Abstract
Background
Recent evidence suggests that climate change and other factors are leading to the emergence of Lyme disease in the province of Quebec, where it previously did not exist. As risk areas expand further north, the population can adopt specific preventive behaviors to limit chances of infection. The objectives of this study were to (1) create an index of Lyme disease prevention behaviors (LDPB), and (2) use the theory of planned behavior (TPB) to explain the decision-making process of people who choose to adopt LDPB.
Methods
A sample of 1959 adults living in a Lyme disease risk area completed a questionnaire by phone (n = 1003) or on the Web (n = 956). The questionnaire measured whether they did or did not adopt the LDPB proposed by public health officials. It also measured some TPB variables, including their attitude or perceived social norms regarding LDPB.
Results
Our findings led to the creation of a Lyme disease prevention index consisting of 10 behaviors, down from the 19 behaviors initially considered for inclusion in the index. Rates of adoption of each behavior varied tremendously, from 4.30 to 83.80%. All variables of the TPB model (attitude, social norms, and perceived control) were significantly associated with intention to adopt preventive behaviors. Intention itself was significantly associated with adoption of LDPB. Likewise, risk perception was positively correlated with the adoption of LDPB.
Conclusions
This study led to the creation of a Lyme disease prevention index that can be used by public health agencies, researchers, and professionals to monitor the evolution over time of individuals’ LDPB adoption rates. It also showed the usefulness of the TPB in understanding the adoption of LDPB and how intention to adopt such behaviors is formed.
Similar content being viewed by others
Background
Floods and heat waves are some of the most common issues linked to climate change, with current predictions showing an increase in their frequency and intensity in the near future [1,2,3,4]. However, the impacts of our changing climate on human health include not only these dangerous climatic events, but also an increase in zoonotic diseases, such as Lyme disease. Linked to a specific species of ticks in eastern and Midwestern North America, Ixodes scapularis, Lyme disease is slowly gaining ground further north, being found in areas where it used to be completely absent [5,6,7,8,9,10,11,12]. These areas include the province of Quebec, Canada, where the number of confirmed cases of Lyme disease rose from 32 in 2011 to 329 in 2017 [13]. This increase can be partly explained by warmer winters, rising global temperature, more rain, higher humidity, and changing patterns of seasonal weather caused by climate change making those previously inhospitable areas more favorable for Ixodes scapularis ticks and their hosts. These factors have led to improved survival and reproduction rates of ticks and their hosts, as well as an extended seasonal risk period [10, 14,15,16,17].
Since it was first identified in North America in the 1970s, Lyme disease has become the most commonly reported zoonotic disease in temperate areas [6, 18,19,20]. Infected Ixodes scapularis ticks can transmit Borrelia burgdorferi, the bacteria causing Lyme disease, to humans and some mammals. It can cause a variety of symptoms in humans, beginning with the most common: a red expanding or bulls-eye rash surrounding the bite. Present in 70 to 80% of infections, this rash can also be accompanied by fever, exhaustion, headaches, neck stiffness, and muscle and joint pain. Untreated, Lyme disease can then cause a wide variety of multisystemic issues, from arthritic joint deterioration to cardiac or neurological problems.
Fortunately, it is possible to reduce the risks of infection from Lyme disease, even in endemic areas. It has been shown that adopting simple behaviors like checking for ticks after going outside, wearing long clothes that cover the skin or using appropriate tick repellent spray can help prevent infection [21,22,23,24]. However, for people living in at-risk areas to implement these actions, they need to be aware of them and consider them effective [25]. Our goal was thus to produce a behavioral index of adaptation to Lyme disease, documenting adoption rates of a wide variety of adaptive behaviors throughout at-risk populations in the province of Quebec. Indices are an ideal way to monitor changes in behaviors throughout the years. Therefore, with the rapid increase of at-risk areas in the province of Quebec and the other provinces in Canada, subsequent studies using such an index could help decision makers better target vulnerable populations for awareness work, as well as provide a better picture of Lyme disease awareness in the population.
Some researchers [26,27,28,29] have developed behavioral measures of adaptation to Lyme disease based on scientific knowledge of what would constitute a good adaptation of individuals. However, these measures have never been tested with sophisticated modern psychometric analyses (e.g. item analysis based on item response theory, confirmatory factor analysis). The objectives of the present study were to start from the behavioral scales developed by these authors (1) to create and validate an index of Lyme disease prevention behaviors (LDPB) and (2) to use the theory of planned behavior (TPB) to explain the decision-making process of people who choose to adopt LDPB. In fact, the TPB will be useful for estimating the nomological validity of the index, and it will be well suited for identifying the social cognitive factors (e.g. social pressure, perceived barriers) that can be used to inform interventions designed to change Lyme disease prevention behaviors.
Theory of planned behavior
The TPB is a theoretical model that has already been successfully used to explain various behaviors related to the environment, such as adoption of climate change adaptation behaviors [30, 31], support for climate change policies [32], environmental sustainability through recycling [33], and use of improved natural grassland [34]. One meta-analysis has shown the effectiveness of the TPB for developing and conducting behavior change interventions [35].
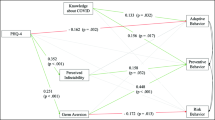
This theoretical framework (see Fig. 1) postulates that intentions to perform LDPB and perceived behavioral control (i.e. people’s perceptions of their ability to perform LDPB and/or the presence of factors that may facilitate or impede performance of LDPD) are the immediate antecedents of LDPB, and that perceived control can have a direct effect on behavior while also influencing behavior indirectly through its effect on intentions.
