Abstract
Background
Many adults are insufficiently physically active, have prolonged sedentary behaviour and report poor sleep. These behaviours can be improved by interventions that include education, goal setting, self-monitoring, and feedback strategies. Few interventions have explicitly targeted these behaviours simultaneously or examined the relative efficacy of different self-monitoring methods.
Methods/Design
This study aims to compare the efficacy of two self-monitoring methods in an app-based multi-behaviour intervention to improve objectively measured physical activity, sedentary, and sleep behaviours, in a 9 week 2–arm randomised trial. Participants will be adults (n = 64) who report being physically inactive, sitting >8 h/day and frequent insufficient sleep (≥14 days out of last 30). The “Balanced” intervention is delivered via a smartphone ‘app’, and includes education materials (guidelines, strategies to promote change in behaviour), goal setting, self-monitoring and feedback support. Participants will be randomly allocated to either a device-entered or user-entered self-monitoring method. The device-entered group will be provided with a activity tracker to self-monitor behaviours. The user-entered group will recall and manually record behaviours. Assessments will be conducted at 0, 3, 6, and 9 weeks. Physical activity, sedentary behaviour and sleep-wake behaviours will be measured using the wrist worn Geneactiv accelerometer. Linear mixed models will be used to examine differences between groups and over time using an alpha of 0.01.
Discussion
This study will evaluate an app-based multi-behavioural intervention to improve physical activity, sedentary behaviour and sleep; and the relative efficacy of two different approaches to self-monitoring these behaviours. Outcomes will provide information to inform future interventions and self-monitoring targeting these behaviours.
Trial registration
ACTRN12615000182594 (Australian New Zealand Clinical Trials Registry. Registry URL: www.anzctr.org.au; registered prospectively on 25 February 2015).
Similar content being viewed by others
Background
Physical activity and sleep are important for the promotion of health and well-being [1–3]. Insufficient moderate-to-vigorous intensity physical activity, prolonged sedentary behaviour, and poor sleep behaviours - sleeping either too few/many hours or having poor quality sleep – increase the risk of cardiovascular disease (CVD), type 2 diabetes, poor quality of life, anxiety, depressive symptoms, and all-cause mortality [2–7]. Internationally, considerable proportions of the adult population report engaging in one or more of these health compromising behaviours [8–13].
Although multi-behaviour change interventions are frequently conducted, few explicitly target improvements in physical activity, sedentary and sleep behaviours [14–16]. There is good rationale to target these behaviours simultaneously, as they are thought to share a reciprocal relationship. Greater activity levels are thought to improve sleep quality, and better sleep quality can contribute to higher levels of moderate-to-vigorous intensity physical activity and total daily activity [17–20]. In addition, these reciprocal relationships may be enhanced through co-action - a mechanism in multi-behaviour change interventions where change in one behaviour can lead to change, either intentionally or unintentionally, in subsequent behaviours [21]. To maximise change in multi-behaviour interventions it is necessary to provide participants with dedicated behaviour change techniques specific to the targeted behaviours such as goal setting, self-monitoring, and feedback on performance [22–24]. There is substantial evidence that self-monitoring improves a number of health behaviours [25, 26]. Self-monitoring involves individuals tracking behaviour, evaluating progress towards a pre-determined standard, and being aware of the factors that inhibit or facilitate progress [23, 24, 27]. Physical activity, sedentary and sleep behaviours can be manually self-monitored by individuals recalling key aspects of the behaviour (e.g., duration of activity or sleep, time to sleep, time to wake) and recording this information into a paper or electronic diary [28–32]. However, this is vulnerable to social desirability and recall bias, and can have high participant burden [33]. Previous interventions have included devices such as pedometers to partially overcome these limitations by asking participants to enter pedometer steps into the intervention platform [33]. Self-monitoring can also now be automated. This can be achieved by using newly available activity trackers (eg. Fitbit) that also allow physical activity, sedentary and sleep behaviours to be self-monitored and automatically synchronised to mobile devices, which can display feedback on behaviour [25, 34]. However, these devices may increase costs of intervention, present additional technical barriers (e.g. synchronising data across multiple platforms) and the also lower some of the cognitive processing associated self-monitoring which is a key part of self-monitoring [27]. The impact of this on the efficacy of self-monitoring interventions is unknown.
Technology-based interventions such as those delivered by websites and smartphone applications ‘apps’ are increasingly used due to the large potential reach they offer, increased access, including the ability to overcome the need to attend face to face sessions to receive the intervention [35–37]. Technology-based interventions can integrate key behaviour strategies, including self-monitoring and feedback, and to date have been successful in improving a variety of health behaviours over shorter time periods (<12 weeks) [26, 36, 37]. Participant usage of and engagement with the intervention platform is frequently examined and appears to be related to intervention efficacy [26, 36, 38]. Though many technology-based interventions observe large declines in usage and engagement during the first four weeks of the intervention period and do not assess behaviour until much later (e.g., week 12) [28, 38, 39]. Examining behaviour change during time periods when usage and engagement frequently declines may provide greater insight on this relationship and improve subsequent interventions.
The primary aim of this study is to compare the efficacy of device-entered and user-entered self-monitoring methods in a app-based multi-behaviour intervention to improve objectively measured physical activity, sedentary, and sleep behaviours, in a 9 week 2-arm randomised trial. Secondary outcomes will include self-reported physical activity, sitting time, sleep quality, sleep hygiene, anxiety, depression, stress, quality of life and cardiometabolic risk. Potential mediators include psychosocial correlates of behaviours and intervention usage and engagement. Process measures will be collected at the conclusion of the 9 week intervention period and will include reasons for participating in the study, expectations of the study, perceived aesthetics, functionality and appropriateness of the intervention platform, and suggested modifications to the intervention.
Methods
Trial design
The Balanced study is a two-arm randomised trial over 9 weeks. The intervention groups are:
-
1)
Balanced intervention with device-entered self-monitoring method,
-
2)
Balanced intervention with user-entered self-monitoring method.
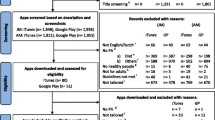
All participants will have access to the same smartphone-based Balanced intervention only the method of self-monitoring is different. Participants in the device-entered self-monitoring group will be provided with a wrist-worn activity tracker to automatically measure and upload physical activity, sedentary and sleep behaviour data. Participants in the user-entered self-monitoring group will recall and manually enter information on physical activity, sedentary and sleep behaviours. Participants will complete assessments at 0, 3, 6, and 9 weeks (Fig. 1). The study received approval from the Human Research Ethics Committee of The University of Newcastle, Australia (Reference Number H-2014-0336) and is registered with the Australian and New Zealand Clinical Trials Registry (ACTRN12615000182594). All participants provided informed consent to participate and could withdraw at any time for any reason. The funding body had no role in the design, conduct or reporting of the trial.
