Abstract
Background
The April 2019 wildfires in Gangwon Province, South Korea forced the evacuation of 1500 individuals and cost more than $100 million in damages, making it the worst wildfire disaster in Korean history. The purpose of this paper was to investigate the mental health effects on survivors following the wildfires.
Methods
Between April and May 2019, outreach psychological support services were delivered to people impacted by the wildfires. Post-disaster psychological responses using a checklist and the Clinical Global Impression Scale-Severity (CGI-S) were evaluated for 206 wildfires survivors. The CGI-S was administered consequently at 1, 3, and 6 months after baseline measurement.
Results
Among four response categories, somatic responses (76.2%) were most frequently observed among the wildfire survivors. Specifically, insomnia (59.2%), anxiety (50%), chest tightness (34%), grief (33%), flashbacks (33%), and depression (32.5%) were reported by over 30% of the participants. The mean CGI-S scores were significantly decreased at 1 month (mean score = 1.94; SE = 0.09) compared to baseline (mean score = 2.94; SE = 0.08) and remained at the decreased level until 6 months (mean score = 1.66; SE = 0.11). However, participants with flashbacks showed significantly higher CGI-S scores compared to those without flashback at 6 months.
Conclusions
Wildfire survivors have various post-disaster responses, especially somatic responses. While most participants’ mental health improved over time, a few of them may have experienced prolonged psychological distress after 6 months. Flashbacks were particularly associated with continuing distress. These results suggest that the characteristics of responses should be considered in early phase intervention and in follow-up plans for disaster survivors.
Similar content being viewed by others
Introduction
Major disasters, including floods, wildfires, earthquakes, and tsunamis increase the risk of physical injury or illness and cause various long- and short-term mental health issues for survivors [1,2,3]. Disaster-related factors can influence the psychiatric impact of the disaster, including disaster type [1]; intensity and duration of exposure [4]; and degree of disaster exposure (e.g., damage to one’s property, moving due to damage to one’s residence, personal or familial injury) [1, 5]. Moreover, victims of man-made disasters (e.g., wars, terrorism, accidents, hazardous materials exposure, explosions, or groundwater contamination) frequently experience anger, a state of suspiciousness, guilt, and self-blame [6, 7]. However, natural disasters (e.g., earthquakes, floods, hurricanes, drought, volcanoes, tornadoes, or tsunamis) mainly cause loss of property and a lack of control over one’s possessions [8,9,10]. Wildfires can possess the characteristics of both types of disasters depending on their cause. Specifically, if wildfires originate from natural causes, such as lightning or climate change, then they are considered as natural disasters. On the other hand, if wildfires are caused by human hazards or have an element of human intent, such as campfires being left burning, then they are considered man-made disasters. Wildfires in this study were characterized as both natural and man-made disasters because they were caused by strong winds (climatic conditions) and sparks (element of human intent) [11].
Wildfires can harm people’s mental health. Specifically, wildfire survivors commonly exhibit various physical, psychological, and cognitive reactions including nightmares, insomnia, anxiety about the recurrence of wildfires, helplessness, and re-experience or flashbacks due to overwhelming trauma experiences, such as witnessing the fire [12,13,14]. Studies investigating the psychiatric disorders of wildfire survivors indicate that they exhibit an increased rate of post-traumatic stress disorder (PTSD) [15, 16]. They also experience increased depression and anxiety symptoms [12, 13]; psychological distress levels [17]; and intake of alcohol, drugs, and hypnotics [18]. Moreover, significant predictors of wildfire-related psychological problems in wildfire survivors were fear for their own or their loved one’s lives, bereavement of someone lost to fire, property loss, witnessing homes being destroyed, pre-existing mental illness, low community cohesion, and recent life stressors [15, 19,20,21]. In some cases, wildfire-related mental health problems can persist for a long time. For example, a study on the survivors of the Ash Wednesday bushfires in Australia reported that 42 and 23% of participants met the diagnostic criteria for PTSD or depression at 1 year and at 20 months following the wildfire, respectively [22]. Additionally, residents in highly affected regions of the Black Saturday bushfires in Australia still suffered from PTSD (15.6%), depression (12.9%), severe distress (12.8%), and heavy alcohol use (24.7%) three to 4 years later [23]. Another longitudinal study conducted 5 years after the Australia bushfires showed that the rate of probable PTSD (14.7%) remained high compared to national levels (4.4%); furthermore, the rate of psychological distress including probable PTSD and depression fluctuated over time [12].
