Abstract
Background
Existing evidence suggests that the indigenous older population who live with their families and friends might experience lesser depressive symptoms due to better emotional support and well-being. The present study aimed to investigate the differentials in the prevalence of the major depressive disorder among tribal and non-tribal older populations in India and to explore the contribution of socio-demographic, health-related, and household factors in such disparities.
Methods
A cross-sectional study was conducted using data from the Longitudinal Aging Study in India (2017–18). The analytical sample included 30,637 older adults, among whom 5,025 and 25,612 belonged to the Scheduled Tribe (ST) and non-Scheduled Tribe (non-ST) social groups, respectively. Major depressive disorder assessed by the Composite International Diagnostic Interview short-form (CIDI-SF) scale was the outcome variable. Descriptive statistics, bivariate and multivariable regression and, decomposition analyses were conducted.
Results
About 4.8% and 8.9% of older adults from the ST and non-ST social groups had major depression. For both tribal and non-tribal groups, older adults who were unmarried, dissatisfied with living arrangements, and those who faced lifetime discrimination were at increased risk of major depression. Findings from differences due to characteristics (E) revealed that if the regional differences were minimized, it would decrease the ST-non-ST gap in major depression by about 19.6%. Similarly, equal self-rated health status and chronic conditions among ST and non-ST groups would decrease the gap in major depression by almost 9.6% and 7.9%, respectively. Additionally, an equal status of Instrumental Activities of Daily Living (IADL) and Activities of Daily Living (ADL) among older adults would decrease the gap in major depression by about 3.8% and 3% respectively. Also, findings from differences due to coefficients (C) revealed that if older adults from the ST group had the same status of ADL as of older adults from the non-ST group, it would decrease the gap in major depression by about 11.8%.
Conclusion
The findings revealed a greater prevalence of major depression in older adults belonging to the non-ST group than the ST group. For both tribal and non-tribal groups, older adults who were unmarried, dissatisfied with living arrangements, and those who faced lifetime discrimination were at increased risk of major depression and these factors along with health-related variables contributed to significant ST-non-ST gap in depression, advantageous to tribal population; suggesting further research on the coping mechanisms of mental illnesses among indigenous population in India.
Similar content being viewed by others
Introduction
With about 3.8% depressed population worldwide, a common mental health issue, depression, is slowly sneaking into the lives of people of all ages [1]. According to the World Health Organization, depression results from persistent sadness and a loss of interest in one’s usual activities, accompanied by an inability to carry out daily activities for at least two weeks [1]. Even though depression is preventable, studies show that more than 75% of individuals do not receive treatment in low-and-middle-income countries [2]. Such negligence is mostly due to the misconception that depression is a part of the ageing process, making the 60 years and above population more vulnerable [3].
India, one of the lower-middle-income countries, is no exception [3]. According to the National Mental Health Survey 2015–16, one in every 20 Indians suffers from depression [4]. Although the most affected age group were those aged 15–49 years, the continuous Indian demographic transition has generated health concerns for the aged people in recent years. According to the Longitudinal Aging Study in India, about 8.3% of older adults aged 60 years and above experienced major depression based on the Short Form Composite International Diagnostic Interview (CIDI-SF) scale [5]. Depression triggers many health problems like obesity, diabetes, heart disease, physical activeness, and vice-versa [6,7,8,9]. A complex interaction of social, psychological, and biological factors further triggers depression in an individual [10,11,12].
In India, inequities in health and healthcare utilization between advantaged and marginalized groups persisted throughout the years [13]. Extant research has demonstrated social status as a significant predictor of health disparities in India [14,15,16,17]. A study from the World Health Organization’s Survey of Global Ageing and Adult Health (WHO-SAGE) indicated higher mental health issues among Scheduled Castes and Muslims than among Higher caste Hindus [18]. Ample evidence shows the depression vulnerability of the tribal population in the Indian context [18,19,20,21]. Changing lifestyle, beliefs, and community living, moving to urban spaces, and triggering adverse life events like morbidity, unemployment, bereavement, stress, and psychological trauma are the emerging factors predisposing to mental health issues like depression [22].
Several studies have associated depression with lower socioeconomic status; however, a study indicated that emotional well-being (associated with depression) and life evaluation (associated with life satisfaction) have different correlates, which are often considered the same mistakenly [23]. For instance, there is a long-run question of whether money buys happiness or not. A study from the US shows that emotional well-being is highly associated with the positive and negative emotions created by circumstances like caring for a sick relative and spending time with family and friends. In contrast, life evaluation was highly associated with socioeconomic status [23]. The study concludes that a high income can bring life satisfaction but not happiness. According to these findings, the indigenous older population living with their families and friends might experience lesser depressive symptoms due to better emotional well-being. However, the long negligence of mental health issues in the tribal population also raises concern on their current situation.
