Abstract
Background
The positive health impact of physical activity (PA) is well known, yet a large proportion of the world’s population remains sedentary. General PA programs are common as health promotion initiatives. However, effectiveness evaluations of such PA programs on individual and organizational aspects, which could inform the decision-making process of public health bodies are still lacking, particularly in the most socially disadvantaged areas, where health promotion schemes are particularly needed. The aim of this study was to assess the effectiveness of a Guided Walking Program in a high social vulnerability context.
Methods
A quasi-experimental, mixed methods study was conducted. The program had a duration of 6 months and a 6-month follow-up period after the intervention. Session frequency was five times a week, where sessions consisted of supervised PA combined with educational sessions. The Reach, Effectiveness, Adoption, Implementation and Maintenance (RE-AIM) framework was followed to assess the program. The International Physical Activity Questionnaire (IPAQ) and accelerometers were used to measure levels of PA. Focus groups were conducted to gain a comprehensive insight on the implementation domain.
Results
Most subjects in the intervention (IG) (n = 74) and control (CG) (n = 74) groups were female (IG:90.5%; CG:95.9%), aged 18–49 years (IG:44.6%; CG:43.2%), received less than 1 minimum wage (IG:74.3%; CG:83.7%) and had 0–4 years of formal education (IG:52.1%; CG:46.1%). The reach of the intervention was 0.3%. The IG showed increased levels of PA at post-intervention and 6-month follow-up. However, the difference between groups was not statistically significant. Adoption data revealed that 89.5% of the professionals in the Primary Health Care Center (health center) team perceived the benefits of the program for the population. The program was independently promoted by the health center team for a further 4 months post-intervention. The qualitative data revealed that the program was discontinued due to participants’ low adherence and human resource limitations in the unit’s operational dynamics.
Conclusions
A health promotion intervention in a socially deprived setting faces challenges but can be effective and feasible to implement. The present study informs the development of future health promotion initiatives in this context.
Trial registration
NCT02857127. Registered: 30 July 2016 (retrospectively registered).
Similar content being viewed by others
Background
According to the World Health Organization [1], approximately 23.3% of the world population and 32.4% of the American population are physically inactive. An estimated one in every three adults is sedentary, and physical inactivity may increase the risk of death by 20% to 30%. [2, 3]. The cost of physical inactivity to the world’s economy is estimated at $53.8 billion [4,5,6]. In Brazil, the percentage of individuals practicing less than 150 min of moderate PA per week was 47.5% while 16% reported practicing no PA in the past 3 months [7].
Offering physical activity programs can help change this scenario worldwide [8,9,10]. Low-income individuals, higher age groups and females are the groups most vulnerable to becoming physically inactive [11], pointing to the need for greater investment in health promotion interventions in this population.
Disparities among socioeconomically different areas may affect the applicability of PA programs. Environmental factors, lower absolute income, greater population density, lack of safety and accessibility in high social vulnerability areas may all negatively impact the practice of PA [12,13,14]. Therefore, it is essential that the nature of these challenges is well understood and the effectiveness of different approaches for promoting PA is objectively measured.
According to Wierenga [15], the heterogeneity of evaluations of health promotion programs hampers comparison of these initiatives, and poses a major barrier to correlating effectiveness and implementation. Thus, it is important that program implementation and its effectiveness analysis are clearly reported to allow comparison across studies [16]. Moreover, it is relevant to conduct studies exploring external validity of interventions, currently little investigated in the scientific literature [17, 18].
The Reach, Effectiveness, Adoption, Implementation and Maintenance (RE-AIM) framework is a complete, global instrument for identifying individual and organizational characteristics of health interventions [19] and has been widely utilized in international studies [20,21,22,23]. A recent systematic review on the use of RE-AIM identified the need for further studies analyzing other operational aspects in addition to intervention effectiveness [23]. In developing countries, particularly in high social vulnerability areas, few studies have employed the RE-AIM to evaluate health promotion interventions, where greater use of this tool may enable comparison of health promotion programs in different contexts. Results of PA programs assessed with this tool allow proper planning of these interventions and enhancement of methodologies [10, 24]. The aim of this study was to assess a Guided Walking Program (program) in a high social vulnerability context, using the RE-AIM framework.
Methods
A controlled, mixed methods, quasi-experimental study was conducted. Data collection occurred between July 2014 and July 2016 at Primary Health Care Centers (health centers) in the City of São Carlos, São Paulo State, Brazil.
The selected areas for data collection were two regions that had the highest Social Vulnerability Index of the State of Sao Paulo (Paulista Index of Social Vulnerability) [25]. The target-population consisted of individuals registered at five health centers in the two areas selected for the study. The two areas, for intervention (IG) and control (CG) groups, respectively, were geographically distant to minimize the risk of bias.