Wildfires tend to occur frequently in Korea. In the past 10 years, an average of 431 wildfires have occurred per year. Additionally, 1.2 large-scale wildfires, defined as “forest damage with an area of more than 1 km2 or lasting more than 24 hours,” have occurred annually [11]. More recently, on April 4, 2019, the east coast sea wildfires (the Gangwon wildfires) burned 17.57 km2 of land and destroyed more than 2800 buildings, forcing 1524 residents to evacuate. The estimated damage was $107.2 million, making it the worst wildfire catastrophe in Korean history [11]. On April 6, the Korean Government issued a “Declaration of a Special Disaster Zone,” requiring government intervention and support. After the evacuation, many people faced displacement or unemployment because their homes or local businesses were destroyed by the fire [11]. Importantly, although there is a large international corpus of literature on the association between wildfire experiences and mental health status, no study has systematically examined the mental health effects of wildfires in Korea. Additionally, data on Asian samples are lacking. For example, the abovementioned studies constitute representative research investigating the effects of wildfires on mental health; however, they were conducted in Australia, Greece, Canada, and the United States, with primarily Caucasian samples [12,13,14,15,16,17,18,19,20,21]. Furthermore, data on immediate psychological responses to disasters, especially those obtained from clinicians, and empirical data from community samples who received psychological support, are lacking. It is crucial to assess the effectiveness of the psychological support services provided by the central and local government. This can help provide directions for how the services should be developed and structured in the future. Therefore, we investigated the mental health impacts and recovery process of survivors of the Gangwon wildfires over 6 months. We hypothesized that wildfire survivors would experience various post-disaster responses in the phase immediately after the disaster; however, most participants’ mental health would gradually improve.
Materials and methods
Participants and procedures
Data were obtained from the outreach psychological support program for survivors delivered by the “Integrated Mental Health Service Team for Wildfires.” The National Center for Disaster Trauma (NCT), a Korean government institution for disaster mental health management, served as the overall supervisory body. The outreach team comprised many psychiatrists and certified mental health professionals, who visited the shelters and homes for survivors to provide counseling and education on relaxation techniques and stress management. They also conducted individual psychiatric interviews.
All survivors who received psychological support services were invited to participate in this study at the beginning of the program. A total of 315 people (age ≥ 19 years) completed the initial assessment (baseline) between April and May 2019. Following the initial assessment, 206 adults agreed to be contacted for follow-up counseling via telephone. We thusly administered the Clinical Global Impression Scale-Severity (CGI-S) at 1, 3, and 6 months after the baseline assessment. Ultimately, we analyzed the data of 206 wildfire survivors who completed follow-up evaluation to assess the impact on their mental health following the wildfires.
Measures
Post-disaster psychological responses-checklist
To evaluate psychological responses to the wildfires, we administered the “Post-disaster Psychological Responses-Checklist.” This was partially modified by several specialists for use in disaster mental health based on the “various responses that may occur after a disaster” (quoted in the Committee for Disaster Behavioral Health, 2015) [24, 25].
This checklist categorizes post-disaster psychological responses into four categories: emotional, somatic, cognitive, and behavioral.
Responses for each category are as follows:
-
Emotional: anxiety, grief, depression, fear, helplessness, hopelessness, anger, guilt, miserableness, shame.
-
Somatic: insomnia, chest tightness, fatigue, changes in appetite, pain, indigestion, tension, nausea, hyperpnea.
-
Cognitive: flashbacks, difficulty concentrating, memory decline, nightmares, poor judgment, suicidal ideation, difficulty accepting the death of a loved one.
-
Behavioral: extreme confusion, caution/suspicion, isolation, alcohol abuse, avoidance/denial, violence/impulsiveness, excessive smoking, drug misuse, self-harm.
Outreach team professionals conducted face-to-face interviews with participants and asked them to provide simple yes/no answers to each post-disaster psychological response item.