According to Fishbein and Ajzen [36], the effect of intention on action should be stronger when actual control is high rather than low. For instance, when people believe that they actually have control over the adoption of LDPB, they tend to act in accordance with their intentions. Conversely, if they believe that they have low control over the adoption of LDPB, they do not tend to act in accordance with their intentions [37].
The TPB also postulates that people’s intention to adopt LDPB should increase to the extent that they hold favorable attitudes toward such behaviors, think that significant others support the performance of these behaviors (i.e. perceived social norms), and perceive that they have control over them.
Finally, the TPB proposes that various background factors (e.g. gender, education, personality) can have primarily indirect effects on intentions and on adoption of LDPB through attitudes, perceived norm, and perceived control. Thus, to gain further insight into the underlying reasons for the implementation of LDPB among Quebec’s at-risk population, we examined the potential impact of two background factors from the health belief model: perceived risk or vulnerability represented by the disease, and perceived impact of the disease (severity) on health [38, 39].
Methods
Participants
A polling firm surveyed 1959 individuals (women, 62.02%), of whom 1003 (women, 68.30%) were contacted by telephone and 956 (women, 55.44%), through the online questionnaire. Cochran’s formula [40] was used to estimate the sample size with a 95% confidence level, a maximal variance of 4 for a five-point scale, and a precision level of 0.12.
All respondents came from a specific subset of Quebec municipalities considered to be at a low to high risk for Lyme disease [41,42,43], in the regions of Estrie, Montérégie, Mauricie-et-Centre-du-Québec, Outaouais, Lanaudière, Montréal, Laurentides, and Chaudière-Appalaches. Quotas by region were specified to the polling firm. They were adjusted using the Kish selection method [44, 45], with a maximum set for the most populous region, Montreal, to ensure that the sample from each region was sufficient and still representative.
Respondents had to be at least 18 years old to participate and the age distribution of the participants was: 18–34 [8.32%], 35–44 [14.09%], 45–54 [18.33%], 55–64 [27.05%], 65–74 [22.61%], 75 and over [9.29%]. They could complete the questionnaire and the interviews in French or in English. Most spoke French (91.88%) and were born in the province of Quebec (89.84%). Their highest education levels were an elementary school diploma (10.11%), a high school diploma (29.50%), a college or professional diploma (26.60%), or a university degree (33.13%). Regarding the composition of their household, 23.84% lived alone, 42.42% lived with another person, and 32.77% lived with two or more other persons.
The household structure consisted of a couple without children in 36.40% of the cases; a couple with children for 32.21% of them; and other structures, including living alone or with a roommate, for 30.12% of the respondents. The household income was less than CAD$20,000 for 8.73%, between CAD$20,000 and CAD$60,000 for 32.21%, between CAD$60,000 and CAD$100, 000 for 20.62%, and over CAD$100, 000 for 20.21%.
Data collection
The data were collected from May 18, 2018, to August 28, 2018, a period during which ticks nymphs are more active. The telephone interviews took an average of 20 min, and the response rate was 24.5%. A maximum of 10 attempts were made to establish contact before rejecting a telephone number. For the online questionnaire, a web panel that had been built by the polling firm prior to this data collection was used. Only the panelists living in the target areas were contacted by email, and their municipalities of residence were verified a second time with a question in the online questionnaire. The online questionnaire took an average of 17 min to complete, and the response rate was 17%.
Measures
Index of Lyme disease prevention behaviors (LDPB)
To identify an initial list of preventive behaviors, 19 items were selected based on a literature review [21, 22, 25, 46,47,48] and recommendations from public health agencies [42, 49]. These items are listed in Table 1. Filter questions allowed participants to answer only the items that concerned them. Thus, questions about behaviors with children, pets, or yard maintenance were not answered by all participants.
Items 3 through 14 and item 19 were coded according to a five-point scale with options: “Always,” “often,” “occasionally,” “rarely,” and “never.” Those answers were then dichotomized with “Always” and “Often” being considered to be LDPB. Items 1, 2, 16, and 18 were dichotomous and used a yes or no format. Item 15 used a four-point scale with options: “Yes, more than once a week,” “Yes, once a week or less,” “no,” and “I don’t have a lawn.” Item 15 was dichotomized as well, with the first two options being considered preventive. The “I don’t have a lawn” option was considered a missing value. Item 17 was coded with a five-point scale with options: “More than once a week,” “once a week,” “once or twice a month,” “less than once a month,” and “never.” Item 17 was dichotomized, and the first two options (i.e. “always” and “often”) were considered to be preventive. Responses to the items were summed to yield a measure of preventive behaviors (Cronbach’s α = 0.710).
Theory of planned behavior constructs
Attitude toward LDPB
Responses to the following question were used as reflective indicators of attitude toward the implementation of LDPB: adopting behaviors that will protect me against Lyme disease in the next year will be […]. Participants rated the item on a four-point scale ranging from “very useful” (4) to “very useless” (1).
Perceived social norms
Responses to the question were used to measure participants’ perception of social norms related to the implementation of LDPB: if I adopt behaviors to protect myself against tick bites and therefore Lyme disease in the next year, people who are important to me will support my choice. Participants rated the item on a four-point scale ranging from “strongly agree” (4) to “strongly disagree” (1).
