Abstract
Background
During the first wave of COVID-19 there was little evidence to guide appropriate child and family programs and policy supports.
Methods
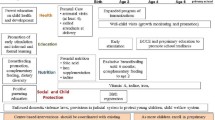
We compared policies and programs implemented to support early child health and well-being during the first wave of COVID-19 in Australia, Canada, the Netherlands, Singapore, the UK, and the USA. Program and policy themes were focused on prenatal care, well-baby visits and immunization schedules, financial supports, domestic violence and housing, childcare supports, child protective services, and food security.
Results
Significant heterogeneity in implementation of OECD-recommended policy responses was found with all of the included countries implementing some of these policies, but no country implementing supports in all of the potential areas.
Conclusions
This analysis gives insight into initial government reactions to support children and families, and opportunities for governments to implement further supportive programs and policies during the current pandemic and future emergencies.
Similar content being viewed by others
Background
Healthy growth and development, from the prenatal environment to the first 5 years of life, plays a major role in health and well-being across the life course [1]. Social and environmental factors, such as family structure, socioeconomic status, housing, and nutrition, during early childhood influences the probability of future obesity, heart disease, mental health, educational outcomes and involvement in the criminal justice system [2]. In particular, adverse childhood experiences (ACEs), such as domestic violence, being the child of a parent with a mental health condition, or experiencing abuse or neglect, are associated with long-term stress-related changes in the nervous, endocrine and immune systems, leading to multiple poor health conditions such as type 2 diabetes, mental disorders, and cognitive decline [3].
Policies and programs that promote positive social and physically active environments for young children and their families have the potential to improve early childhood development, and subsequently health for entire populations. For example, across several countries from a range of political legacies, those that provided mothers with longer maternity leaves and higher maternity pays had higher rates of breastfeeding initiation, which promotes sensory and cognitive development, and is associated with improved infant health and behavioural outcomes [4]. Similarly, countries that publicly funded early childhood education had higher literacy rates at 15 years of age than those that were privately funded [5]. Early childhood education can also positively impact motor development, cognitive function, emotional wellbeing, and social relationships through play [6]. Early childhood food supplementation programs have been found to improve childhood nutrition and psychosocial development, particularly if those programs are delivered through childcare centres [7]. Parental income supports, including child tax credits, have also been found to prevent and mitigate the effects of ACEs and improve long-term health outcomes and educational attainment [8, 9]. Furthermore, programs that target specific populations can decrease social inequity within countries (e.g., evidence-based home visiting programs for vulnerable first-time mothers such as nurse-family partnership) [10, 11]. Thus, governmental policies and programs are able to impact early childhood health and development.
The World Health Organization declared COVID-19 a pandemic on March 11, 2020. In response to rising cases and deaths, numerous countries globally implemented community-wide public health measures such as quarantine, isolation, and closure of community services, workplaces and businesses. These very significant societal changes have had consequences on child health, parent health and family functioning [12, 13]. Quarantine and isolation indoors and loss of work can lead to significant parental stress through social isolation and loss of income. This in turn can impact children through poverty, abuse or neglect, decreased time outdoors to play, engage in physical activity and socialize, and potentially increase sedentary behaviours and screen time. Childcare and schools often serve as settings that can mitigate challenges in the home setting, such as by providing food to low-income children at risk of food insecurity, other health services (eg. vaccinations, mental health services), and holistic healthy physical and cognitive growth and development programming. In addition, COVID-19 has drastically changed how public health services, prenatal, neonatal and pediatric care are delivered. As such, many of the programs created to support early childhood development have been more difficult to access or implement during a global pandemic. Several papers have considered how health and social services can be delivered safely during the pandemic without diminishing access, quality and effectiveness of care [14,15,16,17]. Publications have highlighted gaps that already existed in supporting families in some countries [12, 18], and how the pandemic may widen inequities in prenatal and obstetric care [19]. Recommendations have been made to implement policies that can mitigate the impact of COVID-19 on children, such as reducing barriers to accessing social support, providing support for women at risk of domestic violence, and increased support for education for children that lack technology resources [20]. The first wave of the pandemic was an acute emergency and marked by incredible uncertainty for all of society. Understanding how countries responded to the needs of their families in this context may help to inform future emergency preparedness.
The objective of this paper is to compare the policies and programs that different countries put into place to support child health during the first wave of the COVID-19 pandemic. We aim to contribute to the exploration of the acute impacts of the COVID-19 pandemic on policies and programs to support early childhood development, and identify opportunities for improvement. In addition, we explore the reasons and potential impact of varying approaches on early child health and well-being with a view to improvements in emergency preparedness and response.
Methods
To answer the question, “How did governments support child health during the COVID-19 pandemic through policies and programs?,” we compared the policies and programs implemented by governments in selected countries during their first wave of COVID-19.