Thus, the present study aimed to investigate differentials in the prevalence of depression among the tribal and non-tribal populations in India, primarily focusing on the vulnerable older population. Moreover, we explored the contribution of socio-demographic, health-related, and household factors to depression disparity across tribal and non-tribal older adults in India.
Materials and methods
Data source
The present study utilized the data from the baseline wave (wave 1) of the Longitudinal Aging Study in India (LASI), conducted during 2017–18. The LASI is a biennial panel survey representative of the older and elderly population age 45 and above for India and its states and union territories. The LASI wave 1 interviewed 42,949 households and 72,250 individuals aged 45 + years and their spouses across India’s 30 states and six union territories. It adopted a multistage stratified area probability cluster sampling design: a three-stage sampling design in rural areas and a four-stage sampling design in urban areas.
The LASI is a multi-topic, nationally representative, a large-scale survey conducted jointly by the International Institute for Population Sciences (IIPS), the Harvard T.H. Chan School of Public Health (HSPH), and the University of Southern California (USC). It is the Indian version of the Health and Retirement Studies (HRS). It provides vital information on chronic health conditions, symptom-based health conditions, demography, functional and mental health, household economic status, healthcare utilization, health insurance, work, employment and retirement, and life expectations of 45 years and above participants with their spouses, irrespective of age. Further details regarding the sample design, survey instruments, fieldwork, data collection and processing, and response rates are publicly available in the report [5].
Sample and participants
The Indian constitution divides the social groups into three broad categories- Scheduled Tribes [ST], Scheduled Caste [SC], and Other Backward Classes [OBC]. Those who do not fall in these groups are categorized as “Others”. Both SC and ST include mostly socially backward groups. OBC is socially and economically backward but has a much better situation than SC/ST. The ST group, which has a predominantly tribal population, comprises 8.6% of India’s population. Traditionally, these tribal groups reside away from mainstream Indian society and consume nature-based resources for daily health requirements [24, 25]. We have recoded the social group variable into ST (tribal or indigenous) and Non-ST groups in the present study.
In this study, we utilized the sample of 31,464 Indian older adults aged 60 years and above (5,173 belonging to the ST and 26,291 belonging to the non-ST groups). 827 older adults whose depression information was not available in the data were excluded from this study. Therefore, the analytical sample was 30,637 older adults, among whom 5,025 and 25,612 belonged to the ST and Non-ST social groups, respectively.
Outcome variable
The main outcome variable was major depression among older adults categorized as “Depressed” and “Not depressed”.
Major depression was assessed in LASI using the successfully tested and widely-utilized Composite International Diagnostic Interview short-form (CIDI-SF) scale that assesses psychiatric depression [5, 26]. There are ten questions and the response for all the items (except items “2” and “3”) were in binary format (i.e., “No” coded as 0, and “Yes” coded as 1). Again, those individuals who felt sad, blue or depressed “all day long” or “most of the day” were coded as “Yes”, else they were coded as “No”. Equivalently, individuals who felt sad, blue or depressed “every day” or “almost every day” were coded as “Yes”, else, they were coded as “No”. The scale had a Cronbach’s α reliability coefficient of more than 0.6. Next, we summated the ten items to obtain the CIDI-SF depression scale, with scores ranging from 0 to 10. Based on extant literature, Indian older adults with a score of 5 and more were categorized as “Depressed”, and those with a score of 4 and less were classified as “Not depressed” [27, 28].
Explanatory variables
Based on existing research, we included the following socio-demographic, health-related, and household characteristics in this study. The socio-demographic characteristics of older adults include the following –
-
1)
Age group was coded as (oldest-old, old-old, young-old). The young-old, old-old and oldest-old comprise older adults aged 60 to 69 years, 70 to 79 years, and 80 years or more, respectively.
-
2)
Gender was coded as (male, female).
-
3)
Marital status was coded as (currently married, currently not married).
-
4)
Status of work was coded as (never worked, currently not working, currently working, retired).
-
5)
The level of education was coded as (no formal education, upto primary, secondary and above).
-
6)
Social participation was coded as (socially active, socially inactive). LASI collected information on whether a person goes out of the house for eating, goes outdoors for relaxing, plays indoor games, plays outdoor games or exercises, visits relatives, attends cultural events, attends religious functions, attends group meetings, reads books, newspaper and magazines, watches television or listens to the radio, use a computer for electronic communication. Older adults who undertook any of the above social activities were classified as “socially active” and otherwise were classified as “socially inactive”.
