Abstract
Background
In middle-aged and particularly older adults, body mass index (BMI) is associated with various health outcomes. We examined associations between physical activity (PA) and longitudinal BMI change in persons aged ≥ 50 years.
Methods
The sample included 5159 community-dwelling individuals aged ≥ 50 years (50.5% males, mean (SD) age 73.0 (10.2) years at baseline) who were enrolled in the Mayo Clinic Study of Aging (MCSA). Participants had information on PA within one year of baseline assessment, BMI at baseline, and potential follow-up assessments (mean (SD) follow-up 4.6 (3.7) years). Linear mixed-effect models were used to calculate the association between PA (moderate-vigorous physical activity, MVPA; and all PA composite score) and the longitudinal change in BMI, adjusted for baseline age, sex, education and medical comorbidities. In addition to interactions between years since baseline and PA, we also included 2- and 3-way interactions with baseline age to further assess whether age modifies the trajectory of BMI over time.
Results
We observed a decrease in BMI among participants engaging at a mean amount of PA (i.e., MVPA: 2.7; all PA: 6.8) and with a mean age (i.e., 73 years) at baseline (MVPA: estimate = -0.047, 95% CI -0.059, -0.034; all PA: estimate = -0.047, 95% CI -0.060, -0.035), and this decline is accelerated with increasing age. Participants with a mean age (i.e., 73 years) that engage at an increased amount of MVPA or all PA at baseline (i.e., one SD above the mean) do not decrease as fast with regard to BMI (MVPA: estimate = -0.006; all PA: estimate = -0.016), and higher levels of MVPA or all PA at baseline (i.e., two SD above the mean) were even associated with an increase in BMI (MVPA: estimate = 0.035; all PA: estimate = 0.015). Finally, MVPA but not all PA is beneficial at slowing BMI decline with increasing age.
Conclusion
PA, particularly at moderate-vigorous intensity, is associated with slower decline in longitudinal BMI trajectories. This implies that engaging in PA may be beneficial for healthy body weight regulation in middle and late adulthood.
Similar content being viewed by others
Introduction
The prevalence of overweight and obesity in adults has been increasing over past decades [1]. A growing body of research has demonstrated relationships between higher body weight or body mass index (BMI) and all-cause mortality [2], as well as various medical conditions [3]. While human body weight regulation is complex, engaging in physical activity (PA) is generally associated with reduced body weight or fat in young and middle-aged adults (e.g., [4]). Similarly, longitudinal studies in adults have demonstrated associations between PA and reduced risk of onset of several metabolic diseases including overweight and obesity (e.g., [5]), dementia [6, 7] as well as all-cause mortality [8].
In contrast, among older adults, weight loss, particularly at rapid decline, may be associated with undesirable health outcomes. For example, a more pronounced decline in weight or BMI per decade from mid- to late-life was associated with an increased risk of incident mild cognitive impairment [9]. Similarly, greater BMI instability was associated with faster cognitive decline over an average follow-up of 6 years [10]. However, conflicting results on the association between BMI and cognitive decline have been reported, e.g. studies have shown that a higher BMI may be associated with an increased risk of dementia in longitudinal follow-up (i.e., when BMI was assessed > 20 years before dementia diagnosis), but with a decreased risk of dementia in relatively shorter follow-up (i.e., when BMI was assessed < 10 years before dementia diagnosis [11]). Other studies have also reported associations between a lower BMI and increased risk of mortality [12] or disability in activities of daily living [13] among older community-dwelling persons.
Few studies investigated the associations between PA and BMI in older adults, and results are inconsistent. For example, studies reported an increase in impairments of activities of daily living for persons aged ≥ 65 years with obesity compared to those with low or normal body weight [14], as well as an association between lower levels of PA and physical function in obese individuals aged ≥ 60 years [15]. However, another study reported lower odds of physical and functional impairment when engaging in moderate to vigorous intensity exercise at least once per week in a sample of obese older adults [16].