Country and government selection
The following countries were included in this study: Canada (the federal government of Canada and selected provinces of British Columbia, Alberta, Ontario and Quebec), United Kingdom (UK), Australia, Netherlands, United States of America (USA), and Singapore. In some instances, sub-national territories were included as federal responsibility for some health and social programs may be shared or devolved. Country selection was discussed and finalized amongst all authors. The focus was on the Canadian experience, with information being gathered about both federal and provincial policy interventions. The included provinces were chosen due to their comprising the majority of the Canadian population (> 85%), as well as being most affected by COVID-19 during the first wave. We then selected Organization of Economic Cooperation and Development (OECD) comparator countries, as well as Singapore, representing a variety of political legacies and COVID-19 epidemiologic experiences [21]. In the UK, Australia, Netherlands and Singapore, only federal policies were included due to the structure of their government. Within the USA, in addition to federal policies being explored, Michigan was also chosen for further comparison due to its similarities to Ontario, for which it has previously been used as a comparator to Ontario [22].
Baseline country characteristics and COVID-19 epidemiology
Baseline information about each country was gathered in order to provide insight into the context in which decisions around policies and programs to support families are being made, including prior indicators of early childhood supports, and inform comparison between settings. These measures included population size, Gross Domestic Product (GDP) per capita, percentage (%) of GDP spent on early childhood education (ECE), enrollment of children 3–5 years in ECE, immunization coverage, and Gini coefficient. The Gini coefficient is a measure of income inequality within a group of people, on a range from 0 to 1, with higher numbers indicating greater inequality [23]. The main sources of data were the World Bank [24] and OECD [25,26,27], though in some cases, country specific reports were used due to lack of synthesized international data.
We also compared the countries’ experiences of the COVID-19 pandemic during their first wave by collecting data on date of first case, date of the first peak in cases, the incidence during the peak, their testing capacity during the first wave, and the Government Stringency Index (GSI) during their peak, which is a measure of the intensity of a country’s community-wide public health measures. This information was found through Our World in Data [28,29,30].
Search strategy and data sources
The search strategy was designed to identify policies, programs, announcements, and guidelines released from governmental and public health organizations within each country related to children, parents, families, early childhood development, adverse childhood experiences, child welfare, pre-school, childcare or daycares. Specifically, we were interested in clinical guidelines, financial benefits or government funding of health or social programs, and childcare supports. For the purposes of this paper, a policy is any long-term change in law or regulation, while a program is a shorter-term or temporary activity that includes an active intervention. Public health organizations were included as they are often considered a branch of government, or were heavily involved in advising the government on measures related to the COVID-19 pandemic, potentially including measures to support families. Clinical guidelines were included as access to healthcare is a key determinant in early childhood development. Since the documents that were being considered are not typically peer-reviewed or published in academic literature, we focused on a search of the grey literature.
We designed and reviewed the search strategy with a health sciences librarian from Public Health Ontario. We devised search strings based on our targeted policy topics and repeated the search on a range of pre-designed search engines that pulled information specifically from governmental and public health bodies, as well as on Google. For each search string on each search engine, the first 100 results for each search were reviewed. Based on the findings of this search, targeted iterative manual searches on Google were also completed. Following this, we conducted a manual search of each country’s governmental websites (federal and provincial or state as relevant) to ensure that no other policy decisions were missed by the original search strategy. A manual search of the Netherland’s policies was completed by an author (MH) fluent in the language and then translated to English. We also reviewed guidance documents from national and provincial/state clinical colleges or bodies in pediatrics, obstetrics, and family medicine. The search was performed from August to November 2020. The full search strategy is outlined in Appendix A.
We chose to focus on early childhood development, including the prenatal environment to pre-school-aged children (0–5 years), and therefore any policies or programs specific to school-aged children were excluded (though policies that would apply to both pre-school- and school-aged children were included). Supports for families with young children were included, as the family environment is a key determinant of early childhood development. However, policies that were open to the general public, but not specifically targeting children, parents or families, were excluded. We included policies introduced by these governments from January to August 2020, as this timeframe included the first wave of COVID-19 for all countries.
During analysis, the authors discussed the policies and programs identified through the search, grouped these into the themes of prenatal and pediatric care, parental supports, and childcare and early childhood development, and then created further sub-themes based on consensus.
Results
Baseline characteristics of selected countries
Table 1 provides an overview of the baseline characteristics of the included countries. While each country is unique, there are similarities allowing for useful comparison. In terms of population size, the range was from Singapore’s population of 5.9 million to USA’s 328.2 million [24]. While Singapore has the smallest population, it has the highest population density. The GDP per capita ranged from $46,483 in the UK to $98,520 in Singapore, compared to $46,611 in Canada [24]. In this group of countries, the Gini coefficient ranged from 0.285 in the Netherlands to 0.458 in Singapore [27, 31].
We also examined baseline information about the current status of child health and supports for children in the country which provided context for the overall health of children in the pre-pandemic period (Table 1). In some cases, there was heterogeneity in the way the data were reported between countries, and the year of the most recent data available. The amount spent on ECE, as a percentage of GDP, ranged from about 0.20% in Singapore in 2011 (4–6 years old) and Canada in 2006 (0–6 years old), to over 0.65% in the UK and Australia in 2015 (3–5 years old) [25, 26, 32]. The percentage of children 3–5 years old (0–6 years old in Canada and 4–6 years old in Singapore) enrolled in ECE ranged from 24% in Canada in 2006 to 100% in the UK in 2017 [25, 26]. Immunization coverage for all of the childhood vaccines in all countries examined was > 90%. The largest differences were seen with measles vaccine coverage, which ranged from 90% in Canada and the USA, to 95% in Australia and the UK [33].
