7], malnutrition [8] and health conditions that impair host immune defence [4, 9].
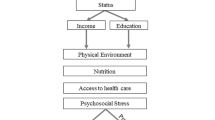
The economic and social conditions that influence TB risk are collectively known as the social determinants of health. Based on the WHO’s Commission on Social Determinants of Health (CSDH), social determinants of health can be divided into structural and intermediary determinants [10]. Factors at the structural level make-up the socioeconomic and political context as well as the individual socioeconomic position that determine people’s exposure to intermediary determinants [10]. Factors at the intermediary level include material circumstances, behaviours, biological, and psychosocial factors that have a direct impact on health outcomes, such as exposure to indoor air pollution [10]. The CSDH conceptual framework is helpful for understanding how TB occurrence may be determined by social determinants of health at the structural and intermediary levels of influence (Fig. 1).
CSDH conceptual framework for action on the social determinants of health [10]
Although improved diagnosis and treatment through national TB programmes has been linked to lower TB mortality, their impact on TB incidence remain unclear [3, 11, 12]. Growing evidence supports the need for primary disease prevention to achieve definitive reductions in TB incidence and mortality by 2035 [13,14,15,16]. In an early study in 2009, Dye et al. identified the national Human Development Index (HDI), under-five mortality rate (U5M), and access to improved sanitation services as dominant predictors of global TB incidence trends between 1997 and 2006 [17]. Since then, several studies have investigated the potential of anti-poverty strategies to accelerate progress on ending TB [18, 19]. Results consistently point to the large impact that such measures could have for TB control.
Observed changes in TB associated health risks since 2006 such as diabetes prevalence [20, 21] and undernourishment [21, 22] highlight the need for an updated analysis of the key determinants of global TB incidence trends. Extending Dye et al.’s study to consider the full period of the millennium development goals (MDGs), we aimed to investigate which social determinants of health may hold promise for accelerating declines in TB incidence. The aim of the study was to identify key social determinants of health that influenced global TB incidence trends 2005–2015. Our objectives were to 1) describe trends in TB incidence between 2005 and 2015, 2) evaluate between countries how social determinants of health are associated with TB incidence rates, and 3) evaluate within countries how trends in social determinants of health are associated with declines in TB incidence rates. Because trends in TB incidence rates differ significantly across country-income groups, we stratified our analysis into high- and upper-middle income countries (HUMICs), and low- and lower-middle income countries (LLMICs).
Methods
Study design and data
The study used an ecological, longitudinal design to evaluate associations between national TB incidence rates and 13 selected indicators of social determinants of health. The study period corresponded to the 11-year MDG era, 2005–2015. Data on national TB incidence rates and social determinants of health for these years were downloaded from public online data repositories in 2020. The study was reported according to STROBE reporting guidelines A.1 [23].
Study sample
The study sample was countries with available TB incidence data in the first year of the MDG period, 2005. Countries with an annualized change in TB incidence rate greater than three standard deviations of the mean were considered outliers with unusual conditions and excluded (N = 1, Ethiopia) [24]. We hypothesised that different public health priorities, healthcare systems, and socioeconomic contexts could mean that the social determinants of TB incidence rates would differ by country income status. We originally grouped countries into two categories, high-income countries versus low- and middle-income countries, using World Bank income classifications from 2005 [25]. However, during the peer-review process we observed that there was a risk of modelling error from too few observations in the high-income country group. Further analysis in Additional file 1: Appendix A.2 showed that average TB incidence rates for 2005 in upper-middle income countries (70.94 per 100,000) were more similar to high-income countries (9.37 per 100,000) than lower-middle income countries (217.35 per 100,000). Grouping upper-middle income countries with high-income countries also resulted in a more equal split in observations, which fulfilled the rule of thumb of at least 10 observations per variable included in our final regression models for both groups. Therefore, our final analysis was grouped into two categories, high-income countries with upper-middle income countries, and low-income countries with lower-middle income countries. Lists of included and excluded countries are provided in the Additional file 1: Appendix A.3 and A.4.