A total of 195 individuals took part, comprising 88% women, and with a mean age of 47.8 (± 12.7) years. For data analysis, the inclusion criteria for both groups were: 18 years of age or older; able to understand the questions; agreeing to participate in the study; and at the “insufficient PA level” (i.e., practicing less than 150 min of PA per week, as measured by the International Physical Activity Questionnaire) [11]. This project was approved by the Ethics Committee of the Federal University of São Carlos (number 384.852).
Intervention
The intervention was carried out by the health centers in partnership with the researcher team and consisted of five weekly health promotion sessions for 6 months. The health promotion sessions included supervised PA combined with educational initiatives. The PA component consisted of 4 days of a 50-min walk and 10 min of stretching/warm-up, and 1 day of varied exercises such as Zumba, stretching and recreational activities. The intensity of the walk was controlled with a Polar FT1 Heart Rate Monitor and by the colored version of the Borg scale measuring perceived exertion of the participants [26]. Participants were instructed to maintain a moderate and/or vigorous intensity of the PA. All classes were supervised by physical education professionals together with the professionals from the health centers and took place in the vicinity of the centers. As a preventive health procedure, blood pressure was measured every session. The weekly frequency and duration of the activities followed the guidance provided by Garber et al. [27].
The educational initiatives took place immediately after the PA component and included the following: 1) Small interactive activities, debates and/or lectures of 10 to 15 min on alternating weeks, focusing on strategies for behavioural change and incentives to incorporate PA into daily life. 2) Daily health tips for 5 min about important behaviors for a healthier lifestyle when practicing PA, such as drinking fluids, applying sunscreen, and wearing appropriate footwear. Additionally, health topics of interest to the group and health promotion themes proposed by the Brazilian Department of Health calendar [28] were discussed.
Motivation strategies to promote adherence to the program were applied throughout the 6-month intervention. Prizes were awarded to those who missed the least number of sessions every month. Example prizes included fruit baskets and sports accessories such as gym towels and gym bottles. Social relationships were also strengthened by stimulating conversation among the participants during the walking sessions. Phone calls were made to those who missed 3 days in a row without justification.
The CG received no information about physical activity recommendations during the three PA level-related assessments.
Data collection
Data collection for both groups was carried out at three timepoints: prior to the intervention (T0), immediately post-intervention (T1) and after a 6-month follow-up period (T2).
Sociodemographic data, including age, sex, education, as well as individual and family income, were collected at baseline (T0).
The RE-AIM framework was used to assess the intervention. This tool was validated in Brazil by Almeida, Brito and Estabrooks in 2013 [24], and showed satisfactory internal and external validity [17, 19]. The RE-AIM instrument has been widely utilized in the literature [17, 20,21,22,23] and consists of five main components: reach, efficacy, adoption, implementation and maintenance. Each of these components is outlined in greater detail below.
Reach
“Reach” measures the dimension and coverage of the intervention in the community [24]. This component was determined by calculating the proportion of participants on the first day of the program divided by the number of people who possibly became aware of the program through various forms of advertising. This study used the following advertising strategies: health center teams were asked to refer patients; banners were displayed in the neighborhood; a car broadcasting an audio message in the neighborhood; door-to-door distribution of invitations and personal invitations within health center waiting rooms. Social media and a website containing information about the program were also used to promote the program during the 6-month intervention. Most of the streets in the vicinity of the health centers were covered by the advertising strategies.
Efficacy or effectiveness
This component evaluates the individual effectiveness of the intervention [17]. Changes in levels of PA were measured using the International Physical Activity Questionnaire (IPAQ), validated for use in Brazil [29], collecting PA time in minutes per week in the leisure time domain and the sum of all domains (total PA). An accelerometer (Actigraph GT3X) was used to calculate the number of counts per minute per day in an average week. The volunteers wore the device around the waist for 8 consecutive days. The data collected were analysed by the software ActiveLife 6.8 version, employing an epoch of 1 s and the “daily” algorithm. The wear-time required for inclusion was 9 h for at least 4 days a week, including at least one weekend day. The cut-offs proposed by Freedson [30] were used in the Active Life software. Both of these evaluations of PA level were performed at T0, T1 and T2.
Individuals who accomplished less than 150 min of leisure time PA (LTPA) a week on the IPAQ were classified as “insufficiently active”.
Adoption
To analyze organizational involvement in the intervention [24], a five-item questionnaire was applied collecting information on the direct or indirect involvement of all professionals with the IG at the health centers. The questionnaire was left at the centers for 15 days and the professionals were instructed to answer them anonymously and voluntarily.
Implementation
“Implementation” measured the extent to which the project was completed as planned. Two forms of measurement were used to grasp “implementation” both at organizational and individual levels.
A questionnaire containing the essential items of the project was devised. This questionnaire was answered by adherent participants (>80% participation) and those most involved from the health center teams (as perceived by all members involved in the program). The questions collected data on the number of participants in the intervention; the Borg scale and Heart Rate Monitor; blood pressure measurements before the activities; project advertising for 2 weeks; the several forms of advertising (sites, folders, banners, personal invitations, home visits within the community, website); counseling for diabetics; monthly blood glucose measurements; and the offering of educational initiatives.