Participant recruitment
Sixty-four participants will be recruited from the Newcastle area, New South Wales, Australia using posters distributed at The University of Newcastle Callaghan campus, local businesses, community notice boards (both physical and electronically), community events; and study advertisements via radio, electronic communication (email lists, social media), and participant registries. Recruitment commenced in July 2015. Individuals interested in participating in the trial will be directed to an online screening survey to assess eligibility. Those who meet the inclusion criteria will be contacted by project staff via phone or email to arrange an appointment time. Ineligible participants will be contacted via phone or email to advise them they are ineligible and offered access to the Balanced app.
Eligibility
To be eligible for inclusion into the study, individuals must report:
-
1.
Being aged between 18 and 55 years,
-
2.
Weight and height consistent with a Body Mass Index (BMI) between 18.5 and 35.0,
-
3.
Engaging in less than 30 min of moderate to vigorous intensity physical activity on 5 days per week which is comparable with recommendations [40],
-
4.
Spending at least 8 h per day sitting on 5 or more days per week, which is comparable with research identifying risk levels of mortality and chronic disease above this level [41, 42],
-
5.
Waking up feeling like they needed more rest/sleep on 14 or more days per month, which is comparable with research identifying higher risk of chronic disease above this level [4],
-
6.
Absence of any condition that makes it unsafe for them to change their activity, sitting and sleep behaviours,
-
7.
Absence of an existing sleep disorder such as insomnia, sleep apnoea, restless legs syndrome,
-
8.
Not being employed in shift work,
-
9.
Not taking any medications to induce sleep,
-
10.
Not travelling to any destination requiring a change in time zone of more than 3 h during the intervention period.
-
11.
Not currently using an app or activity tracker to track physical activity, sedentary or sleep behaviours.
-
12.
Having access to either an Android or iOS smartphone or tablet with access to the internet.
Study procedure
Eligible participants will be asked to attend the University of Newcastle on eight occasions to complete four assessments (2 visits required per assessment). Table 1 provides an overview of the assessments conducted at each visit. Visits 3, 5 and 7 occur 3, 6 and 9 weeks after visit 2. At visits 1, 3, 5, and 7 participants will be provided with an accelerometer to wear continuously for 7 days and return the accelerometer 8 days later visits 2, 4, 6 and 8 respectively, no other assessments occur at visits 1, 3, 5 and 7.
The research assistant performing height, weight, waist circumference and blood pressure measures received training to perform these measures and will be blinded to participant group allocation. Participants will also be provided with a gift voucher to the value of $10 at the completion of each of assessments in visits 2, 4, 6, and 8. Following completion of measurements during visit 2 participants will be randomised to one of the intervention groups and provided with access to the “Balanced” app; participants allocated to the Device-entered self-monitoring group will be provided with a Fitbit (Charge HR) activity tracker.
Intervention
“Balanced” is multi-behavioural intervention to increase time spent being physically active, decrease sedentary time and improve sleep quality. Intervention strategies include the provision of educational materials (e.g. health benefits of target behaviours, National guidelines on each behaviour, behaviour change strategies, creating action plans, sleep hygiene), goal setting and daily self-monitoring. Participants were not required to use the app for any specified time period however were instructed that it was designed for daily monitoring of behaviour and that they could use it as little or as much as they preferred. No prompts were provided to use or engage with the intervention. The intervention is able to be continuously accessed throughout the intervention and assessment periods and is accessible through a specifically designed mobile device app, available on both Android and iOS operating systems. The usability of the platform has been previously evaluated using a think aloud methodology similar to other research [43].
The development of the intervention platform was guided by operationalising constructs from social cognitive and self-regulatory theories (e.g., education, goal setting, self-monitoring, feedback on behaviour) which are consistently identified as important drivers of behaviour change [44–47]. The intervention platform has five sections as detailed below consistent to both intervention groups: 1) Dashboard, 2) Your Stats 3) Progress, 4) Resources and 5) My Profile.
Dashboard
The Dashboard section (Fig. 2) uses a traffic light system to provide participants with a visual representation of their progress toward achieving a predetermined standard level of each behaviour. These levels were selected based on guidelines or available evidence on the lowest risk of overall mortality or cardiovascular disease [1, 2, 48]. The traffic light colours change when the information entered in the Your Stats section is updated (user-entered group) or when the Fitbit is synchronised (device-entered group). Green reflects that a user’s behaviour meets or exceeds the predetermined standard. Orange reflects that a user’s behaviour somewhat lowers their risk, however more positive changes are needed. Red reflects that a participant’s behaviour is markedly below the predetermined standard and associated with significant health risk. The dashboard is intended to operationalise the construct of feedback on behaviour.
Your stats
The Your Stats section (Fig. 3) allows participants to see time spent in moderate-to-vigorous intensity physical activity, time spent sedentary, time to sleep and time to wake, and sleep quality. The user-entered group used this section to enter data on each of these behaviours. In this section, participants can enter goals for all behaviours except sleep quality because individuals can engage in activities that can promote improved sleep quality (eg. sleep hygiene behaviours), but sleep quality is not directly under their control. Participants may also enter a subjective rating to indicate whether they believe their current behaviour is a risk to their health, using a dichotomous yes or no response format, in this section. This seeks to engage participants in evaluation of their behaviour, in relation to the information provided in the resources section and feedback provided by the traffic light system. It is intended to align their perceptions of their behaviour with their actual level of behaviour, as many people are likely to have misaligned perceptions of their lifestyle behaviours [49, 50]. The information entered in this section is intended to operationalise the constructs of goals setting and self-monitoring.
Progress
The Progress section provides graphical feedback of behaviours in comparison to goals on duration of physical activity, sedentary behaviour and sleep, sleep quality, and the pattern of sleep (time to sleep and time to wake), using four time periods: daily, weekly, 3 month, and total usage period. The device-entered group are provided with graphs displaying summaries of the number of minutes spent in moderate-to-vigorous intensity physical activity, and in sedentary behaviour, in 15 min periods (See Fig. 4a). The manual-entered group receives daily summaries for these behaviours in the form of a single bar graph (See Fig. 4b). The sleep pattern graph shows the time to bed and time to wake, as consistency in these times is a key behavioural target for improving sleep quality (Fig. 4c) [12, 51, 52].
Resources
The Resources section provides information on the benefits of, and barriers to improving targeted health behaviours, and details of the criteria used to determine colours in the Traffic Light system on the Dashboard. Strategies to improve behaviours were adapted from our previous interventions and existing resources (i.e. National Guidelines, National Heart Foundation, Sleep Health Foundation), including goal setting strategies [28, 40, 51, 53, 54]. Sleep education materials will include sleep hygiene education information based on existing information [51, 53]. Education materials will promote the formation of habits around target behaviours (i.e. scheduling activities, creating routines around behaviours) to engrain behaviours in daily life and promote longer term changes [55]. These materials use an approach similar to that used in previous interventions, by providing concise information on each behaviour in a “Why”, “How”, and “How much” format [28]. The resources section is intended to operationalise the behaviour change techniques of education and action planning.
