Abstract
Background
Cardiovascular (CV) diseases (CVDs) are the leading cause of mortality worldwide. Globally, there is a growing interest in understanding and addressing modifiable psychosocial risk factors, particularly depression and anxiety, to prevent CVDs and to reduce morbidity and mortality. Despite the high premature mortality rate from CVDs in Latvia, this is the first Latvian study to examine the association of depression and anxiety with CVD morbidity in a primary care population.
Methods
This cross-sectional study was carried out in 2015 within the framework of the National Research Program BIOMEDICINE at 24 primary care facilities throughout Latvia. Consecutive adult patients during a one-week time period at each facility were invited to join the study. Assessments onsite included a 9-item Patient Health Questionnaire (PHQ-9) and a 7-item Generalized Anxiety Disorder scale (GAD-7) followed by a socio-demographic questionnaire and measurements of height, weight, waist circumference, blood pressure, and total cholesterol. The diagnostic Mini International Neuropsychiatric Interview (MINI) was conducted over the telephone within 2 weeks after the visit to the general practitioner. A multivariate model was developed using binary logistic regression.
Results
From the 1565 subjects (31.2% male), CVD was detected in 17.1%. Depression screening was positive (PHQ-9 ≥ 10) for 14.7%, and anxiety screening was positive (GAD-7 ≥ 10) for 10.1% of the study subjects. According to the MINI, 10.3% had current and 28.1% had lifetime depressive episode, and 16.1% had an anxiety disorder. Depression, not anxiety, was statistically significantly related to CVDs with an odds ratio (OR) of 1.52 (p = 0.04) for current depressive symptoms (PHQ-9 ≥ 10) and 2.08 (p = 0.002) for lifetime depressive episode (MINI).
Conclusions
Current depressive symptoms (PHQ-9 ≥ 10) and a lifetime depressive episode (according to the MINI) were significantly associated with increased risk of CV morbidity. Therefore, CV patients should be screened and treated for depression to potentially improve the prognosis of CVDs. Enhanced training and integration of mental health treatment in Latvian primary care settings may improve clinical outcomes.
Similar content being viewed by others
Background
Anxiety and major depressive disorder (MDD) are the most common mental disorders in the European Union (EU) affecting 20.9% of the population (99.4 million people every year). MDD is already now the most important single contributor to the total disease burden not only in the EU but also worldwide, as measured by disability-adjusted life years (DALYs) [1, 2]. Anxiety disorders are the most frequent mental disorders in the general population with a prevalence rate of 14% [1]. Mental disorders, particularly anxiety and depression, are highly prevalent in patients with chronic somatic illnesses, affecting approximately 50% of patients in primary care settings [3, 4], and they are associated with poorer prognosis and increased treatment non-compliance, financial costs, other resource utilization, lost productivity and disability [5, 6]. The comorbidity of depression, anxiety and cardiovascular (CV) diseases (CVDs) is an especially important public health concern because CVDs are the leading cause of death globally, representing 31% of all deaths [7]. In Latvia, the mortality rate from CVDs is one of the highest in the EU, reaching 57% of all death in 2015 [8, 9], with the standard premature mortality from CVDs three times higher than on average than in the EU [10].
Depression and anxiety are highly prevalent in patients with CVDs [11]. Approximately one in five patients hospitalized for an acute coronary event meets the diagnostic criteria for MDD, and about half (40–65%) demonstrate sub-syndromal depressive symptoms [12], a prevalence rate that is at least three times higher than in the general population [13]. This proportion is even greater in stroke survivors, affecting nearly one in three patients [14, 15]. Clinically significant symptoms of anxiety have been reported in 20% to 42% of the CVD population [16,17,18].
Over the last 25 years, a large body of evidence has demonstrated that depression and anxiety are not only more common in CV patients, but that these two psychiatric conditions are also risk factors for increased cardiac morbidity and recurrent CV events and mortality, independent of traditional CV risk factors [19, 20]. The seminal INTERHEART study, involving 15,152 myocardial infarction (MI) cases from 52 countries, revealed that psychosocial factors such as depression and anxiety account for 32% of the population attributable risk (PAR) for MI, a level of risk comparable to that of smoking (PAR, 35.7%) and even greater than that of diabetes (PAR, 9.9%) and hypertension (PAR, 17.9%) [21]. Depression predicts incident coronary heart disease (CHD) (relative risk (RR) = 1.9 (95% confidence interval (CI): 1.49–2.42)) [22] and stroke (hazard ratio (HR) = 1.45 (95% CI: 1.29–1.63)) [23]. Previous meta-analyses evaluating the prognostic association of depression with mortality and new CV events in patients with already established CVDs demonstrated that depression is associated with a 1.6- to 2.6-fold increased risk of future major adverse cardiovascular events, cardiac mortality and all-cause mortality [24, 25], a level similar to traditional CV risk factors such as reduced left ventricular ejection fraction and diabetes [26]. A meta-analysis by Roest et al. in 2010 summarizing 20 prospective studies found that anxiety was associated with a 26% increased risk of incident CHD (HR = 1.26; 95% CI: 1.15–1.38) and a 48% increased risk of cardiac mortality (HR = 1.48; 95% CI: 1.14–1.92), independent of demographic variables, biological risk factors, and health behaviors [27]. A more recent meta-analysis that included 37 studies with 1,565,699 participants found an even stronger association and showed that anxiety was associated with a 52% increased incidence of CVD (HR = 1.52, 95% CI: 1.36–1.71) [28], despite some studies pointing to a possible protective role of anxiety in CVD prognosis [29, 30]. Another recent meta-analysis by Emdin et al. in 2016 concluded that the association of anxiety with stroke was stronger (RR = 1.71, 95% CI: 1.18–2.50) than the association of anxiety with CHD (RR = 1.41, 95% CI: 1.23–1.61) [31].
The largest cross-sectional surveys on CV risk factors in the EU called European Action on Secondary and Primary Prevention by Intervention to Reduce Events (EUROASPIRE) were conducted to determine whether the Joint European Societies guidelines on CVD prevention are being followed in clinical practice [32, 33]. EUROASPIRE III and IV surveys concluded that large proportions of CV patients in the EU do not achieve lifestyle, risk factor and therapeutic targets and there is considerable variations between European countries in patients’ CV risk factor prevalences and use of cardioprotective medications [34, 35]. The Baltic States (Estonia, Latvia and Lithuania) appeared to be among the most profoundly CVD-affected countries within Europe with very high CV mortality rates compared to other countries in the EU [10, 34]. It was explained by high prevalence of CV risk factors (dyslipidemia, obesity, diabetes and hypertension) that may relate to a larger proportion of poorer and older people, patients with lower education, as well as those outside social support networks, problems in doctor-patient relationship, inadequate dosing of drugs, unhealthy lifestyle [36, 37]. Comorbidity of depression and/or anxiety with CVD as a possible explanation has not been sufficiently examined in the Baltic region. Search of the literature revealed only few studies from Lithuania and Estonia that provided conflicting results [38, 39]. As the premature mortality rate from CVD in Latvia is alarmingly high [10], this topic is of particular importance for Latvia where there have been no studies to date.