Epidemiologic indicators during the first wave of the COVID-19 pandemic
An overview of the epidemiology of COVID-19 in the included countries can be seen in Table 2. All countries identified their first case in late January or early February 2020, with the exception of the Netherlands, which identified their first case in late February. The date of the first wave peak ranged from late March to late July [29]. At peak, the number of cases per day ranged from 15.0 cases/million people in Australia to 203.5 cases/million people in the USA [29]. GSI scores indicate that public health measures implemented during each country’s peak were most relaxed in the USA, and the most stringent in Singapore [28]. Testing capacity and test positivity at peak was also assessed. Australia had the second highest testing capacity (2.62 per 1000), but the lowest test positivity (0.7%), while the USA had the highest testing capacity (2.89 per 1000), but mid-range test positivity (8.9%) [30]. On the other hand, the Netherlands, Singapore and the UK had lower testing capacities, and high test positivity rates (19.1–28.9%) [30]. Canada testing capacity was 0.7 per 1000 with a test positivity of 6.6% at the peak of the first wave [30].
Healthcare: prenatal, neonatal and pediatric care
Table 3 gives an overview of the overarching recommendations and guidance from clinical professional agencies and organizations from each country related to prenatal, neonatal and pediatric care.
Overall, there was general uniformity within the recommendations across countries, with only small variations. Each clinical body provided information on infection prevention and control (IPAC) policies, or links to related resources. As well, most clinical guidance focused on the clinical treatment of COVID-19 in patients (eg. pregnant women, infants). Of particular relevance was the guidance provided to health care providers on how to alter patient care schedules in order to reduce in-person contact. Most clinical organizations recommended continuing with current care schedules (ie. prenatal care, well-baby care). Canadian organizations recommended integrating virtual appointments when possible into the schedule, both for prenatal and pediatric care [14, 34]. As well, all countries’ clinical bodies recommended some flexibility in the care schedule if the patient were to have COVID-19 or be suspected to have COVID-19 - in those situations, a delay of 2 weeks would be permissible. Only Singapore recommended prenatal appointments be delayed if there was a general lockdown [35]. The USA recommended that the prenatal schedule be reduced if the risk outweighed the benefit [36]. Finally, there was agreement that the infant series of vaccination should continue as scheduled, as it was deemed an essential service in all countries.
There were a few other notable variations. For example, most jurisdictions specified that only one support person could accompany a patient during labour, while the Netherlands and Quebec allowed for two [37, 38]. As well, there was variation in the degree that different clinical organizations or agencies recommended that healthcare providers perform their own risk assessment based on their location and individual patients.
Parental supports
Table 4 provides an overview of governmental policies and programs to support mothers and/or parents. The included policies and programs were found to be mostly related to financial supports, domestic violence and housing.
In terms of financial supports, Canada, Australia and Singapore created specific benefits for parents, in addition to pre-existing supports, as well as financial supports that were offered to the general population during COVID-19 [39,40,41]. Within Canada, British Columbia provided an additional $225(CAN)/month benefit for children with special needs [42], and Ontario provided a one-time $200–$250(CAN) payment per child additional to the federal benefit [43]. Notably, there was variation in how these benefits were accessed, with Canada and Australia both requiring application to the benefits, while Singapore provided the benefit automatically to anyone who was already receiving other child benefits [39,40,41]. Canada introduced an additional financial support in August 2020 for parents who were forced to take time off of work in order to care for a child that must isolate [44]. Singapore also provided an additional separate benefit for low-income families, and a benefit for newborns [39]. This latter program was explicitly created to encourage people to continue having children during the COVID-19 pandemic. The UK, Netherlands and USA did not make any changes to their current policies or programs specifically related to financial support for families, although families may have benefited from other population-wide programs (e.g., universal tax credits, income programs for workers who were temporarily laid off).
Canada and Australia both increased funding to community organizations addressing domestic violence and for women’s shelters [45, 46]. Additionally, Canada’s federal government created additional shelters specifically for Indigenous women and children [45]. During the COVID-19 pandemic, the UK passed a law that increased protections and supports for those experiencing domestic violence [47]. However, that law was already being considered and drafted prior to the emergence of COVID-19.
Canada, the UK and the Netherlands specifically funded research related to the impact of COVID-19 pandemic on women and children, including the impact on mental health [48,49,50].
All of the countries’ governmental websites provided general information related to maternal mental health and well-being. As well, all countries’ governmental websites provided links to community organizations, programs, or other supports that already exist to aid parents and young children. Additional information including references for information in the tables is contained in Appendix B.
Childcare and early child development
Table 5 provides an overview of all governmental supports for early childhood development, which were found to be related to childcare, child protective services and food security. It should be noted that the term childcare refers to any form of care delivered to children aged 0–5 years, which may include pre-school, nursery school, licensed or unlicensed child care, or in-home services, as the specific way childcare is delivered in each country may vary and is typically a mix of these services.