Study variables
The study outcome was age- and sex-standardized national TB incidence. Seventeen indicators of social determinants of TB incidence rate were identified and considered for inclusion in the study based on the CSDH framework and their availability in five public online data repositories: The World Bank Database, the Global Burden of Disease (GDB) Study, the Human Development Report (HDR), the International Labour Organization database (ILO), and the WHO TB database. All seventeen indicators were continuous variables. Two indicators were considered proxies of TB programme performance and quality (TB case detection rate, TB treatment success rate). We expected a certain degree of collinearity between indicators of socioeconomic development and assessed intercorrelations between indicators of social determinants of health using Pearson correlation. We found HDI, U5M, access to hygiene, access to drinking water, and access to clean cooking technologies to be highly correlated at ρ > 0.8 (Additional file 1: Appendix A.4, A.5) [26]. Among these indicators, HDI was selected as the most comprehensive measure tracking human development. This meant that 13/17 of the original indicators were included in the analysis. We provide a description of each variable considered for inclusion in Table 1, and fuller description of those included in the study in Additional file 1: Appendix A.6.
Missing data
We used linear interpolation and extrapolation to substitute missing observations between 2005–2015. Observed data from 2016 or 2017 was used to interpolate missing observations in 2015. Data on public social protection expenditure for Nicaragua and Sierra Leone could not be extrapolated since the observed values in 2005 and 2015 were identical. Overall characteristics of interpolated and non-interpolated data are provided in the Additional file 1: Appendix A.7.
Data analysis
First, we summarised trends in TB incidence rates as the absolute and percentage change between 2005–2015 using mean and standard deviation (SD). We also described average values of our 13 indicators of social determinants of health in 2005, 2015, and between 2005–2015 using mean and SD. For pooled observations between 2005–2015 we also reported between- and within-country components of the overall SD. Student’s t-test was performed to assess differences in the mean values of social determinants of health between our two categories of country based on World Bank country-income classifications.
Second, we evaluated associations between TB incidence rates and our 13 social determinants of health using univariable and multivariable random effects within-between Poisson regression models. The within-between modelling approach provided the ability to distinguish differing relationships between TB incidence and social determinants based on within- and between-country variation over time [27]. We provide an example interpretation of these two types of variation using HDI. Hypothesizing that this social determinant of health would be associated with lower TB incidence rates, between-country analysis would test whether countries with higher values of HDI have lower national TB incidence rates; whereas within-country analysis would test whether within the same country, years with higher than average HDI have lower TB incidence rates. The significance level was set to 5% and results were reported as incidence rate ratio (IRR). Analyses were carried out in Stata 15.1. The analysis code and data are available online (https://osf.io/x6uag/).
Sensitivity analysis
In a sensitivity analysis, we evaluated multivariable associations between TB incidence rates and more distal indicators of social determinants of health, which included HDI, public social protection spending, current health expenditure, and labour force participation rates. This was to rule out possible attenuation of associations between more distal social determinants of health and TB incidence by intermediary social determinants of health lying on the causal pathway.
Results
Study sample
Of 195 countries with TB incidence rate data in the GBD study, incomplete data in 2005 excluded 53 HUMICs and 24 LLMICs. Ethiopia was excluded due to outlying annualized change in TB incidence rate (Fig. 2). Among the 116 included countries, 48 (41%) were LLMICs and 68 (59%) were HUMICs. The final sample included 24 of the 30 countries defined by the WHO as having a high TB burden and represents 68% of all estimated incident TB cases worldwide [1].
Summary of trends in TB incidence rates between 2005–2015
Across all countries, the mean TB incidence rate in 2005 was 134.77 per 100,000 population (SD:155.44, IQR:220.65). In LLMICs, the mean TB incidence rate in 2005 was 249.57 per 100,000 population (SD:144.74, IQR:165.61), and in HUMICs it was 53.74 per 100,000 population (SD:103.28, IQR:40.51). Overall, TB incidence rates between 2005–2015 declined in 108 of the 116 included countries (93%). Among the eight countries where TB incidence rates increased between 2005–2015, two were LLMICs and six were HUMICs. In LLMICs, the mean change in TB incidence rate between 2005–2015 was -29.48 per 100,000 (SD:25.44, IQR:29.53), and in HUMICs, it was -9.00 per 100,000 population (SD:15.70, IQR:6.70). In LMICs, this corresponded to a mean percentage decline in TB incidence of 13.60%, and in HUMICs, a decline of 20.95%. Descriptive statistics for our 13 social determinants of health in 2005, 2015, and between 2005–2015 are summarized in Table 2. Results of univariable regression analysis are presented in Table 3.
