Abstract
Background
Much scholarly debate has centered on Bangladesh's family planning program (FPP) in lowering the country's fertility rate. This study aimed to investigate the prevalence of using modern and traditional contraceptive methods and to determine the factors that explain the contraceptive methods use.
Methods
The study used data from the 2017–18 Bangladesh Demographic and Health Survey (BDHS), which included 11,452 (weighted) women aged 15–49 years in the analysis. Multilevel multinomial logistic regression was used to identify the factors associated with the contraceptive method use.
Results
The prevalence of using modern contraceptive methods was 72.16%, while 14.58% of women used traditional methods in Bangladesh. In comparison to women in the 15–24 years age group, older women (35–49 years) were more unwilling to use modern contraceptive methods (RRR: 0.28, 95% CI: 0.21–0.37). Women who had at least a living child were more likely to use both traditional and modern contraceptive methods (RRR: 4.37, 95% CI: 3.12–6.11). Similarly, given birth in the previous 5 years influenced women 2.41 times more to use modern method compared to those who had not given birth (RRR: 2.41, 95% CI: 1.65–3.52). Husbands'/partners’ decision for using/not using contraception were positively associated with the use of both traditional (RRR: 4.49, 95% CI: 3.04–6.63) and modern methods (RRR: 3.01, 95% CI: 2.15–4.17) rather than using no method. This study suggests rural participants were 21% less likely to utilize modern methods than urban participants (RRR: 0.79, 95% CI: 0.67–0.94).
Conclusion
Bangladesh remains a focus for contraceptive use, as it is one of the most populous countries in South Asia. To lower the fertility rate, policymakers may design interventions to improve awareness especially targeting uneducated, and rural reproductive women in Bangladesh. The study also highlights the importance of male partners’ decision-making regarding women's contraceptive use.
Similar content being viewed by others
Introduction
In many countries around the world, sexual and reproductive health (SRH) is a serious public health issue, particularly for women [1]. SRH care is referenced in Goal 3 of the United Nations' Sustainable Development Goals (SDGs), which aims to ensure universal access to sexual and reproductive healthcare services, including family planning, information, and education [1]. Contraception is an unique among medical interventions in terms of the breadth of its good consequences and effectiveness as a method of FP and fertility control, conducive for the betterment of the mother and child the health [2,3,4]. While family planning (FP) is acknowledged as one of the century's greatest public health successes, and global acceptance is growing [5]. It has been regarded as one of just a few sustainable, cost-effective interventions that can have an instant impact on women and their families and reach far beyond the individual level [6]. As a result of its inclusion in the Millennium Development Goals (MDGs) and Sustainable Development Goals (SDGs) as an indicator for tracking progress on improving maternal health, family planning helps protect women from high-risk pregnancies, unsafe abortions, reproductive tract infections, and sexually transmitted infections (STIs), including HIV/AIDS [7, 8].
At least 200 million women around the world want to utilize family planning that is both safe and effective however, they are unable to do so, resulting in undesired pregnancies [5]. Abortion is performed on more than 50 million of the 190 million women who fall pregnant each year. Increased contraceptive use in poor nations has resulted in a 40% reduction in maternal fatalities over the last two decades just by reducing the number of unintended pregnancies [9]. However, in Bangladesh, the rising trend in contraceptive prevalence rate (CPR) has paused (e.g., 61.0% in 2011, 62.4% in 2014, and 62.0% in 2017), while the lowering trend in total fertility rate (TFR) has also stalled (2.3 children per woman from 2011 to 2017) [10]. The Government of Bangladesh has set a goal of increasing CPR by 75% by 2021, achieving a below replacement level of fertility (i.e., less than 2.1 children per woman), in order to halt population growth and further enhance mother and child health [11]. Despite the declining TFR in Bangladesh has been observed, special attention should be paid to the use of contraceptives by women of reproductive age in this country, as Bangladesh still has a long way to go to reach the target CPR level of more than 70% [12].To sustain the CPR's upward trend by addressing contraceptive use hurdles, the Government of Bangladesh's family planning initiatives must adopt an evidence-based pragmatic approach. Additional efforts are needed to boost CPR and by identifying the factors of using contraceptive methods that have a significant impact on CPR in Bangladesh, this study may contribute to policymaking to reduce the fertility rate [11].