We therefore aimed to conduct the first study on the association of depression and anxiety with CVDs in a primary care population in Latvia. This study addresses an important gap in the literature by focusing on Latvia. Recent evidence reported major cross-country differences in the determinants of disability among patients with heart disease and supported implementation of country-specific programs to reduce disability among CV patients [40]. Therefore local data are crucially important for the management of CV patients and for medical and nursing education, policy, and program development in Latvia.
Methods
The cross-sectional study was carried out in 2015 within the framework of the National Research Program BIOMEDICINE 2014–2017 to assess the prevalence of the most frequent mental disorders in primary care settings in Latvia. Patients were recruited from 24 primary care facilities all over the country (16 in urban and 8 in rural areas). The survey was conducted in Latvian and Russian (the two most commonly spoken languages in Latvia).
Ethics
This study was approved by the Ethics Committee of the Riga Stradins University, Riga, Latvia (No. 8/ 18.06.2015.). The project was carried out in accordance with the Declaration of Helsinki and its subsequent amendments. All respondents were enrolled only after providing written informed consent.
Subjects and procedures
The inclusion criteria were consecutive treatment-seeking patients visiting a general practitioner (GP), patients aged 18 or older, and patients who had provided their informed consent. The exclusion criteria were patients who refused to participate in the study, patients younger than 18 years of age, and patients with acute medical condition requiring urgent hospitalization.
During a one-week period at each primary care facility, all consecutive patients who corresponded to the inclusion criteria were invited to complete a nine-item Patient Health Questionnaire (PHQ-9) and a seven-item Generalized Anxiety Disorder scale (GAD-7) in Latvian or Russian (language as preferred by participant) followed by an interview with a structured socio-demographic questionnaire and measurements of height, weight, waist circumference, blood pressure and total cholesterol on the same study visit. The Mini International Neuropsychiatric Interview (MINI) was conducted over the telephone by specially trained psychiatrists within a period of two weeks after the first contact. Diagnoses of CVD were confirmed using medical records. CVD was defined as an atherosclerotic vascular disease in the heart (CHD, angina, MI), brain (cerebrovascular disease, transient ischemic attack, stroke) and periphery (peripheral arterial disease), or a combination of these conditions [19]. Additionally, information about the diagnosis of depression and anxiety disorders, prescription of cardiovascular and psychotropic medications, and blood test results of lipids, glucose and glycated hemoglobin from the previous 3 months were obtained from medical documents.
Assessment tools and measures
The PHQ-9 is a self-rating tool that was developed from the Primary Care Evaluation of Mental Disorders (PRIME-MD) questionnaire in the late 1990s to screen and to diagnose patients with depressive disorders in primary care settings [41]. It consists of nine items that correspond to the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) diagnostic criteria for MDD [42]. Respondents rate the questionnaire items from 0 to 3 according to the frequency of their experience over the previous two-week period (not at all, several days, more than half the days, or nearly every day). A systematic review [43] of the diagnostic accuracy of most widely used screening tools for depression among patients with chronic physical health problems found that the PHQ-9 with a cut-off score equal to or greater than 10 has good sensitivity (84%) and specificity (88%) to detect MDD and is even superior to the Hospital Anxiety and Depression Scale (HADS) (sensitivity = 75%; specificity = 81%). The first large-scale UPBEAT-UK study of the accuracy of commonly used depression screening measures within a primary care CHD population also concluded that the PHQ-9 appeared diagnostically superior when compared to HADS [44]. The Latvian and Russian versions of the PHQ-9 for Latvia were validated as a part of the National Research Project BIOMEDICINE 2014–2017 [45, 46].
The GAD-7 is a self-reported measure of anxiety [47, 48]. Participants were asked to consider the preceding two weeks and to rate symptom frequency as not at all (0), several days (1), more than half of all days (2) or nearly all days (3). Scores of 5, 10, and 15 were taken as the cut-off points for mild, moderate and severe anxiety, respectively. Using the threshold score of 10, the GAD-7 has a sensitivity of 89% and a specificity of 82% for generalized anxiety disorder. It is moderately good at screening three other common anxiety disorders: panic disorder (PD) (sensitivity = 74%, specificity = 81%), social anxiety disorder (SAD) (sensitivity = 72%, specificity = 80%) and post-traumatic stress disorder (PTSD) (sensitivity = 66%, specificity = 81%) [49]. A recent psychometric analysis carried out by Conway et al. also supported the reliability and validity of the GAD-7 in cardiac patients [50].
The MINI is a short, structured, diagnostic interview that was developed for DSM-IV and the psychiatric disorders portion of the 10th version of the International Classification of Diseases (ICD-10). It was validated in relation to the SCID-P (Structured Clinical Interview for DSM-III-R Patient Version) and the CIDI (Composite International Diagnostic Interview) [51]. It consists of 120 questions and screens 17 axis I disorders for 24 current and lifetime diagnoses. In this study MINI interview was used to identify current and/or lifetime episodes of major depressive disorder and most common anxiety disorders (generalized anxiety disorder, panic disorder, agoraphobia, social phobia, obsessive-compulsive disorder and post-traumatic stress disorder) [1]. The MINI was previously translated into 67 languages, including Latvian and Russian, according to standard methodology (forward/backward translation and clinician review) [52].
The structured questionnaire contained questions about demographics (age, gender, ethnicity, marital status, employment status, education), the medical reason for a visit to the general practitioner, CV risk factors, history of CVDs, diabetes mellitus and psychiatric disorders, use of CV and psychotropic medications, and days absent from work during last 3 months.
Assessment of CV risk factors was based on recommendations and criteria of the 2012 Joint European Societies’ guidelines on cardiovascular disease prevention [33] and questionnaires of the Finbalt Health Monitor System survey [53]. The following criteria were used for CV risk factors definitions:
-
1.
Family history of premature CVD was defined as a fatal or non-fatal CVD event or/and established diagnosis of CVD in first degree male relatives before 55 years of age or female relatives before 65 years of age.