-
7)
The importance of religion was coded as (not important, very important).
-
8)
Living arrangement satisfaction was coded as (satisfied, neutral, not satisfied).
-
9)
Received ill-treatment was coded as (no, yes) within one year from the interview.
-
10)
Faces discrimination in life was coded as (no, yes).
Next, the health-related characteristics of the older adults include –
-
11)
Self-rated health was coded as (good, average, poor).
-
12)
Chronic morbidity status was coded as (no condition, single condition, multiple conditions). LASI collected information on whether an older adult was ever diagnosed with hypertension or high blood pressure, diabetes or high blood pressure, cancer or malignant tumour, chronic lung diseases, chronic heart diseases, stroke, bone or joint diseases, any neurological or psychological problems, high cholesterol. Individuals having no diseases, any one of the diseases and two or more diseases were categorized into “no condition”, “single condition”, and “multiple conditions”.
-
13)
Physical activity status was coded as (physically inactive, physically active). Physical activity status was assessed based on WHO guidelines on physical activity for 18 years and above [29]. Older adults who performed at least 75 min of vigorous-intensity physical activity or at least 150 min of moderate-intensity physical activity in a day or a combination of both were classified as “Physically active” and otherwise were classified as “Physically inactive”.
-
14)
Difficulty in Activities of Daily Living (ADL) was coded as (no difficulty, faces difficulty). Information was collected on whether a person had difficulty in dressing, walking across a room, eating, going in or out of bed, bathing and using the toilet, respectively. During the interview, older adults who faced difficulty in any one of the activities for more than three months were categorized as “faces difficulty”. Those who did not have difficulty in any activities were included in the “no difficulty” category.
-
15)
Difficulty in Instrumental Activities of Daily Living (IADL) was coded as (no difficulty, faces difficulty). LASI obtained information on whether an individual had difficulty in the following seven instrumental activities of daily living: preparing a hot meal, shopping for groceries, making telephone calls, taking medications, doing work around the house or garden, managing household finance and getting around or reaching an unfamiliar place. During the interview, those who faced difficulty in any one of the activities for more than three months were categorized as “faced difficulty”. Else they were included in the “no difficulty” category.
-
16)
Covered by any health insurance was coded as (yes, no).
Further, the household-related characteristics are –
-
17)
Monthly per capita consumption expenditure was coded as (MPCE) quintile of household (poorest, poorer, middle, richer, richest).
-
18)
Religion was coded as (Hinduism, Islam, Others).
-
19)
The place of residence was coded as (Urban, Rural).
-
20)
The country region that a household is situated (Southern, Northern, Central, Western, Eastern, North-eastern). We constructed the country regions by including the erstwhile 29 states and six union territories of India into six categories based on administrative similarity. The northern part includes Chandigarh, Delhi, Haryana, Himachal Pradesh, erstwhile Jammu and Kashmir, Punjab, Uttaranchal and Rajasthan. The north-eastern region includes Arunachal Pradesh, Assam, Manipur, Meghalaya, Mizoram, Nagaland, Sikkim and Tripura. The central area consists of Madhya Pradesh and Chhattisgarh. The eastern zone consists of Bihar, Jharkhand, Odisha and West Bengal. The western region comprises Dadra and Nagar Haveli, Daman and Diu, Goa, Gujarat and Maharashtra. The southern part includes Andhra Pradesh, Karnataka, Kerala, Pondicherry and Tamil Nadu.
Statistical methods
The present study applied descriptive statistics, bivariate and multivariable regression and decomposition analyses to find out the results. Using the chi-square test for association, the bivariate analysis looked at the unadjusted link between major depression and health-related, socio-demographic, and household variables. The multivariate association was presented using average marginal effects (AME). Multivariable models did not violate the assumptions of multicollinearity.
We also applied the nonlinear multivariate decomposition method to determine the role of explanatory factors in the social divide in major depression among older adults in India. The ST-non-ST disparity in major depression is decomposed in both an overall and specific. The divide in major depression is decomposed into an endowments or features (E) component and a coefficients or effects (C) component in the overall decomposition. The contribution of each health-, and socio-demographic-, and household-related explanatory factor is dissected in-depth for each endowment and coefficient component of the difference in major depression among tribal and non-tribal groups. The endowments component (E) shows how difference in major depression would change if the distribution of older adults from the ST and non-ST groups for each category of the explanatory variable were similar. Suppose older adults from ST and non-ST groups were equally likely to fall into one of the explanatory variable’s categories. In that case, the coefficients component (C) indicates the expected change in the disparity. Decomposition models may be used to get various estimates for different reference categories of categorical data. We provide normalized decomposition estimates to solve this “identifying difficulty.” STATA software version 13 was used for all the statistical calculations in this study.