Several previous Bangladeshi studies identified different sociodemographic factors like women’s age, women's educational level, household wealth status, women working status, administrative division, place of residence, religion, number of household members, breastfeeding practice, husband’s education are significantly associated with contraceptive use [4, 13]. While a growing number of literature suggests that parity, autonomy, desire for children, partner communication [14,15,16], women amenorrheic status, abstaining status, total children born in last five years, and total children ever died have been linked to the use of contraceptives [13]. Preference for sons was also associated with the use of contraceptives among Bangladeshi women [17]. Evidence also shows a significant association between couples’ joint participation in household decision-making and contraceptive use in Bangladesh [18]. A study by Khan et. al., among reproductive aged bangladeshi women reported that having diabetes and hypertension are also linked with the use of contraceptive method, while women having both diabetes and hypertension are more prone to use traditional contraceptive method [19]. Another finding from Bangladesh demonstrates that women's patterns of taking contraception remained unchanged even after experiencing an unexpected pregnancy, while about 54% of women who said they had not taken a contraception before becoming pregnant used modern method after giving birth [20]. Promoting and increasing the contraceptive prevalence rate among women of reproductive age has also been demonstrated to be an effective public health strategy for improving maternal and child health outcomes [21, 22]. Numerous studies demonstrate that increasing CPR directly reduces maternal mortality by reducing unwanted pregnancies, teenage pregnancies, unsafe abortions, and high-risk pregnancies, as well as allowing for pregnancies to be spaced [23, 24].
While several studies have looked at the factors that influence modern contraceptive use only, and very few studies [4, 13, 25] considered both traditional and modern methods; however, these studies applied binary logistic regression after constructing binary outcome variable of current contraception use. Thus, separate determinants of using traditional as well as modern contraception use were not identified among Bangladeshi women.. There is a need to better understand the factors that are associated with the use and choice of method of contraceptives, as the use of contraceptives is suboptimal [26]. Besides, a periodic inspection of prevalence and risk factors is required in order to track its current situation, since high CPR is always expected for controlling births for populous counties like Bangladesh. Therefore, this study would be an addition to fulfill the research gaps. Consequently, this study investigates the prevalence of use of both modern and traditional contraceptive methods and their associated determinants among women of reproductive age in Bangladesh by applying multilevel multinomial logistic regression analysis.
Methods
Data source
We used a secondary data set of the most recent Bangladesh Demographic and Health Survey (BDHS) 2017/18 for this study. The survey was carried out from October 2017 to March 2018 under the National Institute of Population Research and Training (NIPORT), and Ministry of Health and Family Welfare, Bangladesh to ascertain the population’s health status. An overview of the ethical procedure, survey procedure, methodology, sampling, and survey tools could be found in the final report of the BDHS 2017/18 which is publicly available [27].
Sampling and study design
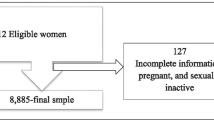
The sampling design of BDHS 2017/18 consisted of a two-stage stratified approach to select the households from a list of enumeration areas (EAs) [27]. Initially, a total of 675 EAs or clusters were selected in this survey as primary sampling units (PSUs). Then, a total of 20,250 households (6,810 in urban and 13,440 in rural) were selected from these PSUs using the stratified sampling method [27]. The married women of reproductive age (15 to 49 years) were interviewed to collect information on the use of contraception methods [27]. From the selected households, 20,376 eligible women were selected for individual interviews from which 20,127 completed their interviews with a response rate of 98.8%. The exclusion criteria of selecting participants have been shown in Fig. 1. Finally, a weighted sample of 11,452 (unweighted 11,523) women who gave information on their contraceptive use was included in the final analysis of this study.