-
2.
The question about leisure-time physical activity was: “How often do you do physical exercise at leisure lasting at least 30 min. making you at least mildly short of breath or perspire?” It was categorized as follows: 1) Unable to perform; 2) 1 time a week or less; 3) 2–3 times a week; 4) 4–6 times a week; 5) Every day.
-
3.
The variable describing the prevalence of smoking was based on several questions regarding different aspects of smoking (smoking status, smoking history, number of cigarettes, last time smoked). It was categorized as follows: 1) Ever smoked and 2) Never smoked.
-
4.
Alcohol consumption representing episodes of heavy drinking was measured with the following question: “Have you used 5 or more doses of alcohol at once during the last 12 months?” It was dichotomized as follows: 1) Yes and 2) No. Dose of alcohol was defined as equal to 10 mL by volume of 8 g by weight of pure alcohol.
-
5.
The question about the use of fresh vegetables and fruits was: “Do you consume at least 200 g of fresh vegetables or/and fruits per day?” And it was categorized as follows: 1) Yes and 2) No.
-
6.
Consumption of fish was considered as a protective factor if patient responded positively to the following question: “Do you consume fish at least 2 times per week (one of which to be oily fish)?”
Statistical analysis
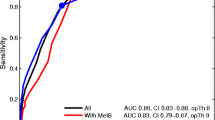
Statistical Package for the Social Sciences (SPSS) version 20.0 (IBM SPSS Corp.) was used for all statistical analyses. Statistical significance was evaluated at the level of p < 0.05. Crude and stratified percentages were used for descriptive statistics. To identify factors associated with the presence of CVDs, univariate and multivariate analyses were carried out. The multivariate model was developed by using binary logistic regression. To avoid multi-collinearity, separate regression models were elaborated for two indicators of depression as independent predictors of CVD- lifetime depressive episode (identified by the MINI interview) and current depressive symptoms (detected through the PHQ-9 instrument). For the final model of multivariate analysis, generalized anxiety disorder (according to the MINI) was chosen, as it gave the best-fitting regression model when compared to other anxiety disorders identified by the MINI or to clinically relevant anxiety symptoms detected by the GAD-7 questionnaire.
Results
Description of the study sample
The mean study response rate was 91.3% (from 1756 approached patients 152 refused to participate), it varied in the range between 86.3–93.7% across 24 primary care facilities all over the country. Those who refused did not significantly differ in the basic socio-demographic characteristics from the rest of the group. In this study, 1604 patients were invited to complete the PHQ-9 and the GAD-7 questionnaires, and 1585 of the approached patients completed both questionnaires. For those who completed both questionnaires, information about the presence of CVD diagnosis was available in 1565 subjects, 489 (31.2%) men and 1076 (68.8%) women, which were included in the final analysis. CVD (angina, myocardial infarction, stroke, transient ischemic attack, chronic cerebrovascular disorder and/or peripheral arterial disease) was detected in 17.1% (n = 268) of the studied population. The prevalence of CVD was slightly higher among men than women, with values of 18.4% and 16.5%, respectively.
One third (31.2%) of the study sample were males, and one third (28.8%) had a university degree. Slightly more than a half (55.8%) of the respondents had reached or exceeded the age of 55 years, and half (51.9%) were employed. One fifth (19.9%) of the study subjects were residing in the capital city, Riga (Table 1).
A positive family history of premature CVD was reported in 38.1% of respondents. At the time of the questionnaire, one third (35.0%) of the study subjects were tobacco smokers, 16.4% had 5 or more drinks of alcohol at least once during the preceding year, one quarter (25.8%) did not include fresh fruits and vegetables in their meals daily, and 60.6% reported that they did not eat fish regularly (i.e., at least twice per week). Daily moderate physical activity was reported by one fifth (20.5%) of individuals. More than two thirds (69.2%) of the patients were overweight according to BMI, and more than half had increased levels of total cholesterol (60.8%). The prevalence of diabetes among the respondents was 9.1%. Systolic or diastolic hypertension were present in 42.6% and 31.1% of patients, respectively. Thus, at the time of the questionnaire, 49.1% of the individuals were taking antihypertensive medications, and 15.2% were taking cholesterol lowering medicines (Table 1).
As shown in Table 1, anxiety disorders (according to the MINI) were identified in 16.1% of patients (8.1% had agoraphobia, 6.1% had generalized anxiety disorder and 0.8% had panic disorder). Anxiety screening (by using the GAD-7 instrument) was positive for one tenth (10.1%) of the study subjects. Current depressive symptoms (PHQ-9 ≥ 10) were present in 14.7% (n = 228) of the individuals. According to the MINI questionnaire, 10.3% (n = 149) had current and 28.1% (n = 407) had lifetime depressive episode. Antidepressants were used by 3.0% of individuals, which could have been for depression or anxiety disorders.
Factors associated with CVD
In the univariate analyses, the factors statistically significantly associated with the presence of CVD (i.e., increasing the odds of CVD) were older age, lower education, economical inactivity, urban place of residence, smoking status, episodes of heavy drinking, being overweight, the presence of diabetes, systolic hypertension, depression and intake of antihypertensive or cholesterol lowering medications (Table 2).
After adjustment, only 6 out of the mentioned 11 factors remained significant predictors of CVD. Older age had one of the strongest associations with the CVD, and it increased the odds approximately five times (p < 0.001). Economic inactivity (including pensioners, disabled persons, housewives, students) doubled the odds of having a CVD (p < 0.001). Residence in the capital city (Riga) increased the risk of CVD approximately nine times (p < 0.001), and living in another urban area increased the odds more than 3 times (p < 0.001) when compared to living in a rural area (Table 2). Individuals who performed moderate physical activity of 30 min once a week or less had decreased odds of having CVD compared to individuals who reported physical activity every day (p = 0.03). Patients who were using antihypertensive or cholesterol lowering medications had three times higher odds of having a CVD (p < 0.001).
The odds ratio (OR) for current depressive symptoms (according to the PHQ-9) was 1.50 (p = 0.046) and for lifetime depressive episode (detected by the MINI) the OR was 2.11 (p = 0.002) (Table 2). The current depressive episode according to the MINI did not show statistically significant results in the univariate analysis or any multivariate model. None of the anxiety measures (MINI and GAD-7) showed statistically significant associations with CVD in either the univariate or the multivariate analyses.
Gender stratified analysis of study population showed that current depressive symptoms (according to the PHQ-9) were associated with 2.04 (p = 0.004) higher odds of having CVD in women, but not in men (data not shown).