Perceived behavioral control
Responses to the two questions (correlation: r = 0.398) were used to assess participants’ perceived control over LDPB: (a) it will be easy to protect myself against Lyme disease in the next year, (b) adopting behaviors to protect myself against Lyme disease in the next year will be […]. Participants rated each item on a four-point scale ranging, respectively, from “strongly agree” (4) to “strongly disagree” (1) and from “very easy” (4) to “very difficult” (1). Responses to the items were summed to obtain a measure of moral norms.
Intention to adopt LDPB
Intention to adopt LDPB was assessed by these two questions: (a) I intend to adopt behaviors to protect myself against tick bites and Lyme disease in the next year, (b) I have made up my mind to adopt behaviors to protect myself against Lyme disease in the next year. Participants rated each item on a four-point scale ranging from “strongly agree” (4) to “strongly disagree” (1). Responses to the items were summed to yield a measure of preventive behaviors (r = 0.691).
Perceived severity and risk
Two variables were added as background factors to the theory of planned behavior: one measured perceived severity of the consequences for health in the event of contracting Lyme disease, and the other measured the perceived risk of contracting Lyme disease in the next year.
Perceived severity
Perceived severity of Lyme disease was assessed by one question: “If you were to contract Lyme disease, would you say that the consequences for your health would be very serious?” Participants rated it on a four-point scale ranging from “Yes, absolutely” (4) to “No, not at all” (1).
Perceived risk
One question was used to measure participants’ perceived risk of contracting Lyme disease: “In your opinion, what is the risk of you contracting Lyme disease in the next year?” Participants rated it on a six-point scale ranging from “Very high” (6) to “Nil” (1).
Statistical analysis
Before performing any statistical analysis, we reweighted the data so that age, gender, number of people living in the household, education level, income, and proportions of people living in each administrative regions would be the same in the sample and the target population [50]. We also conducted a single imputation to handle the missing data for education level, age, household size, household structure, and income with predictive mean matching [51]. We then conducted a series of analyses to construct and evaluate the validity of the Lyme disease prevention index (Objective 1).
First, an item analysis was performed to analyze the relevance of the items and verify the reliability of the index using item response theory (IRT) and more particularly Samejima’s graded response model [52]. The objective of this item analysis was to assess the ability of the items to differentiate between individuals who adopt Lyme disease prevention behaviors and those who do not, according to a psychometric parameter called item discriminant power. This psychometric parameter could be conceived as a description of the association between each item and the measured construct, Lyme disease prevention behavior in the current study.
The item analysis aimed to determine which items to retain in the final index. Baker [53] proposes the following classification to evaluate the discrimination power of an item: (a) very poor: 0.34 or less; (b) poor: 0.35–0.64; (c) moderate: 0.65–1.34; (d) good: 1.35–1.69; and (e) very good: 1.70 or higher.
Second, we conducted a confirmatory factor analysis (CFA) for the retained items to assess the unidimensionality of the prevention index. We tested a model with a single construct representing Lyme disease prevention measured by the retained behaviors. We used various fit indices to assess the fit of our data with this model. The comparative fit index (CFI) and the Tucker-Lewis index (TLI) indicate a good model fit when they exceed 0.90 or 0.95 and the root mean square error of approximation (RMSEA) indicates a good fit when its value is below 0.08 or 0.06 [54, 55].
Third, to further ascertain the nomological validity of the index (a form of validity that pertains to the testing of proposed relationships among constructs in a model), we tested a model including the Lyme disease index as a dependent variable and the TPB constructs and a measure of perceived severity of Lyme disease and of the perceived risk of contracting Lyme disease in the next year, as determinants of the index. Testing the relationships of the index with constructs of a recognized psychosocial theory can further confirm that the index measures Lyme disease prevention behaviors (LDPB). This also helps to identify the factors that determine the adoption of LDPB and the ones that need reinforcement to support adoption of LDPB. Moreover, this model was tested by structural equation modelling (SEM) using Mplus 8 [56].
Model fit is evaluated using CFI, TLI and RMSEA with the same criterion values as for the confirmatory analysis [54, 55]. For CFI and TLI, acceptable model fit is indicated by values greater than or equal to 0.90 and less than 0.95, and excellent model fit is indicated by values greater than or equal to 0.95. For RMSEA, values between 0.05 and 0.08 indicate adequate model fit, whereas values less than or equal to 0.05 indicate excellent model fit [54, 55].
In some cases, perceived behavioral control also has a moderating effect on the effect of intention on behavior [57]. This interaction between latent variables is also tested once the final model without moderation is obtained and show a good fit. Model fit statistics like CFI, TLI, and RMSEA are not available when models with latent variable interaction are being tested with Mplus with function [58].
Results
Because of a high rate of missing data, items 11, 12, and 19 were not retained for the following analyses. Missing data rates were 94.03, 94.03, and 65.70%, respectively. These high rates were due to the filter questions retaining only participants with children under 5 years old for items 11 and 12 and only those with pets for item 19. Consequently, the psychometric analyses were performed on the retained 16 behavioral items.
Descriptive analyses
Means and standard deviations for each variable measured are presented in Table 2. Participants reported adopting a relatively low number of LDPB (M = 4.19 on a maximum score of 10), but a high intention to adopt these behaviors (M = 6.50 on a maximum score of 8), a favorable attitude toward LDPB (M = 3.25 on a maximum score of 4), a high perception of social pressure to perform the behaviors (M = 3.45 on a maximum score of 4), and a strong perception of control over the LDPB (5.59 on a maximum score of 8). The results also showed that people perceived a moderate risk of contracting Lyme disease (M = 3.08 on a maximum score of 6) and a strong risk that Lyme disease would have a negative impact on their health (M = 3.52 on a maximum score of 4). Consistent with many studies [59], the results in Table 2 revealed that the TPB variables were significantly correlated with intentions and the associated behaviors (LDPB in the present study). The results also indicated that the variables (perceived severity and risk) of the health belief model were significantly correlated with intentions and LDPB (see Table 2).