Outcome measure
Method of contraceptive use among married, non-pregnant Bangladeshi women of reproductive age was the primary outcome variable of this study. The contraceptive methods were categorized into 3 groups: using no method (coded as 0), using the traditional method (coded as 1), and using the modern method (coded as 2). It was assessed based on the participants’ self-report of using contraceptives at the time of the survey by asking the following question: “Are you currently doing something or using any method to delay or avoid getting pregnant?”. Those who responded positively were then asked to indicate the specific method they were using individually or in concurrence with their partner [27]. The methods were considered modern when participants used female sterilization, injections, implant/norplant, pills, intrauterine device (IUD), injection, emergency contraception, female condom, and lactational amenorrhea method (LAM). While the traditional methods included periodic abstinence and withdrawal [27, 28].
Explanatory variables
The explanatory variables for contraceptive utilization among women were selected on the basis of previous literatures [13, 18, 29, 30] and the availability of the variables in the BDHS 2017–18 dataset. The explanatory variables along with their categories have been shown in Table 1.
Statistical analysis
Both unweighted and weighted frequencies and percentages were calculated to show the background characteristics of study participants. Considering the complex survey of BDHS, we used the “svy” command in STATA version 17.0 (StataCorp, College Station, TX, USA) for assigning the sample weight to adjust for clustering effect and sample stratification. Since the BDHS 2017/18 used a two-stage stratified cluster sampling having a hierarchical composition, a multilevel regression model would be appropriate to consider the cluster variation in the analysis [31]. Thus, to consider the cluster effect in the analysis, the multilevel multinomial regression model was used to identify the association between outcome and explanatory variables where clusters (EAs) were considered as level-2 factors. We used generalized structural equation modeling (GSEM) using the “gsem” command in STATA to estimate the model. The GSEM model assessed the fixed effects of various explanatory variables and also assessed random effects at the cluster level. Multicollinearity among explanatory variables was checked using variance inflation factor (VIF). The adjusted relative risk ratio (RRR) along with 95% confidence interval (CI) were interpreted and statistical significance was considered when a p-value was less than 0.05.
Results
Background characteristics of study participants are presented in Table 2. A total of 11,452 (weighted) participants were included in the present study. The majority of the women (38.8%) were aged between 25 and 34 years, and 41.2% completed secondary education. Half of them (50.5%) were employed, and 56.2% had 1 to 2 living children. More than half of them (57.7%) had no birth in 5 years. More than two-thirds of them (78.4%) use contraception based on the joint decision. The women do not want to take more children was 65.0%. The maximum of them (42.2%) was rich in wealth household index, and almost one-third (69.4%) of them was from rural areas. Women from the Dhaka division were the highest (26.6%) participants. We found that the prevalence of using modern, and traditional contraceptive methods among Bangladeshi women were 72.2% (95% CI: 70.3–74 0.2) and 14.6% (95% CI: 12.3–16.7), respectively. While about 13.0% of participants did not use any contraceptive method (Fig. 2).
The variations in using contraception methods among Bangladeshi women by the selected individual, household, and community variables are presented in Table 3. Looking at the bivariate association, all the explanatory variables except the place of residence were significantly associated with the use of contraceptive methods of women.
In Table 4, results from the multilevel multinomial regression model show the likelihood (presented as relative risk ratio [RRR]) of using traditional, and modern contraceptive methods relative to using no contraceptive method. Table 4 also presents the random effects (measured as variance) at the cluster level. Compared to the younger aged women (15–24 years), the older aged women, 25–34 years, had significantly 49% (RRR: 0.51, CI: 0.39, 0.66) lower possibilities of using the traditional contraceptive method, while women aged 25–34 years and 35–49 years were 53% (RRR: 0.47, CI: 0.39, 0.56) and 72% (RRR: 0.28, CI: 0.21, 0.37) less likely to use the modern contraceptive method, respectively. Women with secondary education were 30% (RRR: 0.70, CI: 0.51, 0.97) less likely to use the traditional method compared to those having no education. However, the likelihood of traditional method use was 45% (RRR: 1.45, CI: 1.02, 2.05) higher among those whose husbands' education was higher compared to illiterate husbands.