Clinical global impression scale-severity (CGI-s)
Participants’ overall mental health severity was assessed using the CGI-S developed by Guy [26]. This is a single-item scale to evaluate the severity of symptoms interfering with overall daily life function and requiring inpatient care [27]. The CGI-S rating is based on the overall impact of the symptoms, behaviors, and functions observed by clinicians over the previous 7 days.
The clinical symptom severity of participants was rated on the following 7-point scale: 1 = normal, no illness; 2 = borderline ill; 3 = mildly ill; 4 = moderately ill; 5 = markedly ill; 6 = severely ill; 7 = most extremely ill.
Statistical analysis
We conducted a frequency analysis for the psychological responses. Specifically, we conducted linear mixed models (LMM) with repeated measures to examine changes in the CGI-S scores at baseline and at 1, 3, and 6 months. LMM is a model that addresses the limitations of traditional repeated ANOVA measures, including missing data on the response variable. If one measurement is missing, then the entire case is discarded. Thus, LMM was conducted to compensate for missing values, which occurred in cases where symptoms improved and ended, one-sided contact loss occurred, or participants refused further monitoring at the follow-up observation. The LMM performed in this study was a single model in which the participant (id) and time were included as random effects and fixed effects, respectively. Subsequently, we performed post-hoc multiple comparisons with Bonferroni correction to compare the CGI-S scores between measurement times controlling the type I error rate. For responses reported by more than 30% of participants, the mean CGI-S score was compared between groups with and without each response using independent t-tests.
All data were analyzed using IBM SPSS Statics 21.0 (Chicago, IL, USA).
Results
Demographic characteristics
Participants’ average age was 68.72 years (SD = 12.74), and most of the sample comprised adults aged over 65 years (n = 129, 62.6%). More than two-thirds of the sample were women (n = 155, 75.2%).
Psychological responses after wildfire
We observed somatic and emotional responses in 76.2 and 71.8% of participants (n = 206), respectively. This was followed by cognitive and behavioral responses in 50.0 and 16.5% of participants, respectively (Table 1). Specifically, insomnia (59.2%) and anxiety (50%) responses were reported by more than 50% of the sample. Chest tightness (34%), grief (33%), flashbacks (33%), and depression (32.5%) were also observed in more than 30% of participants (Table 1).
Difference in the severity of mental health according to psychological responses
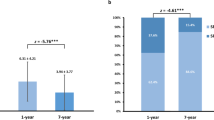
The mean CGI-S score was 2.94 at baseline (SE = 0.08). This decreased to 1.94 (SE = 0.09) at 1 month, 1.62 (SE = 0.10) at 3 months, and 1.66 (SE = 0.11) at 6 months (F = 74.458, p < .001). Table 2 presents the relations between measurement times and the CGI-S. Post-hoc multiple comparisons with Bonferroni correction for CGI-S score differences showed that CGI-S scores were significantly lower at 1, 3, and 6 months compared to baseline (p < .001, respectively), and at 3 months compared to 1 month (p < .05). However, there were no statistically significant differences between 3 and 6 months. The changes in CGI-S over time are presented in Fig. 1.
As shown in Fig. 2, the CGI-S score at baseline was higher in each group with responses compared to those without responses: insomnia (t(172) = 5.303, p < .001), anxiety (t(171) = 3.438, p < .01), chest tightness (t(171) = 3.943, p < .001), flashbacks (t(170) = 3.997, p < .001), and depression (t(171) = 4.388, p < .001).
Moreover, the mean CGI-S score at 1 month was higher in the group with depression than in the group without depression. The mean CGI-S score at 6 months was higher in the group with flashbacks compared to the group without flashbacks {t(123) = 2.767, p < .01, t(79) = 2.126, p < .05, respectively}.
Discussion
This study investigated the mental health effects of a wildfire on affected residents in South Korea. Over 70% of the study population reported at least one of the somatic, emotional, cognitive, and behavioral stress responses immediately after the disaster experience. Most participants in our study were primary survivors who were directly exposed to traumatic stressors, such as witnessing the fire or incurring property damage. Such exposure levels are related to a high rate of psychological discomfort, which is consistent with previous studies demonstrating that mental health effects are associated with directly witnessing a fire or having one’s home destroyed [28,29,30,31].