Multivariable analysis
Results of multivariable within-between regression are presented in Table 3.
Within-country
Within LLMICs, increases in HDI over time were associated with lower TB incidence rates. Within HUMICs, increases in the prevalence of diabetes over time were associated with higher TB incidence rates.
Between-country
Between LLMICs, higher HDI, public social protection spending, TB case detection rates, and TB treatment success rates were associated with lower TB incidence rates, while higher prevalence of HIV/AIDS was associated with higher TB incidence rates. Between HUMICs, higher HDI, health expenditure spending, and prevalence of diabetes were associated with lower TB incidence rates, while higher prevalence of HIV/AIDS and alcohol use disorder were associated with higher TB incidence rates.
Sensitivity analysis
We found that results were largely the same as in the main analysis when only including more distal social determinants of health in our multivariable regression. The only significant difference was that within LLMICs, there was no evidence that social protection spending was associated with lower TB incidence rates (Additional file 1: Appendix A.10).
Discussion
National TB incidence rates decreased in most countries between 2005–2015, declining by a greater proportion in HUMICs compared to LLMICs. Increases observed in HUMICs may have been driven by an increase in prevalence of HIV/AIDS and/or diabetes, whereas increases in LLMICs may have been associated with a slower growth of HDI. In LLMICs, comparing between countries, we find that human development, higher spending on social protection, lower prevalence of HIV/AIDS, and better TB programme performance are significant predictors of lower TB incidence rates. Comparing within-LLMICs, we find a strong link between increases in human development over time and lower TB incidence rates. The pattern appears to be slightly different in HUMICs. Here, comparing between countries, higher human development and spending on healthcare, rather than social protection as in LLMICs, are key predictors of lower TB incidence rates. Our analysis also points to a greater influence of the TB associated comorbidities and health risk behaviours HIV/AIDS, tobacco smoking, and diabetes between-HUMICs relative to between-LLMICs. In addition to lower prevalence of HIV/AIDS, lower prevalence of alcohol use disorder and higher prevalence of diabetes are also significant predictors of lower TB incidence rates. Comparing within-HUMICs, we find a strong link between increases in HIV/AIDS and diabetes prevalence over time and higher TB incidence rates.
To our knowledge, this study provides the most comprehensive insight into the drivers of TB incidence trends at a global level since Dye et al.’s original study in 2009 [17]. More sophisticated statistical methods provide further nuance to our understanding of the drivers of TB incidence and enable us to draw more confident conclusions. The use of a random effects within-between statistical model allows us to evaluate both how variation in determinants between-countries and within-countries over time predicts lower national TB incidence rates.
In relation to existing literature, our findings match evidence that TB disproportionately affects the poorest countries and households, and that human development is a key driver of lower TB incidence [17, 19, 28, 29]. Our findings between-LLMICs are also in line with previous evidence that receipt of social protection, including cash transfers, reduces individuals risk of TB infection and increases their probability of TB treatment success [10, 18, 30]. Evidence that between-HUMICs, health spending is a strong determinant of TB incidence also matches previous evidence [17, 18]. The significance of social protection spending in LLMICs, versus the significance of health spending in HUMICs might indicate a transition in the significance of these determinants as countries develop [31, 32]. However, this would require further research, as distinct from our study, previous evidence supports a positive effect of social protection spending on lower TB incidence rates across Europe [33]. Our findings also add to a large body of literature on the link between both HIV/AIDS and alcohol use and TB incidence [34, 35].
Our contrasting findings for the influence of diabetes prevalence on TB incidence when we compare within- and between-HUMICs, are also consistent with a previous analysis which found that in the same year, diabetes prevalence and TB incidence were inversely related; but that over time, TB incidence was more likely to increase in countries where diabetes prevalence increased [36]. Diabetes is more common in richer countries that have better developed health systems and lower levels of disease risk factors that are positively associated with TB incidence, such as environmental pollutants [37]. Our findings that as the prevalence of diabetes increases declines in TB incidence slow could be explained by diabetes and TB interacting biologically [38], and/or countries national control of TB incidence being temporarily affected by an increasing need to simultaneously respond to growing numbers of diabetes patients. Diabetes management poses a significant financial burden to health systems and could affect funds available for other health priorities [39, 40]. The process of social development involves significant changes in demography, the distribution of risk factors, and organisation and quality of health services [41], and further analysis would be needed to unpack the precise mechanisms underlying the observed within-country association between diabetes prevalence and TB incidence.