Women who had at least a living child were 3.13 (RRR: 3.13, CI: 2.21, 4.45) times more likely to use the traditional method compared to the women who had no living child. Moreover, the likelihood of using the modern method was 3.54 (RRR: 3.54, CI: 2.81, 4.47) times higher among the women who had at least a living child compared to those who had no living child. Women who ever experienced terminated pregnancy were 23% (RRR: 0.77, CI: 0.63, 0.93) and 36% (RRR: 0.64, CI: 0.55, 0.75) less likely to use the traditional and modern method, respectively, compared to those who didn’t experience terminated pregnancy ever. Women giving one birth in the last 5 years were 1.52 (RRR: 1.52, CI: 1.21, 1.90) times more likely to use the traditional method compared to those who had no birth. Similarly, women who gave one birth, and two or more birth were 2.49 (RRR: 2.49, CI: 2.07, 2.98) and 2.41 (RRR: 2.41, CI: 1.56, 3.52) times more prone to use the modern method (Table 4).
The likelihood of using traditional and modern methods were 4.49 (RRR: 4.49, CI: 3.04, 6.63) times and 3.01 (RRR: 3.01, CI: 2.15, 4.17) times higher, respectively, while the decision to use contraception depended on husband/partner compared to the decision taken by women mainly. When the decision was taken jointly, the likelihood of using the traditional and modern method was 2.34 (RRR: 2.34, CI: 1.86, 2.94) times and 1.78 (RRR: 1.78, CI: 1.48, 2.15) times higher, respectively. The women who did not want to take more children were 18.10 (RRR: 18.10, CI: 13.87, 23.61) times and 20.16 (RRR: 20.16, CI: 16.19, 25.12) times more likely to use the traditional and modern method, respectively than those with a desire for more children. Women knowing the ovulatory cycle were 1.93 (RRR: 1.93, CI: 1.63, 2.29) times and 1.19 (RRR: 1.19, CI: 1.04, 1.38) times more likely to use the traditional and modern method, respectively, than those who had not. The rural women were 21% (RRR: 0.79, CI: 0.67, 0.94) less likely to use the modern method than women from urban areas. Compared to the women from the Barisal division, the likelihood of using the modern method was 72% (RRR: 0.68, CI: 0.48, 0.95) less among the women from the Sylhet division. Finally, the cluster random effect was significant for traditional contraceptive method use versus using no method, and for modern contraceptive method versus using no method (Table 4).
Discussion
The study assessed the method of contraceptive use and their predictors among married, non-pregnant Bangladeshi women of the reproductive (15–49 years) age group using the current Bangladesh demographic and health survey dataset (2017–18). In this study, we found 72% of participants were using modern contraceptive method, indicating an increase from 62% found in 2014 among Bangladeshi women [13]. Similar to the modern method, use of traditional contraceptive method is also increased to 14.6% in this study from 8.1% found in 2014 [13], while about 37% Bangladeshi women didn’t use any contraceptive method in 2014 [13], and this figure has reduced to 13% in the present study. Since Bangladesh aimed to have a 75% contraceptive prevalence by 2020, the Health, Population and Nutrition Sector Development Program (HPNSDP) of Bangladesh established strategic goals to enhance the general use of family planning by making family planning services available, acceptable, and cheap to all men and women of reproductive age [32, 33]. These could be plausible reasons of increasing use of contraceptive method in Bangladesh.
The use of modern contraception methods was reported by more than two in three women with the highest use observed in the 25–34 age group. According to a previous study [34], young girls and women are more likely to plan to take contraception which corroborates the findings of the present study. The fact that young women may not intent to be pregnant early, while many older women are not sexually active or have reduced their coital frequency may be connected to older women's decreased propensity to utilize contraception [34]. Sexually active female adolescents from other LMICs in Asia and Africa also frequently experience societal and health system barriers in accessing contraception that is linked to unwanted pregnancies and adverse pregnancy outcomes [35, 36].
