Abstract
Background
The heavy workload of physicians in Taiwan may contribute to poor lifestyles and increased risk for diabetes mellitus (DM). We conducted this study to determine the risk for DM among physicians in Taiwan.
Methods
We used the Taiwan National Health Insurance Research Database to identify 28,440 physicians and 56,880 comparisons (general population) matched at a ratio of 1:2 by age and sex. Participants who had been diagnosed with DM before 2007 were excluded. We compared the risk for DM between physicians and comparisons by following up since 2007 to 2013. Comparisons among physician subgroups were also performed.
Results
After adjustment for hypertension, hyperlipidemia, hyperuricemia, coronary artery disease, congestive heart failure, hyperthyroidism, hypothyroidism, and polycystic ovary syndrome, physicians had a lower risk for DM than the comparisons (adjusted odds ratio [AOR]: 0.75; 95% confidence interval [CI]: 0.68–0.82). In comparisons among physicians, emergency physicians (AOR: 2.21; 95% CI: 1.44–3.40) and surgeons (AOR: 1.26; 95% CI: 1.05–1.52) had a higher risk for DM than other specialists.
Conclusions
This study found that physicians have a lower risk for DM than the general population and emergency physicians and surgeons have a higher risk for DM than other specialists. Thus, more attention should be paid to the occupational health of these doctors.
Similar content being viewed by others
Background
Diabetes mellitus (DM) is a global disease that shows a dramatic increase in prevalence every year. The global diabetic population is expected to reach 366 million in 2011 and 552 million in 2030 [1]. In Taiwan, an increase of over 70% in the total diabetic population was observed from 2000 to 2009 [2]. DM is associated with many subsequent complications, including retinopathy, nephropathy, neuropathy, cardiovascular diseases, and death, and greatly increases the burden of medical expenditures [3,4,5,6,7].
Physicians in Taiwan generally bear a heavy workload, as 50% of the country’s physicians work over 57 h per week, 34.5% work as many as 65 h per week, and approximately 10.6% require an average of 21 extra hours on top of the work average of other professions [8]. Many physicians, such as emergency physicians, surgeons, critical-care specialists, and internists, must accept rotating night shifts, which are considered a risk factor for DM [9]. Heavy workloads and rotating night shifts may contribute to poor lifestyles with insufficient physical activity and unhealthy diets, both of which are also risk factors for developing DM [10]. Searches in PubMed and Google Scholar for studies on the risk for DM in physicians were not found after searching for the key words “physician” and “diabetes mellitus.” Thus, we conducted this research to determine the risk for DM among physicians in Taiwan.
Methods
Data sources
Two sub-datasets of the National Health Insurance Research Database (NHIRD) were used for the current study, namely, the 2010 Registry for Medical Personnel and the Longitudinal Health Insurance Database 2000 (LHID 2000). The 2010 Registry for Medical Personnel includes information about the specialty, work area, license date, hospital level, types of employment, and encrypted identification number of physicians, nurses, pharmacists, and other healthcare providers, which can be linked to claims data [11]. The LHID 2000 features the claims data of 1 million beneficiaries (4.34% of the total population) who were randomly selected from the NHIRD [12]. The NHIRD is derived from the Taiwan National Health Insurance Program, a universal healthcare system that covers nearly 100% of the country’s population [11]. The database of this program contains registration files and original claims data for reimbursement [11]. Large computerized databases derived from this system by the National Health Insurance Administration, Ministry of Health and Welfare, Taiwan, and maintained by the National Health Research Institutes, Taiwan, are provided to scientists in Taiwan for research purposes [11].