My Profile
The My Profile section allowed participants to alter their email address, change their password and provided a description of the research team.
Device-entered self-monitoring
Participants in the device-entered group will self-monitor physical activity, sedentary and sleep behaviour using data from the Fitbit. The Fitbit measures these behaviours and automatically synchronises with the Balanced platform using the Fitbit Application Programming Interface (API) (See Fig. 5) to display information on these behaviours in the Balanced platform. Participants will not be required to interact with the Fitbit website or app in anyway, furthermore they will be asked not to use these throughout the intervention. In the device-entered group, activity and sedentary behaviour are measured using steps per minute criteria of >100 steps and zero steps per minute respectively [56–58]. Time to sleep, time to wake and sleep quality (derived from the ratio of sleep duration/time between time to sleep and time to wake) will be derived from the Fitbit data. Sleep quality is subsequently classified into a 5 point scale where 1 is lower sleep quality and 5 is higher sleep quality [59].
User-entered self-monitoring
Participants in the user-entered group will self-monitor physical activity, sedentary, and sleep behaviour by manually entering this into the intervention platform using the My Stats section (Fig. 3). The user-entered group will be asked to self-monitor time spent in moderate-to-vigorous intensity physical activity, which is defined based on increases in breathing and heart rates and increased difficulty to carry a conversation and talk. The user-entered group will be asked to self-monitor their sedentary behaviour based on time spent sitting. The user-entered group will be asked to enter the time they went to sleep and woke up, and to self-monitor sleep quality using a 5 point scale from 1 (lowest quality) to 5 (highest quality) based on their perceived quality of their sleep.
Randomisation
Participants will be randomised to one of the two intervention groups by a researcher not involved in participant assessments, after completion of their baseline assessment (Visit 2). The randomisation sequence will be generated using a computer-based random number generator using blocks of 4 and 6 [60]. The sequence will be generated by a researcher not involved in participant assessments and will be stored on a central database not accessible to those completing the assessments. Group allocations will be concealed in sequentially numbered opaque envelopes.
Outcome measures
Primary outcome
Activity, sedentary and sleep behaviour
The Geneactiv is a small (36 × 30 × 12 mm, 16 g) waterproof accelerometer which has been shown to provide valid estimates of physical activity, sedentary and sleep behaviours [61, 62]. Participants will be asked to wear the Geneactiv activity monitor 24 h per day for 7 days on their non-dominant wrist and complete a written monitoring log to record the time of day that they go to bed, wake up, arrive at and leave work (if employed) and if the monitor was removed for any reason. Throughout the assessment period participants will receive text message reminders to wear the activity monitor approximately every 3 days.
The monitors will be set to collect data at 40-Hz. For data to be included in the analyses, a minimum of 5 days wear time, with at least 16 h wear per day will be required [63]. Daily time spent in sedentary, light and moderate-to-vigorous intensity physical activity (MVPA) will be determined using the Geneactiv data and the acceleration intensity thresholds developed by Hildebrand et al. [62]. In addition, the duration of specific activity types representing sedentary behaviour (i.e. sitting, standing stationary) and moderate-to-vigorous intensity physical activity (i.e. brisk walking, running) during waking hours will be quantified using the Random Forest activity classifier developed by Pavey and colleagues [64]. Geneactiv data will be used in combination with log data on time to bed and time to wake, to provide Geneactiv derived estimates of sleep onset and offset each day, sleep duration, and nightly awakenings using the R-package “GGIR” [61]. The ratio of sleep duration and time between sleep onset and offset will be used as an indicator of sleep efficiency. The within-participant standard deviation in sleep onset and offset will be calculated to provide a measure of variation in sleep-wake behaviour [65]. The primary outcomes of daily minutes of moderate and vigorous intensity physical activity, sedentary behaviour, sleep efficiency and sleep-wake variability will be averaged across days that satisfy minimum wear time criteria.
Secondary outcomes
Self-reported physical activity, sitting, sleep
Self-report measures of physical activity, sitting and sleep are collected for several reasons including in the event that compliance with the accelerometer protocol is low or device malfunction. Self-reported sitting time can provide insight the domain of sitting that changes occur in and many sleep interventions report changes in self-reported sleep quality allowing comparison to these studies. The Active Australia survey will be used to assess the frequency and duration of self-reported walking for recreation and transport (combined), moderate and vigorous intensity physical activity over the last week. It has demonstrated acceptable levels of test-retest reliability (k = 0.50) and validity (k = 0.26–0.46) in population based surveys and is sensitive to detecting changes in physical activity in interventions [66–68].
The Workforce Sitting Questionnaire will be used to assess self-reported sitting time [69]. This instrument assesses the time spent sitting at work, watching TV, using a computer at home, transport and during other leisure activities on work and non-work days. It has acceptable levels of test-retest reliability (ICC = 0.46 – 0.90) and criterion validity compared to waist worn accelerometry (r = 0.18 – 0.46) [69].
Self-reported sleep quality will be assessed using the Pittsburgh Sleep Quality Index (PSQI) and the Behavioral Risk Factor Surveillance Sleep Module [70, 71]. The PSQI assesses the duration and quality of sleep over the previous month using 19 items that assess seven separate components of sleep, including duration, sleep latency and sleep problems. Each of the seven components are scored from zero to three and are summed to provide an overall score of sleep quality ranging from 0 to 21 where higher scores indicate poorer sleep quality. The Behavioral Risk Factor Surveillance Sleep Module contains 5 items assessing the average duration of sleep in a 24-h period, number of days in the previous month that an individual reports feeling they did not get enough rest or sleep, and unintentionally falling asleep during the day. The instrument also assesses if a person nodded off or fell asleep, even just for a brief moment, while driving in the last 30 days (yes, no, not applicable) and if they have ever been told they snore (yes, no, don’t know, unsure) [71]. Self-reported sleep timing and variation in sleep timing will be assessed using the 18 item Sleep Timing Questionnaire [72]. This instrument assesses the earliest and latest time of day a person usually goes to bed and wakes up, the usual time of day a person goes to bed and wakes up and the variation in these times on both weekends and week days. The Sleep Timing Questionnaire has demonstrated acceptable levels of test-retest reliability (r = 0.70), validity with accelerometery (r = 0.59) and sleep diary (r = 0.83–0.86) measures of sleep timing.
Depression, anxiety and stress
Physical activity, sedentary and sleep behaviours are associated with symptoms of depression, anxiety and stress and participants will complete the Depression, Anxiety and Stress Scale (DASS-21) to assess these [73–77]. Each of the 21 items in this scale asks participants to report how much each emotional experience (e.g., over reacting, feeling sad/depressed, feeling scared for no reason) statement applied to them over the previous week, using three response options from “did not apply to me at all” to “applied to me very much, or most of the time” [73, 74].