The aim of this study was to examine the longitudinal associations between PA and BMI trajectories in community-dwelling persons aged ≥ 50 years. Based on previous literature, marked BMI instability in old age is associated with undesirable health outcomes. It is therefore critical to investigate whether engagement in PA is associated with change in BMI over time. These findings may be relevant for the promotion of a healthy lifestyle in clinical practice, particularly among older persons.
Methods
Study design and sample
This prospective study was conducted in the setting of the population-based Mayo Clinic Study of Aging (MCSA) in Olmsted County, Minnesota, USA [17]. We included 5159 individuals aged ≥ 50 years with available data on PA within 12 months of baseline assessment, and BMI at baseline and potential follow-up assessments. Participants were followed forward in time for a mean of 4.6 years. The MCSA protocols have been approved by the institutional review boards (IRB) of Mayo Clinic and Olmsted Medical Center in Rochester, MN, USA. All participants provided written informed consent before participation. In the case of participants with cognitive impairment sufficient to interfere with capacity, consent was obtained from a legally authorized representative.
Measurement of predictor variables
PA was measured at baseline using a self-reported questionnaire [18,19,20], derived from two validated instruments, i.e., the 1985 National Health Interview Survey and the Minnesota Heart Survey intensity codes [21, 22]. This questionnaire has been used in previous studies on PA in the context of aging and cognitive impairment [19, 20]. Details of the survey was reported elsewhere [16]; briefly, the questionnaire inquired about engagement in PA as well as exercise in late-life (i.e., over the past one year) and distinguished between three intensity levels by providing examples for each level: (1) light PA (such as laundry, vacuuming, making beds or dusting); (2) moderate PA (such as scrubbing floors, washing windows, gardening or raking leaves); (3) heavy PA (such as carrying heavy objects, heavy digging, pushing a mower or hard manual labor); (4) light physical exercise (such as leisurely walking or slow dancing); (5) moderate physical exercise (such as hiking or swimming); and (6) vigorous physical exercise (such as jogging or playing tennis singles). Participants were asked to provide information about the frequency at which they carried out these activities: ≤ 1 time per month, 2–3 times per month, 1–2 times per week, 3–4 times per week, 5–6 times per week, and daily. For the purpose of this study, we calculated two scores: (1) A late-life all PA composite score by taking light, moderate, and vigorous physical activities and exercise, converting each to days per week, adding them up and dividing the total by 2 to get an overall score. The scores range from 0 to 21, with a higher score indicating higher level of PA. (2) A late-life moderate-vigorous physical activity (MVPA) score by adding the days per week variables for moderate and vigorous exercise. Both scores were z- scored for use in the models.
Measurement of outcome variables
Participants’ weight (in kg) and height (in m) was measured at each study visit to calculate BMI according to the formula: kg/m2. For descriptive purpose, we categorized participants into six BMI groups [23]: <18.5 (underweight), ≥ 18.5 to < 25 (normal/ healthy weight), ≥ 25 to < 30 (overweight), ≥ 30 to < 35 (obesity class I), ≥ 35 to < 40 (obesity class II), ≥ 40 (obesity class III). BMI was measured every 15 months on average.
Covariates
We assessed age, sex, years of education based on ten different educational level determinations (e.g., high school diploma = 12 years, Bachelor’s degree = 16 years, Master’s degree = 18 years, etc.), and medical comorbidity as assessed through the weighted Charlson Index [24].