Discussion
To the best of our knowledge, this is the first study in Latvia that explores the association between CVD and depression and anxiety in the primary care population. The main findings of this cross-sectional study were that individuals with current depressive symptoms (PHQ-9 ≥ 10) demonstrated 2.08 (95% CI: 1.30–3.32, p = 0.002) times higher odds of having a CVD, and a lifetime depressive episode according to the MINI was associated with an adjusted OR for CVD of 1.52 (95% CI: 1.02–2.25, p = 0.04).
Association of depression and CVDs
An overview of 59 prognostic studies from 3 meta-analyses demonstrated that depression was associated with a 1.5- to 2.7-fold increased risk of incident CVD [24, 54]. A more recent and updated meta-analysis by Gan et al. reviewed 30 prospective studies (n = 893,850) published up to April 2014 with a follow-up duration ranging from 2 to 37 years. They found a more modest association of depression, with CHD and MI reporting pooled RRs of 1.30 (95% CI: 1.22–1.40) and 1.30 (95% CI: 1.18–1.44), respectively [20]. Due to the cross-sectional nature of this study, we are not able to draw conclusions about causality of the established link between depression and CVDs. But our findings in the context of previous research suggest that depression might be a risk factor for increased CV morbidity in Latvian population that has to be investigated in future prospective studies. Although we found a cross-sectional relationship between the current depressive symptoms (PHQ-9 ≥ 10) and lifetime depressive episode according to the MINI, unexpectedly there was no statistically significant association with a diagnosis of current depressive episode detected with the structured psychiatric interview (MINI). Our finding could be explained in two ways. First, 97 individuals of our study population who completed the PHQ-9 questionnaire were not interviewed with the MINI, so this omission could have attenuated the statistical power of the MINI results. Second, the MINI is a categorically based depression assessment tool that could have excluded individuals with sub-syndromal depressive symptoms from case status. On the other hand, the PHQ-9 is a dimensional assessment tool, which could have allowed the inclusion of people with clinically significant depressive symptoms who failed to meet the formal criteria for DSM IV and ICD-10 diagnosis. However, the existing evidence showed that sub-threshold depressive symptoms were significantly associated with increased disability, morbidity and mortality [55]. Therefore, we consider the statistically significant association of the PHQ-9 score ≥ 10 with CVD in the Latvian primary care population as a clinically relevant finding and an easily assessed marker for primary care providers to target.
Evidence about the comorbidity of depression and CVD in other Baltic countries is contradictory. A cross-sectional study in Lithuania involving 317 individuals from primary care centers in 20 cities investigated the association between psychosocial stress, manifested as anxiety and depression, and CVD using the Hospital Anxiety and Depression Scale (screening tool for detection of elevated anxiety and depressive symptoms) [38]. Burokiene et al. demonstrated a modest but significant correlation between CVD and current depressive symptoms (OR = 1.18; 95% CI: 1.07–1.31, p = 0.001) but found no statistically important correlation between current anxiety symptoms and CVD. On the other hand, a cross-sectional study involving 1094 patients from 23 primary care practices across Estonia that explored which co-morbid diseases are associated with depression (using the Depression Section of the Composite International Diagnostic Interview) did not confirm higher co-morbidity of CVD in depressed patients when compared to non-depressed individuals [39].
Specific genetic, behavioral and pathophysiological factors have been established as contributing to the initiation, progression, and clinical manifestation of athero-thrombotic CVD in those suffering from depression and anxiety disorders. Behavioral factors are related to an unhealthy lifestyle (smoking, excessive alcohol consumption, unhealthy diet, sedentary behavior) and poor treatment adherence (medical treatment regimen, maintaining smoking cessation, participation in cardiac rehabilitation) [56,57,58,59,60]. Pathophysiological factors worsening CVD include dysregulation in the autonomic nervous system and hypothalamic-pituitary-adrenal axis as well as metabolic and immuno-inflammatory dysregulations. These pathophysiological factors can lead to coronary vasoconstriction, hypertension, left ventricular hypertrophy, reduced heart rate variability, endothelial dysfunction, platelet activation, hypercoagulability, and the production of pro-inflammatory cytokines (C-reactive protein, interleukin-6, intercellular adhesion molecule-1). These changes elevate the risk of ventricular arrhythmias, MI and stroke [61,62,63]. We examined whether our finding of the association of depression and CVD could be explained by other common traditional and non-traditional CV risk factors, including smoking, exercise, body mass index, and alcohol consumption [22]. In their meta-analysis, Nicholson et al. reported that only half (10 out of 21) of the studies evaluated this range of CV risk factors [22]. In the logistic regression analysis of our study, the association between depressive measures and CVD morbidity remained significant even after adjustment for the traditional CV risk factors.
Association of anxiety and CVDs
In contrast to depression, which in numerous studies has been linked to the increased morbidity and mortality of CVDs, less is known about the influence of anxiety symptoms and anxiety disorders. The most recent meta-analysis, summarizing a total of 37 studies including 1,565,699 participants, demonstrated a 52% increased risk of CVD onset (HR = 1.52, 95% CI: 1.36–1.71) for patients with anxiety symptoms and disorders. This finding seemed to be independent of traditional CV risk factors and depression [28]. The most extensively studied anxiety disorders associated with the onset and progression of CVDs, adverse cardiovascular outcomes, including mortality, are generalized anxiety disorder, panic disorder and post-traumatic stress disorder [64]. Patients with GAD suffer from excessive anxiety and worry, accompanied by somatic anxiety symptoms as well as from restlessness, irritability, difficulty concentrating, muscle tension, sleep disturbances and being easily fatigued. Panic disorder is characterised by recurrent panic attacks, which are discrete periods of intense fear or discomfort, accompanied by various somatic and psychic symptoms. PTSD develops after a terrifying ordeal that involved physical harm or the threat of physical harm and is characterised by recurrent and intrusive distressing recollections of the event, nightmares, dissociative flashback episodes, distress at exposure to cues that resemble the traumatic event, avoidance of stimuli associated with the trauma, estrangement from others, sleep disturbances, irritability, difficulty concentrating, hypervigilance and exaggerated startle response [65, 66]. However, in contrast, some studies reported beneficial effects of anxiety on CV morbidity and mortality [29, 30]. These studies proposed left ventricular function as an important factor that may modulate the prognostic significance of anxiety and may improve risk stratification in CV patients.