For TB programme performance, we find that in LLMICs, between-countries, those with higher TB programme performance have lower TB incidence rates. However, similar to Dye et al., we still find no evidence in either LLMICs or HUMICs that increases in TB control performance over time are associated with lower TB incidence [17]. Further research is needed to understand how investments in this area can lead to much needed impacts on TB transmission [17].
This study had a number of strengths. Data were selected from the most comprehensive online sources and represent the best available data today. The use of within-between random effects specifications allowed us to evaluate both, more causally robust within-country relationships, and policy relevant between-country relationships. This methodological approach builds on Dye et al.’s evaluation of incidence trends as 10-year averages. The study also has limitations. First, like Dye et al. it relies on estimated values of TB incidence, TB treatment success, and TB case detection from national TB surveillance systems [17]. All associations were also investigated at the population level, and as such should not be interpreted as causal or as applying to the individual level [42]. Excluding countries with missing data at baseline affects the generalizability of our findings to these countries. Nevertheless, inclusion of 24/30 high TB burden countries gives confidence that our results are likely to apply in settings where action to reduce TB incidence is most needed [1]. The range of predictors in our model, also resulted in very small coefficients for some variables like prevalence of HIV/AIDS and made it difficult to compare effect sizes. Finally, we also had to exclude some predictors that could have provided further insight into preventing TB due to high levels of missing data including proportion of urban population living in slums, coverage of social protection and labour programmes, and total TB expenditure.
In the shadow of the global COVID-19 crisis which threatens to reverse decade long gains in development [43], intensified innovation and cost-saving solutions will be required to achieve End TB Strategy goals by 2030. Largely consistent with Dye et al.’s findings from 2009, this study provides updated evidence that indicators of human and social development may be stronger determinants of TB incidence decline than indicators of TB programme performance, especially in LLMICs [17]. Our study also reinforces the positive impact that actions to prevent rising rates of HIV/AIDS and diabetes could have on reducing TB incidence rates in HUMICs [2]. As promoted by the WHO, this could include intensified collaborative activities on diabetes and tuberculosis prevention, including integration of TB control strategies in broader health interventions that target non-communicable diseases [44]. Action on diabetes prevention in countries of lower socioeconomic status might become more urgent considering the projected increases in diabetes prevalence in low- and middle-income countries by 0.7–2.3% between 2019 and 2045, where most of the global TB burden is concentred today [21, 45, 46]. To maximise reductions in global TB incidence, investments should be targeted to countries in most need of support. Findings from our between-country analysis point to a number of indicators including low human development and social protection spending, high HIV prevalence and alcohol use, and poor TB programme performance that could be used to target strategic investments to reduce TB incidence globally [47].
In the future, research is needed to understand how national TB programmes can support the implementation of cost-effective approaches to improve human development in LLMICs, and prevent HIV/AIDS, and diabetes in HUMICs. It would be important for such efforts to consider the spill over effects of action on the social determinants of TB for other disease prevention programmes, especially those focused on HIV/AIDS and diabetes.
Conclusion
In LLMICs, TB incidence rates remain highest in countries with low human development, social protection spending, and TB programme performance, and high rates of HIV/AIDS. Strengthening human development is likely to accelerate declines in TB incidence. In HUMICs, TB incidence rates remain highest in countries with low human development, health spending, and diabetes prevalence, and high rates of HIV/AIDS and alcohol use. Here, slowing rising rates of HIV/AIDS and diabetes is likely to accelerate declines in TB incidence. Further research should focus on which investments are most likely to translate into change in these areas.