In addition, a focus group was conducted at the end of the intervention to analyze information on program implementation. A previously trained mediator applied the focus group techniques, forming a small group of participants and professionals with greatest adherence to the program. The mediator did not participate at any time in the program, and was given a checklist about the essential items of the program divided into four dimensions: dissemination, adherence, class protocol and assessments.
Maintenance
To assess this domain on the organizational level, continuity of the program was checked at the health centers. Structural conditions (human and physical resources) contributing to the maintenance of the program were explored in structured interviews. The questions asked were: 1) Did the Project continue after the end of 6-month intervention when the research team withdrew?; 2) If not, what were the main difficulties?
On the individual level, participants’ PA level was analyzed after 6 months of intervention by the IPAQ and the accelerometer using the same methodology applied for the effectiveness domain. Behavioral changes were determined, by comparing these data with T0 and T2, as well as against the CG.
Data analysis
Quantitative data
Descriptive analysis was carried out using absolute and relative frequency measures for categorical variables, and mean, standard deviation and median for numeric variables. Data were analyzed using the Statistical Package for the Social Sciences (SPSS) software, version 22.0. Data normality was verified by the Kolmogorov-Smirnov test. The Chi-square test was used to compare categorical data between the IG and CG. Generalized estimation equations with the inverse Gaussian distribution function were used for non-parametric data. The normal distribution function and the identity link function were used for the PA scores. For the weekly and daily PA variables, the inverse Gaussian distribution function and the identity binding function were used. For these variables, 1 min per week or 1 min per day was added to all values to avoid null values (values must be >0 in an inverse Gaussian distribution). In all cases, an unstructured correlation matrix was used to independently estimate each variance and covariance, while the Huber-White estimator was used to account for the possible heteroskedasticity resulting from the calculation of standard errors. For each outcome, the effect of belonging to a given group, the time elapsed since the beginning of the intervention (T0, T1 and T2), and the interaction of these two factors were estimated to evaluate possible differences in the temporal trends of PA between the groups.
The Bonferroni’ test was used for multiple post-hoc comparisons [31, 32]. A statistically significant difference for values of p < 0.05 was adopted.
Qualitative data
The focus group was formed to analyse the implementation domain. The discourse of all participants in the group was sound recorded and transcribed after previous consent. Subsequently, inferences and interpretations were analyzed by dimension following three steps: data pre-analysis, content exploration and treatment of results [33, 34]. Some key excerpts of discourse were highlighted for reporting in the results.
Results
Sample selection and recruitment
For the IG, a total of 195 users of the health centers participated in the program. Of the total participants, 74 users met the inclusion criteria and agreed to take part in the study. For the CG, 299 registered users of a health center located in another high vulnerability area of the city not part of the project were selected. Of this group, 100 service users met the inclusion criteria. The “not found” for the CG refers to individuals that had moved or for whom the research team did not have access to the new address or who were not found after 3 visits. The CG was matched with the IG for gender and age, giving 74 individuals for inclusion in the CG. Participant losses (Fig. 1) were determined by the imputation method of missing data and intention-to-treat.
Sociodemographic and economic characteristics
Sociodemographic and economic characteristics of the groups were similar (Table 1). Both groups consisted predominantly of women (IG: 90.5%; CG: 95.9%), individuals aged 18 to 49 -years (IG: 44.6%; CG: 43.2%), with more than 4 years of formal education (IG: 61.6%; CG: 77.8%), a family income higher than 1 minimum wage (IG: 83.8%; CG: 70.3%) and an individual income of up to one minimum wage (IG: 73.6%; CG: 83.8%).
RE-AIM dimensions
Reach
The reach of the project was 0.3%. This was calculated as a ratio of the number of participants on the first day of the program (n = 27) to the number of people who most likely heard about the program (n = 7480). This latter number was calculated based on the number of houses on the streets in the vicinity of the health centers and the mean number of residents per household (three).
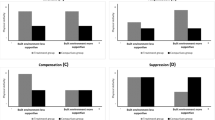
PA level (effectiveness/efficacy and maintenance)
The descriptive analyses of the groups for the three timepoints are depicted in the Box-Plot (Fig. 2). The comparative analyses according to group, timepoint and interaction between group and timepoint are shown in Table 2. A significant difference in Total PA and Counts per minute was found for the group and timepoint interaction (p = 0.032; p = 0.014). Both groups gradually increased PA practice from T0 to T2 in LTPA, Total PA and Counts per minute, with the exception of the CG for LTPA (T0–52.8; 95%CI = 32.6–73.0, T1–73.0; 95%CI = 46.0–99.9; T2–71.3; 95%CI = 53.5–89.2) and the IG for Counts per minute (T0–638.4; 95%CI = 580.5–696.3; T1–693.9; 95%CI = 629.3–758.6; T2–655.4; 95%CI = 591.4–719.3). Despite a decrease in minutes per week between T1 and T2, LTPA remained higher than at baseline (T0).