We have not found a statistically significant association of GAD (detected by the MINI) with CVD (p = 0.25). This could be explained by the insufficient sample size of our study population. Only 89 individuals corresponded to the MINI diagnostic criteria of GAD. Similarly, a previously mentioned cross-sectional study in the primary care population of Lithuania (n = 317) by Burokiene et al. also reported no significant correlation between anxiety and CVD [38]. There is a need for larger studies with increased numbers of patients conducted in Latvia and the Baltic region to explore the association of anxiety and CVD morbidity with sufficient statistical power.
Association of other CV risk factors and CVDs
Several reports have shown that some well-established CV risk factors, such as tobacco smoking, heavy drinking and sedentary lifestyle [19], may be associated with major depression and anxiety disorders [67,68,69,70]. Although the univariate analysis of our study demonstrated relationships between these risk factors and CVD, after adjustment, only sedentary lifestyle maintained a statistically significant association with CVD. It was found in our study that moderate physical activity once a week or less decreased the odds of CVD when compared to everyday activity. This might be explained by the fact that individuals who are performing physical activity more frequently are more likely to have been detected as having a higher risk for CVD and thus have received a strong recommendation from the primary care physician to practice a health-promoting lifestyle. Our data analysis shows a tendency for some binge drinking episodes within the last 12 months to be preventive in relation to CVD when compared with absence of alcohol abuse. This might be because the population of non-abusers partially consists of people who have stopped their heavy drinking habit due to some cardiovascular health threats. In future studies, it might be prudent to use more sensitive instrument for alcohol consumption that takes into account not only recent but also lifetime habits.
Another new finding was the highest adjusted odds ratio of 8.98 (95% CI: 5.16–15.63, p < 0.001) for individuals living in the urban area of Riga (capital of Latvia) compared to those living in rural areas. This result seems to be consistent with the data obtained in the Prospective Urban Rural Epidemiologic cohort study involving more than 150,000 adults in 17 high-, middle-, and low-income countries [71]. Yusuf et al. (2014) reported that urban communities had a higher CV risk-factor burden than rural communities but had lower rates of CV events and lower case fatality rates. Our study adds to this finding by Yusuf et al. and other similar studies that reported the significance and relevance of considering the place of residence (urban versus rural) as an important moderator and/or confounding factor to include in future studies on CV risks and outcomes [22, 27].
The EUROASPIRE studies have shown that effectiveness of CV risk factors management in the EU is still far from optimal and that major cross-country differences exist [34, 35]. The Baltic countries are among the most profoundly CVD-affected countries with higher CV mortality rates compared to other countries in the EU [10]. Local data are very important to develop country-specific management programs for CV patients [40]. However, previous largest studies on CV risk factors prevalence in Latvian population have not assessed depression and anxiety as possible risk factors [36, 72, 73]. Findings of this study suggest that detection and treatment of depression should be included in CV patients` management programs and future research on CV risk factors in Latvia.
Strengths and limitations
The strengths of this study include the use of a diagnostic interview for the diagnosis of anxiety disorders, a sample that includes persons from a wide range of ages, and a hierarchical multivariate analysis that includes adjustment for anxiety and multiple traditional CV and socio-economic risk factors, including place of residence, which has rarely been used in previous studies. Another strength is that only specially trained psychiatrists were involved in data collection.
The results of this study must be considered in the context of some limitations. Although this is a large, nationally representative primary care convenience sample survey that provides comprehensive data, due to the cross-sectional design of this study, we are not able to draw unequivocal conclusions about the direction of the identified associations between depression or anxiety and CVD morbidity. Second, the PHQ-9 using the standard cut-point of ≥ 10 has been recognized as a reliable tool for detecting depression in chronic somatic conditions, including CVD, and has been found to be even superior to other commonly used screening instruments [43, 44]. However, the PHQ-9 is not a standardized criterion for the diagnosis of depression, which may lead to false positive results. Moreover, there is an ongoing discussion about the optimal PHQ-9 thresholds specific for patients with CVD, with some studies indicating that the PHQ-9 cut-off score of ≥8 or even ≥6 would improve the sensitivity and specificity of this instrument [44, 74]. Further studies are needed to clarify the optimal PHQ-9 threshold for the Latvian CVD population. Third, there is a need for increased numbers of patients to improve the statistical significance of our findings.
Conclusions
We have found a statistically significant association between current depressive symptoms (PHQ-9 ≥ 10) and lifetime depressive episode (according to the MINI) with increased risk of CVD morbidity; however, the same association was not found for anxiety disorders or current anxiety symptoms. Living in an urban area, especially in the capital city, has been established as an important associated factor that was rarely used in previous research. The findings of this study suggest that CV patients should be screened and treated for depression to potentially improve the prognosis of CVD. Enhanced training and integration of mental health treatment in Latvian primary care settings may improve clinical outcomes. Further research with a larger sample size should be undertaken to better assess the effect of anxiety on CVD morbidity and to investigate the optimal PHQ-9 threshold for the Latvian CVD population.
Abbreviations
- CHD:
-
Coronary heart disease
- CI:
-
Confidence interval
- CIDI:
-
Composite International Diagnostic Interview
- CV:
-
Cardiovascular
- CVD:
-
Cardiovascular disease
- DSM-IV:
-
Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition
- EU:
-
European Union
- GAD:
-
Generalized anxiety disorder
GAD-7
Generalized Anxiety Disorder questionnaire, 7
- GP:
-
General practitioner
- HADS:
-
Hospital Anxiety and Depression Scale
- HbA1c:
-
Glycated hemoglobin
- HR:
-
Hazard ratio
- ICD-10:
-
10th version of the International Classification of Diseases
- MDD:
-
Major depression
- MI:
-
Myocardial infarction
- MINI:
-
Mini International Neuropsychiatric Interview
- OCD:
-
Obsessive-compulsive disorder
- OR:
-
Odds ratio
- PAR:
-
Population attributable risk
- PD:
-
Panic disorder
- PHQ-9:
-
Patient Health Questionnaire, 9
- PTSD:
-
Post-traumatic stress disorder
- RR:
-
Relative risk
- SAD:
-
Social anxiety disorder
- SCID-P:
-
Structured Clinical Interview for DSM-III-R Patient Version
- SPSS:
-
Statistical package for the Social Sciences
References
Wittchen HU, Jacobi F, Rehm J, Gustavsson A, Svensson M, Jönsson B, Olesen J, Allgulander C, Alonso J, Faravelli C, et al. The size and burden of mental disorders and other disorders of the brain in Europe 2010. Eur Neuropsychopharmacol. 2011;21(9):655–79.