All methods were carried out in accordance with relevant guidelines and regulations.
Results
Descriptive statistics
Table 1 represents the distribution of ST and Non-ST older adults by socio-demographic, health-related and household characteristics in India. About 4.8% and 8.9% of older adults from ST and non-ST social groups had major depression. About 14.2% of older adults from ST category and 27.5% of older adults from non-ST category never worked. About 73.6% and 55.1% of older adults from ST and non-ST categories had no formal education, respectively. Nearly 29.7% and 20.5% of older adults from ST and non-ST categories did not give importance to religion, respectively. About 4.4% of older adults from ST category and 5.2% of older adults from non-ST category were not satisfied with their living arrangements. Almost 17.6% and 23.6% of the older adults from ST and non-ST categories had poor self-rated health, respectively. About 10.7% of older adults from ST category and 25.0% of older adults from non-ST category had multiple chronic conditions. Almost 38.5% and 26.7% of older adults from ST and non-ST categories were physically activity, respectively. Almost 19.5% & 43.6% of older adults from ST category and 23.2% & 48.0% of older adults from non-ST category had difficulty in ADL and IADL, respectively.
Figure 1 reveals the prevalence of depression among older adults by social groups in India. The highest prevalence of major depression was found among older adults from SC (9.9%) followed by OBC (9.0), Others (7.8%) and ST (4.8%) groups.
Bivariate analysis
Table 2 depicts the bivariate association between depression and socio-demographic, health-related, and household characteristics of ST and Non-ST older adults in India.
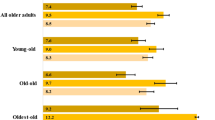
Figure 2 represents the weighted percentage of the total, Non-ST and ST older adults with major depression in India. It was found that in all the age groups, older adults from non-ST groups had higher prevalence of major depression.
Multivariate analysis
Table 3 represents the multivariate association between depression and socio-demographic, health-related and household characteristics of ST and Non-ST older adults in India. The odds of depression were higher among young-old in compairison to the odds of depression among oldest old in non-ST population (OR: 1.51; CI: 1.27–1.80). Among the ST (OR: 1.97; CI: 1.36—2.87) and non-ST (OR: 1.26; CI: 11.13—1.41) population, the odds of depression among currently non-married older adults were higher in reference to the odds to depression among currently married older adults. The likelihood of depression was high among currently working older adults in reference to older adults who never worked among non-ST population (OR: 1.29; CI: 1.10—1.52). The likelihood of depression was high among socially inactive older adilts in comparison to older adults who were socially active (OR: 1.45; CI: 1.24—1.70) in non-ST population. In the non-ST population the odds of depression were higher among older adults for whom religion was very important in comparison to the odds of depression among older adults for whom religion was not important (OR: 1.34; CI: 1.17—1.53). The likelihood of depression was high among older adults who were not satisfied with their current living arrangement (OR: 2.55; CI: 2.17—3.01), received ill treatment (OR: 2.02; CI: 1.70—2.40) and faced discrimination in life (OR: 1.68; CI: 1.49—1.90) in reference to their counterparts in both ST and non-ST population. Among the ST and non-ST population the likelihood of depression was high among older adults with poor SRH, multiple morbidity status and difficulty in ADL. The older adults who were physically active had higher odds of depression in reference to the odds of depression among older adults who were physically inactive in ST (OR: 1.86; CI: 1.24—2.79) and non-ST population (OR: 1.20; CI: 1.06—1.35).
Decomposing the caste differentials in depression
Table 4 reveals the overall decomposition of differential in depression among older adults from ST and non-ST groups in India. It was found that differences in effects (C) account for 56.2% of the observed social group differences in the prevalence of major depression. However, 43.8% of the differentials in major depression among ST and non-ST groups was explained by differences in compositional characteristics (E).
Table 5 represents the detailed decomposition (with normalized coefficients) of ST-non-ST differential in depression among older adults in India. Differences due to characteristics (E) is explained at first. It was revealed that if the regional differences were minimized, it would decrease the gap in major depression among ST and non-ST groups by about 19.6%. Similarly, an equal level of self-rated health and chronic conditions among ST and non-ST would result in reduced gap in major depression by almost 9.6% and 7.9%, respectively. Additionally, equal IADL and ADL difficulty among ST and non-ST older adults would result in reduced gap in major depression by about 3.8% and 3%, respectively. Moreover, if health insurance coverage is equalized among older adults from ST and non-ST populations, it would decrease the gap in major depression by about 3.4%.