In this study, education status of the women or even their husbands were not independently associated with the decision for acceptance of modern contraception methods a finding similar to that observed in the previous BDHS (2011–14) [13]. However, globally, several studies amongst LMICs in Asia and Africa suggest increased demand for modern contraceptive methods with higher educational status of women that often correlates with their desire for career planning and development [30, 37, 38]. Moreover, a previous study from Nepal [39] suggests that substantially higher educational status of husbands compared to wives is an independent predictor for their acceptance of condoms for routine contraception purposes. A previous round of the BDHS (2011) had found that contraception use was higher in the employed women in contradiction to the current round where contraception use was greater in the unemployed women [25]. Furthermore, the positive employment status of the married women in the present study did not indicate any statistically significant increase in their use of any contraception method after adjustment for covariates.
Women in this study having 3 or more children were more likely to use both MC and traditional methods compared to those having no living children, a factor that strongly correlates with the desire to have no more children, indicative of the achievement of desired family size. A previous study in East African countries also argued that women who have more children are more likely to use a modern contraceptive method [38]. Previous study also suggests that completion of desired family size is a reliable indicator of willingness to use MC methods [38]. However, one in five women in this group were still using only traditional methods of contraception which have a high risk of failure and unintended pregnancies. Consequently, family planning programs in the country may encourage women using traditional conraceptive methods to switch to those modern methods that are compatible with their socio-cultural milieu [40]. In the current study, women's preference for having children was a significant factor of contraceptive usage. Contraception use was more prevalent among women who didn't desire more children than among those who did. This result is consistent with the earlier research [4, 41].
In this study, women with a history of terminated pregnancy were significantly less likely to use any contraceptive method. This finding is in line with the previous study in Nepal [42], and Malawi [34]. However, the inclusion of past experiences with terminated pregnancies as a factor warrants further discussion because it might either be an unwanted naturally terminated pregnancy (miscarriage) or one that was purposefully terminated [34].
In this study, the use of both modern and traditional methods was reported by the women as primarily a decision by the husband and significantly less likely to be a joint decision. However, similar to the BDHS 2011 round, the practice of spousal joint decision making was observed to increase the likelihood of practicing modern contraceptive methods [18].However, a contradictory finding was observed in another study where women who were empowered to exercise sexual autonomy were most likely to enhance their capacity to utilize modern contraception regardless of their educational levels [43]. This finding demonstrate the necessity of involvement of men in the Bangladesh family planning and reproductive health programmes has been long recognized for nearly three decades and the present analysis also indicates that men are the primary decision-makers in the Bangladeshi society with regards to determining their family size and the acceptance of contraception by their wives [13, 44].
Awareness of the ovulation period was a significant predictor of any type of contraception use by women in this study, a finding corroborated by evidence from previous studies where the authors identified that women who knew their ovulation cycle were more likely to use contraception than those who did not know their cycle [45, 46]. The likelihood of using contraception to prevent conception during the ovulatory phase may be higher among women who are aware of their ovulatory cycle than among those who are unaware of it [46].. Future research needs to be directed towards understanding the association between choice of contraception method and knowledge of ovulatory cycle so that the policymakers could assess whether interventions designed to improve the knowledge of the reproductive cycle in Bangladeshi women could enhance their acceptability of modern contraceptive methods.
According to the study, women in rural regions use modern contraception less frequently than those in urban. This result was in line with earlier research conducted in Bangladesh [4] and Ethiopia [29, 47]. This can be due to rural women's inferior access to maternal health care service, such as contraception [29]. Another possible causes for observed inequalities in contraceptive usage between rural and urban areas include differences in cultural views and beliefs [46]. Besides, Urban women are more likely to use any type of contraception and have better access to contraception as a whole [48].
One of the strengths of this study was using the most recent nationally representative (BDHS 2017–18) data set. And also, this study used the multilevel model to consider the cluster effect on the determinant factors of contracetion methods use in Bangladesh which is the appropriate analysis approach for such data set. We identified the determinats of both traditional and modern contraception methods among Bangladeshi women. There are a few study limitations. First, data on some variables such as joint families and the opinion of mothers-in-law regarding contraception use were not captured. Similarly, the opinion of men regarding their acceptance of barrier methods of contraception by themselves or any modern contraception methods by their female partners was also not included.