Availability of data and materials
The datasets generated and/or analysed during the current study are available in the Open Science Framework repository, https://osf.io/x6uag/
Abbreviations
- TB:
-
Tuberculosis
- WHO:
-
World Health Organization
- HIV:
-
Human Immunodeficiency Virus
- AIDS:
-
Acquired Immune Deficiency Syndrome
- HDI:
-
Human Development Index
- HUCI:
-
High- and upper-middle-income country
- LLMIC:
-
Low- and lower-middle-income country
- SDG:
-
Sustainable Development Goals
- CSDH:
-
Commission on Social Determinants of Health
- U5M:
-
Under-5 mortality
- MDG:
-
Millennium Development Goals
- GDB:
-
Global Burden of Disease Study
- HDR:
-
Human Development Report
- STROBE:
-
Strengthening the reporting of observational studies in epidemiology
- ILO:
-
International Labour Organization
- IRR:
-
Incidence rate ratio
- SD:
-
Standard deviation
- IQR:
-
Interquartile range
- CI:
-
Confidence interval
- ART:
-
Antiretroviral therapy
References
World Health Organization. Global Tuberculosis Report 2022 [Internet]. Geneva: World Health Organization, 20. Available from: https://apps.who.int/iris/rest/bitstreams/1474924/retrieve. Cited on 16.01.2023
World Health Organization. The End TB Strategy. Geneva: World Health Organization; 2018. Available from: https://www.who.int/tb/post2015_TBstrategy.pdf?ua=1. Cited on 08.12.2019.
Lönnroth K, Castro KG, Chakaya JM, et al. Tuberculosis control and elimination 2010–50: cure, care, and social development. Lancet. 2010;375:1814–29.
Lonnroth K, Jaramillo E, Williams BG, Dye C, Raviglione M. Drivers of tuberculosis epidemics: the role of risk factors and social determinants. Soc Sci Med. 2009;68(12):2240–6.
Bobrik A, Danishevski K, Eroshina K, McKee M. Prison health in Russia: the larger picture. J Public Health Policy. 2005;26(1):30–59.
Menzies D, Joshi R, Pai M. Risk of tuberculosis infection and disease associated with work in health care settings. Int J Tuberc Lung Dis. 2007;11(6):593–605.
Rieder HL. International Union against Tuberculosis and Lung Disease. Epidemiologic Basis of Tuberculosis Control. New Delhi: International Union against Tuberculosis and Lung Disease; 1999.
Lönnroth K, Williams BG, Cegielski P, Dye C. A consistent log-linear relationship between tuberculosis incidence and body mass index. Int J Epidemiol. 2010;39:149–55.
Lienhardt C. From exposure to disease: the role of environmental factors in susceptibility to and development of tuberculosis. Epidemiol Rev. 2001;23(2):288–301.
Solar O, Irwin A. A conceptual framework for action on the social determinants of health. Social Determinants of Health Discussion Paper 2. Geneva: The World Health Organization; 2001. Available from: https://www.who.int/sdhconference/resources/ConceptualframeworkforactiononSDH_eng.pdf. Cited on 21.02.2020.
Hargreaves JR, Boccia D, Evans CA, Adato M, Petticrew M, Porter JD. The social determinants of tuberculosis: from evidence to action. Am J Public Health. 2011;101(4):654–62.
Lonnroth K, Raviglione M. Global epidemiology of tuberculosis: prospects for control. Semin Respir Crit Care Med. 2008;29(5):481–91.
Dye C, Williams BG. Eliminating human tuberculosis in the twenty-first century. J R Soc Interface. 2008;5(23):653–62.
Dye C, Glaziou P, Floyd K, Raviglione M. Prospects for Tuberculosis Elimination. Annu Rev Public Health. 2013;34(1):271–86.
Houben RMGJ, Menzies NA, Sumner T, Huynh GH, Arinaminpathy N, Goldhaber-Fiebert JD, et al. Feasibility of achieving the 2025 WHO global tuberculosis targets in South Africa, China, and India: a combined analysis of 11 mathematical models. Lancet Glob Health. 2016;4(11):e806-15.
Vesga JF, Hallett TB, Reid MJA, Sachdeva KS, Rao R, Khaparde S, et al. Assessing tuberculosis control priorities in high-burden settings: a modelling approach. Lancet Glob Health. 2019;7(5):e585–95.