Also, findings from differences due to coefficients (C) revealed that currently married status (8.6%) and being socially active (10.3%) significantly contributed to the ST-non-ST inequality in major depression in this study. Similarly, it was found that if older adults from non-ST population had the same status of ADL as of older adults from ST population, it would decrease the gap in major depression by about 11.8%. Similarly, if older adults from ST group had the same coverage of health insurance as of non-ST group, this would decrease the gap in major depression by almost 7.9%. Additionally, if older adults from non-ST population had same level of physical activity as of older adults from ST population, it would decrease the gap in major depression by about 5.7%.
Discussion
The present study investigated the differentials in the prevalence and determinants of major depression among ST and non-ST populations and decomposed the key socio-demographic, health, and household factors that accounted for the ST/non-ST-based inequalities in major depression among older adults in India by utilizing large-scale nationally representative survey data. The prevalence of major depression in the ST population was lower than the non-ST population (4.8% vs. 8.9%). Multiple studies based on indigenous tribal populations in India reported a lower prevalence of severe depression than in our study [30, 31]. For instance, a study conducted in the tribal community living in the Phek district of Nagaland, India, found that nearly 1.2% of older adults were experiencing depression [30]. Another recent study based on the tribal population of the Mysuru district in Karnataka, India, found a prevalence of severe depression of 3.5% among older adults [31]. In contrast, several other small-scale studies have reported a greater prevalence of depression in tribal older adults in India [32, 33]. The inconsistencies in the prevalence of depression may be partially due to variations in geographical areas, sample measures, and measurement tools.
Results from multivariable analysis demonstrated that physically active older adults had significantly higher odds of major depression than their physically inactive counterparts, which is inconsistent with most of the previous studies [34, 35]. This inconsistent relationship may be due to different definitions of physical activeness in other studies. This study did not find any association between various socio-demographic factors such as age and working status and major depression in the tribal population. On the other hand, in the non-tribal group, increasing age and current working status were significantly positively related to major depression. Moreover, other socio-demographic factors such as gender and educational attainments were unrelated to major depressive disorders in tribal and non-tribal populations.
There are possible explanations for the lower depressive symptoms in the ST population than in the non-ST population. Many studies have reported that tribal populations have a lower level of non-communicable chronic conditions [36], more physically active lifestyle [37, 38], healthy diet and lifestyles [39, 40], and belief in spiritual rituals that can play a significant role in healing and wellness [41]. On the other hand, these behaviors like physical activeness, lesser chronic conditions, healthy diet patterns, active lifestyles, and spiritual orientations have been associated with reduced depressive symptoms [42,43,44,45]. Therefore, it could be possible that such behaviors in tribal populations could effectively enhance mental health.
The decomposition analysis showed that the selected explanatory variables explained nearly 43.8% of the ST/non-ST inequality in major depression in the present study. The major contributors to the explained component were regional differences, self-rated health status, and chronic conditions. Around 19.6% of inequalities in major depression were attributed to regional differences; this is due to the dissimilarities in the distribution of ST and non-ST populations across different regions. For instance, as our data showed, the ST population is majorly concentrated in the north-eastern region, while a greater proportion of the non-ST population is concentrated in the northern and western regions of India. Differentials in self-rated health contributed to nearly 10% of the caste inequalities in the prevalence of major depression, resulting from the fact that a greater proportion of older adults in the non-ST group reported poor self-rated health than older adults in the ST group (23.4% vs. 14.9%). These findings are consistent with the other studies suggesting that poor self-rated health [46,47,48] is linked to having major depressive disorders in older persons.
Importantly, age, marital status and social participation contributed significantly to the ST-Non-ST differentials in major depression which may imply the greater buffering effects of increasing age, presence of structural support and participation in social activities on reducing major depression among older adults from ST category than those from non-ST group. Consistent with our findings, numerous studies have reported that widowhood and lack of social support can elevate stress, therefore, leading to higher levels of depression [49,50,51,52].
Nearly 8% of the inequalities in major depression were attributed to the differentials in the prevalence of chronic conditions among ST and non-ST populations; this is because a greater proportion of older adults in the non-ST group reported having multiple chronic conditions than older adults in the ST group (26.8% vs. 13.9%). Although studies related to chronic conditions in the tribal population in India are limited, the available studies reported a severe lack of awareness of chronic diseases among the tribal population in India [53]. However, in comparison to the general population, tribal population are expected to have lesser chances of cardiovascular diseases as they are physically active and are more prone to have plant-based foods. Another important contributor to the ST-non-ST differential in major depression was ADL and IADL functional difficulty. The findings are also in concordance with previous studies on the linkage between multiple chronic conditions [54, 55], functional limitations [56] and major depression.