Health related quality of life
Health related quality of life will be assessed using the valid and reliable Centres for Disease Control Healthy Days Instrument [78–80]. This instrument assesses the self-rated health, frequency of physical and mental unhealthy days over the previous 30 days and the presence of activity limitations.
Mediators
Lifestyle behaviour habit
The 4-item automaticity subscale of self-report behavioural automaticity index will be used to assess the level of automaticity associated with physical activity, sedentary and sleep behaviours (thus 12 items in total) [81]. Example items are “Not sitting for prolonged periods is something I do without thinking”, “Consistent sleep and wake times are something I do without having to consciously remember.” Each item is assessed using a 7 point scale from Strongly Disagree to Strongly Agree. The four items for each behaviour are summed to create an overall score from 7 to 21, where higher scores indicate greater levels of automaticity. Previous research has shown that this subscale is reliable, relates to prospective behavior, and moderates between-person intention-behavior relations as theorized [81].
Sleep hygiene
Participants’ sleep hygiene practices will be assessed using the 13 item Sleep Hygiene Index, which assesses the frequency that participants engage in behaviours that affect sleep hygiene [82]. Each item uses a five point response scale (always, frequently, sometimes, rarely and never) which are summed to provide an overall score where higher scores indicate poorer sleep hygiene practices. The Sleep Hygiene Index has acceptable levels of internal consistency (Cronbach’s α = 0.66), test-retest reliability (r = 0.71), and validity compared to the Pittsburgh Sleep Quality Index (r = 0.37 – 0.45) and the Epworth Sleepiness Scale (r = 0.24).
Social cognitive factors
The Balanced intervention was guided by social cognitive and self-regulatory theories and items adapted from previous research are used to assess the constructs of intentions, motivation, action planning, outcome expectancies, outcome expectations, behavioural strategies, situational control, social support, and self-efficacy over a one month period [83]. The original instrument demonstrated acceptable levels of internal consistency (α = 0.63–0.79) [83]. The items were modified to align with the target behaviours of the Balanced intervention (e.g., regular physical activity, limit sedentary behaviour, regular sleep and wake times). A total of 11 items were used to assess these constructs for each of the three target behaviours. For each of the target behaviours a single item was used to assess intentions, motivation, action planning, situational control, social support, and self-efficacy and two items for both outcome expectancies and outcome expectations. Participants were asked to indicate their agreement with each statement using a five point scale, from Strongly Disagree to Strongly Agree.
Using five items that are answered on a five point scale, from Strongly Agree to Strongly Disagree participants reported their confidence to engage in regular physical activity, limit sedentary behaviour, and keep regular sleep and wake times, any two of these behaviours and all three of these behaviours (5 items total). Using three items that are answered on a five point scale, from Strongly Agree to Strongly Disagree participants also indicated how much they agree that their current physical activity, sedentary and sleep behaviours are a risk to their health. These items are adapted from previously used items and modified to assess the target behaviours of the intervention [49].
Usability, satisfaction and process evaluation
Participant perceptions of usability of the intervention platform will be assessed using the System Usability Scale, a 10 item scale that uses a 5 point response to assess agreement with each item from Strongly Agree to Strongly Disagree [84]. All items are weighted by 2.5 (including several reverse scored items) to provide an overall score from 0 to 100 where higher scores indicate greater levels of usability. Eleven items will be used to assess participant satisfaction with the intervention including the perceived usefulness of the app to self-monitor behaviours and change behaviours, the level of detailed feedback provided and the accuracy of information provided. Participants were asked to indicate their agreement with each statement using a five point scale, from Strongly Disagree to Strongly Agree. These items are similar to those used in previous studies to assess satisfaction with the intervention [28]. A randomly selected subsample of participants will also be asked to complete semi-structured interviews after completion of the study to provide information to be used as part of the process evaluation. This will include discussion on the aspects of the intervention that they believed worked well and that could be improved, information of how regularly they would like to use the app and why they did or did not use the app.
Engagement and use of the intervention platform
Engagement with and use of the intervention will be measured using usage statistics captured by the app database. For each behaviour and behavioural goal information is collected on the time of day and date that the entry is made and edited, the actual entry (e.g. 30 min of physical activity), and the method of entry (device-entered, user-entered). These measures are collected daily throughout the intervention period.
Socio-demographics, Anthropometrics and cardiometabolic risk
Participants will provide information on their age, gender, years of education, occupational level, hours of work (daytime, night time, afternoon), number of days worked in previous week and average hours of work each day. Presenteeism at work over the previous 28 days will be assessed using a single item from the World Health Organization Health and Work Performance Questionnaire [85, 86]. This item asks participants to rate their performance at work on a scale of 0 to 10, where zero is the worst performance.
A research assistant blinded to group allocation will measure height, weight, waist circumference, and blood pressure with participants dressed in light clothing and without shoes. Weight (kg) will be measured on a calibrated digital scale to 0.01 kg (Biospace BSM370 Portable Automatic BMI Stadiometer, Biospace CO, Ltd., Seoul Korea). Weight will be measured twice if the two values are within 0.1 kg. If measurements vary by more than 0.1 kg a third measurement will be taken and the average of the two measures that are within 0.1 kg will be recorded. Height (cm) will be measured to 0.1 cm using a stadiometer (Biospace BSM370 Portable Automatic BMI Stadiometer, Biospace CO, Ltd., Seoul, Korea). Two measures of height will be taken and if values are not within 0.3 cm a third measure will be taken. The average of the two height measures within 0.3 cm will be taken. Waist circumference (cm) will be measured at the umbilicus (Seca 203, Seca Gmph & Co. Hamburg, Germany). Two measures will be taken, if these measures are not within 0.5 cm a third measure of waist circumference will be taken. The average of the two waist circumference measures within 0.5 cm will be taken [87].
Blood pressure and resting heart rate will be taken using a digital sphygmomanometer (Omron HEM-7320, Omron Healthcare, Co., Ltd., Kyoto, Japan) after participants have been seated quietly for 5 min. Following a 5-min minimum of sitting, two measures of blood pressure will be taken with a minimum 2-min period of rest between measures. If the two measures vary by more than 10 mm Hg (systolic), 5 mm Hg (diastolic) and 5 bpm for resting heart rate, up to five additional measures will be performed until three of the measures are within these ranges. The average of the three measures within this range will be taken [87]. Measures of total cholesterol, HDL cholesterol, LDL cholesterol, triglycerides and glucose will be taken using a capillary sample of blood drawn from the finger using the Cardiochek PA (Polymer Technology Systems, Inc., Indiana, US; BHR Pharmaceuticals Ltd., Nuneaton, UK). The measures are taken non-fasted and the time of the last meal consumed will be recorded. Capillary blood samples, presenteesism, and health related quality of life are assessed at visits 2 and 8 to limit participant burden associated with collecting capillary blood samples and due to the recall periods used in the presenteeism and health related quality of life measures.