In Canada, childcare centres were closed across the country in an attempt to reduce transmission of COVID-19, a decision made by each province. As such, there were variations across provinces in how childcare for children of essential workers was provided. Most provinces either permitted some designated childcare centres to remain open for children of essential workers or set up emergency childcare centres. Alternatively, the British Columbia government provided financial support for essential workers to arrange in-home childcare [51,52,53,54]. The Netherlands, UK and Michigan also closed childcare centres, but designated some to remain open for children of essential workers [55,56,57]. As childcare centres reopened, the UK introduced policy to reduce barriers to accessing tax-free childcare [58]. In contrast, Australia and Singapore kept childcare centres open throughout the first wave, although, Australia did see many childcare centres close due to parents choosing to withdraw their children [41, 59]. In response, Australia offered to pay for childcare for 2 months and also provided financial support to childcare services to help them maintain their staff until enrollment increased again [41]. Singapore introduced multiple policies to reduce barriers to high quality childcare centres, including decreasing fee caps and increasing both universal and targeted subsidies [59]. Singapore also created the KIDStart Initiative, a pilot early childhood development program for children from low-income families [59].
In terms of child protective or welfare services, almost all countries transitioned to a mix of in-person and virtual services, in order to reduce in-person contact. In Ontario, these services are managed through Ontario Children’s Aid Societies, delivered at the municipal level, creating further variation, with services continuing fully in-person in some municipalities, but not others [60]. Only England had a brief period where all services were moved to fully virtual [61]. Alternatively, Singapore child protective services began to proactively reach out to families in at-risk neighbourhoods, including in-person visits [59].
There was a large variation in the types of programs countries enacted to reduce the risk of food insecurity amongst children. Canada, the Netherlands and the USA increased funding to food banks and other emergency food relief organizations [45, 56, 62]. Three countries, the USA, Singapore and the UK, also instituted specific programs or interventions in addition to general increased funding to food relief organizations. The USA reduced barriers to accessing existing supports, such as the Special Supplemental Nutrition Program for Women, Infants and Children [62]. Singapore created a working group to assess and address food insecurity in young families, though their recommendations had not yet been made public [63]. At the same time, Singapore also increased food vouchers for low-income families [63]. The UK mandated that any childcare centres and schools that were providing food to children should find a way to continue providing that food [58].
Additionally, all of the countries’ governmental websites provided general information related to child mental health and well-being, though this very often focused more on adolescents. As well, all countries’ governmental websites provided links to community organizations, programs, or other supports that already exist to aid parents and young children.
Discussion
Overview
Our findings indicate that these countries provide helpful comparisons and contrasts through the variation in policy approaches in addressing maternal and early childhood concerns during the COVID-19 pandemic. Overall, there was significant heterogeneity in implementation of OECD-recommended policy responses. Overall, Singapore, Canada and Australia introduced a greater number of supports over a broader range of policy areas, while the Netherlands and USA introduced fewer policies or programs. Most policies were related to financial supports potentially indicating a gap for those who experience barriers to completing financial applications or filing taxes (e.g., undocumented residents), or where money can’t buy services (e.g., childcare if insufficient providers). It was also not clear if the financial supports were sufficient to meet needs as we did not find evidence of evaluation of the impact of implemented programs and policies. In contrast, there was relative consensus on clinical care during the prenatal, neonatal and pediatric stages.
Reasons for variations in policies
There is likely a large range of factors that influenced the variation in policies and programs introduced by the governments of these countries. The overarching political legacy and culture of these countries may have influenced the governments’ approaches. For example, within this group of countries, the USA has a legacy of less redistributive policies and cultural attitudes that are less accepting of government intervention. Therefore, it may not be surprising that the USA also enacted fewer supports for parents and young children during the first wave of the COVID-19 pandemic [64, 65]. In comparison, Canada has a legacy of greater social welfare supports than the USA and implemented more supports for children and families during COVID-19 [65]. Interestingly, the Netherlands, which has a much larger social welfare support system than the USA and Canada, also introduced fewer policies to support parents and young children during COVID-19. Potential explanations for this observation could be a higher baseline threshold of early childhood supports and fewer restrictions in the first wave compared to other countries. For example, in the Netherlands parents are already reimbursed a percentage for child care costs, depending on their income, and all employed parents have paid sick leave and additional paid “caretaking leave” to care for a sick family member [66, 67].
Potential impacts of policies
Preliminary studies indicated that COVID-19 and the community-wide public health measures implemented to reduce transmission of COVID-19 have already had significant impacts on maternal and child health and well-being [68]. The first wave of the COVID-19 pandemic required rapid response given the sudden disruption of long-standing systems of support, with many losing employment and access to childcare and other public health services. Furthermore, the public health measures and the closure of specific ECD programs likely disproportionately affected families already at-risk, from lower socioeconomic communities [69]. Nevertheless, the effectiveness of the policies presented here to counteract the negative impacts of COVID-19 on maternal and child health will take time to be understood.
Previous research has demonstrated the effectiveness of policies to support mothers and children in improving long-term health outcomes [11]. In line with the best available evidence, the OECD has compiled a list of possible governmental policies to counteract the negative impacts of COVID-19 on children [70]. All of the countries discussed in this study implemented some (e.g., prenatal care, child vaccination, child protection services), but not all, of the recommended actions (e.g., well child visits were discretionary in some jurisdictions, daycares closed, maternal supports for income, domestic violence and food required knowledge of available programs and in many cases application processes), suggesting significant opportunity for emergency preparedness and low barrier entry to responsive programs to protect this vulnerable group. In particular, while all governments provided information on their websites to pre-existing resources for mental health supports for young children and parents, no government created new supports or policies specifically targeting this area of need in the first wave of the COVID-19 pandemic. As well, Canada, Australia and the USA should consider how supports for early childhood development vary across their states or provinces and how this might affect health and health equity.