Regarding the changes in CGI-S scores over time, the mean score decreased within 1 month after the disaster, which was maintained at 6 months. Our observation is notable in the context of previous studies. Specifically, regarding the Australian Ash Wednesday, Australian Black Saturday, and the Blue Mountain bushfires, most of the affected people eventually coped with the adversity; moreover, few people experienced probable PTSD, depression, or psychological distress [20, 22, 32,33,34,35,36,37,38]. However, it is unknown whether the improved CGI-S scores in the current study occurred naturally or due to the psychological support provided, since data were obtained from the group who received psychological support. Additionally, the follow-up period was only 6 months.
Among the four categories of responses, somatic responses were most frequently observed in the wildfire victims. This is in line with the finding showing that somatization is frequent in wildfire victims [13]. Acute traumatic stress is known to activate the sympathetic nervous system and evoke a neuroendocrine stress response, which are subsequently associated with post-traumatic somatic symptoms [39,40,41]. We considered that the socio-demographic characteristics of our participants, such as having a high proportion of older adults and women, may have partially influenced the results. Older adults and women are not only regarded as vulnerable populations regarding their psychological responses following disasters [42, 43], but also tend to complain of somatic symptoms more frequently [42, 44]. Depression, anxiety, and stress reactions are often expressed as somatic symptoms, especially in older adults [45]. In addition, the tendency to emphasize somatic symptoms when suffering psychological distress has been frequently reported in samples from East Asian cultural contexts, including Korea and China [46].
Furthermore, many participants reported experiencing vivid flashback responses in the current study. For example, they said, “The embers still fly around before my eyes” or “The embers are chasing me.” Notably, regarding flashback responses, the mean CGI-S score at 6 months after the wildfire was higher in the group which experienced flashbacks relative to the group which did not experience flashbacks. A previous longitudinal study investigating the alterations in the network structure of PTSD symptoms found that the re-experience cluster including flashbacks and distressing reminders played crucial roles until 6 months. Thus, re-experience symptoms may play a key role in the evolution and persistence of PTSD [47]. These results were consistent with other studies indicating that early re-experience symptoms predict the development of PTSD [48, 49].
In our study, 33.0% of participants reported grief responses. The wildfires destroyed their houses and households, and the survivors grieved the loss of their meaningful possessions. This suggests that survivors could experience a serious mourning reaction, not only to loss of life, but also to property. Notably, anger was reported at a low level (14.1%) compared to studies in which anger was a frequent and important mediator of psychopathology in man-made disasters [50,51,52,53]. Even though wildfires are considered as man-made disasters under Korean law, a survivor’s response might vary depending on the cause of the wildfire. In the 2019 Gangwon wildfires, an electrical short was identified as the origin, and the rapid spread was attributed to climatic and topographical characteristics [11]. Compared to previous wildfires which were mainly man-made, it was difficult to place blame for this wildfire as it was heavily influenced by natural factors.
Our findings highlight the necessity of long-term policies and intervention programs to care for individuals who are affected by disasters and experience mental health problems, as well as the need for a community-expanded approach. Consistent with this, the “Integrated mental health service team” have provided ongoing mental health programs for survivors. This includes education for community residents, long-term follow-up counseling and a psychiatric institution referral if needed, and group therapy based on stabilization and cognitive-behavioral techniques. Considering our findings regarding somatic responses and flashbacks, we suggest that body-based stabilization techniques may be more effective than cognitive approaches. Further studies are necessary to compare the effectiveness of body-based stabilization versus cognitive intervention and/or investigate the long-term effect of community-based mental health interventions on the mental health impacts of the wildfires.