Conclusions
The study finds about one-fourth of Bangladeshi women of reproductive age did not use any form of modern contraception. Women with 3 or more children and those having awareness of women’s ovulatory cycle were significantly more likely to use contraceptive methods, However, women's education, occupation, and household wealth did not significantly improve their likelihood of using any contraception method. Husbands were also the key drivers of decision-making in regulating the fertility of their wives but shared decision-making by both husband and wife considerably augmented the acceptability of modern contraception technologies. These findings suggest that women's empowerment for health promotion requires delicate messaging that encourages their participation in planning and deciding on their family size while reducing taboos and misconceptions about modern contraception methods.
Availability of data and materials
The data that support the findings of this study are available from Demographic and Health Surveys (DHS) Program dataset of Bangladesh (https://dhsprogram.com/) but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of Bangladesh Demographic and Health Surveys (BDHS) Program.
Abbreviations
- SRH:
-
Sexual and Reproductive Health
- SDG:
-
Sustainable Development Goal
- FP:
-
Family Planning
- STI:
-
Sexually Transmitted Infections
- CPR:
-
Contraceptive Prevalence Rate
- TFR:
-
Total Fertility Rate
- BDHS:
-
Bangladesh Demographic and Health Survey
- EAs:
-
Enumeration Areas
- PSU:
-
Primary Sampling Unit
- RRR:
-
Relative Risk ratio
- CI:
-
Confidence Interval
- WHO:
-
World Health Organization
References
Nguyen TT, Neal S. Contraceptive prevalence and factors influencing utilization among women in Pakistan: a focus on gender-based violence. Fulbright Rev Econ Policy. 2021;1:119–34.
Rahman M, Haque SE, Zahan S, Islam J, Rahman M, Asaduzzaman MD, et al. Maternal high-risk fertility behavior and association with chronic undernutrition among children under age 5 y in India, Bangladesh, and Nepal: do poor children have a higher risk? Nutrition. 2018;49:32–40.
Oye-Adeniran BA, Adewole IF, Umoh AV, Oladokun A, Gbadegesin A, Ekanem EE. Community-based study of contraceptive behaviour in Nigeria. Afr J Reprod Health. 2006;10:90–104.
Haq I, Sakib S, Talukder A. Sociodemographic factors on contraceptive use among ever-married women of reproductive age: evidence from three demographic and health surveys in Bangladesh. Med Sci. 2017;5:31.
Eo O, Vy A, Va W. Prevalence and determinants of contraceptive use among women of child-bearing age in a rural community in southern Nigeria. J Community Med Prim Heal Care. 2017;29:97–107.
Tsui AO, McDonald-Mosley R, Burke AE. Family planning and the burden of unintended pregnancies. Epidemiol Rev. 2010;32:152–74.
Starbird E, Norton M, Marcus R. Investing in family planning: key to achieving the sustainable development goals. Glob Heal Sci Pract. 2016;4:191–210.
Arbab AA, Bener A, Abdulmalik M. Prevalence, awareness and determinants of contraceptive use in Qatari women. East Mediterr Health J. 2011;17(1):11–8.
Cleland J, Conde-Agudelo A, Peterson H, Ross J, Tsui A. Contraception and health. Lancet. 2012;380:149–56.
National Institute of Population Research and Training (NIPORT), ICF International. Bangladesh Demographic and Health Survey 2017–18. Dhaka, Bangladesh, and Rockville, Maryland, USA; 2020.
Kamrul Islam M, Rabiul Haque M, Hema PS. Regional variations of contraceptive use in Bangladesh: a disaggregate analysis by place of residence. PLoS ONE. 2020;15:1–18.
National Institute of Population Research, Training, Mitra and Associates and II. Bangladesh Demographic and Health Survey 2011. 2013.
Hossain MB, Khan MHR, Ababneh F, Shaw JEH. Identifying factors influencing contraceptive use in Bangladesh: evidence from BDHS 2014 data. BMC Public Health. 2018;18:1–14.