Dye C, Lonnroth K, Jaramillo E, Williams BG, Raviglione M. Trends in tuberculosis incidence and their determinants in 134 countries. Bull World Health Organ. 2009;87(9):683–91.
Siroka A, Ponce NA, Lonnroth K. Association between spending on social protection and tuberculosis burden: a global analysis. Lancet Infect Dis. 2016;16(4):473–9.
Carter DJ, Glaziou P, Lönnroth K, Siroka A, Floyd K, Weil D, et al. The impact of social protection and poverty elimination on global tuberculosis incidence: a statistical modelling analysis of Sustainable Development Goal 1. Lancet Glob Health. 2018;6(5):e514–22.
Dunachie S, Chamnan P. The double burden of diabetes and global infection in low and middle-income countries. Trans R Soc Trop Med Hyg. 2019;113(2):56–64.
Odone A, Houben RM, White RG, Lönnroth K. The effect of diabetes and undernutrition trends on reaching 2035 global tuberculosis targets. Lancet Diabetes Endocrinol. 2014;2(9):754–64.
FAO, IFAD and WFP. 2015. The State of Food Insecurity in the World 2015 [Internet document]. Meeting the 2015 international hunger targets: taking stock of uneven progress. Rome: FAO, 2015. Available from: https://www.fao.org/3/a-i4646e.pdf. Cited on 02.11.2021
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Int J Surg. 2014;12(12):1495–9.
Howell DC. Statistical methods in human sciences. New York: Wadsworth; 1998.
The World Bank Group. World Bank Country and Lending Groups [Internet document]. New York: World Bank, 2020 . Available from: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups. Cited on 04.01.2020
The British Medical Journal. Correlation and regression [Internet]. London: The British Medical Journal, 2020 . Available from: https://www.bmj.com/about-bmj/resources-readers/publications/statistics-square-one/11-correlation-and-regression. Cited on 05.09.2020
Bell A, Fairbrother M, Jones K. Fixed and Random effects models: making an informed choice. Qual Quant. 2019;53:1051–74. https://doi.org/10.1007/s11135-018-0802-x.
Boccia D, Hargreaves J, De Stavola BL, et al. The association between household socioeconomic position and prevalent tuberculosis in Zambia: a case-control study. PLoS ONE. 2011;6(6):e20824.
Bhargava A, Pai M, Bhargava M, Marais BJ, Menzies D. Can social interventions prevent tuberculosis? The Papworth experiment (1918–1943) revisited. Am J Respir Crit Care Med. 2012;186:442–9.
Nery JS, Rodrigues LC, Rasella D, Aquino R, Barreira D, Torrens AW, Boccia D, Penna GO, Penna MLF, Barreto ML, Pereira SM. Effect of Brazil’s conditional cash transfer programme on tuberculosis incidence. Int J Tuberc Lung Dis. 2017;21(7):790–6.
Hollo V, Amato-Gauci A, Kodmon C, Manissero D. Tuberculosis in the EU and EEA/ EFTA countries: what is the latest data telling us? Euro Surveill. 2009;14. pii:19151.
D’Ambrosio L, Centis R, Spanevello A, Migliori GB. Improving tuberculosis surveillance in Europe is key to controlling the disease. Euro Surveill. 2010;15. pii:19513.
Reeves A, Basu S, McKee M, Stuckler D, Sandgren A, Semenza J. Social protection and tuberculosis control in 21 European countries, 1995–2012: a cross-national statistical modelling analysis. Lancet Infect Dis. 2014;14(11):1105–12.
Zumla A, Malon P, Henderson J, et al. Impact of HIV infection on tuberculosis. Postgrad Med J. 2000;76:259–68.
Imtiaz S, Shield KD, Roerecke M, Samokhvalov AV, Lönnroth K, Rehm J. Alcohol consumption as a risk factor for tuberculosis: meta-analyses and burden of disease. Eur Respir J. 2017;50(1):1700216.
Goldhaber-Fiebert JD, Jeon CY, Cohen T, Murray MB. Diabetes mellitus and tuberculosis in countries with high tuberculosis burdens: individual risks and social determinants. Int J Epidemiol. 2011;40(2):417–28. https://doi.org/10.1093/ije/dyq238. Epub 2011 Jan 20. PMID: 21252210; PMCID: PMC3621385.