Item analysis
Excel add-in EIRT [60] provided the results for the item analysis. These results revealed that 14 of the 16 items composing the LDPD scale have acceptable discrimination power (i.e. they can help to differentiate individuals who adapt well to avoid Lyme disease from those who do not adapt as well). “Have a fence around property to prevent deer from coming in the yard” (item 16) and “Have a path or layer of wood chips or mulch to separate the patio, garden, or other installations from the trees or tall grass” (item 18) were removed because of poor correlations with the rest of the items (ρ = 0.170 and ρ = 0.180, respectively) as well as poor discrimination indices (discrimination power < .34; see the second column in Table 3). It is more likely that respondents adopted those behaviors not to prevent Lyme disease but for landscaping purposes.
The results in Table 3 also showed that the most adopted behavior was “Regularly mow lawn or have it mown” (80.2%) and that the least adopted behavior was “Put clothes in the dryer for six minutes to eliminate ticks that may be there after being outdoors” (4.3%).
Confirmatory factor analysis
The results of the CFA with all 14 remaining items showed a poor fit (CFI = 0.759 TLI = 0.716 and RMSEA = 0.063; χ2(77) = 675.698, p < 0.0001). Mplus provided modification parameter estimates and indices to identify problematic indicators. Some pairs of items had strong correlations and were thus combined into a single construct. “Look into ways to prevent Lyme disease” and “Look into potential consequences of Lyme disease for physical or mental health” were combined into “Look for information about Lyme disease,” which was set to “yes” if respondents did at least one of the items. “Wear pants and long-sleeved sweaters when practicing outdoor activities” and “Wear closed shoes when practicing outdoor activities” were combined into “Wear clothes that cover more skin,” and the behavior was considered adopted if respondents did at least one of the two former behaviors. “Tuck the bottom of sweater or shirt into pants when practicing outdoor activities” and “Tuck the bottom of pants into socks or boots when practicing outdoor activities” were combined into “Tuck clothes when practicing outdoor activities,” which was also considered adopted if respondents did at least one of the behaviors. “Regularly mow lawn or have it mown” and “Increase frequency of lawn maintenance” were also combined into “Increase frequency of lawn maintenance including mowing,” which was considered adopted if at least one of the two behaviors were adopted. With those changes, the model fit indices indicated an adequate fit (CFI = 0.941, TLI = 0.924, and RMSEA = 0.029). Thus, the final model was comprised of 10 behaviors (a combination of behaviors 1 and 2; 3 and 4; 5 and 6, 7, 8, 9, 10, 13, 14; and 15 and 17). Figure 2 presents this final prevention index.
Final model for the Lyme disease prevention index tested by confirmatory analysis. LDPB-1: Look into ways to prevent Lyme disease; LDPB-2: Wear clothes that cover more skin; LDPB-3: Tuck clothes when practicing outdoor activities; LDPB-4: Use bug repellent when outdoor; LDPB-5: Walk on cleared paths and trails, avoiding tall grass during outdoor activities; LDPB-6: Wear light-coloured clothing to make it easier to check for ticks during outdoor activities; LDPB-7: Examine body for ticks and remove them immediately after being outdoor; LDPB-8: Examine clothes and items to avoid bringing ticks into home after being outdoor; LDPB-9: Put clothes in the dryer for 6 minutes to eliminate ticks that may be there after being outdoor; LDPB-10: Increase frequency of lawn maintenance including mowing
Theory of planned behavior
The tested TPB model without the moderating effect of perceived control on the behavior index (see Fig. 3) accounted for 56.6% of the intention to adopt LDPB and 39.1% of the variance of the preventive behaviors. Attitudes, social norms, and perceived control all proved to be significantly associated with behavioral intention (γ = 0.110, γ = 0.355, and γ = 0.503, respectively, and all with p < 0.001). The association between intention and behavior was significant (γ = 0.625 with p < 0.001). The fit of the model was good (CFI = 0.97; TLI = 0.964; RMSEA = 0.028; χ2(99) = 253.482, p < 0.0001).
In a second analysis, the perceived risk of contracting Lyme disease and the perceived impact of this disease (severity) on health were introduced simultaneously into the standard TPB as background factors. The fit of the model to the data was poorer than that of the standard model, but nonetheless acceptable (CFI = .936; TLI = .921; RMSEA = .038; χ2(125) = 469.044, p < 0.0001). This model, to which we added two external variables, accounted for 59.4% (+ 2.8%) of the variance of people’s behavioral intention to adopt LDPB and 38.5% (− 0.6%) of the variance of the preventive behaviors. The effect of perceived risk was significant on the perceived social norms (γ = 0.202; p < 0.001) and perceived behavioral control (γ = − 0.134; p < 0.001). Severity was significant on attitude (γ = 0.134; p < 0.001), perceived social norms (γ = 0.239; p < 0.001), and perceived behavioral control (γ = 0.116; p = 0.006).