Study design
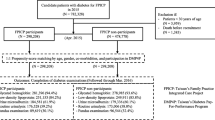
We identified all physicians from the 2010 Registry for Medical Personnel and comparisons (i.e., general population after excluding healthcare providers) from the LHID 2000 registered in 2010 by matching age and sex at a ratio of 1:2 for this study (Fig. 1). Residents were excluded because they did not have a specialty board and, therefore, cannot be categorized into a physician specialty for comparison. Residents also tend to have short experiences as physicians, which means their work may not completely reflect the effect of occupational exposure. DM was defined by the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes of 250 in at least one hospitalization or at least three ambulatory care events. Participants who had been diagnosed with DM before 2007 were excluded. Comorbidities were defined as hypertension (ICD-9-CM: 401–405), hyperlipidemia (ICD-9-CM: 272), hyperuricemia (ICD-9-CM: 274), coronary artery disease (ICD-9-CM: 410–414), congestive heart failure (ICD-9-CM: 428), hyperthyroidism (ICD-9-CM: 242), hypothyroidism (ICD-9-CM: 243–244), and polycystic ovary syndrome (ICD-9-CM: 256.4) in at least one hospitalization or at least three ambulatory care events between 2007 and 2013. We compared the risk of DM between physicians and comparisons, as well as among physician subgroups, in terms of specialty, age, and sex by following up the participants’ medical histories since January 1, 2007 to December 31, 2013. We classified the physicians into the following six specialties for the analysis: internal medicine, surgery, obstetrics and gynecology (Ob/Gyn), pediatrics, emergency medicine, family medicine, and other specialties.
Ethics statement
This study was conducted according to the Declaration of Helsinki. The Institutional Review Board of Chi-Mei Medical Center approved of this study and waived the need for informed consent from participants because the dataset consists of de-identified data. This waiver does not affect the rights and welfare of the participants.
Statistical analysis
We used the chi-square test for categorical variables and the independent t-test for continuous variables to compare the demographic characteristics between the two groups. Conditional logistic regression was used to compare the risk for DM between physicians and comparisons. Comparisons of risks for DM among specialty, age, and sex subgroups in physicians were performed by unconditional logistic regression with adjustment of age, sex, hypertension, hyperlipidemia, hyperuricemia, coronary artery disease, congestive heart failure, hyperthyroidism, hypothyroidism, and polycystic ovary syndrome. SAS (version 9.4 for Windows, SAS Institute, Inc., Cary, NC, USA) was used for all analyses in this study, and significance was set at 0.05 (two-tailed).
Results
We identified 28,440 physicians and 56,880 age- and sex-matched comparisons for the current study (Table 1). The mean age of both physicians and comparisons was 46.5 ± 10.9 years. Males made up 85.3% of the participants in both groups. Compared with the general population, more physicians had hypertension (20.0% vs. 18.9%, p < 0.001) and hyperlipidemia (19.3% vs. 13.7%, p < 0.001) but fewer physicians had coronary artery disease (5.4% vs. 6.0%, p < 0.001) and congestive heart failure (0.5% vs. 1.1%, p < 0.001).
Conditional logistic regression analyses with adjustment for hypertension, hyperlipidemia, hyperuricemia, coronary artery disease, congestive heart failure, hyperthyroidism, hypothyroidism, and polycystic ovary syndrome showed that physicians had a lower risk for DM than the general population (adjusted odds ratio [AOR]: 0.75; 95% confidence interval [CI]: 0.68–0.82) (Table 2). Stratified analyses according to age showed a lower risk for DM in physicians in the subgroups of 35–49 years (AOR: 0.68; 95% CI: 0.57–0.81) and 50–64 years (AOR: 0.74; 95% CI: 0.65–0.85). Although male physicians had a lower risk for DM than male comparisons (AOR: 0.74; 95% CI: 0.67–0.82), the same trend was not observed between female physicians and comparisons (AOR: 0.95; 95% CI: 0.64–1.42).
Emergency physicians (AOR: 2.21; 95% CI: 1.44–3.40) and surgeons (AOR: 1.26; 95% CI: 1.05–1.52) had a higher risk for DM than other specialists (Table 3). Older and male physicians had a higher risk than their counterparts.
Discussion
The current study found that the risk for DM in physicians was lower than that in the general population. Stratified analyses showed lower risks in the age subgroups of 35–49 years and 50–64 years and in the male population. Emergency physicians and surgeons had a higher risk for developing DM than other specialists. In physicians, male sex and older age were risk factors for DM.