World Health Organisation: Depression http://www.who.int/mediacentre/factsheets/fs369/en/ (2017). Accessed 30 Apr 2017.
Gili M, Comas A, García-García M, Monzón S, Antoni S-B, Roca M. Comorbidity between common mental disorders and chronic somatic diseases in primary care patients. Gen Hosp Psychiatry. 2010;32(3):240–5.
Roca M, Gili M, Garcia-Garcia M, Salva J, Vives M, Garcia Campayo J, Comas A. Prevalence and comorbidity of common mental disorders in primary care. J Affect Disord. 2009;119(1–3):52–8.
Egede LE. Major depression in individuals with chronic medical disorders: prevalence, correlates and association with health resource utilization, lost productivity and functional disability. Gen Hosp Psychiatry. 2007;29(5):409–16.
Scott KM, Bruffaerts R, Tsang A, Ormel J, Alonso J, Angermeyer MC, Benjet C, Bromet E, de Girolamo G, de Graaf R, et al. Depression-anxiety relationships with chronic physical conditions: results from the world mental health surveys. J Affect Disord. 2007;103(1–3):113–20.
Global Atlas on Cardiovascular Disease Prevention and Control. Geneva: World Health Organisation. http://www.who.int/mediacentre/factsheets/fs317/en/ (2012). Accessed 29 Apr 2017.
The Centre for Disease Prevention and Control of Latvia: The Statistical Yearbook of Health Care in Latvia. https://www.spkc.gov.lv/en/statistics (2015). Accessed 14 Apr 2017.
The Centre for Disease Prevention and Control of Latvia: The Potential years of life lost. https://www.spkc.gov.lv/en/statistics (2015). Accessed 5 Feb 2017.
Eurostat: The Causes of death- diseases of the circulatory system. http://ec.europa.eu/eurostat/statistics-explained/index.php/Causes_of_death_statistics (2013). Accessed 8 Feb 2017.
Rutledge T, Linke SE, Krantz DS, Johnson BD, Bittner V, Eastwood JA, Eteiba W, Pepine CJ, Vaccarino V, Francis J, et al. Comorbid depression and anxiety symptoms as predictors of cardiovascular events: results from the NHLBI-sponsored Women's ischemia syndrome evaluation (WISE) study. Psychosom Med. 2009;71(9):958–64.
Lichtman JH, Froelicher ES, Blumenthal JA, Carney RM, Doering LV, Frasure-Smith N, Freedland KE, Jaffe AS, Leifheit-Limson EC, Sheps DS, et al. Depression as a risk factor for poor prognosis among patients with acute coronary syndrome: systematic review and recommendations: a scientific statement from the American Heart Association. Circulation. 2014;129(12):1350–69.
Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR, Rush AJ, Walters EE, Wang PS. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R). JAMA. 2003;289(23):3095–105.
Hackett ML, Yapa C, Parag V, Anderson CS. Frequency of depression after stroke: a systematic review of observational studies. Stroke. 2005;36(6):1330–40.
Hackett ML, Pickles K. Part I: frequency of depression after stroke: an updated systematic review and meta-analysis of observational studies. Int J of stroke : official J of the Int Stroke Society. 2014;9(8):1017–25.
Lane D, Carroll D, Ring C, Beevers DG, Lip GY. The prevalence and persistence of depression and anxiety following myocardial infarction. Br J Health Psychol. 2002;7(Pt 1):11–21.
Campbell Burton CA, Murray J, Holmes J, Astin F, Greenwood D, Knapp P. Frequency of anxiety after stroke: a systematic review and meta-analysis of observational studies. Int J of stroke : official J of the Int Stroke Society. 2013;8(7):545–59.
Todaro JF, Shen BJ, Raffa SD, Tilkemeier PL, Niaura R. Prevalence of anxiety disorders in men and women with established coronary heart disease. J of cardiopulmonary rehabilitation and prevention. 2007;27(2):86–91.
Piepoli MF, Hoes AW, Agewall S, Albus C, Brotons C, Catapano AL, Cooney MT, Corra U, Cosyns B, Deaton C, et al. 2016 European guidelines on cardiovascular disease prevention in clinical practice: the sixth joint task force of the European Society of Cardiology and Other Societies on cardiovascular disease prevention in clinical practice (constituted by representatives of 10 societies and by invited experts) developed with the special contribution of the European Association for Cardiovascular Prevention & rehabilitation (EACPR). Atherosclerosis. 2016;252:207–74.
Gan Y, Gong Y, Tong X, Sun H, Cong Y, Dong X, Wang Y, Xu X, Yin X, Deng J, et al. Depression and the risk of coronary heart disease: a meta-analysis of prospective cohort studies. BMC psychiatry. 2014;14:371.
Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F, McQueen M, Budaj A, Pais P, Varigos J, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364(9438):937–52.
Nicholson A, Kuper H, Hemingway H. Depression as an aetiologic and prognostic factor in coronary heart disease: a meta-analysis of 6362 events among 146 538 participants in 54 observational studies. Eur Heart J. 2006;27(23):2763–74.
Pan A, Sun Q, Okereke OI, Rexrode KM, Hu FB. Depression and risk of stroke morbidity and mortality: a meta-analysis and systematic review. JAMA. 2011;306(11):1241–9.
Frasure-Smith N, Lesperance F. Depression and cardiac risk: present status and future directions. Heart. 2010;96(3):173–6.
Meijer A, Conradi HJ, Bos EH, Thombs BD, van Melle JP, de Jonge P. Prognostic association of depression following myocardial infarction with mortality and cardiovascular events: a meta-analysis of 25 years of research. Gen Hosp Psychiatry. 2011;33(3):203–16.
Rozanski A, Blumenthal JA, Davidson KW, Saab PG, Kubzansky L. The epidemiology, pathophysiology, and management of psychosocial risk factors in cardiac practice. J Am Coll Cardiol. 2005;45(5):637–51.
Roest AM, Martens EJ, de Jonge P, Denollet J. Anxiety and risk of incident coronary heart disease: a meta-analysis. J Am Coll Cardiol. 2010;56(1):38–46.
Batelaan NM, Seldenrijk A, Bot M, van Balkom AJ, Penninx BW. Anxiety and new onset of cardiovascular disease: critical review and meta-analysis. The British J of psychiatry : the J of mental sci. 2016;208(3):223–31.
Meyer T, Buss U, Herrmann-Lingen C. Role of cardiac disease severity in the predictive value of anxiety for all-cause mortality. Psychosom Med. 2010;72(1):9–15.