Statistical analysis
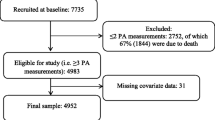
We calculated linear mixed-effect models with random subject-specific intercepts and slopes to examine the association between late-life PA at baseline and change in BMI over time. In our models, the PA variables were the independent variables (predictors), and the trajectories for individual yearly longitudinal change in BMI were the dependent variables (outcomes). We only included participants who had information on PA, years of education, and Charlson Index at baseline, respectively; were aged ≥ 50 years; and had information on BMI at baseline and potentially follow-up assessments. For a detailed flow chart on the sample selection, please refer to Fig. 1. All models included PA (z-scored), sex, time in years from baseline, age (z-scored), education years and Charlson comorbidity index and 2- and 3-way interactions amongst PA, age, and time in years since baseline. We conducted the analyses separately for all PA (z-scored composite score) and z-scored MVPA score. To help visualize the results, given that 2- and 3-way interactions can be difficult to interpret, we created plots (please refer to Fig. 2 and Fig. 3) utilizing the fixed effects equations from our models. In each plot are four lines showing BMI trajectory over time for (1) those with average PA and average age, (2) those with average PA and age one standard deviation (SD) above the mean, (3) those with PA one SD above the mean and average age, and (4) those with both PA and age one SD above the mean, respectively. All covariates were considered to have the average value for the purposes of the plots. All statistical analyses were done using the conventional two-tailed alpha level of 0.05 and performed with SAS 9.4 (SAS Institute, Inc; Cary, NC) and R, version 4.1.2 (R Foundation for Statistical Computing, Vienna, Austria).
Results
Detailed descriptive demographics at baseline are shown in Table 1. In our sample of 5159 participants, the mean (SD) age was 73.0 (10.2) years, and the mean (SD) BMI at baseline was 28.6 (5.6). The mean (SD) follow-up was 4.6 (3.7) years. 914 participants had one assessment of BMI, 812 participants had two assessments, 640 participants had three assessments, 573 had four assessments, and 2220 participants had ≥ five assessments of BMI. The mean (SD) times of follow-up BMI assessments was of 4.4 (2.8).
Association of MVPA (last 12 months) and change in BMI
Participants engaging at an average amount of MVPA over the past 12 months and at the average age at baseline, decrease in BMI annually (estimate = -0.047, 95% CI [-0.059, -0.034], p < 0.0001) (Table 2). Those that are at the average for MVPA but are older at baseline (i.e., someone who is one SD above the mean age), fall even faster in terms of their BMI (-0.047–0.041 = -0.088). On the other hand, participants at the average age that perform an increased amount of MVPA (i.e., someone who is one SD above the mean MVPA) do not decrease as fast on BMI (-0.047 + 0.041 = -0.006), and at higher levels of MVPA (i.e., someone who is two SD above the mean in MVPA), BMI starts to increase over time (-0.047 + 2*0.041 = 0.035). There was also a marginally significant positive (estimate = 0.012, 95% CI [-0.001, 0.026], p = 0.068) 3-way interaction between years since baseline, age at baseline, and MVPA. This means that, the older one gets, the more beneficial MVPA is at mitigating BMI decline, as displayed in Fig. 2.
Association of all PA (last 12 months) and change in BMI
Participants engaging at an average amount of all PA over the past 12 months and at the average age at baseline, decrease in BMI annually (estimate = -0.047, 95% CI [-0.060, -0.035], p < 0.0001) (Table 3). Those that are at the average for all PA but are older at baseline (i.e., someone who is one SD above the mean in age), fall even faster in terms of their BMI (-0.047 – 0.040 = -0.087). On the other hand, participants at the average age that perform an increased amount of all PA (i.e., someone who is one SD above the mean all PA) do not decrease as fast on BMI (-0.047 + 0.031 = -0.016), and at higher levels of all PA (i.e., someone who is two SD above the mean in all PA), BMI starts to increase over time (-0.047 + 2*0.031 = 0.015). We did not observe a 3-way interaction (estimate = -0.002, 95% CI [-0.015, 0.012], p = 0.806) between years since baseline, age at baseline, and all PA, as displayed in Fig. 3.
Discussion
Among participants engaging at a mean amount of PA (i.e., MVPA score of 2.7, or all PA score of 6.8) and with a mean age at baseline (i.e., 73 years), we observed a decrease in BMI over time. This decline is accelerated with increasing age. In addition, participants with a mean age (i.e., 73 years) that engaged at an increased amount of MVPA or all PA at baseline did not decrease as fast with regard to BMI, and higher levels of MVPA or all PA were even associated with an increase in BMI. Finally, MVPA but not all PA, is more beneficial at slowing BMI decline with increasing age. This result indicates that particularly PA engagement at higher intensities rather than overall PA may be important to slow a decline of BMI that may negatively impact health.