Adoption
A total of 19 questionnaires were fully completed and analyzed for the “Adoption” domain. This figure represented 59.3% of the professionals working in the health centers involved (Table 3).
The vast majority of responses were positive. Notably, most of the team commented about the program, and all the professionals that answered had referred individuals for the program. Also, the majority of respondents saw the program benefits.
Implementation
The questionnaires were applied to two Community Health Workers and three participants involved in the intervention (Table 4).
It should be noted that, although only a few individuals reported the monitoring of exercise intensity using the colored Borg scale, all remembered using the Heart Rate Monitor, which had the same function.
The focus group found that, regarding the program advertising campaign, the participants reported a range of channels that made them aware of the study: “I heard of it through the internet, on Facebook (…) And the advertising car also passed by.” (Participant 1).
The active participation of health center professionals was also a key element in advertising the program: “What we did was: each professional had their own coverage area to take care of, which involved communicating mainly with individuals such as Participants 2 and 3. So the team went ahead and handed out flyers.” (Community Health Workers 1).
Regarding group adherence to the program, fluctuation in the number of participants was evident (Participant 2: “Some days there are 40, some days there are 30 something.”). The strategies for improving adherence were also noted (Participant 1: "The teacher will also call to find out what happened and the staff will let you know when they are going to be absent."). The target-population was of the age proposed (Participant 3: "A lot older than 20 years.").
As for the class protocol and monitoring measures, several aspects were highlighted including how the classes developed, as well as the materials used. When asked about the pressure blood check, warm-up and stretching, all participants reported these were done every day. The devices used were also highlighted (Participant 3: "That little device here (abdomen) and on the arm too."; Participant 2: “It’s called a pedometer.”). Comments were also made on the devices for maintaining PA intensity and verbal orientations: “They encourage you to push a little. Feeling a little breathless, otherwise it does not work. Just walking around does not work, you have to be panting.” (Participant 1).
The educational initiatives were also highlighted: “At least three times a week there was some sort of orientation. (…) About diseases too. Breast cancer, for men also prostate. They always had these orientation sessions.” (Participant 1).
Finally, for health assessments, the evaluation protocol followed by participants and anthropometric measurements were mentioned (Participant 1: We were weighed, took measurements and had a questionnaire. Also about memory. A very thorough evaluation. And I’ve been through the evaluation again.)
Maintenance (organizational level)
The program was independently promoted by the health center teams for a further 4 months post-intervention. After these 4-months, based on the health professionals´ report, it was decided to suspend the Project due to the increased workload burden and low attendance rate of the sessions, as well as infrastructure and human resource limitations in the centers’ operational dynamics. The professionals also reported a lack of time to execute and lead the Project considering their other operational activities in the health centers. Moreover, the low participant adherence immediately after the 6-month intervention led to demotivation of the health professionals who decided not to continue the activity.
Discussion
The program aim was to promote regular PA in the long term within a socioeconomically deprived context. The program was found to be effective and had adequate involvement of the health center professionals but low adherence post-intervention.
This study was a pioneering investigation in Brazil since previous research has focused on non-deprived areas [35,36,37,38], applied different interventions [35,36,37,38,39] and used other measurement tools [37, 39]. In contrast to the present investigation, previous studies assessed interventions in more generic contexts, involving different target-publics or failed to analyze mixed educational and supervised intervention. Brazilian studies that utilized the same tool as the present study analyzed the university environment or analyzed interventions involving only educational initiatives for behavioral change [35, 40, 41].
Only one quarter of the residents that accepted the invitation to participate in the intervention were considered active, showing a lower PA level than the general Brazilian population [42]. Locations with the highest poverty indexes are considered to be those that have the greatest difficulty accessing health promotions and poor information relative to other regions [43,44,45]. This investigation involved individuals who predominantly had a low educational level, low income, female gender and older age. The elderly are a group more prone to physical inactivity and, thus, in need of more accurate information concerning their health [10, 11]. Thus, the study results are congruent with the goals of policies promoting a more active lifestyle to reduce costs in health services, especially among socially vulnerable individuals [4, 28, 46, 47].
Adherence remained a challenge. Despite wide advertising prior to the beginning of the program, the reach was low, differing from other studies [22, 47, 48]. It is important to emphasize that a large proportion of residents in the area studied worked full-time and travelled to work at the time of the intervention, a factor that could possibly explain the low adherence levels and high number of dropouts from the program. Moreover, the “Reach” domain of the RE-AIM framework is measured on the first day of the intervention [24], which does not reflect the actual number of subjects who underwent the program over time. Future studies should consider this information when applying interventions in disadvantaged areas.