An explanation for the lower risk for DM observed among physicians in comparison with the general population is that, despite heavier workloads and the related poor lifestyle, the former have better medical knowledge, higher disease awareness, and easier healthcare access than the latter; these benefits may mitigate the risk for DM among physicians. The current result is also compatible with previous studies in Taiwan that showed that, despite physicians having higher risks for hypertension, hyperlipidemia, migraine, and herniated intervertebral disc than the general population [13,14,15,16], the former were also less vulnerable to major and life-threatening diseases, including cardiovascular, cancer, and severe sepsis than the latter [13, 17,18,19].
The finding of lower risks for DM in the subgroups of age 35–64 years and male physicians suggests that age and sex are effect modifiers. Although a better medical background may be a protective factor for physicians, younger physicians (< 35 years) have shorter occupational exposures and may not reflect the true status of a physician. The current result is compatible with a previous study that reported that physicians have a lower risk for stroke than the general population; however, this lower risk was not found in physicians younger than 35 years [17]. Older physicians (≥65 years) may have less disease awareness and medical access and more comorbidities, which may decrease the benefit of a better medical background [19]. Why a lower risk for DM was found only in male physicians is not clear. A previous study showed a similar finding, i.e., all-cancer risk was lower in male physicians than in the male general population; however, female physicians did not show this trend [18]. Further studies on this disparity are necessary.
The finding that emergency physicians and surgeons are at higher risk for DM than other physician specialties may be related to the heavier work stress and frequent night shifts of the former. A stressful work environment may increase the risk of type 2 DM [20]. A population-based study previously reported that participants with high job stress have a 45% higher risk for developing type 2 DM than those with low job stress [20]. According to the SESMAT study in France, emergency physicians accumulate more stress than other physicians [21]. Work-family conflict and quality of teamwork are independent predictors of stress [21]. A burnout and satisfaction research showed that emergency physicians have a 3-fold higher burnout rate compared with those of other specialties [22]. A study recruiting 2860 participants in Japan reported that shift workers had a higher risk for DM than fixed daytime workers [23]. Another study recruiting 10 participants who had undergone a 10-day laboratory protocol reported that circadian misalignment increases serum glucose [24]. In Nurses’ Health Studies I and II, extended periods of rotating night-shift work among nurses resulted in a significant increase in risk for type 2 DM [9]. In addition, rotating night-shift workers may develop unhealthy behaviors, including smoking and irregular mealtimes, which may also increase the risk for DM [9].
Among physicians, older age and male sex were associated with increased risk for DM, compatible with previous studies. A nationwide study in Taiwan reported that the incidence of DM was higher in men, especially in the 20–59-year-old age group, then in women [2]. Impaired fasting glucose is significantly more common in men than in women [25]. One possible reason for this difference is that men tend to have lower hepatic sensitivity to insulin and, therefore, generally higher fasting levels of plasma glucose than women [26].
The current study presents two strengths: it is the first study to compare the risk for DM between physicians and the general population and the study features a nationwide design. Several limitations must also be acknowledged. First, some important risk factors of DM, including body mass index, life style, and family history of DM, were not considered in this work. However, we adjusted for hypertension and hyperlipidemia, which may serve as substitutes for body mass index and lifestyle. Second, data on occupational exposure, including workload, stress, and night shifts, were not available, and this lack of information may affect our comparisons among physician specialties. Third, the discrepancy about lower risk of DM but higher prevalence of hypertension and hyperlipidemia in the physicians than in the general population could not be explained in the present study. Because it is beyond the scope of this study, further research about this issue is warranted in the future. Fourth, a six-year follow-up may not be long enough to confirm our findings; a longer research period may be necessary. Finally, the results may not be generalized to other nations due to differences in race, health care systems, and cultures.
Conclusion
The current study revealed that, despite their heavy workloads, physicians are at lower risk for DM than the general population. This finding could be explained by the former having better medical knowledge, higher disease awareness, and easier healthcare access, which may compensate for the effect of heavy workloads, than their general-population counterparts. Comparisons among physicians revealed that emergency physicians and surgeons are at higher risk for developing DM than other specialists, which may be explained by these two specialties experiencing heavier work stresses and more frequent night shifts than their counterparts in other specialties. In addition, male sex and older age were predictive of DM risk in physicians. The results of this work provide an important reference for future efforts to improve occupational health among physicians, especially those in high-risk specialties, such as emergency physicians and surgeons.