Previous longitudinal research has reported conflicting results. For example, studies have demonstrated a stable or decreasing BMI over time [25, 26], whereas others found an increase in BMI over time, albeit with differing trajectories for specific age groups (i.e., up to old age [25,26,27,28]). Results from longitudinal studies on the association between baseline levels of PA and BMI changes over time focusing on older adults are scarce, while those on middle-aged adults are conflicting [29, 30]. For example, some studies reported a significant association between higher levels of PA at baseline and a decreasing BMI [31] or a reduced weight gain [32, 33]. Whereas, other studies did not find such an association [34, 35]. The conflicting findings may be due to different sample sizes with regard to age, sex distribution, recruitment, as well as different study methodology, particularly with regard to the assessment of PA. Therefore, our study expands on the existing body of literature by showing that particularly MVPA may be associated with slower BMI decline over time in older adults.
We did not examine potential mechanisms that may explain our observed association between PA and slower decline in BMI trajectories in older adults. However, it has been postulated in the literature that BMI is not exclusively influenced by PA. Other behavioral factors such as nutrition (e.g. [36]), longitudinal patterns of PA behavior, e.g. stability of PA engagement over the lifespan [37, 38] as well as metabolic mechanisms related to PA (e.g. [39]) or socio economic status (e.g. [40]) may impact body weight management. Furthermore, in adults, a high BMI is usually due to a high fat mass which is associated with negative effects on health and may lead to reduced quality of life due to functional impairment [41]. However, of note, weight loss in older adults is mostly characterized by decline in lean body mass (particularly muscle mass) and is associated with an increased mortality, whereas a decline in body fat mass is associated with a reduced mortality [42]. As the mean age of our sample was 73 years at baseline, a low BMI may actually indicate a reduced skeletal muscle mass, which in turn is related to a reduction of physical functioning and an increased risk of falls [43]. In addition, weight gain in older adults may be beneficial for maintaining cognitive functioning, whereas weight loss should be avoided; and this has been referred to in literature as the obesity paradox in cognition [44]. Indeed, several studies reported that a decline in BMI was associated with an increased risk of incident mild cognitive impairment [9], faster rates of cognitive decline [45], as well as decreased cognitive performance [46] or abilities [47]. Since cognitive status may have an impact on the association between PA and BMI trajectories, we additionally adjusted our models for cognitive status at baseline (i.e., being cognitively unimpaired, or having mild cognitive impairment or dementia). However, this additional adjustment did not alter our results and conclusions (data not shown). In general, future research should explore potential mechanism that may explain our observations that PA and MVPA are differently associated with longitudinal BMI depending on the age of participants. One may hypothesize that this difference is due to types of PA or PA stimulus, personal (e.g., health) conditions, body composition, or BMI limitations when relating it to PA.
The strengths of our study are the follow-up period of 4.6 years, and the large sample of more than 5000 community-dwelling older individuals. Major limitations pertain to the use of a self-reported questionnaire to assess PA which may be likely to induce recall bias. However, previous research in a different sample derived from the MCSA has shown that our PA questionnaire has moderate to good internal consistency, and test-retest correlation coefficients range between 0.33 for vigorous intensity activity and 0.50 for moderate intensity activity [18]. Furthermore, only 26% of participants were not overweight or obese at baseline, which may have limited our ability in the statistical analyses to capture meaningful changes in BMI. There is limited evidence of an association between greater amounts of PA and attenuated weight gain with the effect diminishing with increasing age [30]. Further longitudinal studies are needed, particularly to investigate the effects of increasing or decreasing PA over time on BMI trajectories, and also the impact of continued versus interrupted PA engagement over the lifespan on BMI trajectories. In addition, with regard to the outcome of interest (i.e. BMI trajectories), it would be interesting to examine whether the PA related change in BMI is due to loss of lean body mass (mainly muscle mass) or body fat mass, which may have different implications for health in older adults. Additionally, future studies should also consider dietary intake as a covariate.