However, positive results were found regarding effectiveness and maintenance. The IG considerably increased PA levels, including during the follow-up period. In terms of public health gains, despite the recommendations of at least 150 min of weekly moderate PA, the increase of at least 10 min of weekly PA for a large percentage of the participants is a highly relevant result, given that the prevalence of physical inactivity and sedentary behavior continues to rise, and the number of insufficiently active or inactive subjects (< 10 min of PA a week) in Brazil remains high [49].
Analysis between groups did not identify statistically significant differences in increased PA levels over time. The study performed three home assessments using a questionnaires on PA level and made three requests to use the accelerometer for a week. These assessments may have encouraged volunteers of the CG to reflect on their health behaviors. Other studies involving interventions for vulnerable groups also showed an increased PA level in the control group, even in randomized interventions [50, 51]. This fact demonstrates a possible “assessment as intervention” effect, evidencing the importance of the population’s participation in scientific studies.
On the organizational level, it was reported that the involvement of health center teams was successful in this context. The level of involvement of professionals in these teams was indeed better than expected, because a large number of these professionals reported experiencing burnout, overload and high demand of administrative activities, which would typically deter them from becoming more involved in group activities directed toward health prevention and promotion [39, 52,53,54]. This result may be attributable to the positive perception reported by the professionals in the focus group regarding the adequate functioning of the program. This must be considered when applying similar studies in the future.
The study also expected to find difficulties for the health centers to continue the program immediately after our team left. However, this problem occurred only after 4 months. Importantly, a lack of resources plus the absence of a specialized professional to apply PA interventions may have affected the continuity of the program [54,55,56]. Furthermore, the low-income population’s understanding about the role of all the professionals involved in primary care and the prevention and promotion of health should be strongly reinforced since the adherence of participants decreased after withdrawal of the research group.
Regarding the implementation domain, despite the structural limitations of the location, in general, the research team was able to accomplish the proposed activities in their work plan. The results were better than those reported in some other health intervention studies that utilized the RE-AIM framework as an evaluation tool [23, 57]. The challenges of rigorously following the application protocols of an intervention occur due to the dynamic process in which this takes place over time.
The non-randomized design, low population adherence, location structural barriers, as well as the high level of dropouts, were considered relevant limitations to the analyses of the present study. Although the sample was selected by convenience, the groups may have had different characteristics, but were similar for sociodemographic characteristics and level of physical activity before starting the program.
Future studies should address these limitations, but continue to measure more than one type of evaluation of the RE-AIM domains to ensure sensitive analysis of all variables. This would generate a greater wealth of details for the discussion and results. For a more thorough intervention assessment, a cost analysis is recommended in order to facilitate applicability of these interventions in practice and enable comparison of cost-effectiveness of different interventions.
Conclusions and implications
We can conclude that the analyses of individual and organizational levels of the program performed using the RE-AIM framework showed positive results of program participation, including the health professionals of the health centers. Therefore, given the challenges faced, such as infrastructure and low-income population behavior characteristics, the program was considered effective.
This study was carried out in a disadvantaged area in Brazil. Despite specific differences in disadvantaged areas in other Brazilian states and poor countries, we believe that low income, low education and poor living conditions are similar among all impoverished areas. Therefore, this study may serve as a model for further studies which should continue to explore the challenges that social vulnerability areas represent in terms of health promotion.
Change history
18 October 2017
A correction to this article has been published.
Abbreviations
- CG:
-
Control group
- IG:
-
Intervention group
- IPAQ:
-
International Physical Activity Questionnaire
- LTPA:
-
Leisure-time physical activity
- PA:
-
Physical activity
References
WHO. Core Indicators: Health Situation in the Americas; 2016. p. 20.
World Health Organization - WHO. Media centre. Physical activity. Available in: <http://www.who.int/mediacentre/factsheets/fs385/en/. Accessed June 2017.
Lee M, Shiroma EJ, Lobelo F, Pekka P, Blair SN, Katzmarzyk PT: Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet 2012, 380:11. https://doi.org/10.1016/S0140-6736(12)61031-9
Turi BC, Codogno JS, Fernandes RA, Monteiro HL: Caminhada e gastos com saúde em adultos usuários do sistema público de saúde brasileiro: estudo transversal retrospectivo. Ciência Saúde Coletiva 2015, 11(20):8. doi: https://doi.org/10.1590/1413-812320152011.00092015.
Bielemann RM, Knuth AG, Hallal PC: Atividade física e redução de custos por doenças crônicas ao Sistema Único de Saúde. Revista Brasileira de Atividade Física & Saúde 2009, 15(1):6.
Ding D, Lawson KD, Kolbe-Alexander TL, Finkelstein EA, Katzmarzyk PT, van Mechelen W, Pratt M, Committee LPASE: The economic burden of physical inactivity: a global analysis of major non-communicable diseases. Lancet 2016, 388(10051):1311–1324. https://doi.org/10.1016/S0140-6736(16)30383-X.