In a third analysis, we tested the standard TPB model with the moderating effect of perceived control on the relationship between intention and behavior. We chose that model because it showed better fit indices than the extended model in which we had added two predictive variables (perceived risk and perceived severity). The results revealed that it (see Fig. 4) accounted for 57.7% of the intention to adopt LDPB and 59.3% of the variance of the behaviors. Again, attitude, social norms, and perceived control all proved to be significantly associated with behavioral intention (γ = 0.152, γ = 0.374 and γ = 0.472, respectively, and all with p < 0.001). The association of intention with behavior was significant (γ = 0.653 with p < 0.001), as was the moderating effect of perceived control on the association of intention with behavior (γ = 0.343 with p = 0.01). Model fit indices like CFI, TLI, and RMSEA are not available for testing a model with a moderating effect [58]. Thus, we used the proportion of variance explained in the intention to perform LDPB and the actual adoption of LDPB to compare the TPB model without interaction with the TPB model with interaction. We kept the model with the moderating effect of perceived control on the association between intention and LDPB. We did this because of the greater proportion of variance explained, in line with the TPB, which assesses the presence of this moderating effect [57].
Discussion
The main goal of this study was to produce and validate an index of adaptation to Lyme disease that could be used to monitor the evolution of the Quebec population’s adoption of preventive behaviors. Concerning the population’s adaptation to Lyme disease, the data from this study show that Quebeckers are eager to learn more about the disease and how to better prepare against it, with 56.90% of respondents seeking information in this regard. Overall, the data from the final index, composed of 10 behaviors, shows that Quebeckers are still at the first stage of adopting preventive behaviors: the rate of adoption of each behavior varies widely, with the least common being “Put clothes in the dryer for six minutes to eliminate ticks that may be there after being outdoors” at only 4.30%, and the most commonly practiced being “lawn maintenance including mowing” at 83.80%. It seems that the more specific LDPB are the least commonly practiced. Indeed, drying the clothes after being outdoors or examining the clothes or the skin for ticks are both adopted by 20% or less of the respondents. Of note, all of the measured behaviors that are comparable to similar behaviors examined by Aenishaenslin et al. [27] showed an increased rate of adoption in our study. As an example, in their 2015 study, where they examined the adoption of LDPB in Québec’s Montérégie region, performing tick checks after outdoor activities was reported by only 7.00% of the participants. Such a behavior could be compared to examining the clothes or the skin in our study, in which the reported adoption rates were 13.60 and 20.01%, respectively. While the specific questions and behaviors used in their study were different from ours, this highlights the importance of creating an index that can be reused throughout the years to monitor the evolution of Quebeckers’ adaptation to Lyme disease, as the infected ticks become more widespread across the province.
On another note, the final index combined some of the behaviors originally included in the study with others that were similar, but also excluded some that had poor fit discrimination indices. For example, we found that most behaviors related to lawn care had poor correlations with the rest of the items. This could mean that respondents adopted those behaviors for general landscaping reasons, not as preventive measures specifically designed to protect themselves from Lyme disease. The final result was an index of adaptation to Lyme disease composed mainly of behaviors closely related to individuals and their own bodies and clothes, instead of more structural behaviors related to their households and lands. These individual behaviors are all easy to adopt, consisting of simple actions like checking for ticks on your clothes or skin after coming back from a hike in the woods, and are commonly suggested by health authorities and even some local municipalities. They are also, and most importantly, good indicators of a population’s rate of adaptation because, unlike some of the behaviors removed from the index because of poor fit, they seem to be more often undertaken specifically to prevent Lyme disease.
Our results also showed that risk perception was positively correlated with the adoption of LDPB. Furthermore, they showed that perceived risk had a significant influence on perceived control and perceived social norms. Perceived risk seemed to have an influence on the adoption of LDPB and needs to be further investigated. Measuring perceived risk as a latent construct with multiple indicators could be a solution to help better estimate its influence in the TPB model of LDPB adoption.
Even though the TPB model including perceived risk and perceived severity as background factors was not the tested model with the highest data fit, the significant relationship observed between risk perception and perceived severity with the adoption of LDPB cannot be dismissed. This finding is also in line with other studies on perceived risk and preventive health behaviors, which have demonstrated that risk perception was associated with the adoption of preventive behaviors [27, 47, 61,62,63]. As such, while this finding is unsurprising, it provides important information that could be used by health authorities and local governments, who would do well to include information on the risks and consequences of Lyme disease when creating information booklets or messages intended for the population. However, it should be noted that, overall, Lyme disease is already perceived by most of our respondents (94.3%) as having a severe impact on health, and that despite the currently low rate of confirmed cases in Quebec, 34.6% of them perceived a risk of being infected with the disease in the following year.
In this same line of inquiry, we conducted some basic analyses of the decision-making process that could explain why people would choose to adopt LDPB. The TPB model had excellent results, showing that all variables of the model (i.e. attitude, social norms, and perceived control) were significantly associated with intention to adopt preventive behaviors, and that intention itself was significantly associated with adoption of LDPB. While the use of the TPB model in this study was limited to a small subset of questions, further research on the specific variables making up the attitudes, social norms, and perceived control over LDPB could help provide tailored messaging specific to targeted demographics. Such targeted messaging, using the data obtained from the model, has been proven to be more effective than more generic health messages in other cases involving health behaviors [64, 65].
This study has some limitations. First, though it is comparable to most other studies on pro-environmental behavior [30, 66, 67], ours was reliant on self-reported of adoption of preventive behaviors, which could lead some participants to overestimate the extent to which they adopted these behaviors. Consequently, to reduce participants’ socially desirable response bias, we indicated to the participants that their responses were anonymous. Second, the study’s low response rate (24.5%) suggests that the sample may be biased, as the participants were likely to be more interested in adopting Lyme disease prevention behaviors than was the general population. Third, the TPB’s belief variables could not be measured due to concerns about the length of the questionnaire. We preferred to limit the length of the questionnaire to favor a better response rate. Measuring participants’ behavioral, normative and control beliefs could have provided more detailed information regarding the dominant beliefs that underlie people’s decisions to adopt or not Lyme disease prevention behaviors. As previously mentioned, such a study could also help health and government officials to develop more tailored messages in the Province of Quebec.