Diet is also assessed in order to account for the effects of any changes in diet on physical activity and sleep and also measures of cardiometabolic risk [88–90]. Dietary items will assess consumption of fruit, vegetables, takeaway food consumption, drinks containing caffeine, and drinks containing alcohol. Fruit and vegetable consumption is assessed by the number of serves of these foods usually eaten each day. Consumption of takeaway food (pies, pastries, fried foods, hot chips, or takeaway meals) is assessed as the number of times per week. These items are based on an existing instrument that has demonstrated acceptable levels of validity compared to a 4 day food diary (r = 0.32 – 0.55) [91]. Alcohol and caffeine consumption are assessed using 4 items to assess the number of days in the last week that drinks containing alcohol and caffeine were consumed, and the number of drinks consumed on each day. These latter items are adapted from existing instrument used to assess risky alcohol consumption [92].
Power and sample size
A statistician independent of the research team performed the power and sample size calculations were based on detecting between group differences in changes in physical activity (30 min difference, standard deviation = 30), sedentary behaviour (90 min difference, standard deviation =110), variation in time to sleep (30 min difference, standard deviation = 40), variation in time to wake (30 min difference, standard deviation = 35), and sleep efficiency (5 % difference, standard deviation = 5) at the end of the intervention. Assuming a correlation of 0.6 between the repeated measurements, a total sample of 48 participants will give the study 80 % power to detect a group by time interaction for each of the five primary outcome variables, using an alpha level of 0.01. Hence a minimum of 64 participants (32 per treatment arm) will be recruited into the study to allow for 35 % attrition over the study period.
Analysis
Baseline data will be summarized as the number of observations, means, standard deviations, medians, minimums and maximums where the data are continuous and as number of observations and frequencies where the data are categorical. Analyses will follow an intention to treat approach. There are five primary outcomes in the study: minutes of moderate-to-vigorous intensity physical activity, minutes of sedentary behaviour, variation in time to sleep, variation in time to wake, and sleep efficiency. The primary analysis will test for between-group differences across the four study assessment points using separate linear mixed models for each outcome, with fixed effects for treatment group (device-entered vs. user-entered), time (assessment 1, 2, 3 and 4) and their interaction. Since the standard errors of the fixed effects depend on the variance-covariance structure that is used in the analysis, several possible structures including models with multiple random effects (e.g., intercept, time) as well as inclusion of autocorrelated error structures (e.g., AR1, Toeplitz) will be examined. Based on Akaike Information Criterion (AIC) the most reasonable fitting model will be selected. The interaction term will be tested at 1 % to allow for increased type 1 error rates associated with multiple primary outcomes. Secondary analyses will examine changes in composite measures of the primary outcome variables and selected secondary outcomes at the 0.05 level of significance.
Discussion
Large proportions of the population report insufficient physical activity, high volumes of sedentary behaviour and poor sleep [8–13]. Consequently, interventions targeting these behaviours must have large reach, an objective that can be achieved by delivering interventions using technology-based approaches [26, 37]. Technology-based approaches also allow participants to access intervention materials at times and places convenient to them and do not require face to face contact which is a limitation of traditional practitioner delivered treatments e.g., behavioural change counselling [26, 37]. This study demonstrates the efficacy of a novel app-based multi-behaviour intervention to improve physical activity, sedentary behaviour and sleep quality.
An important aspect of this study is examining the relative efficacy two different approaches to self-monitoring behaviour: device-entered and user-entered. These approaches have been used previously in interventions seeking to improve physical activity and sleep, although their relatively efficacy to improve these behaviours has not been directly compared [28, 31, 93]. Examining differences in the efficacy of these self-monitoring approaches is important to inform future behaviour change interventions. Automated approaches reduce bias and burden associated with manual recording, but require resources with financial implications. It is therefore important to understand the relative efficacy on behaviour change.
Strengths of the study include a multi-behaviour approach targeting physical activity, sedentariness and sleep: this approach can leverage the potential for reciprocal effects among the three behaviours and the occurrence of any co-action effects that may occur [17, 18, 22, 90]. A further strength of the study is the recruitment of a population-based non clinical sample. Few studies have been conducted in populations who report poor sleep yet do not have a diagnosed sleep condition [17, 37], although over 20 % of the population report inadequate sleep, only approximately half of this is due to sleep conditions [94]. In addition, interventions using app-based interventions and/or website-based interventions frequently observe non-usage attrition over the first 4 weeks of the intervention period, yet do not assess behaviour change until well after non-usage attrition has occurred (e.g. 12 weeks) [28, 36, 38, 39]. A strength of this study is the timing of assessments which are intended to capture changes in behaviour and platform usage over a time period which is infrequently examined.
In summary this study simultaneously targets improvements in physical activity, sedentariness and sleep quality, and will provide important information on the efficacy of different self-monitoring strategies. A multiple behaviour intervention that can improve these behaviours and which has large reach, as provided by app-based delivery methods, has considerable potential given the health risks associated with these behaviours and the proportions of the population that engage in these behaviours in ways that adversely impact health.
References
Cappuccio FP, D’Elia L, Strazzullo P, Miller MA. Quantity and Quality of Sleep and Incidence of Type 2 Diabetes A systematic review and meta-analysis. Diabetes Care. 2010;33(2):414–20.
Chau JY, Grunseit AC, Chey T, Stamatakis E, Brown WJ, Matthews CE, Bauman AE, van der Ploeg HP. Daily sitting time and all-cause mortality: a meta-analysis. PLoS One. 2013;8(11):e80000.
Lee IM, Shiroma EJ, Lobelo F, Puska P, Blair SN, Katzmarzyk PT. Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet. 2012;380(9838):219–29.
Shankar A, Syamala S, Kalidindi S. Insufficient Rest or Sleep and Its Relation to Cardiovascular Disease, Diabetes and Obesity in a National. Multiethnic Sample PLoS One. 2010;5(11):e14189.
Alvaro PK, Roberts RM, Harris JK. A Systematic Review Assessing Bidirectionality between Sleep Disturbances, Anxiety, and Depression. Sleep. 2013;36(7):1059–68.
Lee SWH, Ng KY, Chin WK. The impact of sleep amount and sleep quality on glycemic control in type 2 diabetes: A systematic review and meta-analysis. Sleep Med Rev. 2016. doi:10.1016/j.smrv.2016.02.001.
Buysse DJ. Sleep health: can we define It? does it matter? Sleep. 2014;37(1):9–17.