Moreover, it should be noted that the positive impact of these policies and programs will be mediated by the extent of implementation and uptake. For example, baseline access to large outdoor environments and having at least one parent free from working at home is a positive predictor of children’s physical activity [71]. Additionally, there is evidence that indicates that programs that automatically enroll participants and have fewer barriers to access will have greater uptake and impact than programs that require applications [72, 73]. Thus, Singapore may see a greater impact of their financial supports due to it automatically being given to those already receiving other social supports in contrast to Canada where participants had to apply for certain COVID-19 financial benefits.
Strengths and limitations of study
To the best of our knowledge, this is the only study that has looked at the acute response of governments to support young children and families during the acute first wave period of the pandemic. This study used a comprehensive and iterative search strategy of the grey literature. This allowed us to identify all relevant policy options and programs that the intended users or recipients would have access to via public websites.
Our study is limited by the number of countries included. We purposefully chose these countries in order to provide a broad range of political traditions and COVID-19 experiences. However, since we wanted to also allow the findings to be comparable to the Canadian context, all of these countries are high-income. All of the included countries, with the exception of Singapore, are OECD comparator countries. This means that our findings may not be applicable to low- and middle- income countries. Most of the countries included share responsibilities for funding and delivery of health and social programs/services between federal, state/provincial/territorial and local administrative/municipal levels of government. Due to the large number of entities involved, it was not possible to review programs and services at all levels of government which could impact interpretation, for example if the most impactful programs were delivered at the local level. As well, though our comparison is thorough, and we briefly explored possible reasons for variations in policy choices, a much greater political analysis would be required to fully understand the reasons for each countries’ specific policy and program decisions. Lastly, while we explored each countries’ governmental response and recommendations provided by clinical colleges and bodies, the degree of uptake and implementation of these programs by the targeted population has not been explored here.
Future directions
In the future, the implementation, uptake, and impact of these policies and programs should be assessed. Possible outcome indicators for evaluation could include infant mortality rate, low birth weight rate, vaccination coverage, educational attainment and literacy rates. Lastly, all countries should consider how to maintain a sufficient and ongoing baseline of support to optimize early childhood health and development across these policy areas, and identify in emergency planning specific program and policy areas that might require additional investment during acute and sustained emergencies.
Conclusion
This study explored the variation in how families and young children were supported during the first wave of the COVID-19 pandemic in Canada, Australia, Netherlands, Singapore, UK and USA through governmental policies and programs, as well as changes to healthcare provision. All of the included countries implemented some policies and programs to support families and young children, but there was a large range in the number, magnitude, and accessibility of these supports. None of the countries implemented supports in all of the potential areas identified. As the COVID-19 pandemic continues, there is an opportunity for every country to provide a sufficient baseline of healthy child policies and programs to optimize early childhood outcomes, and develop comprehensive plans for future responses to acute and sustained emergencies.
Availability of data and materials
All the data used in the study is from publicly available sources and data sets, which are provided in the references section.
Abbreviations
- ACE:
-
Adverse Childhood Event
- COVID-19:
-
Coronavirus Disease 2019
- ECE:
-
Early Childhood Education
- GDP:
-
Gross Domestic Product
- IPAC:
-
Infection Prevention and Control
- OECD:
-
Organization for Economic Co-operation and Development
- UK:
-
United Kingdom
- USA:
-
United States of America
References
Maggi S, Irwin LJ, Siddiqi A, Hertzman C. The social determinants of early child development: an overview. J Paediatr Child Health. 2010;46(11):627–35.
Hertzman C. Tackling inequality: get them while they’re young. BMJ. 2010;340(7742):346–8.
Danese A, McEwen BS. Adverse childhood experiences, allostasis, allostatic load, and age-related disease. Physiol Behav. 2012;106(1):29–39.
Andres E, Baird S, Bingenheimer JB, Markus AR. Maternity leave access and health: a systematic narrative review and conceptual framework development. Matern Child Health J. 2016;20(6):1178–92.
van den Heuvel M, Hopkins J, Biscaro A, Srikanthan C, Feller A, Bremberg S, et al. A comparative analysis of early child health and development services and outcomes in countries with different redistributive policies. BMC Public Health. 2013;13(1):1049.
Bento G, Dias G. The importance of outdoor play for young children's healthy development. Porto Biomed J. 2017;2(5):157–60.
Kristjansson E, Francis DK, Liberato S, Benkhalti Jandu M, Welch V, Batal M, et al. Food supplementation for improving the physical and psychosocial health of socio-economically disadvantaged children aged three months to five years. Cochrane developmental, psychosocial and learning problems group, editor. Cochrane Database Syst Rev. 2015. https://doi.org/10.1002/14651858.CD009924.pub2.
Cancian M, Slack KS, Yang MY. The effect of family income on risk of child maltreatment. Soc Serv Rev. 2013;87(3):417–37.
Marr C, Hingtgen S, Sherman A, Windham K, Cox K. Temporarily expanding child tax credit and earned income tax credit would deliver effective stimulus, help avert poverty spike. Center on Budget and Policy Priorities 2020. https://www.cbpp.org/research/federal-tax/temporarily-expanding-child-tax-credit-and-earned-income-tax-credit-would. Accessed 13 Jan 2021.