Meyer T, Hussein S, Lange HW, Herrmann-Lingen C. Anxiety is associated with a reduction in both mortality and major adverse cardiovascular events five years after coronary stenting. Eur J Prev Cardiol. 2015;22(1):75–82.
Emdin CA, Odutayo A, Wong CX, Tran J, Hsiao AJ, Hunn BHM. Meta-analysis of anxiety as a risk factor for cardiovascular disease. Am J Cardiol. 2016;118(4):511–9.
Ian G, Dan A, Knut B-J, Gudrun B, Gunilla B, Renata C, Jean D, Guy De B, Shah E, Bjørn G, et al. Fourth joint task force of the European Society of Cardiology and Other Societies on cardiovascular disease prevention in clinical practice (constituted by representatives of nine societies and by invited experts). Eur J Cardiovasc Prev Rehabil. 2007;14(2):E1–E40.
Perk J, De Backer G, Gohlke H, Graham I, Reiner Z, Verschuren M, Albus C, Benlian P, Boysen G, Cifkova R, et al. European guidelines on cardiovascular disease prevention in clinical practice (version 2012). The fifth joint task force of the European Society of Cardiology and Other Societies on cardiovascular disease prevention in clinical practice (constituted by representatives of nine societies and by invited experts). Eur Heart J. 2012;33(13):1635–701.
Kotseva K, Wood D, De Backer G, De Bacquer D, Pyorala K, Keil U. EUROASPIRE III: a survey on the lifestyle, risk factors and use of cardioprotective drug therapies in coronary patients from 22 European countries. European J of cardiovascular prevention and rehabilitation : official J of the European Society of Cardiology, Working Groups on Epidemiol and Prevention and Cardiac Rehabilitation and Exercise Physiol. 2009;16(2):121–37.
Kotseva K, De Bacquer D, De Backer G, Ryden L, Jennings C, Gyberg V, Abreu A, Aguiar C, Conde AC, Davletov K, et al. Lifestyle and risk factor management in people at high risk of cardiovascular disease. A report from the European Society of Cardiology European Action on secondary and primary prevention by intervention to reduce events (EUROASPIRE) IV cross-sectional survey in 14 European regions. Eur J Prev Cardiol. 2016;23(18):2007–18.
Erglis A, Dzerve V, Pahomova-Strautina J, Narbute I, Jegere S, Mintale I, Ligere R, Apinis P, Lejnieks A, Misina D, et al. A population-based cross-sectional study of cardiovascular risk factor in Latvia. Med (Kaunas, Lithuania). 2012;48(6):310–6.
Viigimaa M, Erglis A, Latkovskis G, Maeots E, Petrulioniene Z, Slapikas R, Gocentiene A, Bramlage P, Brudi P. Prevalence of dyslipidemia in statin-treated patients in the Baltic states (Estonia, Latvia, and Lithuania): results of the dyslipidemia international study (DYSIS). Med (Kaunas, Lithuania). 2014;50(1):44–53.
Burokienė N, Karčiauskaitė D, Kasiulevičius V, Kučinskas V, Kučinskienė ZA. Manifestation of anxiety and depression and their association with cardiovascular diseases in the Lithuanian population. Acta Medica Lituanica. 2014;21(3):123–30.
Suija K, Kalda R, Maaroos H-I. Patients with depressive disorder, their co-morbidity, visiting rate and disability in relation to self-evaluation of physical and mental health: a cross-sectional study in family practice. BMC Fam Pract. 2009;10:38.
Assari S. Cross-country differences in the additive effects of socioeconomics, health behaviors and medical comorbidities on disability among older adults with heart disease. The J of Tehran University Heart Center. 2015;10(1):24–33.
Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary care evaluation of mental disorders. Patient health questionnaire. JAMA. 1999;282(18):1737–44.
Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–13.
Meader N, Mitchell AJ, Chew-Graham C, Goldberg D, Rizzo M, Bird V, Kessler D, Packham J, Haddad M, Pilling S. Case identification of depression in patients with chronic physical health problems: a diagnostic accuracy meta-analysis of 113 studies. The British J of general practice : the J of the Royal College of General Practitioners. 2011;61(593):e808–20.
Haddad M, Walters P, Phillips R, Tsakok J, Williams P, Mann A, Tylee A. Detecting depression in patients with coronary heart disease: a diagnostic evaluation of the PHQ-9 and HADS-D in primary care, findings from the UPBEAT-UK study. PLoS One. 2013;8(10):e78493.
Rancans E, Vrublevska J, Trapencieris M, Snikere S, Ivanovs R, Logins R, Berze L. P.2.H.016 - validity of patient health questionnaire (PHQ-9) in detecting depression in primary care settings in Latvia – the results of the National Research Project BIOMEDICINE. Eur Neuropsychopharmacol. 2016;26(l):481.
Vrublevska J, Trapencieris M, Rancans E. Adaptation and validation of the patient health Questionnaire-9 to evaluate major depression in a primary care sample in Latvia. Nordic J Of Psychiatry. 2018;72(2):112–8.
Swinson RP. The GAD-7 scale was accurate for diagnosing generalised anxiety disorder. Evidence-based med. 2006;11(6):184.
Spitzer RL, Kroenke K, Williams JB, Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–7.
Kroenke K, Spitzer RL, Williams JB, Monahan PO, Lowe B. Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection. Ann Intern Med. 2007;146(5):317–25.
Conway A, Sheridan J, Maddicks-Law J, Fulbrook P, Ski CF, Thompson DR, Doering LV. Accuracy of anxiety and depression screening tools in heart transplant recipients. Applied nursing research : ANR. 2016;32:177–81.
Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Hergueta T, Baker R, Dunbar GC. The Mini-international neuropsychiatric interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. The J of clin psychiatry. 1998;59(Suppl 20):22–33.
Boudrot A, Sheehan D, Acquadro C. Lost in translation: translatability of psychiatric terms-the example of the Mini-international neuropsychiatric interview (M.I.N.I.). Value Health. 2013;16(7):A599–A599.
Kasmel A, Helasoja V, Lipand A, Prättälä R, Klumbiene J, Pudule I. Association between health behaviour and self-reported health in Estonia, Finland, Latvia and Lithuania. Eur J Pub Health. 2004;14(1):32–6.
Rugulies R. Depression as a predictor for coronary heart disease. A review and meta-analysis. Am J Prev Med. 2002;23(1):51–61.