Bonke J. Trends in short and long sleep in Denmark from 1964 to 2009, and the associations with employment, SES (socioeconomic status) and BMI. Sleep Med. 2015;16(3):385–90.
Jean-Louis G, Williams N, Sarpong D, Pandey A, Youngstedt S, Zizi F, Ogedegbe G. Associations between inadequate sleep and obesity in the US adult population: analysis of the national health interview survey (1977–2009). BMC Public Health. 2014;14(1):290.
Bauman A, Ainsworth BE, Sallis JF, Hagströmer M, Craig CL, Bull FC, Pratt M, Venugopal K, Chau J, Sjöström M. The Descriptive Epidemiology of Sitting: A 20-Country Comparison Using the International Physical Activity Questionnaire (IPAQ). Am J Prev Med. 2011;41(2):228–35.
Ng SW, Popkin BM. Time use and physical activity: a shift away from movement across the globe. Obes Rev. 2012;13(8):659–80.
Duncan M, Kline CE, Rebar A, Vandelanotte C, Short C. Associations between variability in time to sleep and waking times and lifestyle behaviours. J Public Health. 2016;24:31–40.
Rezende LFM, Sá TH, Mielke GI, Viscondi JYK, Rey-López JP, Garcia LMT. All-Cause Mortality Attributableto Sitting Time. Am J Prev Med.
Filion AJ, Darlington G, Chaput JP, Ybarra M, Haines J. Examining the influence of a text message-based sleep and physical activity intervention among young adult smokers in the United States. BMC Public Health. 2015;15:671.
Ashton LM, Hutchesson MJ, Rollo ME, Morgan PJ, Collins CE. A scoping review of risk behaviour interventions in young men. BMC Public Health. 2014;14(1):1–23.
King K, Meader N, Wright K, Graham H, Power C, Petticrew M, White M, Sowden AJ. Characteristics of Interventions Targeting Multiple Lifestyle Risk Behaviours in Adult Populations: A Systematic Scoping Review. PLoS One. 2015;10(1):e0117015.
Kredlow MA, Capozzoli MC, Hearon BA, Calkins AW, Otto MW. The effects of physical activity on sleep: a meta-analytic review. J Behav Med. 2015;38(3):427–49.
Kline CE. The bidirectional relationship between exercise and sleep: Implications for exercise adherence and sleep improvement. Am J Lifestyle Med. 2014;8(6):375–379.
Madden KM, Ashe MC, Lockhart C, Chase JM. Sedentary behavior and sleep efficiency in active community-dwelling older adults. Sleep Sci. 2014;7(2):82–8.
Lambiase MJ, Gabriel KP, Kuller LH, Matthews KA. Temporal relationships between physical activity and sleep in older women. Med Sci Sports Exerc. 2013;45(12):2362–8.
Johnson SS, Paiva AL, Mauriello L, Prochaska JO, Redding C, Velicer WF. Coaction in multiple behavior change interventions: consistency across multiple studies on weight management and obesity prevention. Health Psychology Off J Div Health Psychol Am Psychol Assoc. 2014;33(5):475–80.
Mc Sharry J, Olander EK, French DP. Do single and multiple behavior change interventions contain different behavior change techniques? A comparison of interventions targeting physical activity in obese populations. Health psychology : official journal of the Division of Health Psychology, American Psychological Association. 2015;34(9):960–965.
Michie S, Abraham C, Whittington C, McAteer J, Gupta S. Effective techniques in healthy eating and physical activity interventions: a meta-regression. Health Psychol. 2009;28:690–701.
Michie S, Ashford S, Sniehotta FF, Dombrowski SU, Bishop A, French DP. A refined taxonomy of behaviour change techniques to help people change their physical activity and healthy eating behaviours: the CALO-RE taxonomy. Psychol Health. 2011;26(11):1479–98.
Alley S, Schoeppe S, Guertler D, Jennings CA, Duncan MJ, Vandelannote C. Interest and preferences for using advanced physical activity tracking devices: results of a national cross sectional survey. BMJ Open. 2016;6(7):e011243.
Davies C, Spence J, Vandelanotte C, Caperchione C, Mummery W. Meta-analysis of internet-delivered interventions to increase physical activity levels. Int J Beh Nut Phys Act. 2012;9(1):52.
Bandura A. Theories of Cognitive Self-RegulationSocial cognitive theory of self-regulation. Organ Behav Hum Decis Process. 1991;50(2):248–87.
Duncan M, Vandelanotte C, Kolt GS, Rosenkranz RR, Caperchione CM, George ES, Ding H, Hooker C, Karunanithi M, Maeder AJ et al. Effectiveness of a web- and mobile phone-based intervention to promote physical activity and healthy eating in middle-aged males: randomized controlled trial of the ManUp study. JMIR. 2014;16(6):e136.
Morgan PJ, Lubans DR, Collins CE, Warren JM, Callister R. 12-month outcomes and process evaluation of the SHED-IT RCT: An internet-based weight loss program targeting men. Obesity. 2011;19(1):142–51.
Kirwan M, Duncan MJ, Vandelanotte C, Kerry Mummery W. Using smartphone technology to monitor physical activity in the 10,000 steps program: A matched case–control trial. J Med Internet Res. 2012;14(2):176–85.
Espie CA, Kyle SD, Williams C, Ong JC, Douglas NJ, Hames P, Brown JS. A randomized, placebo-controlled trial of online cognitive behavioral therapy for chronic insomnia disorder delivered via an automated media-rich web application. Sleep. 2012;35(6):769–81.
Christensen H, Batterham PJ, Gosling JA, Ritterband LM, Griffiths KM, Thorndike FP, Glozier N, O’Dea B, Hickie IB, Mackinnon AJ. Effectiveness of an online insomnia program (SHUTi) for prevention of depressive episodes (the GoodNight Study): a randomised controlled trial. Lancet Psychiatry. 2016;3(4):333–341.
Compernolle S, Vandelanotte C, Cardon G, De Bourdeaudhuij I, De Cocker K. Effectiveness of a Web-Based, Computer-Tailored, Pedometer-Based Physical Activity Intervention for Adults: A Cluster Randomized Controlled Trial. J Med Internet Res. 2015;17(2):e38.
Ferguson T, Rowlands A, Olds T, Maher C. The validity of consumer-level, activity monitors in healthy adults worn in free-living conditions: a cross-sectional study. Int J Behav Nutr Phys Act. 2015;12(1):42.
Bort Roig J, Gilson ND, Puig-Ribera A, Contreras RS, Trost SG. Measuring and influencing physical activity with smartphone technology: a systematic review. Sports Medicine (Auckland, NZ). 2014;44(5):671–86.
Vandelanotte C, Müller AM, Short CE, Hingle M, Nathan N, Williams SL, Lopez ML, Parekh S, Maher CA. Past, Present, and Future of eHealth and mHealth Research to Improve Physical Activity and Dietary Behaviors. J Nutr Educ Behav. 2016;48(3):219–28:e211.