Navarro V, Muntaner C, Borrell C, Benach J, Quiroga Á, Rodríguez-Sanz M, et al. Politics and health outcomes. Lancet. 2006;368(9540):1033–7.
Siddiqi A, Irwin LJ, Hertzman C. Early child development: a powerful equalizer. In: Improving equity in health by addressing social determinants. Geneva: World Health Organization; 2011. p. 115–41.
Thapa SB, Mainali A, Schwank SE, Acharya G. Maternal mental health in the time of the COVID-19 pandemic. Acta Obstet Gynecol Scand. 2020;99(7):817–8.
Van Lancker W, Parolin Z. COVID-19, school closures, and child poverty: a social crisis in the making. Lancet Public Health. 2020;5(5):e243–4.
Bogler T, Bogler O. Interim schedule for pregnant women and children during the COVID-19 pandemic. Can Fam Physician. 2020; https://www.cfp.ca/news/2020/03/25/3-24. Accessed 26 Jan 2021.
Graham WJ, Afolabi B, Benova L, Campbell OMR, Filippi V, Nakimuli A, et al. Protecting hard-won gains for mothers and newborns in low-income and middle-income countries in the face of COVID-19: call for a service safety net. BMJ Glob Health. 2020;5(6):e002754.
Jago CA, Singh SS, Moretti F. Coronavirus disease 2019 (COVID-19) and pregnancy: combating isolation to improve outcomes. Obstet Anesth Dig. 2020;40(4):198–9.
Zhang X-B, Gui Y-H, Xu X, Zhu D-Q, Zhai Y-H, Ge X-L, et al. Response to children’s physical and mental needs during the COVID-19 outbreak. World J Pediatr. 2020;16(3):278–9.
Hynan MT. Covid-19 and the need for perinatal mental health professionals: now more than ever before. J Perinatol. 2020;40(7):985–6.
Onwuzurike C, Meadows AR, Nour NM. Examining inequities associated with changes in obstetric and gynecologic care delivery during the coronavirus disease 2019 (COVID-19) pandemic. Obstet Gynecol. 2020;136(1):37–41.
Douglas M, Katikireddi SV, Taulbut M, McKee M, McCartney G. Mitigating the wider health effects of covid-19 pandemic response. BMJ. 2020;369:m1557.
Canadian Institute for Health Information. OECD interactive tool: international comparisons — peer countries, Canada 2018. https://www.cihi.ca/en/oecd-interactive-tool-peer-countries-can. Accessed 20 Jan 2021.
Murphy RP, Emes J, Eisen B. Ontario vs Michigan: lessons from the wolverine state. Fraser Institute. 2016; https://www.fraserinstitute.org/sites/default/files/study-ont-vs-mich.pdf. Accessed 20 Oct 2021.
De Maio FG. Income inequality measures. J Epidemiol Amp Community Health. 2007;61(10):849–52.
World Bank. World Bank open data. In: Open Data. 2022; https://data.worldbank.org/. Accessed 27 Mar 2022.
Organisation for Economic Coperation and Development. Starting strong II: early childhood education and care. In: OECD 2006. https://www.oecd-ilibrary.org/education/starting-strong-ii_9789264035461-en. Accessed 18 Jan 2021.
Organisation for Economic Cooperation and Development. OECD family database - OECD [Internet]. In: OECD Family Database. 2019. https://www.oecd.org/els/family/database.htm. Accessed 18 Jan 2021.
Organisation for Economic Cooperation and Development. Income distribution database. In: income distribution database. 2020. https://stats.oecd.org/Index.aspx?DataSetCode=IDD. Accessed 18 Jan 2021.
Ritchie H, Ortiz-Ospina E, Beltekian D, Mathieu E, Hasell J, Macdonald B, et al. Policy responses to the coronavirus pandemic - statistics and research. In: Our World in Data. 2021; https://ourworldindata.org/policy-responses-covid. Accessed 18 Jan 2021.
Ritchie H, Ortiz-Ospina E, Beltekian D, Mathieu E, Hasell J, Macdonald B, et al. Coronavirus (COVID-19) cases - statistics and research. In: Our World in Data. 2021. Available from: https://ourworldindata.org/covid-cases. Accessed 18 Jan 2021.
Ritchie H, Ortiz-Ospina E, Beltekian D, Mathieu E, Hasell J, Macdonald B, et al. Coronavirus (COVID-19) testing - statistics and research. In: Our World in Data. 2021; https://ourworldindata.org/coronavirus-testing. Accessed 18 Jan 2021.
Li TW. Income inequality in Singapore falls to lowest level in almost two decades as household incomes rise. The Straits Times: In; 2020. https://www.straitstimes.com/singapore/income-inequality-in-singapore-falls-to-lowest-levels-in-almost-two-decades.
Early Childhood Development Agency. Ensuring quality early childhood education and childcare services. 2012. https://www.ecda.gov.sg/PressReleases/Pages/Ensuring-quality-early-childhood-education-and-childcare-services.aspx.
Vanderslott S, Dadonaite B, Roser M. Vaccination. Our World in Data: In; 2013. https://ourworldindata.org/vaccination.