Conclusion
In conclusion, we found that PA, particularly at moderate-vigorous intensity, carried out within 12 months of baseline data acquisition, is associated with a slower decrease in BMI. Given that a decline in BMI in old age can have negative health consequences, our findings underline the importance of engaging in PA to limit unhealthy weight loss in old age, and of promoting a healthy lifestyle, including but not limited to regular PA, in clinical practice, particularly among older persons who are at risk of unhealthy weight loss.
Availability of data and materials
The datasets used and analyzed during the current study are available to qualified researchers from the Mayo Clinic Study of Aging upon reasonable request (https://www.mayo.edu/research/centers-programs/alzheimers-disease-research-center/data-requests).
Abbreviations
- BMI:
-
Body mass index
- kg:
-
Kilograms
- m:
-
Meters
- MCSA:
-
Mayo Clinic Study of Aging
- MVPA:
-
Moderate-vigorous physical activity
- N:
-
Number of participants
- PA:
-
Physical activity
- SD:
-
Standard deviation
References
NCD Risk Factor Collaboration. Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19·2 million participants. The Lancet. 2016;387:1377–96. https://doi.org/10.1016/S0140-6736(16)30054-X
Global BMI, Mortality Collaboration. Body-mass index and all-cause mortality: individual-participant-data meta-analysis of 239 prospective studies in four continents. The Lancet. 2016;388:776–86. https://doi.org/10.1016/S0140-6736(16)30175-1
Samper-Ternent R, Al Snih S. Obesity in older adults: epidemiology and implications for disability and disease. Rev Clin Gerontol. 2012;22:10–34. https://doi.org/10.1017/s0959259811000190
Tremblay A, Després JP, Leblanc C, Craig CL, Ferris B, Stephens T, Bouchard C. Effect of intensity of physical activity on body fatness and fat distribution. Am J Clin Nutr. 1990;51:153–7. https://doi.org/10.1093/ajcn/51.2.153
Cleven L, Krell-Roesch J, Nigg CR, Woll A. The association between physical activity with incident obesity, coronary heart disease, diabetes and hypertension in adults: a systematic review of longitudinal studies published after 2012. BMC Public Health. 2020;20:726. https://doi.org/10.1186/s12889-020-08715-4
Tolppanen A-M, Solomon A, Kulmala J, Kåreholt I, Ngandu T, Rusanen M, et al. Leisure-time physical activity from mid- to late life, body mass index, and risk of dementia. Alzheimers Dement. 2015;11:434–443e6. https://doi.org/10.1016/j.jalz.2014.01.008
Krell-Roesch J, Feder NT, Roberts RO, Mielke MM, Christianson TJ, Knopman DS, et al. Leisure-time physical activity and the risk of Incident Dementia: the Mayo Clinic Study of Aging. J Alzheimers Dis. 2018;63:149–55. https://doi.org/10.3233/JAD-171141
Warburton DER, Nicol CW, Bredin SSD. Health benefits of physical activity: the evidence. CMAJ. 2006;174:801–9. https://doi.org/10.1503/cmaj.051351
Alhurani RE, Vassilaki M, Aakre JA, Mielke MM, Kremers WK, Machulda MM, et al. Decline in weight and incident mild cognitive impairment: Mayo Clinic Study of Aging. JAMA Neurol. 2016;73:439–46. https://doi.org/10.1001/jamaneurol.2015.4756
Aiken-Morgan AT, Capuano AW, Arvanitakis Z, Barnes LL. Changes in body Mass Index are related to faster cognitive decline among african american older adults. J Am Geriatr Soc. 2020;68:2662–7. https://doi.org/10.1111/jgs.16814