Cheng SK, Dizon J. Computerised cognitive behavioural therapy for insomnia: a systematic review and meta-analysis. Psychother Psychosom. 2012;81(4):206–16.
Eysenbach G. The law of attrition. J Med Internet Res. 2005;7(1):e11.
Donkin L, Hickie IB, Christensen H, Naismith SL, Neal B, Cockayne NL, Glozier N. Rethinking the Dose–response Relationship Between Usage and Outcome in an Online Intervention for Depression: Randomized Controlled Trial. J Med Internet Res. 2013;15(10):e231.
Department of Health. Australia’s Physical Activity and Sedentary Behaviour Guidelines for Adults (18–64 years). Canberra: Australian Government; 2014.
van der Ploeg HP, Chey T, Korda RJ, Banks E, Bauman A. Sitting time and all-cause mortality risk in 222 497 Australian adults. Arch Intern Med. 2012;172(6):494–500.
George ES, Rosenkranz RR, Kolt GS. Chronic disease and sitting time in middle-aged Australian males: findings from the 45 and Up Study. Int J Behav Nutr Phys Act. 2013;10(1):1–8.
Kirwan M, Duncan MJ, Vandelanotte C, Mummery WK. Design, Development, and Formative Evaluation of a Smartphone Application for Recording and Monitoring Physical Activity Levels: The 10,000 Steps “iStepLog”. Health Educ Behav. 2013;40(2):140–151.
Davies CA, Spence JC, Vandelanotte C, Caperchione CM, Mummery WK. Meta-analysis of internet-delivered interventions to increase physical activity levels. IJBNPA. 2012;9:52.
Webb T, Joseph J, Yardley L, Michie S. Using the internet to promote health behavior change: a systematic review and metaanalysis of the impact of theoretical basis, use of behavior change techniques, and mode of delivery on efficacy. J Med Internet Res. 2010;12(1):e4.
Bandura A. Social Cognitive Theory of self-regulation. Organi Behav Hum Decis. 1991;50.
Maes S, Karoly P. Self-Regulation Assessment and Intervention in Physical Health and Illness: A Review. Applied Psychology. 2005;54(2):267–299.
Commonwealth of Australia. Australia’s Physical Activity and Sedentary Behaviour Guidelines for Adults (18–64 years). Canberra: Commonwealth of Australia; 2014.
Duncan MJ, Gilson N, Vandelanotte C. Which population groups are most unaware of CVD risks associated with sitting time? Prev Med. 2014;65:103–8.
Vandelanotte C, Duncan MJ, Hanley C, Mummery WK. Identifying population subgroups at risk for underestimating weight health risks and overestimating physical activity health benefits. J Health Psychol. 2011;16(5):760–9.
Irish LA, Kline CE, Gunn HE, Buysse DJ, Hall MH. The role of sleep hygiene in promoting public health: A review of empirical evidence. Sleep Med Rev. 2015;22:23–36.
Buman MP, Hekler EB, Bliwise DL, King AC. Exercise Effects on Night-to-Night Fluctuations in Self-rated Sleep among Older Adults with Sleep Complaints. J Sleep Res. 2011;20(1 Pt 1):28–37.
Sleep Health Foundation. Good Sleep Habits. Blacktown, NSW: Sleep Health Foundation; 2011.
Sitting less for adults [http://heartfoundation.org.au/images/uploads/main/Active_living/Sitting_less_adults.pdf]. Accessed 1 Nov 2014.
Marteau TM, Hollands GJ, Fletcher PC. Changing human behavior to prevent disease: the importance of targeting automatic processes. Science. 2012;337(6101):1492–5.
Tudor-Locke C, Sisson SB, Collova T, Lee SM, Swan PD. Pedometer-determined step count guidelines for classifying walking intensity in a young ostensibly healthy population. Can J Appl Physiol. 2005;30(6):666–76.
Marshall SJ, Levy SS, Tudor-Locke CE, Kolkhorst FW, Wooten KM, Ji M, Macera CA, Ainsworth BE. Translating physical activity recommendations into a pedometer-based step goal: 3000 steps in 30 minutes. Am J Prev Med. 2009;36(5):410–5.
Wong SL, Colley R, Connor Gorber S, Tremblay M. Actical accelerometer sedentary activity thresholds for adults. J Phys Act Health. 2011;8(4):587–91.
Girschik J, Fritschi L, Heyworth J, Waters F. Validation of self-reported sleep against actigraphy. J Epidemiol. 2012;22(5):462–8.
Ryan P. RALLOC. Stata module to design randomized controlled trials. Boston: Boston College Department of Economics, Statistical Software Components S319901; 2011.http://econpapers.repec.org/software/bocbocode/s319901.htm. Accessed 27 Feb 2015.
van Hees VT, Sabia S, Anderson KN, Denton SJ, Oliver J, Catt M, Abell JG, Kivimaki M, Trenell MI, Singh-Manoux A. A Novel, Open Access Method to Assess Sleep Duration Using a Wrist-Worn Accelerometer. PLoS One. 2015;10(11):e0142533.
Hildebrand M, VT VANH, Hansen BH, Ekelund U. Age group comparability of raw accelerometer output from wrist- and hip-worn monitors. Med Sci Sports Exerc. 2014;46(9):1816–24.
Sabia S, van Hees VT, Shipley MJ, Trenell MI, Hagger-Johnson G, Elbaz A, Kivimaki M, Singh-Manoux A. Association between questionnaire- and accelerometer-assessed physical activity: the role of sociodemographic factors. Am J Epidemiol. 2014;179(6):781–90.
Pavey TG, Gilson ND, Gomersall SR, Clark B, Trost SG. Field evaluation of a random forest activity classifier for wrist-wornaccelerometer data. J Sci Med Sport. 2016. doi:10.1016/j.jsams.2016.06.003.
Buysse DJ, Cheng Y, Germain A, Moul DE, Franzen PL, Fletcher M, Monk TH. Night-to-night sleep variability in older adults with and without chronic insomnia. Sleep Med. 2010;11(1):56–64.
Brown WJ, Bauman A, Chey T, Trost S, Mummery K. Comparison of surveys used to measure physical activity. Aust N Z J Public Health. 2004;28(2):128–34.
Brown WJ, Bauman A, Trost S, Mummery WK, Owen N. Test-retest reliability of four physical activity measures used in population surveys. J Sci Med Sport. 2004;7(2):205–15.
Reeves MM, Marshall AL, Owen N, Winkler EAH, Eakin EG. Measuring physical activity change in broad-reach intervention trials. J Phys Act Health. 2010;7(2):194–202.
Chau JY, van der Ploeg HP, Dunn S, Kurko J, Bauman AE. A tool for measuring workers’ sitting time by domain: the Workforce Sitting Questionnaire. Br J Sports Med. 2011;45(15):1216–22.