Limitations
This study had several limitations. First, variables such as demographic data, factors related to disaster experience, pre-trauma history of mental disorders, and having a social support system could not be sufficiently evaluated. Additionally, the CGI-S was the only objective measurement used in this study due to constraints in the research conditions. The primary purpose of the mental health support team was not to conduct rigorous research, but to provide optimal mental health service. Therefore, it was difficult to thoroughly design the study or gather extensive data. Previous findings indicate that a pre-disaster history of mental disorders, greater incident exposure to disaster, lack of social support, or experiencing an extra socioeconomic stressor are significant predictors for developing psychological distress after disasters [54,55,56,57,58]. Considering this, shortage of such data could be a major limitation of our study. However, despite these limitations in data collection, the CGI-S scales constitute an easily understood and practical measurement tool that can be readily managed by a clinician in a practice setting [27]. Second, clinical measures were based on a simple confirmation (yes or no) of each response. Because the survey methodology did not use structured clinical interviews, no formal diagnosis was possible, and our analysis is based solely on the manifestation of each response. Third, the participants in this study were not fully representative of all Gangwon wildfire survivors because only people who received mental health services were invited to participate in this study. People who are more severely affected by a disaster are more likely to seek counseling, which might contribute to an elevated measure of post-disaster psychological distress. Therefore, caution is needed when generalizing these findings. In addition, the average age of the sample was 68.72 years, which also limits the generalization of interpretation. The proportion of older adults aged 65 years and over in Gangwon Province is 19.1%, which is 14.9% higher than the rest of the nation [59]; thus, this limitation was difficult to avoid. Finally, our study lacked a control population, which is significant to determine the comparative effect of the disaster on the affected population.
Despite these limitations, our study is the first to investigate the mental health impacts of wildfires in Korean history. Knowledge from this study could inform policymakers when planning supportive programs to alleviate the mental health impacts of natural disasters.
Conclusion
The present findings highlight several significant outcomes. First, even though many participants experienced significant psychological distress immediately after the disaster, most seemed to recover over time. Second, despite the general trend of resilience, a significant proportion of participants presented with prolonged psychological distress. Specifically, flashback responses could be a predictor of long-term psychopathology. Finally, an adequate public mental health service system is needed for survivors affected by disasters. Consequently, this study will help build more empirically informed evidence regarding how survivors’ mental health is influenced by disasters and elucidate the necessity of mental health support and programs for disaster survivors.
Availability of data and materials
The datasets generated and/or analyzed during the current study are not publicly available due to confidentiality; however, data is accessible from the corresponding author on reasonable request.
Abbreviations
- PTSD:
-
Post-traumatic stress disorder
- NCT:
-
National Centre for Disaster Trauma
- CGI-S:
-
Clinical Global Impression Scale-Severity
- LMM:
-
Linear mixed models
References
Goldmann E, Galea S. Mental health consequences of disasters. Annu Rev Public Health. 2014;35:169–83.
Kar N. Psychological impact of disasters on children: review of assessment and interventions. World J Pediatr. 2009;5(1):5–11.
Norris FH, Friedman MJ, Watson PJ. 60,000 disaster victims speak: part II. Summary and implications of the disaster mental health research. Psychiatry. 2002;65(3):240–60.
Wagner SL, White N, Randall C, Regehr C, White M, Alden LE, et al. Mental disorders in firefighters following large-scale disaster. Disaster Med Public Health Preparedness. 2021;15(4):504–17.
Amstadter AB, Acierno R, Richardson LK, Kilpatrick DG, Gros DF, Gaboury MT, et al. Posttyphoon prevalence of posttraumatic stress disorder, major depressive disorder, panic disorder, and generalized anxiety disorder in a Vietnamese sample. J Traumatic Stress. 2009;22(3):180–8.
Kar N. Indian research on disaster and mental health. Indian J Psychiatry. 2010;52(Suppl 1):S286–90.
Murthy RS. Mental health of survivors of 1984 Bhopal disaster: a continuing challenge. Ind Psychiatry J. 2014;23(2):86–93.
Bonanno GA, Brewin CR, Kaniasty K, Greca AM. Weighing the costs of disaster: consequences, risks, and resilience in individuals, families, and communities. Psychol Sci Public Interest. 2010;11(1):1–49.
Hackbarth M, Pavkov T, Wetchler J, Flannery M. Natural disasters: an assessment of family resiliency following hurricane Katrina. J Marital Fam Ther. 2012;38(2):340–51.
Freedy JR, Shaw DL, Jarrell MP, Masters CR. Towards an understanding of the psychological impact of natural disasters: An application of the conservation resources stress model. J Traumatic Stress. 1992;5(3):441–454.