Conclusions
Our findings led to the creation and validation of a Lyme disease prevention index made from a specific set of behaviors easily adoptable by people living in areas at risk of Lyme disease. As ticks progress further north, year after year, the widespread adoption of these measures would help protect the population from this disease. Our index can be used by public health agencies, researchers, and professionals to monitor the evolution over time of individuals’ rates of LDPB. Finally, the results of this study also showed the usefulness of the TPB as a framework for understanding the adoption of LDPB and how intention to adopt such behaviors is formed. It explained 57.7% of the variance of intention, along with a high percentage of the effect of intention on behavior (65%), making it a good questionnaire for further studies in this field.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- TPB:
-
Theory of planned behavior
- LDPB:
-
Lyme disease prevention behavior
- CFA:
-
Confirmatory factor analysis
- CFI:
-
Comparative fit index
- TLI:
-
Tucker-Lewis index
- RMSEA:
-
Root mean square error of approximation
- SEM:
-
Structural equation model
References
Asadieh B, Krakauer NY. Global trends in extreme precipitation: climate models versus observations. Hydrol Earth Syst Sci. 2015;19(2):877–91.
Bao J, Sherwood SC, Alexander LV, Evans JP. Future increases in extreme precipitation exceed observed scaling rates. Nat Clim Chang. 2017;7(2):128–32.
Gie C, Stocker TF, Qin D, Plattner G-K, MMB T, Allen SK. Changements climatiques 2013 Les éléments scientifiques; 2013. p. 11. Report No.: 9789291692385.
Schar C. Climate extremes: the worst heat waves to come. Nat Clim Chang. 2016;6(2):128–9.
Berry P, Clarke K, Fleury MD, Parker S. Human health. In: Warren FJ, Lemmen DS, editors. Canada in a changing climate: sector perspectives on impacts and adaptation. Ottawa: Government of Canada; 2014. p. 191–232.
Brownstein J, Holford T, Fish D. Effect of climate change on Lyme disease risk in North America. Ecohealth. 2005;2(1):38–46.
Khatchikian CE, Prusinski MA, Stone M, Backenson PB, Wang I-N, Foley E, et al. Recent and rapid population growth and range expansion of the Lyme disease tick vector, Ixodes scapularis, in North America. Evolution. 2015;69(7):1678–89.
McPherson M, García-García A, Cuesta-Valero FJ, Beltrami H, Hansen-Ketchum P, MacDougall D, et al. Expansion of the Lyme disease vector Ixodes Scapularis in Canada inferred from CMIP5 climate projections. Environ Health Perspect. 2017;125(5):057008.
Ogden NH, Radojević M, Wu X, Duvvuri VR, Leighton PA, Wu J. Estimated effects of projected climate change on the basic reproductive number of the Lyme disease vector ixodes scapularis. Environ Health Perspect. 2014;122(6):631–8.
Simon JA, Marrotte RR, Desrosiers N, Fiset J, Gaitan J, Gonzalez A, et al. Climate change and habitat fragmentation drive the occurrence of Borrelia burgdorferi, the agent of Lyme disease, at the northeastern limit of its distribution. Evol Appl. 2014;7(7):750–64.
Wu X, Lu Y, Zhou S, Chen L, Xu B. Impact of climate change on human infectious diseases: empirical evidence and human adaptation. Environ Int. 2016;86:14–23.
Bouchard C, Leonard E, Koffi JK, Pelcat Y, Peregrine A, Chilton N, et al. The increasing risk of Lyme disease in Canada. Can Vet J. 2015;56(7):693.
Santé et Services sociaux Québec. Maladie de Lyme - Évolution de la maladie au Québec. 2017 [cited 2017 Jul 13]. Available from: http://www.msss.gouv.qc.ca/professionnels/zoonoses/maladie-lyme/evolution-de-la-maladie-au-quebec/.
Boeckmann M, Joyner TA. Old health risks in new places? An ecological niche model for I. Ricinus tick distribution in Europe under a changing climate. Health Place. 2014;30:70–7.
Campbell-Lendrum D, Manga L, Bagayoko M, Sommerfeld J. Climate change and vector-borne diseases: what are the implications for public health research and policy? Philos Trans R Soc B. 2015;370(1665):20130552.
Ogden NH, Maarouf A, Barker IK, Bigras-poulin M, Lindsay LR. Climate change and the potential for range expansion of the Lyme disease vector Ixodes scapularis in Canada. Int J Parasitol. 2005;36(1):63–70.
Monaghan AJ, Moore SM, Sampson KM, Beard CB, Eisen RJ. Climate change influences on the annual onset of Lyme disease in the United States. Ticks Tick-borne Dis. 2015;6(5):615–22.
Bouchard C, Beauchamp G, Leighton PA, Lindsay R, Bélanger D, Ogden NH. Does high biodiversity reduce the risk of Lyme disease invasion? Parasit Vectors. 2013;6(1):195.
Leighton PA, Koffi JK, Pelcat Y, Lindsay LR, Ogden NH. Predicting the speed of tick invasion: an empirical model of range expansion for the Lyme disease vector Ixodes scapularis in Canada. J Appl Ecol. 2012;49(2):457–64.