Kivimäki M, Luukkonen R, Batty GD, Ferrie JE, Pentti J, Nyberg ST, et al. Body mass index and risk of dementia: analysis of individual-level data from 1.3 million individuals. Alzheimers Dement. 2018;14:601–9. https://doi.org/10.1016/j.jalz.2017.09.016
Landi F, Zuccalà G, Gambassi G, Incalzi RA, Manigrasso L, Pagano F, et al. Body mass index and mortality among older people living in the community. J Am Geriatr Soc. 1999;47:1072–6. https://doi.org/10.1111/j.1532-5415.1999.tb05229.x
Lv Y-B, Yuan J-Q, Mao C, Gao X, Yin Z-X, Kraus VB, et al. Association of Body Mass Index with disability in activities of Daily living among chinese adults 80 years of age or older. JAMA Netw Open. 2018;1:e181915. https://doi.org/10.1001/jamanetworkopen.2018.1915
Woo J, Leung J, Kwok T. BMI, body composition, and physical functioning in older adults. Obes (Silver Spring). 2007;15:1886–94. https://doi.org/10.1038/oby.2007.223
Riebe D, Blissmer BJ, Greaney ML, Garber CE, Lees FD, Clark PG. The relationship between obesity, physical activity, and physical function in older adults. J Aging Health. 2009;21:1159–78. https://doi.org/10.1177/0898264309350076
Germain CM, Vasquez E, Batsis JA. Physical activity, Central Adiposity, and functional Limitations in Community-Dwelling older adults. J Geriatr Phys Ther. 2016;39:71–6. https://doi.org/10.1519/JPT.0000000000000051
Roberts RO, Geda YE, Knopman DS, Cha RH, Pankratz VS, Boeve BF, et al. The Mayo Clinic Study of Aging: design and sampling, participation, baseline measures and sample characteristics. Neuroepidemiology. 2008;30:58–69. https://doi.org/10.1159/000115751
Geda YE, Roberts RO, Knopman DS, Christianson TJH, Pankratz VS, Ivnik RJ, et al. Physical exercise, aging, and mild cognitive impairment: a population-based study. Arch Neurol. 2010;67:80–6. https://doi.org/10.1001/archneurol.2009.297
Krell-Roesch J, Syrjanen JA, Bezold J, Trautwein S, Barisch-Fritz B, Boes K, et al. Physical activity and trajectory of cognitive change in older persons: Mayo Clinic Study of Aging. J Alzheimers Dis. 2021;79:377–88. https://doi.org/10.3233/JAD-200959
Krell-Roesch J, Syrjanen JA, Vassilaki M, Barisch-Fritz B, Trautwein S, Boes K, et al. Association of non-exercise physical activity in mid- and late-life with cognitive trajectories and the impact of APOE ε4 genotype status: the Mayo Clinic Study of Aging. Eur J Ageing. 2019;16:491–502. https://doi.org/10.1007/s10433-019-00513-1
Folsom AR, Caspersen CJ, Taylor HL, Jacobs DR, Luepker RV, Gomez-Marin O, et al. Leisure time physical activity and its relationship to coronary risk factors in a population-based sample. Minn Heart Surv Am J Epidemiol. 1985;121:570–9. https://doi.org/10.1093/oxfordjournals.aje.a114035
National Center for Health Statistics. Current estimates from the National Health interview survey. United States, 1985. Vital Health Stat. 1986;10:i–iv.
World Health Organization. Obesity - preventing and managing the global epidemic: report on a WHO Consultation. Geneva: World Health Organization; 2000.
Charlson ME, Pompei P, Ales KL, MacKenzie C. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83. https://doi.org/10.1016/0021-9681(87)90171-8
Chiu P-W, Yu T, Kukreti S, Strong C. BMI Trajectory In Relation to Cause-Specific Mortality In Taiwan’s Adult Population; 2021.