Elwood C, Raeside A, Boucoiran I, Van Schalkwyk J, Money D, Yudin M, et al. Updated SOGC committee opinion - COVID-19 in pregnancy [internet]. 2020. https://www.sogc.org/common/Uploaded%20files/SOGC%20Committee%20Opinion200514may2020Final.pdf. .
College of Obstetricians & Gynaecologists, Singapore. Committee opinion - management of pregnancy and birth in women with coronavirus disease (COVID-19). 2020. https://www.ams.edu.sg/view-pdf.aspx?file=media%5c5443_fi_921.pdf&ofile=(Committee+Opinion)+Management+of+Pregnancy+and+Birth+in+Women+with+Covid-19+April+(20200420).pdf. Accessed 20 Oct 2021.
American College of Obstetricians and Gynecologists. COVID-19 FAQs for obstetrician-gynecologists, obstetrics. 2020. https://www.acog.org/en/ClinicalInformation/Physician FAQs/COVID 19 FAQs for Ob Gyns Obstetrics. Accessed 31 Aug 2020.
Government of Quebec. Pregnancy, delivery and the postnatal period during the coronavirus disease (COVID-19) pandemic. 2020. https://www.quebec.ca/en/health/health-issues/a-z/2019-coronavirus/information-for-pregnant-women-coronavirus-covid-19/. Accessed 30 Aug 2020.
Nederlandese Vereniging Voor Obstetrie & Gynaecologie. Perinatologische zorg in tijden van COVID-19. NVOG. 2020. https://www.nvog.nl/actueel/perinatologische-zorg-in-tijden-van-covid-19/. Accessed 30 Aug 2020.
Government of Singapore. Singapore budget 2020 - supplementary budget statement. 2020. https://www.singaporebudget.gov.sg/budget_2020/resilience-budget/supplementary-budget-statement. Accessed 13 Jan 2021.
Canada revenue agency. Canada child benefit (CCB) payment increase: CRA and COVID-19 [Internet] 2020. https://www.canada.ca/en/revenue-agency/campaigns/covid-19-update/covid-19-ccb-payment-increase.html. Accessed 13 Jan 2021.
Australian Bureau of Statistics. Methods changes during the COVID-19 period. 2020. https://www.abs.gov.au/articles/methods-changes-during-covid-19-period. Accessed 30 Aug 2020.
Columbia B. Ministry of Children and Family Development. Province provides emergency fund for children with special needs. 2020; https://news.gov.bc.ca/releases/2020CFD0043-000650.
Ontario Ministry of Education. Archived - get support for families. 2020. https://www.ontario.ca/page/get-support-families. Accessed 13 Jan 2021.
Canada Revenue Agency Canada Recovery Caregiving Benefit (CRCB) 2020. https://www.canada.ca/en/revenue-agency/services/benefits/recovery-caregiving-benefit.html. Accessed 24 Jan 2021.
Department of Finance Canada. Canada’s COVID-19 economic response plan. 2020. https://www.canada.ca/en/department-finance/economic-response-plan.html. Accessed 13 Jan 2021.
Murphy K. Australian government pumps $1bn into health and family violence services as coronavirus spreads. In: The Guardian. 2020; http://www.theguardian.com/australia-news/2020/mar/29/australian-government-to-pump-1bn-into-health-and-family-violence-services-as-coronavirus-spreads. Accessed 13 Jan 2021.
UK Government. Domestic abuse bill 2020: overarching factsheet. 2020. https://www.gov.uk/government/publications/domestic-abuse-bill-2020-factsheets/domestic-abuse-bill-2020-overarching-factsheet. Accessed 13 Jan 2021.
Canadian Institutes of Health Research. Government of Canada funds 49 additional COVID-19 research projects – details of the funded projects. 2020. https://www.canada.ca/en/institutes-health-research/news/2020/03/government-of-canada-funds-49-additional-covid-19-research-projects-details-of-the-funded-projects.html. Accessed 13 Jan 2021.
Dutch research council (NWO). Corona: fast-track data. 2020. https://www.nwo.nl/en/researchprogrammes/corona-fast-track-data. Accessed 13 Jan 2021.
Economic and Social Research Council. Social science and COVID-19 2020. https://esrc.ukri.org/files/news-events-and-publications/news/esrc-covid-19-activity/. Accessed 30 Aug 2020.
Government of Ontario. Ontario offers emergency child care to more frontline staff. 2020. https://news.ontario.ca/en/release/56696/ontario-offers-emergency-child-care-to-more-frontline-staff. Accessed 30 Aug 2020.
Government of Quebec. Questions and answers on education and families during the COVID-19 pandemic. 2020. https://www.quebec.ca/en/health/health-issues/a-z/2019-coronavirus/answers-questions-coronavirus-covid19/questions-answers-education-families-covid-19/. Accessed 30 Aug 2020.
Johnson L. COVID-19: Alberta expands eligibility for child care to include all essential workers. In: Edmonton Journal; 2020. https://edmontonjournal.com/news/politics/covid-19-alberta-expands-eligibility-for-child-care-to-include-all-essential-workers.
British Columbia Ministry of Child and Family Development. Ministry of Children & Family Development response to COVID-19. 2020. https://www2.gov.bc.ca/gov/content/family-social-supports/covid-19-information. Accessed 13 Jan 2021.