Ogden NH, Lindsay LR, Morshed M, Sockett PN, Artsob H. The emergence of Lyme disease in Canada. Can Med Assoc J. 2009;180(12):1221–4.
Smith G, Wileyto EP, Hopkins RB, Cherry BR, Maher JP. Risk factors for Lyme disease in Chester County, Pennsylvania. Public Health Rep. 2001;116(1 suppl):146–56.
Vázquez M, Muehlenbein C, Cartter M, Hayes EB, Ertel S, Shapiro ED. Effectiveness of personal protective measures to prevent Lyme disease. Emerg Infect Dis. 2008;14(2):210–6.
Connally NP, Durante AJ, Yousey-Hindes KM, Meek JI, Nelson RS, Heimer R. Peridomestic Lyme disease prevention. Results of a population-based case-control study. Am J Prev Med. 2009;37(3):201–6.
Finch C, Al-Damluji MS, Krause PJ, Niccolai L, Steeves T, O’Keefe CF, et al. Integrated assessment of behavioral and environmental risk factors for Lyme disease infection on Block Island, Rhode Island. PLoS One. 2014;9(1):e84758.
Bouchard C, Aenishaenslin C, Rees EE, Koffi JK, Pelcat Y, Ripoche M, et al. Integrated social-behavioral and ecological risk maps to prioritize local public health responses to Lyme disease. Environ Health Perspect. 2018 Apr 5;126(4):047008.
Aenishaenslin C, Ravel A, Michel P, Gern L, Milord F, Waaub J-P, et al. From Lyme disease emergence to endemicity: a cross sectional comparative study of risk perceptions in different populations. BMC Public Health. 2014;14(1):1298.
Aenishaenslin C, Michel P, Ravel A, Gern L, Milord F, Waaub J-P, et al. Factors associated with preventive behaviors regarding Lyme disease in Canada and Switzerland: a comparative study. BMC Public Health. 2015;15:185–95.
Garvin JH, Gordon TF, Haignere C, JP DC. Development of a public health assessment tool to prevent lyme disease: tool construction and validation. Perspect Health Inf Manag. 2005;6;2. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2047320/. [cited 2019 Feb 15].
Gould LH, Nelson RS, Griffith KS, Hayes EB, Piesman J, Mead PS, et al. Knowledge, attitudes, and behaviors regarding Lyme disease prevention among Connecticut residents, 1999-2004. Vector Borne Zoonotic Dis. 2008;8(6):769–76.
Bichard E, Kazmierczak A. Are homeowners willing to adapt to and mitigate the effects of climate change? Clim Chang. 2012;112(3–4):633–54.
Deng Y, Wang M, Yousefpour R. How do people’s perceptions and climatic disaster experiences influence their daily behaviors regarding adaptation to climate change? — a case study among young generations. Sci Total Environ. 2017;581–582:840–7.
Wang X. The role of future orientation, cultural worldviews, and collective efficacy in the American public’s climate change attitudes and policysupport. Int J Pub Opin Res. 2018;30:493–503.
Ahmad MS, Bazmi AA, Bhutto AW, Shahzadi K, Bukhari N. Students’ responses to improve environmental sustainability through recycling: quantitatively improving qualitative model. Appl Res Qual Life. 2016;11(1):253–70.
Borges JAR, Oude Lansink AGJM. Identifying psychological factors that determine cattle farmers’ intention to use improved natural grassland. J Environ Psychol. 2016;45:89–96.
Steinmetz H, Knappstein M, Ajzen I, Schmidt P, Kabst R. How effective are behavior change interventions based on the theory of planned behavior?: a three-level meta-analysis. Z Psychol. 2016;224(3):216–33.
Fishbein M, Ajzen I. Predicting and changing behavior: the reasoned action approach. New York: Psychology Press; 2010.
Ajzen I. From intentions to actions: a theory of planned behavior. In: Kuhl J, Beckman J, editors. Action-control: From cognition to behavior. Heidelberg: Springer; 1985. p. 11–39.
Rosenstock IM. The health belief model and preventive health behavior. Health Educ Behav. 1974;2(4):354–86.
Conner M, Norman P. Predicting health behaviour. Maidenhead, Berkshire: Open University Press; 2005.
Cochran WG. Sampling technique. 2nd ed. New York: Wiley; 1963.
Institut national de santé publique. Rapport de surveillance de la maladie de Lyme: Année 2016. 2017 [cited 2020 June 5]. Available from: https://www.inspq.qc.ca/sites/default/files/publications/2296_surveillance_maladie_lyme_2016.pdf.
Institut national de santé publique du Québec. La maladie de Lyme et les maladies transmises par les tiques . 2017 [cited 2017 Jul 10]. Available from: https://www.inspq.qc.ca/zoonoses/maladie-de-lyme.
Institut national de santé publique. Liste des municipalités à risque d’acquisition de la maladie de Lyme. 2018 [cited 2018 Sep 3]. Available from: https://www.inspq.qc.ca/sites/default/files/documents/zoonoses/municipalites-risque-maladie-lyme-juillet2018.pdf.
Kish L. Multipurpose sample designs. Surv Methodol. 1988;14(1):19–32..
Kish L. Optima and proxima in linear sample designs. Journal of the Royal Statistical Society Series A (General). 1976;139:80–95.
Aenishaenslin C, Bouchard C, Koffi JK, Ogden NH. Exposure and preventive behaviours toward ticks and Lyme disease in Canada: results from a first national survey. Ticks Tick-borne Dis. 2017;8(1):112–8.