Availability of data and materials
Data are available from the National Health Insurance Research Database (NHIRD), which is published by the Taiwan National Health Insurance Bureau. Due to legal restrictions imposed by the government of Taiwan in relation to the Personal Information Protection Act, data cannot be made publicly available. Requests for data can be sent as a formal proposal to the NHIRD (http://nhird.nhri.org.tw).
Abbreviations
- AOR:
-
Adjusted odds ratio
- CI:
-
Confidence interval
- DM:
-
Diabetes mellitus
- ICD-9-CM:
-
International Classification of Diseases, Ninth Revision, Clinical Modification
- LHID:
-
Longitudinal Health Insurance Database
- NHIRD:
-
National Health Insurance Research Database
- Ob/Gyn:
-
Obstetrics and gynecology
References
Guariguata L, Whiting D, Weil C, Unwin N. The international diabetes federation diabetes atlas methodology for estimating global and national prevalence of diabetes in adults. Diabetes Res Clin Pract. 2011;94:322–32.
Jiang YD, Chang CH, Tai TY, Chen JF, Chuang LM. Incidence and prevalence rates of diabetes mellitus in Taiwan: analysis of the 2000-2009 Nationwide health insurance database. J Formos Med Assoc. 2012;111:599–604.
Duckworth W, Abraira C, Moritz T, Reda D, Emanuele N, Reaven PD, Zieve FJ, Marks J, Davis SN, Hayward R, Warren SR, Goldman S, McCarren M, Vitek ME, Henderson WG, Huang GD, Investigators VADT. Glucose control and vascular complications in veterans with type 2 diabetes. N Engl J Med. 2009;360:129–39.
Huang CC, Weng SF, Tsai KT, Chen PJ, Lin HJ, Wang JJ, Su SB, Chou W, Guo HR, Hsu CC. Long-term mortality risk after hyperglycemic crisis episodes in geriatric patients with diabetes: a national population-based cohort study. Diabetes Care. 2015;38:746–51.
Huang CC, Chou W, Lin HJ, Chen SC, Kuo SC, Chen WL, Chen JH, Wang HY, Guo HR. Cancer history, bandemia, and serum creatinine are independent mortality predictors in patients with infection-precipitated hyperglycemic crises. BMC Endocr Disord. 2013;13:23.
Huang CC, Chien TW, Su SB, Guo HR, Chen WL, Chen JH, Chang SH, Lin HJ, Wang YF. Infection, absent tachycardia, cancer history, and severe coma are independent mortality predictors in geriatric patients with hyperglycemic crises. Diabetes Care. 2013;36:e151–2.
Huang CC, Kuo SC, Chien TW, Lin HJ, Guo HR, Chen WL, Chen JH, Chang SH, Su SB. Predicting the hyperglycemic crisis death (PHD) score: a new decision rule for emergency and critical care. Am J Emerg Med. 2013;31:830–4.
Chen KY, Yang CM, Lien CH, Chiou HY, Lin MR, Chang HR, Chiu WT. Burnout, job satisfaction, and medical malpractice among physicians. Int J Med Sci. 2013;10:1471–8.
Pan A, Schernhammer ES, Sun Q, Hu FB. Rotating night shift work and risk of type 2 diabetes: two prospective cohort studies in women. PLoS Med. 2011;8:e1001141.
Manson JE, Rimm EB, Stampfer MJ, Colditz GA, Willett WC, Krolewski AS, Rosner B, Hennekens CH, Speizer FE. Physical activity and incidence of non-insulin-dependent diabetes mellitus in women. Lancet. 1991;338:774–8.
National Health Insurance Research Database. Background. Accessed from https://nhird.nhri.org.tw/en/index.html on July, 2018.
National Health Insurance Research Database. Data subsets. Accessed from https://nhird.nhri.org.tw/en/Data_Subsets.html on July, 2018.
Chen YT, Huang CC, Weng SF, Hsu CC, Wang JJ, Lin HJ, Su SB, Guo HR, Juan CW. Acute myocardial infarction: a comparison of the risk between physicians and the general population. Biomed Res Int. 2015;2015:904328.