Safety MotIa: The east coast sea wildfires in Gangwon-do White paper. In. Edited by Safety MotIa; 2019.
Bryant RA, Gibbs L, Gallagher HC, Pattison P, Lusher D, MacDougall C, et al. Longitudinal study of changing psychological outcomes following the Victorian black Saturday bushfires. Australian New Zealand J Psychiatry. 2018;52(6):542–51.
Papanikolaou V, Adamis D, Mellon RC, Prodromitis G. Psychological distress following wildfires disaster in a rural part of Greece: a case-control population-based study. Int J Emerg Mental Health. 2011;13(1):11–26.
Psarros C, Theleritis C, Economou M, Tzavara C, Kioulos KT, Mantonakis L, et al. Insomnia and PTSD one month after wildfires: evidence for an independent role of the "fear of imminent death". Int J Psychiatry Clin Pract. 2017;21(2):137–41.
Brown MRG, Agyapong V, Greenshaw AJ, Cribben I, Brett-MacLean P, Drolet J, et al. Significant PTSD and other mental health effects present 18 months after the fort Mcmurray wildfire: findings from 3,070 grades 7-12 students. Front Psychiatry. 2019;10:623.
Jones RT, Ribbe DP, Cunningham PB, Weddle JD, Langley AK. Psychological impact of fire disaster on children and their parents. Behav Modif. 2002;26(2):163–86.
Afifi WA, Felix ED, Afifi TD. The impact of uncertainty and communal coping on mental health following natural disasters. Anxiety Stress Coping. 2012;25(3):329–47.
Caamano-Isorna F, Figueiras A, Sastre I, Montes-Martínez A, Taracido M, Piñeiro-Lamas M. Respiratory and mental health effects of wildfires: an ecological study in Galician municipalities (north-West Spain). Environment Health. 2011;10:48.
Agyapong VIO, Hrabok M, Juhas M, Omeje J, Denga E, Nwaka B, et al. Prevalence rates and predictors of generalized anxiety disorder symptoms in residents of Fort McMurray six months after a wildfire. Front Psychiatry. 2018;9:345.
Forbes D, Alkemade N, Waters E, Gibbs L, Gallagher C, Pattison P, et al. The role of anger and ongoing stressors in mental health following a natural disaster. Australian New Zealand J Psychiatr. 2015;49(8):706–13.
Moosavi S, Nwaka B, Akinjise I, Corbett SE, Chue P, Greenshaw AJ, et al. Mental health effects in primary care patients 18 months after a major wildfire in Fort McMurray: risk increased by social demographic issues, clinical antecedents, and degree of fire exposure. Front Psychiatr. 2019;10:683.
McFarlane AC, Clayer JR, Bookless CL. Psychiatric morbidity following a natural disaster: an Australian bushfire. Soc Psychiatry Psychiatr Epidemiol. 1997;32(5):261–8.
Bryant RA, Waters E, Gibbs L, Gallagher HC, Pattison P, Lusher D, et al. Psychological outcomes following the Victorian black Saturday bushfires. Australian New Zealand J Psychiatr. 2014;48(7):634–43.
CfDM H. Disaster and mental health. Seoul: Hakjisa; 2015.
Young BH, Ford JD, Ruzek JI, Friedman MJ, Gusman FD. Disaster mental health services: a guidebook for clinicians and administrators. National Center for Post-Traumatic Stress Disorder; 1998.
Guy W, ECDEU assessment manual for PR, Rockville M. US Department of Health, education, and welfare, public health service, alcohol, drug abuse, and mental health administration, NIMH Psychopharmacology Research Branch, Division of Extramural Research Programs. 1976.
Busner J, Targum SD. The clinical global impressions scale: applying a research tool in clinical practice. Psychiatr. 2007;4(7):28–37.
Carr VJ, Lewin TJ, Kenardy JA, Webster RA, Hazell PL, Carter GL, et al. Psychosocial sequelae of the 1989 Newcastle earthquake: III. Role of vulnerability factors in post-disaster morbidity. Psychol Med. 1997;27(1):179–90.