Zajacova A, Huzurbazar S, Greenwood M, Nguyen H, Long-Term BMI. Trajectories and health in older adults: hierarchical clustering of functional curves. J Aging Health. 2015;27:1443–61. https://doi.org/10.1177/0898264315584329
Huang F, Zhang M, Li Y, Li Z, Fang J, Guo K. The longitudinal trajectory of body mass index in the chinese population: a latent growth curve analysis. PLoS ONE. 2018;13:e0207845. https://doi.org/10.1371/journal.pone.0207845
Tittlbach SA, Jekauc D, Schmidt SCE, Woll A, Bös K. The relationship between physical activity, fitness, physical complaints and BMI in german adults - results of a longitudinal study. Eur J Sport Sci. 2017;17:1090–9. https://doi.org/10.1080/17461391.2017.1347963
Fogelholm M, Kukkonen-Harjula K. Does physical activity prevent weight gain–a systematic review. Obes Rev. 2000;1:95–111. https://doi.org/10.1046/j.1467-789x.2000.00016.x
Jakicic JM, Powell KE, Campbell WW, Dipietro L, Pate RR, Pescatello LS, et al. Physical activity and the Prevention of Weight Gain in adults: a systematic review. Med Sci Sports Exerc. 2019;51:1262–9. https://doi.org/10.1249/MSS.0000000000001938
Botoseneanu A, Liang J. The effect of stability and change in health behaviors on trajectories of body mass index in older Americans: a 14-year longitudinal study. J Gerontol A Biol Sci Med Sci. 2012;67:1075–84. https://doi.org/10.1093/gerona/gls073
Hamer M, Brunner EJ, Bell J, Batty GD, Shipley M, Akbaraly T, et al. Physical activity patterns over 10 years in relation to body mass index and waist circumference: the Whitehall II cohort study. Obes (Silver Spring). 2013;21:E755–61. https://doi.org/10.1002/oby.20446
Lee I-M, Djoussé L, Sesso HD, Wang L, Buring JE. Physical activity and weight gain prevention. JAMA. 2010;303:1173–9. https://doi.org/10.1001/jama.2010.312
Williamson DF, Madans J, Anda RF, Kleinman JC, Kahn HS, Byers T. Recreational physical activity and ten-year weight change in a US national cohort. Int J Obes Relat Metab Disord. 1993;17:279–86.
Parker DR, Gonzalez S, Derby CA, Gans KM, Lasater TM, Carleton RA. Dietary factors in relation to weight change among men and women from two southeastern New England communities. Int J Obes Relat Metab Disord. 1997;21:103–9. https://doi.org/10.1038/sj.ijo.0800373
Alfadda AA, Sallam RM, Park J. Diet and Nutrition for Body Weight Management. J Obes. 2019;2019:6798096. https://doi.org/10.1155/2019/6798096
Telama R, Yang X, Viikari J, Välimäki I, Wanne O, Raitakari O. Physical activity from childhood to adulthood: a 21-year tracking study. Am J Prev Med. 2005;28:267–73. https://doi.org/10.1016/j.amepre.2004.12.003
Gordon-Larsen P, Nelson MC, Popkin BM. Longitudinal physical activity and sedentary behavior trends: adolescence to adulthood. Am J Prev Med. 2004;27:277–83. https://doi.org/10.1016/j.amepre.2004.07.006
Imierska M, Kurianiuk A, Błachnio-Zabielska A. The influence of physical activity on the bioactive lipids metabolism in Obesity-Induced muscle insulin resistance. Biomolecules. 2020. https://doi.org/10.3390/biom10121665
Laaksonen M, Sarlio-Lähteenkorva S, Leino-Arjas P, Martikainen P, Lahelma E. Body weight and health status: importance of socioeconomic position and working conditions. Obes Res. 2005;13:2169–77. https://doi.org/10.1038/oby.2005.269
Seidell JC, Visscher TL. Body weight and weight change and their health implications for the elderly. Eur J Clin Nutr. 2000;54(Suppl 3):33–9. https://doi.org/10.1038/sj.ejcn.1601023
Allison DB, Zannolli R, Faith MS, Heo M, Pietrobelli A, VanItallie TB, et al. Weight loss increases and fat loss decreases all-cause mortality rate: results from two independent cohort studies. Int J Obes Relat Metab Disord. 1999;23:603–11. https://doi.org/10.1038/sj.ijo.0800875
Reid KF, Pasha E, Doros G, Clark DJ, Patten C, Phillips EM, et al. Longitudinal decline of lower extremity muscle power in healthy and mobility-limited older adults: influence of muscle mass, strength, composition, neuromuscular activation and single fiber contractile properties. Eur J Appl Physiol. 2014;114:29–39. https://doi.org/10.1007/s00421-013-2728-2