Brasil. Ministério da Saúde. Agência Nacioonal de Saúde Suplementar. Vigilância de fatores de risco e proteção para doenças crônicas por inquérito telefônico - VIGITEL. Brasília. 2015:167.
Knuth AG, Bacchieri G, Victora CG, Hallal PC: Changes in physical activity among Brazilian adults over a 5-year period. J Epidemiol Community Health 2010, 64(7):591–595.
Kohl HW, Craig CL, Lambert EV, Inoue S, Alkandari JR, Leetongin G, Kahlmeier S, Group LPASW: The pandemic of physical inactivity: global action for public health. Lancet 2012, 380(9838):294–305.
Reis RS, Salvo D, Ogilvie D, Lambert EV, Goenka S, Brownson RC, Committee LPASE: Scaling up physical activity interventions worldwide: stepping up to larger and smarter approaches to get people moving. Lancet 2016, 388(10051):1337–1348. https://doi.org/10.1016/S0140-6736(16)30728-0
Hallal PC, Matsudo S, Farias JC: Measurement of physical activity by self-report in low- and middle-income countries: more of the same is not enough. J Phys Act Health 2012, 9 Suppl 1:S88–90.
Silva ICM, Payne VLC, Hino AA, Varela AR, Reis RS, Ekelund U, Hallal PC. Physical Activity and safety from crime among adults: a systematic review. J Phys Act Health, 2016, 13: 663–670. doi: https://doi.org/10.1123/jpah.2015-0156http://dx.doi.org/10.1123/jpah.2015-0156
Sallis JF, Slymen DJ, Conway TL, Frank LD, Saelens BE, Cain K, Chapman JE. Income disparities in perceived neighborhood built and social environment attributes. Health Place. 2011;17(6):1274–83.
Ball K, Carver A, Downing K, Jackson M, O'Rourke K. Addressing the social determinants of inequities in physical activity and sedentary behaviours. Health Promot Int. 2015;30(Suppl 2):18–9.
Wierenga D, Engbers LH, Empelen PV, Duijts S, Hildebrandt VH, Mechelen WV. What is actually measured in process evaluations for worksit health promotion programs: a systematic review. BMC Public Health. 2013;13(1190):16. https://doi.org/10.1186/1471-2458-13-1190.
Jauregui E, Pacheco AM, Soltero EG, O'Connor TM, Castro CM, Estabrooks PA, McNeill LH, Lee RE. Using the RE-AIM framework to evaluate physical activity public health programs in México. BMC Public Health. 2015;15(162):9. https://doi.org/10.1186/s12889-015-1474-2.
Galaviz KI, Harden SM, Smith E, Blackman KC, Berrey LM, Mama SK, Almeida FA, Lee RE, Estabrooks PA. Physical activity promotion in Latin American populations: a systematic review on issues of internal and external validity. Int J Behav Nutr Phys Act. 2014;11:77. https://doi.org/10.1186/1479-5868-11-77.
Hoehner CM, Ribeiro IC, Parra DC, Reis RS, Azevedo MR, Hino AA, Soares J, Hallal PC, Simões EJ, Brownson RC. Physical activity interventions in Latin America: expanding and classifying the evidence. Am J Prev Med. 2013;44(3):e31–40.
Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am J Public Health. 1999;89(9):1322–7.
Olstad DL, Ball K, Abbott G, McNaughton SA, Le HN, Ni Mhurchu C, Pollard C, Crawford DA. A process evaluation of the Supermarket Healthy Eating for Life (SHELf) randomized controlled trial. Int J Behav Nutr Phys Act. 2016;13:27. https://doi.org/10.1186/s12966-016-0352-3.
Zoellner JM, Hedrick VE, You W, Chen Y, Davy BM, Porter KJ, Bailey A, Lane H, Alexander R, Estabrooks PA. Effects of a behavioral and health literacy intervention to reduce sugar-sweetened beverages: a randomized-controlled trial. Int J Behav Nutr Phys Act. 2016;13:38. https://doi.org/10.1186/s12966-016-0362-1.
Caperchione CM, Duncan M, Kolt GS, Vandelanotte C, Rosenkranz RR, Maeder A, Noakes M, Karunanithi M, Mummery WK. Examining an Australian physical activity and nutrition intervention using RE-AIM. Health Promot Int. 2016;31(2):450–8. https://doi.org/10.1093/heapro/dav005.
Harden SM, Gaglio B, Shoup JA, Kinney KA, Johnson SB, Brito F, Blackman KC, Zoellner JM, Hill JL, Almeida FA, et al. Fidelity to and comparative results across behavioral interventions evaluated through the RE-AIM framework: a systematic review. Syst Rev. 2015;4:155. https://doi.org/10.1186/s13643-015-0141-0.
Almeida FA, Brito FA, Estabrooks PA. Modelo RE-AIM: Tradução e Adaptação cultural para o Brasil. REFACS. 2013;1(1):10.
São Paulo: Índice Paulista de Vulnerabilidade Social. In. Edited by Paulo ALdEdS. São Paulo: Fundação SEADE; 2010: 20.