Meeks TW, Vahia IV, Lavretsky H, Kulkarni G, Jeste DV. A tune in ‘a minor’ can ‘b major’: a review of epidemiology, illness course, and public health implications of subthreshold depression in older adults. J Affect Disord. 2011;129(1–3):126–42.
Goldstein CM, Gathright EC, Garcia S. Relationship between depression and medication adherence in cardiovascular disease: the perfect challenge for the integrated care team. Patient preference and adherence. 2017;11:547–59.
Doyle F, Rohde D, Rutkowska A, Morgan K, Cousins G, McGee H. Systematic review and meta-analysis of the impact of depression on subsequent smoking cessation in patients with coronary heart disease: 1990 to 2013. Psychosom Med. 2014;76(1):44–57.
Swardfager W, Herrmann N, Marzolini S, Saleem M, Farber SB, Kiss A, Oh PI, Lanctot KL. Major depressive disorder predicts completion, adherence, and outcomes in cardiac rehabilitation: a prospective cohort study of 195 patients with coronary artery disease. The J of clin psychiatry. 2011;72(9):1181–8.
Gehi A, Haas D, Pipkin S, Whooley MA. Depression and medication adherence in outpatients with coronary heart disease: findings from the heart and soul study. Arch Intern Med. 2005;165(21):2508–13.
DiMatteo MR, Lepper HS, Croghan TW. Depression is a risk factor for noncompliance with medical treatment: meta-analysis of the effects of anxiety and depression on patient adherence. Arch Intern Med. 2000;160(14):2101–7.
Dhar AK, Barton DA. Depression and the link with cardiovascular disease. Frontiers in psychiatry. 2016;7:33.
Pogosova N, Saner H, Pedersen SS, Cupples ME, McGee H, Hofer S, Doyle F, Schmid JP, von Kanel R. Psychosocial aspects in cardiac rehabilitation: from theory to practice. A position paper from the cardiac rehabilitation section of the European Association of Cardiovascular Prevention and Rehabilitation of the European Society of Cardiology. Eur J Prev Cardiol. 2015;22(10):1290–306.
Penninx BW. Depression and cardiovascular disease: epidemiological evidence on their linking mechanisms. Neurosci Biobehav Rev. 2017;74(Pt B):277–86.
Celano CM, Daunis DJ, Lokko HN, Campbell KA, Huffman JC. Anxiety disorders and cardiovascular disease. Current psychiatry reports. 2016;18(11):101.
APA. Diagnostic and statistical manual of mental disorders, fifth edition (DSM-5). Washington, DC: American Psychiatric Association; 2013.
Bandelow B, Baldwin D, Abelli M, Altamura C, Dell'Osso B, Domschke K, Fineberg NA, Grunblatt E, Jarema M, Maron E, et al. Biological markers for anxiety disorders, OCD and PTSD - a consensus statement. Part I: neuroimaging and genetics. The world J of biol psychiatry: the official J of the World Federation of Societies of Biol Psychiatry. 2016;17(5):321–65.
Khalid A, Kunwar AR, Rajbhandari KC, Sharma VD, Regmi SK. A study of prevalence and comorbidity of depression in alcohol dependence. Indian J Psychiatry. 2000;42(4):434–8.
Ziedonis D, Hitsman B, Beckham JC, Zvolensky M, Adler LE, Audrain-McGovern J, Breslau N, Brown RA, George TP, Williams J, et al. Tobacco use and cessation in psychiatric disorders: National Institute of Mental Health report. Nicotine and Tobacco Research: Official J Of The Society For Research On Nicotine And Tobacco. 2008;10(12):1691–715.
Pacek LR, Storr CL, Mojtabai R, Green KM, La Flair LN, Alvanzo AAH, Cullen BA, Crum RM. Comorbid alcohol dependence and anxiety disorders: a National Survey. J of dual diagnosis. 2013;9(4):271–80.
Figueiredo JHC, NAdSe S, BdB P, GMM d O. Major Depression and Acute Coronary Syndrome-Related Factors. Arq Bras Cardiol. 2017;108(3):217–27.
Yusuf S, Rangarajan S, Teo K, Islam S, Li W, Liu L, Bo J, Lou Q, Lu F, Liu T, et al. Cardiovascular risk and events in 17 low-, middle-, and high-income countries. N Engl J Med. 2014;371(9):818–27.
Kalvelis A, Stukena I, Bahs G, Lejnieks A. Do we correctly assess the risk of cardiovascular disease? Characteristics of risk factors for cardiovascular disease depending on the sex and age of patients in Latvia. European J of Cardiovascular Med. 2011;3:19–23.
Erglis A, Mintale I, Latkovskis G, Balode I, Jegere S, Bajare I, Rozenbergs A, Greenlaw N, Ferrari R, Steg PG. Management of coronary artery disease patients in Latvia compared with practice in Central-Eastern Europe and globally: analysis of the CLARIFY registry. Medicina. 2015;51(4):240–6.
Thombs BD, Ziegelstein RC, Whooley MA. Optimizing detection of major depression among patients with coronary artery disease using the patient health questionnaire: data from the heart and soul study. J Gen Intern Med. 2008;23(12):2014–7.
Acknowledgements
We would like to thank The National Research Program BIOMEDICINE 2014-2017 for the funding of this study and Dr. Liene Berze and Dr. Raivis Logins from the Department of Psychiatry and Narcology at the Riga Stradins University for their substantial contributions to data collection.
Funding
This study was funded by the National Research Program BIOMEDICINE 2014–2017, Ministry of Education and Sciences, Republic of Latvia. The article-processing charge was funded by the Riga Stradins University.
Availability of data and materials
The data that support the findings of this study are available from Prof. Elmars Rancans, e-mail: erancans@latnet.lv, upon reasonable request.
Author information
Authors and Affiliations
Contributions
ER and JV participated in the conception and design of the study. ER coordinated the study. DZ consulted about mental health and tobacco addiction aspects, and IM consulted about cardiological aspects of the study design and data analysis. JV and RI participated in data collection. AK performed the analyses. RI wrote the first draft of the manuscript. All authors participated in the writing and revision of the successive drafts of the manuscript. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Ethics Committee of the Riga Stradins University, Riga, Latvia (No. 8/ 18.06.2015.). The project was conducted in accordance with the Declaration of Helsinki and its subsequent amendments. All patients were enrolled after providing written informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Ivanovs, R., Kivite, A., Ziedonis, D. et al. Association of depression and anxiety with cardiovascular co-morbidity in a primary care population in Latvia: a cross-sectional study. BMC Public Health 18, 328 (2018). https://doi.org/10.1186/s12889-018-5238-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-018-5238-7