Abstract
Background
Schizophrenia is a serious and debilitating psychiatric disorder that is linked to marked social and occupational impairment. Despite the vital relevance of medication, non-adherence with recommended pharmacological treatments has been identified as a worldwide problem and is perhaps the most difficult component of treating schizophrenia. There are limited studies conducted on magnitude and potential factors of medication non-adherence among peoples with schizophrenia in Ethiopia.
Objectives
This study aimed to assess medication non-adherence and associated factors among peoples with schizophrenia at comprehensive specialized hospitals in Northwest Ethiopia.
Methods
An institutional-based cross-sectional study was conducted among 387 peoples with schizophrenia at selected hospitals in the Northwest of Ethiopia from June to August 2022. Study participants were enrolled using systematic random sampling. Medication non-adherence was measured using Medication Adherence Rating Scale (MARS). Data entry and analysis were done using Epi-data version 4.6.0 and SPSS version 24, respectively. A multivariable logistic regression model was fitted to identify factors associated with medication non-adherence. Variables with a p-value of < 0.05 at a 95% confidence interval were considered statistically significant.
Results
The prevalence of medication non-adherence was 51.2% (95% CI: 46.3, 56.3). Duration of treatment for more than ten years (AOR = 3.76, 95% CI: 1.43, 9.89), substance use (AOR = 1.92, 95% CI: 1.17, 3.13), antipsychotic polypharmacy, (AOR = 2.01, 95% CI: 1.11, 3.63) and extra-pyramidal side effect (AOR = 2.48, 95% CI: 1.24, 4.94) were significantly associated with medication non-adherence.
Conclusion
In this study, half of the participants were found to be medication non-adherent. Respondents with a longer duration of treatment, substance users, those on antipsychotic polypharmacy, and those who develop extra-pyramidal side effect need prompt screening and critical follow-up to improve medication adherence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Mental disorders are clinically severe disruptions in an individual's cognition, emotional regulation, or behavior. These disturbances are linked to dysfunctions in psychological, biological, or developmental processes, resulting in distress or dysfunction in critical areas of functioning [1]. Schizophrenia is a serious, debilitating, chronic psychiatric disorder distinguished by recurrent or chronic psychosis that is linked to marked social and occupational impairment and it affects 1% of the general population worldwide [2].
Non-adherence in the treatment of mental disorders can be characterized as the failure to get started on the treatment regimen, an untimely cessation of treatment, or the inadequate implementation of medical instructions, especially those related to administration of drugs [3]. Medication non adherence is a multi-faceted challenge linked with therapeutic alliance between the clinician and the patient, factors related to medications and factors related to the patients and their illness [4].The significance of maintenance therapy in schizophrenia has been well proved and sustained maintenance treatment with antipsychotic medication appears crucial in relapse prevention and control of psychotic symptoms [5, 6].
Poor adherence to prescribed medication is prominent across disorders, but it can be especially detrimental to the patient and burdensome to society in schizophrenia [7]. Despite the vital relevance of medication, non-adherence with recommended pharmacological treatments has been identified as a worldwide problem and is perhaps the most difficult component of treating patients with schizophrenia [8]. Non-adherence to antipsychotic drugs has a major impact on the course and prognosis of individuals with schizophrenia. It may raise the likelihood of symptomatic relapse, decrease treatment effectiveness, affect, suicidal attempts, frequent emergency department visits or re-hospitalizations and, as a result, lower quality of life [9, 10]. Poor antipsychotic drug adherence affects illness progression and linked with higher healthcare utilization and treatment costs [11].
Worldwide, there are regional variations in the rate of medication non-adherence among patients with schizophrenia. A comprehensive literature review revealed that non-adherence rates in schizophrenia are approximately 50%, with a wide range from 4% (found in a study with depot neuroleptic drugs) to 72% [12]. A study done in France among 291 participants reported that, 30% of them were considered to be non-adherent [13]. In Turkey 24.2% of individual with schizophrenia found to be non-adherent [14]. A study done among Nigerian out-patients with schizophrenia revealed that 62.5% of subjects were non-adherent to antipsychotic medications [15]. In Ethiopian context, the prevalence rate of antipsychotic non-adherence among peoples with schizophrenia ranges between 26.5% [16] and 48.4% [17].
Studies have shown that a frequent dosing schedule and severe illness symptoms [18] low level of therapeutic alliance, use of atypical antipsychotics [13], long-term substance abuse, financial restraints, medication related adverse effects, low level of insight [19], being female, poor social support, number of medications, complex drug regimen, were strong determinants of antipsychotic non-adherence among individuals with schizophrenia.
Identifying factors that are responsible for medication non-adherence is the first approach toward formulating effective solutions in order to improve level of adherence and treatment outcome of the peoples with schizophrenia. There are limited studies conducted on magnitude of medication non-adherence among peoples with schizophrenia in Ethiopia. Therefore, this study aims to assess the prevalence of medication non adherence and associated factors among peoples with schizophrenia attending outpatient psychiatry department at comprehensive specialized hospitals in Northwest Ethiopia.