Government of Michigan. Whitmer - executive order 2020–51: expanding child care access during the COVID-19 pandemic - RESCINDED. 2020. https://www.michigan.gov/whitmer/0,9309,7-387-90499_90705-526011%2D%2D,00.html. Accessed 30 Aug 2020.
Government of Netherlands. Childcare for children of people working in crucial sectors 2020. https://www.government.nl/topics/coronavirus-covid-19/documents/publications/2020/03/20/childcare-for-children-of-people-working-in-crucial-sectors. Accessed 30 Aug 2020.
Key worker: official list of UK personnel who can still send children to school. In: The Guardian 2020. http://www.theguardian.com/world/2020/mar/20/key-worker-official-list-of-uk-personnel-who-can-still-send-children-to-school. Accessed 30 Aug 2020.
Working Families. Coronavirus (COVID-19) – what financial support is there for working families?. 2020. https://workingfamilies.org.uk/articles/coronavirus-support/. .
Channel news Asia. MSF to strengthen social safety nets ensuring ‘no Singaporean is left behind’ amid COVID-19: Masagos Zulkifli 2020. https://www.channelnewsasia.com/news/singapore/covid-19-msf-strengthen-social-safety-nets-masagos-zulkifli-13051466. Accessed 13 Jan 2021.
Ontario Ministry of Child and Youth Services. About Ontario’s children aid societies. 2020. http://www.children.gov.on.ca/htdocs/English/professionals/childwelfare/societies/index.aspx. Accessed 30 Aug 2020.
Government of United Kingdom. Coronavirus (COVID-19): guidance for children’s social care services. 2020. https://www.gov.uk/government/publications/coronavirus-covid-19-guidance-for-childrens-social-care-services/coronavirus-covid-19-guidance-for-local-authorities-on-childrens-social-care. Accessed 30 Aug 2020.
Food and Nutrition Service, U. S department of agriculture. FNS Responds to COVID-19 2020. https://www.fns.usda.gov/coronavirus. Accessed 30 Aug 2020.
Singapore Ministry of Social and Family Development. Impact of COVID-19 on Singaporeans and supporting measures. 2020. https://www.msf.gov.sg/media-room/Pages/Impact-of-COVID-19-on-Singaporeans-and-Supporting-Measures.aspx. Accessed 13 Jan 2021.
Fishback P. Social welfare expenditures in the United States and the Nordic countries: 1900-2003. In: Cambridge, MA: National Bureau of Economic Research; 2010. http://www.nber.org/papers/w15982.pdf. .
Stefan Svallfors. Welfare regimes and welfare opinions: a comparison of eight Western countries. In: Vogel J, editor. European welfare production: institutional configuration and distributional outcome. Dordrecht: Springer Netherlands; 2003. p. 171–196.
Pfau-Effinger B. Welfare state policies and the development of care arrangements. Eur Soc. 2005;7(2):321–47.
Yerkes MA, Javornik J. Creating capabilities: childcare policies in comparative perspective. J Eur Soc Policy. 2019;29(4):529–44.
Ontario Agency for Health Protection and Promotion (public health Ontario) Negative impacts of community-based public health measures on children, adolescents and families during the COVID-19 pandemic: update. 2021. https://www.publichealthontario.ca/-/media/documents/ncov/he/2021/01/rapid-review-neg-impacts-children-youth-families.pdf?la=en. Accessed 20 Oct 2021.
Spinelli M, Lionetti F, Setti A, Fasolo M. Parenting stress during the COVID-19 outbreak: socioeconomic and environmental risk factors and implications for children emotion regulation. Fam Process. 2020;60(2):639–53.
Organisation for Economic Co-operation and Development. Combatting COVID-19’s effect on children. 2020. http://www.oecd.org/coronavirus/policy-responses/combatting-covid-19-s-effect-on-children-2e1f3b2f/. Accessed 15 Sep 2020.
Pombo A, Luz C, Rodrigues LP, Ferreira C, Cordovil R. Correlates of children's physical activity during the COVID-19 confinement in Portugal. Public Health. 2020;189:14–9.
Dorn S. Automatic enrollment strategies: helping state coverage expansions achieve their goals. Washington, DC: Urban Institute; 2007. p. 35.
Hefford M, Crampton P, Foley J. Reducing health disparities through primary care reform: the New Zealand experiment. Health Policy. 2005;72(1):9–23.
Acknowledgements
A special thanks to Public Health Ontario’s Library Services for helping with formatting the numerous references.
Funding
No funding was received for the completion of this research.
Author information
Authors and Affiliations
Contributions
All authors contributed to the conceptualization and design of the project. JK performed data extraction. All authors contributed to data analysis. JK wrote the first draft of the manuscript, with all authors contributing to revisions. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable, as all information freely available in public domain.
Consent for publication
Not applicable.
Competing interests
The authors declare no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Appendix A.
Additional file 2:
Appendix B.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kearon, J., Carsley, S., van den Heuvel, M. et al. Early (years) reactions: comparative analysis of early childhood policies and programs during the first wave of the COVID-19 pandemic. BMC Public Health 22, 1383 (2022). https://doi.org/10.1186/s12889-022-13344-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-022-13344-0