Carr VJ, Lewin TJ, Webster RA, Hazell PL, Kenardy JA, Carter GL. Psychosocial sequelae of the 1989 Newcastle earthquake: I. community disaster experiences and psychological morbidity 6 months post-disaster. Psychol Med. 1995;25(3):539–55.
Heinrichs M, Wagner D, Schoch W, Soravia LM, Hellhammer DH, Ehlert U. Predicting posttraumatic stress symptoms from pretraumatic risk factors: a 2-year prospective follow-up study in firefighters. Am J Psychiatry. 2005;162(12):2276–86.
North CS, Pfefferbaum B, Kawasaki A, Lee S, Spitznagel EL. Psychosocial adjustment of directly exposed survivors 7 years after the Oklahoma City bombing. Compr Psychiatry. 2011;52(1):1–8.
Bonanno GA, Diminich ED. Annual Research Review: Positive adjustment to adversity--trajectories of minimal-impact resilience and emergent resilience. J Child Psychol Psychiatr. 2013;54(4):378–401.
Galea S, Vlahov D, Resnick H, Ahern J, Susser E, Gold J, et al. Trends of probable post-traumatic stress disorder in New York City after the September 11 terrorist attacks. Am J Epidemiol. 2003;158(6):514–24.
McFarlane AC, Van Hooff M. Impact of childhood exposure to a natural disaster on adult mental health: 20-year longitudinal follow-up study. Brit J Psychiatr. 2009;195(2):142–8.
Norris FH, Tracy M, Galea S. Looking for resilience: understanding the longitudinal trajectories of responses to stress. Soc Sci Med. 2009;68(12):2190–8.
Parslow RA, Jorm AF, Christensen H. Associations of pre-trauma attributes and trauma exposure with screening positive for PTSD: analysis of a community-based study of 2,085 young adults. Psychol Med. 2006;36(3):387–95.
Pietrzak RH, Feder A, Singh R, Schechter CB, Bromet EJ, Katz CL, et al. Trajectories of PTSD risk and resilience in world trade center responders: an 8-year prospective cohort study. Psychol Med. 2014;44(1):205–19.
van Griensven F, Chakkraband ML, Thienkrua W, Pengjuntr W, Lopes Cardozo B, Tantipiwatanaskul P, et al. Mental health problems among adults in tsunami-affected areas in southern Thailand. JAMA. 2006;296(5):537–48.
Ford C. Somatic symptoms, somatization, and traumatic stress: An overview. Nordic J Psychiatr. 1997;51(1):5–13.
Morris MC, Rao U. Psychobiology of PTSD in the acute aftermath of trauma: integrating research on coping, HPA function and sympathetic nervous system activity. Asian J Psychiatr. 2013;6(1):3–21.
Pace TW, Heim CM. A short review on the psychoneuroimmunology of posttraumatic stress disorder: from risk factors to medical comorbidities. Brain Behav Immun. 2011;25(1):6–13.
Ursano RJ, Fullerton CS, Weisaeth L, Raphael BJ. Individual and community responses to disasters. Todp. 2007:3–26.
Goldmann E, Galea S. Mental health consequences of disasters. Ann Review Public Health. 2014;35:169–83.
Bromet EJ, Gluzman S, Schwartz JE, Goldgaber D. Somatic symptoms in women 11 years after the Chornobyl accident: prevalence and risk factors. Environ Health Perspect. 2002;110(Suppl 4):625–9.
Vasilopoulos A, Marinou S, Rammou M, Sotiropoulou P, Roupa Z, Siamaga E. A research on anxiety and depression of the elderly in the community. Hellenic J Nurs Sci. 2018; 11(3):59–66.
Zhou X, Min S, Sun J, Kim SJ, Ahn JS, Peng Y, et al. Extending a structural model of somatization to south Koreans: cultural values, somatization tendency, and the presentation of depressive symptoms. J Affect Disord. 2015;176:151–4.
Ge F, Yuan M, Li Y, Zhang J, Zhang W. Changes in the network structure of posttraumatic stress disorder symptoms at different time points among youth survivors: a network analysis. J Affect Disord. 2019;259:288–95.
Kleim B, Ehlers A, Glucksman E. Early predictors of chronic post-traumatic stress disorder in assault survivors. Psychol Med. 2007;37(10):1457–67.