Nagase T, Kunii O, Wakai S, Khaleel A. Obstacles to modern contraceptive use among married women in southern urban Maldives. Contraception. 2003;68:125–34.
Islam R, Islam AZ, Rahman M. Unmet need for family planning: experience from urban and rural areas in Bangladesh. Public Heal Res. 2013;3:37–42.
Rahman MM, Islam AZ, Islam MR. Rural-urban differentials of knowledge and practice of contraception in Bangladesh. J Popul Soc Stud [JPSS]. 2010;18:87–110.
Hoq MN. Influence of the preference for sons on contraceptive use in Bangladesh: a multivariate analysis. Heliyon. 2020;6: e05120.
Islam AZ. Factors affecting modern contraceptive use among fecund young women in Bangladesh: does couples’ joint participation in household decision making matter? Reprod Health. 2018;15:1–9.
Khan MN, Islam MM, Islam RM. Pattern of contraceptive use among reproductive-aged women with diabetes and/or hypertension: findings from Bangladesh demographic and health survey. BMC Womens Health. 2022;22:1–8.
Khan MN, Islam MM. Women’s experience of unintended pregnancy and changes in contraceptive methods: evidence from a nationally representative survey. Reprod Health. 2022;19:1–11.
Seltzer JR. The origins and evolution of family planning programs in developing countries. Rand Corporation; 2002.
Ahmed S, Li Q, Liu L, Tsui AO. Maternal deaths averted by contraceptive use: an analysis of 172 countries. Lancet. 2012;380:111–25.
World Health Organization. Contraception fact sheet. Hum Reprod Programe. 2012;:4.
Nonvignon J, Novignon J. Trend and determinants of contraceptive use among women of reproductive age in Ghana. African Popul Stud. 2014;:956–67.
Islam AZ, Mondal MNI, Khatun ML, Rahman MM, Islam MR, Mostofa MG, et al. Prevalence and determinants of contraceptive use among employed and unemployed women in Bangladesh. Int J MCH AIDS. 2016;5:92.
Blackstone SR, Iwelunmor J. Determinants of contraceptive use among Nigerian couples: evidence from the 2013 demographic and health survey. Contracept Reprod Med. 2017;2:1–8.
NIPORT and ICF. Mitra and associates. Dhaka, Bangladesh: ICF International. Bangladesh Demographic and Health Survey 2017–18. Dhaka, Bangladesh, and Rockville, Maryland, USA: NIPORT and ICF; 2020.
Hubacher D, Trussell J. A definition of modern contraceptive methods. Contraception. 2015;92:420–1.
Dagnew GW, Asresie MB, Fekadu GA, Gelaw YM. Modern contraceptive use and factors associated with use among postpartum women in Ethiopia; further analysis of the 2016 Ethiopia demographic and health survey data. BMC Public Health. 2020;20:1–9.
Kabagenyi A, Habaasa G, Rutaremwa G. Low contraceptive use among young females in Uganda: does birth history and age at birth have an influence? analysis of, 2011 demographic and health survey. J Contracept Stud. 2016;1(1):4.
Khan HR, Shaw E. Multilevel logistic regression analysis applied to binary contraceptive prevalence data. J Data Sci. 2011;9:93–110.
Ministry of health and family welfare (mohfw) [Bangladesh]. Strategic Plan for Health, Population, and Nutrition Sector Development Program 2011–16. Dhaka, Bangladesh. 2011. http://www.nationalplanningcycles.org/planning-cycle/BGD. Accessed 8 Dec 2022.
FP2020 Commitment Maker. Family Planning 2020 Commitment: Bangladesh. https://fp2030.org/bangladesh. Accessed 8 Dec 2022.
Forty J, Rakgoasi SD, Keetile M. Patterns and determinants of modern contraceptive use and intention to usecontraceptives among Malawian women of reproductive ages (15–49 years). Contracept Reprod Med. 2021;6:1–12.
Olika AK, Kitila SB, Terfa YB, Olika AK. Contraceptive use among sexually active female adolescents in Ethiopia: trends and determinants from national demographic and health surveys. Reprod Health. 2021;18:1–11.