Buysse DJ, Reynolds 3rd CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213.
(CDC). CfDCaP. Behavioral Risk Factor Surveillance System Survey Questionnaire. Atlanta, Georgia: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 2009.
Monk TH, Buysse DJ, Kennedy KS, Pods JM, DeGrazia JM, Miewald JM. Measuring sleep habits without using a diary: the sleep timing questionnaire. Sleep. 2003;26(2):208–12.
Lovibond PF, Lovibond SH. The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav Res Ther. 1995;33(3):335–43.
Antony MM, Bieling PJ, Cox BJ, Enns MW, Swinson RP. Psychometric properties of the 42-item and 21-item versions of the Depression Anxiety Stress Scales in clinical groups and a community sample. Psychol Assess. 1998;10(2):176.
Rebar AL, Stanton R, Geard D, Short C, Duncan MJ, Vandelanotte C. A meta-meta-analysis of the effect of physical activity on depression and anxiety in non-clinical adult populations. Health Psychol Rev. 2015;9(3):366–378.
Rebar AL, Vandelanotte C, Van Uffelen J, Short C, Duncan MJ. Associations of overall sitting time and sitting time in different contexts with depression, anxiety, and stress symptoms. Ment Health Phys Act. 2014;7(2):105–10.
Porkka Heiskanen T, Zitting KM, Wigren HK. Sleep, its regulation and possible mechanisms of sleep disturbances. Acta Physiol (Oxford, England). 2013;208(4):311–28.
Centres for Disease Control and Prevention. Measuring Healthy Days. Atlanta, Georgia: Centres for Disease Control and Prevention; 2000.
Andresen EM, Catlin TK, Wyrwich KW, Jackson-Thompson J. Retest reliability of surveillance questions on health related quality of life. J Epidemiol Community Health. 2003;57(5):339–43.
Moriarty DG, Zack MM, Kobau R. The Centers for Disease Control and Prevention’s Healthy Days Measures - population tracking of perceived physical and mental health over time. Health Qual Life Outcomes. 2003;1:37.
Gardner B, Abraham C, Lally P, de Bruijn G-J. Towards parsimony in habit measurement: Testing the convergent and predictive validity of an automaticity subscale of the Self-Report Habit Index. Int J Behav Nutr Phys Act. 2012;9(1):102.
Mastin DF, Bryson J, Corwyn R. Assessment of sleep hygiene using the Sleep Hygiene Index. J Behav Med. 2006;29(3):223–7.
Dewar DL, Lubans DR, Morgan PJ, Plotnikoff RC. Development and evaluation of social cognitive measures related to adolescent physical activity. J Phys Act Health. 2013;10(4):544–55.
Brooke J. US: A “quick and dirty” usability scale. London: Taylor and Francis; 1996.
Kessler RC, Ames M, Hymel PA, Loeppke R, McKenas DK, Richling DE, Stang PE, Ustun TB. Using the World Health Organization Health and Work Performance Questionnaire (HPQ) to evaluate the indirect workplace costs of illness. J Occupational Environ Med/Am College Occupational Environ Med. 2004;46(6 Suppl):S23–37.
Kessler RC, Barber C, Beck A, Berglund P, Cleary PD, McKenas D, Pronk N, Simon G, Stang P, Ustun TB et al. The World Health Organization Health and Work Performance Questionnaire (HPQ). J Occupational Environ Med/Am College Occupational Environ Med. 2003;45(2):156–74.
Aguiar EJ, Morgan PJ, Collins CE, Plotnikoff RC, Young MD, Callister R. The PULSE (Prevention Using LifeStyle Education) trial protocol: a randomised controlled trial of a Type 2 Diabetes Prevention programme for men. Contemporary Clin Trials. 2014;39(1):132–44.
Penev PD. Update on Energy Homeostasis and Insufficient Sleep. J Clin Endocrinol Metab. 2012;97(6):1792–801.
Pepin V, Boucetta S, Chan-Thim E, Parwanta Z, Gouin J-P, Dang-Vu TT. The Role of Sleep and Physical Activity on the Risk for Cardiovascular Disease. Curr Cardiovasc Risk Reports. 2014;8(12):1–10.
Chennaoui M, Arnal PJ, Sauvet F, Leger D. Sleep and exercise: a reciprocal issue? Sleep Med Rev. 2015;20:59–72.
O’Reilly S, McCann L. Development and validation of the Diet Quality Tool for use in cardiovascular disease prevention settings. Aust J Primary Health. 2012;18:138–47.
Bush K, Kivlahan DR, McDonell MB, Fihn SD, Bradley KA. The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Ambulatory Care Quality Improvement Project (ACQUIP). Alcohol Use Disorders Identification Test. Arch Intern Med. 1998;158(16):1789–95.
Cadmus-Bertram LA, Marcus BH, Patterson RE, Parker BA, Morey BL. Randomized Trial of a Fitbit-Based Physical Activity Intervention for Women. Am J Prev Med. 2015;49(3):414–8.
Hillman DR, Lack LC. Public health implications of sleep loss: the community burden. Med J Aust. 2013;199(8):7–10.
Acknowledgements
The Balanced app was developed by Headjam Inc. The authors thank Luke Kellett, Sarah Cook, and Ben Norman from Headjam Inc for their assistance in the development of the app.
Funding
This project is supported by Vanguard Grant (ID 100629) from the National Heart Foundation of Australia. The Funder had no role in the conduct of the trial or interpretation of results. MJD is supported by a Future Leader Fellowship (ID 100029) from the National Heart Foundation of Australia. CV is supported by a Future Leader Fellowship (ID 100427) from the National Heart Foundation of Australia. AR (GNT1105926) is supported by an Early Career Fellowship from the National Health Medical Research Council.
Availability of data and material
Requests for data can be made to the corresponding author.
Authors’ contributions
MJD is the overall lead. MJD, CV, SGT, ALR, NR, WJB conceived the study and prepared the funding application. NWB and MJD contributed expertise and text on behavioural interventions, psychological assessment. SGT and MJD lead development of the accelerometer methodology. BM, AR, SF participated in data acquisition. All authors read and approved the manuscript.
Competing interests
The authors declares that they have no competing interests.
Consent for publication
Participants provided consent for data associated with their participation in the study to be published.
Ethics approval and consent to participate
The study received ethical approval Human Research Ethics Committee of the University of Newcastle, Australia (Reference Number H-2014-0336). All participants provided informed consent to participate in the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Duncan, M.J., Vandelanotte, C., Trost, S.G. et al. Balanced: a randomised trial examining the efficacy of two self-monitoring methods for an app-based multi-behaviour intervention to improve physical activity, sitting and sleep in adults. BMC Public Health 16, 670 (2016). https://doi.org/10.1186/s12889-016-3256-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-016-3256-x