Kuo WY, Huang CC, Weng SF, Lin HJ, Su SB, Wang JJ, Guo HR, Hsu CC. Higher migraine risk in healthcare professionals than in general population: a nationwide population-based cohort study in Taiwan. J Headache Pain. 2015;16:102.
Liu C, Huang CC, Hsu CC, Lin HJ, Guo HR, Su SB, Wang JJ, Weng SF. Higher risk for cervical herniated intervertebral disc in physicians: a retrospective nationwide population-based cohort study with claims analysis. Medicine (Baltimore). 2016;95:e5055.
Chan FK, Hsu CC, Lin HJ, Wang JJ, Su SB, Huang CC, Weng SF. Physicians as well as nonphysician health care professionals in Taiwan have higher risk for lumbar herniated intervertebral disc than general population. Medicine. 2018;97:e9561.
Tam HP, Lin HJ, Weng SF, Hsu CC, Wang JJ, Su SB, Huang CC, Guo HR. The risk of stroke in physicians: a population-based cohort study in Taiwan. Epidemiology. 2017;28:S48–53.
Lee YS, Hsu CC, Weng SF, Lin HJ, Wang JJ, Su SB, Huang CC, Guo HR. Cancer incidence in physicians: a Taiwan national population-based cohort study. Medicine. 2015;94:e2079.
Shen HN, Lu CL, Li CY. Do physicians have lower risk of severe sepsis and associated mortality? A matched cohort study. Crit Care Med. 2014;42:816–23.
Huth C, Thorand B, Baumert J, Kruse J, Emeny RT, Schneider A, Meisinger C, Ladwig KH. Job strain as a risk factor for the onset of type 2 diabetes mellitus: findings from the MONICA/KORA Augsburg cohort study. Psychosom Med. 2014;76:562–8.
Estryn-Behar M, Doppia MA, Guetarni K, Fry C, Machet G, Pelloux P, Aune I, Muster D, Lassaunière JM, Prudhomme C. Emergency physicians accumulate more stress factors than other physicians-results from the French SESMAT study. Emerg Med J. 2011;28:397–410.
Shanafelt TD, Boone S, Tan L, Dyrbye LN, Sotile W, Satele D, West CP, Sloan J, Oreskovich MR. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med. 2012;172:1377–85.
Morikawa Y, Nakagawa H, Miura K, Soyama Y, Ishizaki M, Kido T, Naruse Y, Suwazono Y, Nogawa K. Shift work and the risk of diabetes mellitus among Japanese male factory workers. Scand J Work Environ Health. 2005;31:179–83.
Scheer FA, Hilton MF, Mantzoros CS, Shea SA. Adverse metabolic and cardiovascular consequences of circadian misalignment. Proc Natl Acad Sci U S A. 2009;106:4453–8.
Ter Horst KW, Gilijamse PW, de Weijer BA, Kilicarslan M, Ackermans MT, Nederveen AJ, Nieuwdorp M, Romijn JA, Serlie MJ. Sexual dimorphism in hepatic, adipose tissue, and peripheral tissue insulin sensitivity in obese humans. Front Endocrinol. 2015;6:182.
Geer EB, Shen W. Gender differences in insulin resistance, body composition, and energy balance. Gend Med. 2009;6(Suppl 1):60–75.
Acknowledgements
Nil.
Funding
Nil.
Author information
Authors and Affiliations
Contributions
SGL, JYC, and CC Huang designed the study, interpreted the data, and wrote the manuscript. IJF performed statistical analysis. CC Hsu, YFW, CYY, and JJW provided clinical experience and helped draft the manuscript. JYC and CC Huang supervised the whole study and were responsible for all communications. All authors have read and approve of the final manuscript.
Authors’ information
Nil.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was conducted according to the Declaration of Helsinki. The Institutional Review Board of Chi-Mei Medical Center approved of this study and waived the need for informed consent from participants because the dataset consists of de-identified data. This waiver does not affect the rights and welfare of the participants.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Lee, SG., Feng, IJ., Hsu, CC. et al. Risk of diabetes mellitus in physicians: a nationwide study in Taiwan. BMC Public Health 19, 1047 (2019). https://doi.org/10.1186/s12889-019-7403-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-019-7403-z