Serafim THS, Nakamura PM, Pereira G, Nakamura FY, Kokubun E. Development of the color scale of perceived exertion: preliminary validation. Percept Mot Skills. 2014;118(3):884–900. https://doi.org/10.2466/27.06.PMS.119c28z5.
Garber CE, Blissmer B, Deschenes MR, Franklin BA, Lamonte MJ, Lee IM, Nieman DC, Swain DP, Medicine ACoS. American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc. 2011;43(7):1334–59.
BRASIL. Ministério da Saúde. Calendário da Saúde. Brasília, 2014. Avaliable in: <http://portalsaude.saude.gov.br/index.php/cidadao/comunicacao/leia-mais-comunicacao/136-chamada-eventos>. Accessed 15 Jul 2014.
Matsudo S, Araujo T, Matsudo V, Andrade D, Andrade E, Oliveira LC, Braggion G. Questionário Internacional de Atividade Física (IPAQ): estudo de validade e reprodutibilidade no Brasil. Rev Bras Ativ Fís Saúde. 2001;6(2):5–12.
Freedson OS, Melanson E, Sirard J. Calibration of the computer science and applications. Ins accelerometer Med Sci Sports Exer. 1998;30(5):77781. https://doi.org/10.1097/00005768-199805000-00021
Ziegler A, Vens M. Generalized estimating equations. Handook of Epidemiology Springer. 2014; https://doi.org/10.1007/978-1-4614-0499-6.
Costa EF, Andrade DR, Garcia LMT, Ribeiro EHC, Santos TI, Florindo AA. Avaliação da efetividade da promoção da atividade física por agentes comunitários de saúde em visitas domiciliares. Cad Saúde Pública. 2015;31(10):2185–98. DOI https://doi.org/10.1590/0102-311X00106014
Bardin L. Análise de Conteúdo. São Paulo, Edeições. 2011;70 229p
Minayo MCS. O desafio do conhecimento: pesquisa qualitativa em saúde. Hucitec. 2010;12:407.
Benedetti TRB, Schwingel A, Gomez LSR, Chodzko-Zajko W. Programa “VAMOS” (Vida Ativa Melhorando a Saúde): da concepção aos primeiros resultados. Rev Bras Cineantropom Desempenho Hum. 2012;14(6):14. https://doi.org/10.5007/1980-0037.2012v14n6p723.
Banos RM, Mensorio MS, Cebolla A, Rodilla E, Palomar G, Lisón JF, Botella C. An internet-based self-administered intervention for promoting healthy habits and weight loss in hypertensive people who are overweight or obese: a randomized controlled trial. BMC Cardiaovascular Disorders. 2015;15:83. https://doi.org/10.1186/s12872-015-0078-1.
Simões EJ, Hallal PC, Siqueira FV, Schmaltz C, Menor D, Malta DC, Duarte H, Hino AA, Mielke GI, Pratt M. Effectiveness of a scaled up physical activity intervention in Brazil: A natural experiment. Prev Med. 2016;7 doi: https://doi.org/10.1016/j.ypmed.2016.09.032
Ueno DT, Gobbi S, Teixeira CVL, Sebastião É, Prado AKG, Costa JLR, Gobbi LTB. Efeitos de três modalidades de atividade física na capacidade funcional de idosos. Rev Bras Educ Fís Esporte. 2012;26(2):8.
Costa EF, Andrade DR, Garcia LM, Ribeiro EH, Santos TI, Florindo AA. Evaluation of the effectiveness of home-based physical activity promotion by community health workers. Cad Saude Publica. 2015;31(10):2185–98. https://doi.org/10.1590/0102-311X00106014.
Sandreschi PF, Petreça DR, Mazo GZ. Avaliação de um programa universitário de atividade física para idosos pelo modelo RE-AIM. Rev Bras Ativ Fís Saúde. 2015;20(3):11. http://dx.doi.org/10.12820/rbafs.v.20n3p270.
Squarcini CFR, Rocha SV, Munaro HLR, Benedetti TRB, Almeida FA. Physical activity programs for elderly persons: an evaluation of Brazilian scientific production using the RE-AIM framework. Rev Bras Geriatr Gerontol. 2015;18(4):11. https://doi.org/10.1590/1809-9823.2015.14103.
BRASIL: Agência Nacional de Saúde Suplementar. Vigilância de fatores de risco e proteção para doenças crônicas por inquérito telefônico. Brasília: Ministério da Saúde; 2015.
Bonevski B, Randell M, Paul C, Chapman K, Twyman L, Bryant J, Brozek I, Hughes C. Reaching the hard-to-reach: a systematic review of strategies for improving health and medical research with socially disadvantaged groups. BMC Med Res Methodol. 2014;14:42.
Cambota JN, Rocha FF. Determinantes das desigualdades na utilização de serviços de saúde: análise para o Brasil e regiões. Pesquisa e Planejamento Econômico. 2015;45(2):26.