Xiang K, Xu Z, Hu YQ, He YS, Dan YL, Wu Q, Fang XH, Pan HF. Association between ambient air pollution and tuberculosis risk: A systematic review and meta-analysis. Chemosphere. 2021;277:130342. https://doi.org/10.1016/j.chemosphere.2021.130342. Epub 2021 Mar 23. PMID: 33794431.
Dooley KE, Chaisson RE. Tuberculosis and diabetes mellitus: convergence of two epidemics. Lancet Infect Dis. 2009;9(12):737–46. https://doi.org/10.1016/S1473-3099(09)70282-8. PMID:19926034;PMCID:PMC2945809.
Mendis S, Fukino K, Cameron A, Laing R, Filipe A Jr, Khatib O, Leowski J, Ewen M. The availability and affordability of selected essential medicines for chronic diseases in six low- and middle-income countries. Bull World Health Organ. 2007;85(4):279–88. https://doi.org/10.2471/blt.06.033647. PMID:17546309;PMCID:PMC2636320.
Kirigia JM, Sambo HB, Sambo LG, Barry SP. Economic burden of diabetes mellitus in the WHO African region. BMC Int Health Hum Rights. 2009;31(9):6. https://doi.org/10.1186/1472-698X-9-6. PMID:19335903;PMCID:PMC2674592.
Wahdan MH. The epidemiological transition. EMHJ - Eastern Mediterranean Health Journal, 1996;2 (1), 8–20, 1996 https://apps.who.int/iris/handle/10665/118829.
Freedman DA. Ecological Inference and the Ecological Fallacy. International Encyclopedia of the Social & Behavioral Sciences. 1999;Technical Report No. 549.
United Nations Development Programme. COVID-19 AND HUMAN DEVELOPMENT: Assessing the Crisis, Envisioning the Recovery [Internet document]. New York: United Nations Development Programme, 2021. Available from: http://hdr.undp.org/sites/default/files/covid-19_and_human_development_0.pdf. Cited on 25.07.2021
World Health Organization. Contributing to health system strengthening—guiding principles for national tuberculosis programmes [Internet document]. Geneva: World Health Organization, 2008. Available from: https://www.who.int/healthsystems/Stop_TB_HSS_policy_paper_EN.pdf. Cited on 27.11.2021
Lönnroth K, Roglic G, Harries AD. Improving tuberculosis prevention and care through addressing the global diabetes epidemic: from evidence to policy and practice. Lancet Diabetes Endocrinol. 2014;2(9):730–9.
International Diabetes Federation. IDF DIABETES ATLAS Ninth edition 2019 [Internet document]. Brussels, International Diabetes Deferation: 2019. Available from: https://www.diabetesatlas.org/upload/resources/material/20200302_133351_IDFATLAS9e-final-web.pdf. Cited on 30.08.2021
Uthman OA, Okwundu C, Gbenga K, Volmink J, Dowdy D, Zumla A, Nachega JB. Optimal Timing of Antiretroviral Therapy Initiation for HIV-Infected Adults With Newly Diagnosed Pulmonary Tuberculosis: A Systematic Review and Meta-analysis. Ann Intern Med. 2015;163(1):32–9.
Acknowledgements
Not applicable.
Funding
Open access funding provided by Karolinska Institute. The authors received no financial support for the research, authorship, and/or publication of this article from a pharmaceutical company or other agency. All authors have full access to the data in the study and accept responsibility to submit for publication.
Author information
Authors and Affiliations
Contributions
Fiona A. Költringer: Conceptualisation, data collection and management, formal analysis, methodology, writing – original draft, review & editing; Kristi Sidney Annerstedt: Conceptualisation, methodology, writing – review & editing; Delia Boccia: Conceptualisation, writing – review & editing; Daniel J. Carter: Conceptualisation, methodology, writing – review & editing; William E. Rudgard: Conceptualisation, formal analysis, methodology, writing – original draft, review & editing, project supervision. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Költringer, F.A., Annerstedt, K.S., Boccia, D. et al. The social determinants of national tuberculosis incidence rates in 116 countries: a longitudinal ecological study between 2005–2015. BMC Public Health 23, 337 (2023). https://doi.org/10.1186/s12889-023-15213-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-023-15213-w