There are some strengths and limitations of this study worth mentioning. The utilization of a large sample from a national representative survey in deriving the estimates is the potential strength of the study. An additional strength of the study is using the CIDI-SF scale for deriving reliable and valid estimates for major depression. There are potential limitations to the study. Firstly, our explanatory variables, such as self-reporting of the diagnosed chronic conditions, can be under-reported either due to unawareness about the chronic condition among the older adults or by recall bias. Moreover, the responses to the variables like self-rated health may be biased because individuals use response scales in systematically different ways. Finally, our results are based on the cross-sectional data; therefore, establishing a causal direction of the association of explanatory variables with major depression is not possible.
Conclusions
The present study found a greater prevalence of major depression in older adults in the ST group than in the non-ST group. A greater percentage of the ST/non-ST inequality in major depression, advantageous to tribal population in the present study was explained by age, marital status, and social participation, suggesting further research on the coping mechanisms of mental illnesses among the indigenous population in India. The ST-non-ST differentials in the major depression were also attributed to regional differences, self-rated health status, and chronic conditions, which need to be explored in future research.
Availability of data and materials
The study uses secondary data which is available on reasonable request through https://www.iipsindia.ac.in/content/lasi-wave-i
References
World Health Organization. Depression. 2021. https://www.who.int/news-room/fact-sheets/detail/depression. Accessed 10 Jan 2022.
Evans-Lacko S, Aguilar-Gaxiola S, Al-Hamzawi A, Alonso J, Benjet C, Bruffaerts R, et al. Socio-economic variations in the mental health treatment gap for people with anxiety, mood, and substance use disorders: results from the WHO World Mental Health (WMH) surveys. Psychol Med. 2018;48:1560–71.
Pilania M, Bairwa M, Kumar N, Khanna P, Kurana H. Elderly depression in India: an emerging public health challenge. Australas Med J. 2013;6:107.
Gururaj G, Varghese M, Benegal V, Rao G, Pathak K, Singh L, et al. National Mental Health Survey of India, 2015–16: Mental Health Systems. Bengaluru, India: National Institute of Mental Health and Neuro Sciences NIMHANS Publ; 2016.
The Longitudinal Ageing Study in India 2017–18 - National report. International Institute for Population Sciences, National Programme for Health Care of Elderly, Ministry of Health and Family Welfare, Harvard T. H. New Delhi: Chan School of Public Health, and the University of Southern California. India Report; 2020.
Renn BN, Feliciano L, Segal DL. The bidirectional relationship of depression and diabetes: a systematic review. Clin Psychol Rev. 2011;31:1239–46.
Da Silva MA, Singh-Manoux A, Brunner EJ, Kaffashian S, Shipley MJ, Kivimäki M, et al. Bidirectional association between physical activity and symptoms of anxiety and depression: the Whitehall II study. Eur J Epidemiol. 2012;27:537–46.
Wium-Andersen MK, Wium-Andersen IK, Prescott EIB, Overvad K, Jørgensen MB, Osler M. An attempt to explain the bidirectional association between ischaemic heart disease, stroke and depression: a cohort and meta-analytic approach. Br J Psychiatry. 2020;217:434–41.
Pan A, Sun Q, Czernichow S, Kivimaki M, Okereke OI, Lucas M, et al. Bidirectional association between depression and obesity in middle-aged and older women. Int J Obes. 2012;36:595–602.
Green M, Benzeval M. Ageing, social class and common mental disorders: longitudinal evidence from three cohorts in the West of Scotland. Psychol Med. 2011;41:565–74.
Triolo F, Harber-Aschan L, Belvederi MM, Calderón-Larrañaga A, Vetrano DL, Sjöberg L, et al. The complex interplay between depression and multimorbidity in late life: Risks and pathways: Depression and multimorbidity. Mechanisms Ageing Dev. 2020:111383.
Simon RW, Lively K. Sex, anger and depression. Soc Forces. 2010;88:1543–68.
Brinda EM, Attermann J, Gerdtham U-G, Enemark U. Socio-economic inequalities in health and health service use among older adults in India: results from the WHO Study on Global AGEing and adult health survey. Public Health. 2016;141:32–41.