Assis MMA, Jesus WLA. Acesso aos serviços de saúde: abordagens, conceitos, políticas e modelo de análise. Ciência & Saúde Coletiva. 2012;11(17):10.
BRASIL. Secretaria de Vigilância em Saúde. Política Nacional de Promoção da Saúde. Portaria n° 687 MS/GM, de 30 de março de 2006. Brasília: Ministério da Saúde; 2006. p. 60.
World Health Organization (WHO). World report on Ageing and Health; 2015. p. 260. Avaliable in: http://apps.who.int/iris/bitstream/10665/186463/1/9789240694811_eng.pdf. Accessed June 2017.
Salvador EP, Ribeiro EH, Andrade DR, Florindo AA. Descrição metodológica da seleção de participants em uma intervenção para a promoção da atividade física pela Estratégia de Saúde da Família. Rev Bras Ativ Fis e Saúde. 2012;17(4):6.
Madeira MC, Siqueira FC, Facchini LA, Silveira DS, Tomasi E, Thumé E, Silva SM, Dilélio A, Piccini RX. Physical activity during commuting by adults and elderly in Brazil: prevalence and associated factors. Cad Saude Publica. 2013;29(1):165–74.
Blackford K, Jancey J, Lee AH, James A, Howat P, Waddell T. Effects of a home-based intervention on diet and physical activity behaviours for rural adults with or at risk of metabolic syndrome: a randomised controlled trial. Int J Behav Nutr Phys Act. 2016;13:13. https://doi.org/10.1186/s12966-016-0337-2.
Luten KA, Reijneveld SA, Dijkstra A, de Winter AF. Reach and effectiveness of an integrated community-based intervention on physical activity and healthy eating of older adults in a socioeconomically disadvantaged community. Health Educ Res. 2016;31(1):98–106.
Borges RA. Programas de promoção de atividade física no SUS: barreiras e facilitadores organizacionais. Florianópolis: Universidade Federal de Santa Catarina; 2014.
Ramos LR, Malta DC, Gomes GA, Bracco MM, Florindo AA, Mielke GI, Parra DC, Lobelo F, Simoes EJ, Hallal PC. Prevalence of health promotion programs in primary health care units in Brazil. Rev Saude Publica. 2014;48(5):837–44.
Maissiat GS, Lautert L, Pai DD, Tavares JP. Contexto de trabalho, prazer e sofrimento na Atenção Básica em saúde. Rev Gaúcha Enferm. 2015;36(2):7.
Gomes GA, Kokubun E, Mieke GI, Ramos LR, Pratt M, Parra DC, Simões E, Florindo AA, Bracco M, Cruz D, et al. Characteristics of physical activity programs in the Brazilian primary health care system. Cad Saude Publica. 2014;30(10):2155–68.
Peres CRFB, Caldas Júnior AL, Silva RF, Marin MJS. O Agente Comunitário de Saúde frente ao processo de trabalho em equipe: facilidades e dificuldades. Rev Esc Enferm USP. 2011;45(4):6.
Ory MG, Altpeter M, Belza B, Helduser J, Zhang C, Smith ML. Perceptions about community applications of RE-AIM in the promotion of evidence-based programs for older adults. Eval Health Prof. 2015;38(1):15–20. https://doi.org/10.3389/fpubh.2014.00143.
Acknowledgements
This paper had the support of the São Carlos Health Department. All the authors would like to acknowledge the contributions of Evelyn Helena Corgosinho Ribeiro and Emanuel Péricles Salvador.
Funding
This study was financed by the Sao Paulo Research Foundation - FAPESP (grant. Alex Antonio Florindo receives a fellowship from the Brazilian National Council for Scientific and Technological Development (CNPq) (grant 306635/2016–0).
Availability of data and materials
The datasets generated and/or analyzed during the current study are not publicly available due to:
- Advertising and educational initiatives: these materials were developed for the specific characteristics of the locale.
- Database: the Ethics Committee requires that the database remain anonymous.
However, the materials are available from the corresponding author upon request.
Author information
Authors and Affiliations
Contributions
CT: participated in the intervention, collected and interpreted data; IM, AE, LM, NC participated in the intervention and the data collection; AA: analyzed data and reviewed the paper; GA: supervised the intervention, analyzed and interpreted the data. All authors participated in the writing, editing, reading and reviewing of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This project was approved by the Ethics Committee of the Federal University of São Carlos (number 384.852). All participants signed a consent form allowing the collection and publication of data.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional information
A correction to this article is available online at https://doi.org/10.1186/s12889-017-4826-2.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Baba, C.T., Oliveira, I.M., Silva, A.E.F. et al. Evaluating the impact of a walking program in a disadvantaged area: using the RE-AIM framework by mixed methods. BMC Public Health 17, 709 (2017). https://doi.org/10.1186/s12889-017-4698-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-017-4698-5