Beaujean DJMA, Bults M, van Steenbergen JE, Voeten HACM. Study on public perceptions and protective behaviors regarding Lyme disease among the general public in the Netherlands: implications for prevention programs. BMC Public Health. 2013;13(1):225.
Beaujean D, Van Velsen L, Van Gemert-Pijnen JEWC, Maat A, Van Steenbergen JE, Crutzen R. Using risk group profiles as a lightweight qualitative approach for intervention development: an example of prevention of tick bites and lyme disease. J Med Internet Res. 2013;2:e45.
Gouvernement du Canada. Prévention de la maladie de Lyme. 2017 [cited 2017 Jul 2]. Available from: https://www.canada.ca/fr/sante-publique/services/maladies/maladie-lyme/prevention-maladie-lyme.html.
Deville J-C, Särndal C-E. Calibration estimators in survey sampling. J Am Stat Assoc. 1992;87(418):376–82.
White IR, Royston P, Wood AM. Multiple imputation using chained equations: issues and guidance for practice. Stat Med. 2011;30(4):377–99.
Samejima F. Estimation of latent ability using a response pattern of graded scores (Psychometrika monograph no. 17). Psychometric Society: Richmond; 1969.
Baker FB. The basics of item response theory. College Park, MD.: ERIC clearinghouse on assessment and Evaluation; 2001.
Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Model Multidiscip J. 1999;6(1):1–55.
Kline R. Principles and practice of structural equation modeling. 3rd ed. New York: Guildford Publications; 2011. p. 427.
Muthén LK, Muthén BO. Mplus User’s Guide. 8th Edition. Los Angeles: Muthén & Muthén; 1998-2017. 950 p.
Ajzen I. The theory of planned behavior. In: Lange PAM, Kruglanski AW, Higgins ET, editors. Handbook of theories of social psychology. London: Sage; 2012. p. 438–59.
Little TD, Bovaird JA, Widaman KF. On the merits of orthogonalizing powered and product terms: implications for modeling interactions among latent variables. Struct Equ Model. 2006;13(4):497–519.
Conner M, Sparks P. Theory of planned behaviour and the reasoned action approach. In: Predicting and changing health behaviour: research and practice with social cognition models. 3rd ed: Open University Press; 2015. p. 142–88.
Valois P, Houssemand C, Germain S, Abdous B. An open source tool to verify the psychometric properties of an evaluation instrument. Procedia Soc Behav Sci. 2011;15:552–6.
Herrington JE, Campbell GL, Bailey RE, Cartter ML, Adams M, Frazier EL, et al. Predisposing factors for individuals’ Lyme disease prevention practices: Connecticut, Maine, and Montana. Am J Public Health. 1997;87:2035–8.
Herrington JE. Risk perceptions regarding ticks and Lyme disease: a national survey. Am J Prev Med. 2004;26.
Mowbray F, Amlot R, Rubin GJ. Predictors of protective behaviour against ticks in the UK: a mixed methods study. Ticks Tick-Borne Dis. 2014;5(4):392–400.
D’Ippoliti D, Michelozzi P, Marino C, De’Donato F, Menne B, Katsouyanni K, et al. The impact of heat waves on mortality in 9 European cities: results from the EuroHEAT project. Environmental Health. 2010;9(37) Available from. https://doi.org/10.1186/1476-069X-9-37.
Lowe D, Ebi KL, Forsberg B. Heatwave early warning systems and adaptation advice to reduce human health consequences of Heatwaves. Int J Environ Res Public Health. 2011;8(12):4623.
Bakhsh K, Rauf S, Zulfiqar F. Adaptation strategies for minimizing heat wave induced morbidity and its determinants. Sustain Cities Soc. 2018;41:95–103.
Liu T, Xu YJ, Zhang YH, Yan QH, Song XL, Xie HY, et al. Associations between risk perception, spontaneous adaptation behavior to heat waves and heatstroke in Guangdong province, China. BMC Public Health. 2013;13(1):913.
Acknowledgments
We gratefully acknowledge financial support from the Green Fund, funded by the Institut national de santé publique du Québec (INSPQ). We also wish to thank the 1 959 participants for their time.
Funding
This research was supported by the Green Fund of the Québec government (QC, Canada) as part of the 2013–2020 Climate Change Action Plan (http://www.mddelcc.gouv.qc.ca/cgfv/programmes.htm). The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
PV, DB, DT, and MT were involved in the conception of the study and the study design. PV, DB, CA, CB and SB were involved in the conception of the survey. PV and DT advised on the data analyses, and MT conducted the data analyses. PV and DB wrote the initial manuscript, which has been reviewed by all authors. CA, CB, SB, and DT contributed to subsequent revisions of the manuscript. All authors read and approved the final manuscript and agreed to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Human Subject Research Ethics Board, Université Laval, QC, Canada (reference number 109526, file number 2014–301 ACF). In the introduction of the study, participants were explicitly asked for their informed oral consent before they could answer the phone survey, and they were explicitly asked for their informed written consent before they could answer the Web survey. This method was approved by the committee.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1.
Questionnaire.pdf. Questionnaire on Individual Adaptation to Lyme Disease. Description of data: English language version of the questionnaire developed and used for this study.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Valois, P., Bouchard, D., Aenishaenslin, C. et al. Development and validation of a behavioral index for adaptation to lyme disease. BMC Public Health 20, 1435 (2020). https://doi.org/10.1186/s12889-020-09535-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-020-09535-2