Subramanian SV, Nandy S, Irving M, Gordon D, Lambert H, Davey SG. The mortality divide in India: the differential contributions of gender, caste, and standard of living across the life course. Am J Public Health. 2006;96:818–25.
Bora JK, Raushan R, Lutz W. The persistent influence of caste on under-five mortality: Factors that explain the caste-based gap in high focus Indian states. PLoS One. 2019;14:e0211086.
Deshpande A. Does caste still define disparity? A look at inequality in Kerala, India. Am Econ Rev. 2000;90:322–5.
Seth A, Tomar S, Singh K, Chandurkar D, Chakraverty A, Dey A, et al. Differential effects of community health worker visits across social and economic groups in Uttar Pradesh, India: a link between social inequities and health disparities. Int J Equity Health. 2017;16:1–9.
Gupta A, Coffey D. Caste, religion, and mental health in India. Popul Res Policy Rev. 2020;39:1119–41.
Kumar MM, Pathak VK, Ruikar M. Tribal population in India: a public health challenge and road to future. J Fam Med Primary Care. 2020;9:508.
Devarapalli SSK, Kallakuri S, Salam A, Maulik PK. Mental health research on scheduled tribes in India. Indian J Psychiatry. 2020;62:617.
Sadath A, Uthaman SP, Kumar TS. Mental health in tribes: A case report. Indian J Soc Psychiatry. 2018;34:187.
Mental health of Scheduled Tribe populations in India. 2018. https://www.georgeinstitute.org/mental-health-of-scheduled-tribe-populations-in-india. Accessed 10 Jan 2022.
Kahneman D, Deaton A. High income improves evaluation of life but not emotional well-being. Proc Natl Acad Sci. 2010;107:16489–93.
Chandramouli C, General R. Census of India 2011. Provisional Population Totals: Government of India. New Delhi. 2011. 409–13.
Kamat S. Education and social equity with a special focus on scheduled castes and scheduled tribes in elementary education. 2008.
Kessler RC, Andrews G, Mroczek D, Ustun B, Wittchen H-U. The World Health Organization Composite International Diagnostic Interview short-form (CIDI-SF). Int J Methods Psychiatr Res. 1998;7:171–85.
Muhammad T, Meher T. Association of late-life depression with cognitive impairment: evidence from a cross-sectional study among older adults in India. BMC Geriatr. 2021;21:364.
Trainor K, Mallett J, Rushe T. Age related differences in mental health scale scores and depression diagnosis: Adult responses to the CIDI-SF and MHI-5. J Affect Disord. 2013;151:639–45.
WHO WHO. WHO guidelines on physical activity and sedentary behaviour: at a glance. 2020.
Kham S, Langstieh BT. Depression and Related Factors among the Elderly Chakhesang Population. Indian J Gerontol. 2018;32(1).
Sindhu KV, Chandrashekarappa SM, Thambad M, Boralingiah P, Gopi A, Murthy MN. Anxiety and depression among elderly tribal population of HD Kote, Mysuru. India: Prevalence and factors associated with it; 2022.
Vimala G, Phalke VD. A Cross Sectional Study on Assessment of Health Problems and Psychosocial Problems of Elderly Tribal Population. J Krishna Inst Med Sci (JKIMSU). 2020;9(4).
Pilania M, Bairwa M, Khurana H, Kumar N. Prevalence and predictors of depression in community-dwelling elderly in rural Haryana, India. Indian J Community Med. 2017;42:13.
Goodwin RD. Association between physical activity and mental disorders among adults in the United States. Prev Med. 2003;36:698–703.
Schuch FB, Vancampfort D, Firth J, Rosenbaum S, Ward PB, Silva ES, et al. Physical activity and incident depression: a meta-analysis of prospective cohort studies. Am J Psychiatry. 2018;175:631–48.
A., B, M., J, N. A, H. B, Y. J, M. K J. Tribal Health in India: Bridging the gap and a roadmap for the future. Executive Summary and Recommendations. Ministry of Health and Family Welfare and Ministry of Tribal Affairs, Government of India. 2018. http://tribalhealthreport.in/. Accessed 23 Sep 2022.
Chandel S, Rhetso A, Malik SL, Kulshreshtha M. The association between body physique and physical fitness: a cross-sectional study among a tribal community of Dadra and Nagar Haveli, India. Int J Appl Exerc Physiol. 2018;7:11–20.
Kapoor AK, Dhall M, Tyagi R. Nutritional status and ageing among Car Nicobarese and Nolia males of India. Open Anthropol J. 2010;3(1).
Harford T. Fifty things that made the modern economy. Paris. 2017.