Michael T, Ehlers A, Halligan SL, Clark DM. Unwanted memories of assault: what intrusion characteristics are associated with PTSD? Behav Res Ther. 2005;43(5):613–28.
Yoo S, Sim M, Choi J, Jeon K, Shin J, Chung S, et al. Psychological responses among humidifier disinfectant disaster victims and their families. J Korean Med Sci. 2019;34(4):e29.
Tran BN, Tanase MA, Bennett LT, Aponte C. High-severity wildfires in temperate Australian forests have increased in extent and aggregation in recent decades. PLoS One. 2020;15(11):e0242484.
Ishikawa S, Motoya R, Sasagawa S, Takahashi T, Okajima I, Takeishi Y, et al. Mental health problems among undergraduates in Fukushima, Tokyo, and Kyoto after the march 11 Tohoku earthquake. Tohoku J Exp Med. 2015;236(2):115–22.
Kabir H, Maple M, Islam MS, Usher K. The Current Health and Wellbeing of the Survivors of the Rana Plaza Building Collapse in Bangladesh: A Qualitative Study. Int J Environ Res Public Health. 2019;16(13):2342.
Jacobson MH, Norman C, Nguyen A, Brackbill RM. Longitudinal determinants of depression among world trade center health registry enrollees, 14-15 years after the 9/11 attacks. J Affect Disord. 2018;229:483–90.
Lebowitz AJ. Relational satisfaction from providing and receiving support is associated with reduced post-disaster depression: data from within one year of the 2011 Japan triple disaster. Community Ment Health J. 2017;53(2):202–14.
Mason S, Wardrope J, Turpin G, Rowlands A. The psychological burden of injury: an 18 month prospective cohort study. Emerg Med J. 2002;19(5):400–4.
Sareen J. Posttraumatic stress disorder in adults: impact, comorbidity, risk factors, and treatment. Can J Psychiatry. 2014;59(9):460–7.
Tang B, Liu X, Liu Y, Xue C, Zhang L. A meta-analysis of risk factors for depression in adults and children after natural disasters. BMC Public Health. 2014;14:623.
Erderly population ration of Korea. https://kosis.kr/statHtml/statHtml.do?orgId=101&tblId=DT_1YL20631&vw_cd=MT_GTITLE01&list_id=101&scrId=&seqNo=&lang_mode=ko&obj_var_id=&itm_id=&conn_path=K1&path=%25EC%25A3%25BC%25EC%25A0%259C%25EB%25B3%2584%2520%253E%2520%25EC%259D%25B8%25EA%25B5%25AC%25EA%25B3%25A0%25EB%25A0%25B9%25EC%259D%25B8%25EA%25B5%25AC%25EB%25B9%2584%25EC%259C%25A8%28%25EC%258B%259C%25EB%258F%2584%252F%25EC%258B%259C%252F%25EA%25B5%25B0%252F%25EA%25B5%25AC%29. Accessed 10 June 2022.
Acknowledgements
We gratefully acknowledge the support provided by the National Center for Disaster and Trauma for this study. We would like to thank the members of the Integrated Psychological Support Group for Gangwon wildfires, Republic of Korea.
Funding
This study was supported by a clinical research grant (No. 2021–04) from the National Center for Mental Health, Republic of Korea.
Author information
Authors and Affiliations
Contributions
JH, MS, and JL devised the project, the main conceptual ideas, and proof outline. SH collected and analyzed the data. MS, JL, and SH contributed to the interpretation of the results. JH and SH took the lead in writing the manuscript. All authors provided critical feedback and helped shape the research, analysis, and manuscript. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All methods were carried out in accordance with relevant guidelines and regulations (declaration of Helsinki). Written informed consent for participation was waived by the Institutional Review Board (IRB) of the National Center for Mental Health, as it was not required for this study in accordance with the national legislation and the institutional requirements. This study was conducted with the approval of the IRB of the National Center for Mental Health (IRB approval NO. 116271–2020-16).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Hong, J.S., Hyun, S.Y., Lee, J.H. et al. Mental health effects of the Gangwon wildfires. BMC Public Health 22, 1183 (2022). https://doi.org/10.1186/s12889-022-13560-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-022-13560-8