Chandra-Mouli V, McCarraher DR, Phillips SJ, Williamson NE, Hainsworth G. Contraception for adolescents in low and middle income countries: needs, barriers, and access. Reprod Health. 2014;11:1–8.
Liu DH, Raftery AE. How do education and family planning accelerate fertility decline? Popul Dev Rev. 2020;46:409–41.
Bakibinga P, Matanda DJ, Ayiko R, Rujumba J, Muiruri C, Amendah D, et al. Pregnancy history and current use of contraception among women of reproductive age in Burundi, Kenya, Rwanda, Tanzania and Uganda: analysis of demographic and health survey data. BMJ Open. 2016;6: e009991.
Gubhaju B. The influence of wives’ and husbands’ education levels on contraceptive method choice in Nepal, 1996–2006. Int Perspect Sex Reprod Health. 2009;35(4):176–85.
Bishwajit G, Tang S, Yaya S, Feng Z. Unmet need for contraception and its association with unintended pregnancy in Bangladesh. BMC Pregnancy Childbirth. 2017;17:1–9.
Worku AG, Tessema GA, Zeleke AA. Trends of modern contraceptive use among young married women based on the 2000, 2005, and 2011 Ethiopian demographic and health surveys: a multivariate decomposition analysis. PLoS ONE. 2015;10: e0116525.
Khanal V, Joshi C, Neupane D, Karkee R. Practices and perceptions on contraception acceptance among clients availing safe abortion services in Nepal. Kathmandu Univ Med J. 2011;9:179–84.
Viswan SP, Ravindran TKS, Kandala N-B, Petzold MG, Fonn S. Sexual autonomy and contraceptive use among women in Nigeria: findings from the demographic and health survey data. Int J Womens Health. 2017;9:581.
Piet-Pelon NJ, Rob U. Male involvement in the Bangladesh family planning and reproductive health program. Int Q Community Health Educ. 1997;17:195–206.
Nyarko SH. Prevalence and correlates of contraceptive use among female adolescents in Ghana. BMC Womens Health. 2015;15:1–6.
Mandiwa C, Namondwe B, Makwinja A, Zamawe C. Factors associated with contraceptive use among young women in Malawi: analysis of the 2015–16 Malawi demographic and health survey data. Contracept Reprod Med. 2018;3:1–8.
Mengesha ZB, Worku AG, Feleke SA. Contraceptive adoption in the extended postpartum period is low in Northwest Ethiopia. BMC Pregnancy Childbirth. 2015;15:1–6.
Hussain N. Demographic, socio-economic and cultural factors affecting knowledge and use of contraception differentials in Malda District, West Bengal. Community Med Heal Educ. 2011;1.
Acknowledgements
Authors want to thank Demographic Health Surveys (DHS) for providing the datasets with no cost and permit us for using the data for independent research.
Funding
The author(s) received no specific funding for this work.
Author information
Authors and Affiliations
Contributions
Satyajit Kundu: Conceptualization, methodology, data curation, formal analysis, writing-original draft, writing-review & editing, supervision; Subarna Kundu: Data curation, formal analysis, writing-original draft; Md. Ashfikur Rahman: Writing-original draft, writing-review & editing; Humayun Kabir: Writing-original draft, writing-review & editing; Md. Hasan Al Banna: Writing-original draft, writing-review & editing; Saurav Basu: Writing-original draft, writing-review & editing; Hasan Mahmud Reza: writing-review & editing; Ahmed Hossain: Writing-original draft, writing-review & editing. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
We used secondary data set from the Demographic and Health Surveys (DHS) Programme for this study which is publicly available upon suitable request; therefore, further ethical approval was not required. Details of the ethical procedures followed by the DHS Program can be found in the BDHS report [10]. All the procedures were performed in accordance with the relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors have declared that no competing interest exist.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kundu, S., Kundu, S., Rahman, M.A. et al. Prevalence and determinants of contraceptive method use among Bangladeshi women of reproductive age: a multilevel multinomial analysis. BMC Public Health 22, 2357 (2022). https://doi.org/10.1186/s12889-022-14857-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-022-14857-4