Sutar R, Lahiri A, Diwan S, Satpathy P, Rozatkar A. Determinants of mental health care access in a Tribal District of Central India: findings from a health camp. J Neurosci Rural Pract. 2021;12:335–42.
Hodge DR. Spiritual competence: what it is, why it is necessary, and how to develop it. J Ethn Cult Divers Soc Work. 2018;27:124–39.
Azar D, Ball K, Salmon J, Cleland V. The association between physical activity and depressive symptoms in young women: A review. Ment Health Phys Act. 2008;1:82–8.
Pfeiffer JA, Hart JL, Wood LA, Bhatnagar A, Keith RJ, Yeager RA, et al. The importance of urban planning: Views of greenness and open space is reversely associated with self-reported views and depressive symptoms. Popul Med. 2021;3(1).
Kato T. Effects of flexibility in coping with chronic headaches on depressive symptoms. Int J Behav Med. 2015;22:506–11.
Ribeiro SM, Malmstrom TK, Morley JE, Miller DK. Fruit and vegetable intake, physical activity, and depressive symptoms in the African American Health (AAH) study. J Affect Disord. 2017;220:31–7.
Mulsant BH, Ganguli M, Seaberg EC. The relationship between self-rated health and depressive symptoms in an epidemiological sample of community-dwelling older adults. J Am Geriatr Soc. 1997;45:954–8.
Jahn DR, Cukrowicz KC. Self-rated health as a moderator of the relation between functional impairment and depressive symptoms in older adults. Aging Ment Health. 2012;16:281–7.
Han B. Depressive symptoms and self-rated health in community-dwelling older adults: a longitudinal study. J Am Geriatr Soc. 2002;50:1549–56.
Muhammad T, Maurya P. Social support moderates the association of functional difficulty with major depression among community-dwelling older adults: evidence from LASI, 2017–18. BMC Psychiatry. 2022;22:317.
Srivastava S, Debnath P, Shri N, Muhammad T. The association of widowhood and living alone with depression among older adults in India. Sci Rep. 2021;11:1–13.
Beutel ME, Brähler E, Wiltink J, Kerahrodi JG, Burghardt J, Michal M, et al. New onset of depression in aging women and men: contributions of social, psychological, behavioral, and somatic predictors in the community. Psychol Med. 2019;49:1148–55.
Brinda EM, Rajkumar AP, Attermann J, Gerdtham UG, Enemark U, Jacob KS. Health, social, and economic variables associated with depression among older people in low and middle income countries: world health organization study on global AGEing and adult health. Am J Geriatr Psychiatry. 2016;24:1196–208.
Dsouza RJ, Sunny R, Sambhalwar PB, Hariharan S, Mohanraj S, Menon N. Perception of noncommunicable diseases among the tribals of the Gudalur Valley, Nilgiris, Tamil Nadu. Curr Med Issues. 2021;19:132.
Jiang C, Zhu F, Qin T. Relationships between chronic diseases and depression among middle-aged and elderly people in China: a prospective study from CHARLS. Curr Med Sci. 2020;40:858–70.
Majidi M, Khadembashi N, Etemad K, Jafari M, Khodakarim S. Associated factors with major depression: a path analysis on NHANES 2013–2014 study. Int J Cult Ment Health. 2018;11:763–73.
Schieman S, Plickert G. Functional limitations and changes in levels of depression among older adults: a multiple-hierarchy stratification perspective. J Gerontol B Psychol Sci Soc Sci. 2007;62:S36-42.
Acknowledgements
Not applicable.
Funding
No funding was received for the study.
Author information
Authors and Affiliations
Contributions
Conceived and designed the research paper: RR, SS, TM, MK and RP; analyzed the data: SS and RP; Contributed agents/materials/analysis tools: TM, MK and RP; Wrote the manuscript: RR, SS, TM, MK and RP. All authors read, reviewed and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The survey agencies that conducted the field survey for the data collection have collected prior informed consent (written and verbal) from the respondent. Informed consent was obtained from all subjects and/or their legal guardian(s). The Indian Council of Medical Research (ICMR) extended the necessary guidance and ethical approval for conducting the LASI survey. The study is approved by ethics committee of ICMR. All experimental protocols were approved by Indian Council of Medical Research. All the methods were conducted using relevant guidelines.
Consent for publication
Not applicable.
Competing interests
The authors declare that there is no competing interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Rashmi, R., Srivastava, S., Muhammad, T. et al. Indigenous population and major depressive disorder in later life: a study based on the data from Longitudinal Ageing Study in India. BMC Public Health 22, 2258 (2022). https://doi.org/10.1186/s12889-022-14745-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-022-14745-x