Kronschnabl JM, Kneip T, Weiss LM, Bergmann M. Bodyweight change and cognitive performance in the older population. PLoS ONE. 2021;16:e0249651. https://doi.org/10.1371/journal.pone.0249651
Arvanitakis Z, Capuano AW, Bennett DA, Barnes LL. Body Mass Index and decline in cognitive function in older Black and White Persons. J Gerontol A Biol Sci Med Sci. 2018;73:198–203. https://doi.org/10.1093/gerona/glx152
Driscoll I, Espeland MA, Wassertheil-Smoller S, Gaussoin SA, Ding J, Granek IA, et al. Weight change and cognitive function: findings from the Women’s Health Initiative Study of Cognitive Aging. Obes (Silver Spring). 2011;19:1595–600. https://doi.org/10.1038/oby.2011.23
Dahl AK, Hassing LB, Fransson EI, Gatz M, Reynolds CA, Pedersen NL. Body mass index across midlife and cognitive change in late life. Int J Obes (Lond). 2013;37:296–302. https://doi.org/10.1038/ijo.2012.37
Acknowledgements
We acknowledge support by the KIT-Publication Fund of the Karlsruhe Institute of Technology.
Funding
This research was supported by R01AG057708. The Mayo Clinic Study of Aging is supported by the NIH (U01 AG006786, P30 AG062677, R37 AG011378, R01 AG041851), the Alexander Family Alzheimer’s Disease Research Professorship of the Mayo Clinic, GHR, Mayo Foundation for Medical Education and Research, the Liston Award, the Schuler Foundation and used the resources of the Rochester Epidemiology Project (REP) medical records linkage system, which is supported by the National Institute on Aging (AG 058738), by the Mayo Clinic Research Committee, and by fees paid annually by REP users.
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
LC: interpretation of the data, drafting the manuscript, revising the manuscript. JAS: analysis and interpretation of the data, revising the manuscript. YEG: data collection, study funding, revising the manuscript. LRC: analysis and interpretation of the data, revising the manuscript. RCP: data collection, study funding, revising the manuscript. MV: interpretation of the data, revising the manuscript. AW: revising the manuscript. JKR: design and conceptualization of the study, interpretation of the data, revising the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The MCSA protocols have been approved by the institutional review boards (IRB) of Mayo Clinic and Olmsted Medical Center in Rochester, MN, USA. All methods were performed in accordance with the relevant guidelines and regulations. All participants provided written informed consent before participation. In the case of participants with cognitive impairment sufficient to interfere with capacity, consent was obtained from a legally authorized representative.
Consent for publication
Not applicable.
Competing interests
Yonas E. Geda receives funding from the NIH and Roche, and served on Lundbeck Advisory Board. Maria Vassilaki has received research funding from F. Hoffmann-La Roche Ltd and Biogen and consulted for F. Hoffmann-La Roche Ltd, outside of this study; currently she receives research funding from NIH and has equity ownership in Abbott Laboratories, Johnson and Johnson, Medtronic, AbbVie, Merck, and Amgen. Ronald C. Petersen serves as a consultant for Roche, Inc., Merck, Inc., Biogen, Inc., Eisai, Inc., Genentech, Inc. Eli Lilly, Inc., and Nestle, Inc., served on a DSMB for Genentech, receives royalties from Oxford University Press and UpToDate, and receives NIH funding. The other authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Cleven, L., Syrjanen, J.A., Geda, Y.E. et al. Association between physical activity and longitudinal change in body mass index in middle-aged and older adults. BMC Public Health 23, 202 (2023). https://doi.org/10.1186/s12889-023-15119-7
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-023-15119-7