Materials and methods
Study area and period
This study was conducted at the University of Gondar Comprehensive Specialized Hospital (UoGCSH), Felege-Hiwot Comprehensive Specialized Hospital (FHCSH), and Tibebe-Ghion Comprehensive Specialized Hospital (TGCSH) from June 1 to August 30 2022. The psychiatry department of UoGCSH offers services for individuals with mental health disorders, catering to both outpatient and inpatient needs. On average, 820 patients have follow-up visits per month in the psychiatry outpatient clinic [20]. Felege-Hiwot Comprehensive Specialized Hospital (FHCSH) provides mental health services through its inpatient unit with seventeen beds and four outpatient departments. Annually, it attends to a total of 19,200 clients, averaging 1,600 clients per month. Tibebe-Ghion Specialized Hospital (TGCSH) provides mental health services through four outpatient departments, one emergency room, and two inpatient units with a total capacity of 13 beds. Additionally, it offers psychotherapy services. Based on the monthly report from the psychiatry unit, TGCSH attends to a total of 4,864 outpatient clients annually, averaging 405 clients per month [21].
Study design and population
An institution-based cross-sectional study was employed. All adult peoples with schizophrenia having a regular follow up at the outpatient departments’ psychiatric clinic in the comprehensive specialized hospitals of Northwest Ethiopia were the source population. All adult individuals with schizophrenia having a regular follow up at the outpatient departments of UoGCSH, FHCSH and TGCSH during the study period were the study populations. Participants with the age of 18 years and above, taking antipsychotic medication, who had an insight to respond oral questions (satisfy the requirement in the insight assessment tool (get 3 out of 3), and patients who had one or more previous visits were included under the study. Participants who had incomplete medical record were excluded from the study.
Sample size determination
The sample size was calculated using a single population proportion formula as follows:
where, n is the desired sample size for a population of > 10,000, Z is the typical normal distribution set at 1.96 (which corresponds to 95% CI), the p-value signifies that positive prevalence was utilized in calculating the optimal sample size, and d is the degree of accuracy 0.05 required (a marginal error is 0.05). Even if there are studies conducted in our country, as this is a multicenter study, to get better representative sample, we used proportion as 50% in sample size calculation. Therefore, \(n=\frac{( 1.96{)}^{2} \times 0.5 (1-0.5)}{{0.05}^{2}}=384\)
Then, by adding 5% non-response rate, the final calculated sample size was 403.
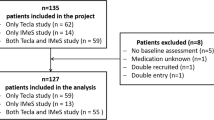
Sampling technique and procedure
The comprehensive specialized hospitals in the Northwestern Ethiopia were selected by a random lottery method. The total number of schizophrenia patients on follow up within 3 months was taken from the patients’ registration document to allocate samples proportionally within study areas. After proportional allocation, a systematic random sampling technique was used to select the study participants. The sampling fraction (k) was calculated by dividing the total number of peoples with schizophrenia within 3 months in the study area by the total sample size; (2625/403 gives 6.5 ≈ 6). The average number of peoples with schizophrenia in UoGCSH, FHCSH, and TGCSH were 1100, 1150, and 375, respectively. Therefore, the proportional allocation of sample size was 169 for UoGCSH, 176 for FHCSH, and 58 for TGCSH. The starting point was selected randomly from 1 to 6. Then, participants were interviewed, and concurrently, relevant data was reviewed from medical charts for every sixth respondents until the requirement for a sample was fulfilled. A unique identification card number was utilized as a questionnaire code in order to prevent the inclusion of the same respondents in the study more than once.
Operational definitions
Medication non-adherence
According to medication adherence rating scale (MARS), a value of less than 6 out of ten items is defined as non-adherence and value of ≥ 6 indicates adherence [22].
Antipsychotic polypharmacy
Refers to the co-prescription of more than one antipsychotic drug for a patient. Polypharmacy was documented when a particular patient was prescribed more than one antipsychotic drug for a minimum duration of one month or longer. [23, 24].
Extra-pyramidal side effect
Was screened using Simpson Angus Scale (SAS), with score of 0.65 and above [25].
Current substance use
Using at least one of a specific substance (alcohol, Khat or cigarettes) for nonmedical purposes within the last 3 months according to the Alcohol, Smoking, and Substance Involvement Screening Tool (ASSIST) [26].
Data collection instrument and procedure
A structured questionnaire was adopted from a previous literature [17] with some modifications for the context of the study area and socio-demographic characteristics of study participants was used. It was translated to the local Amharic language, and then back translated to the English version to check consistency. Translation was not required for variables obtained from medical records of the patients. The data collected by patient interview includes sociodemographic characteristics, substance use, and medication non- adherence. Physical examination and observation was used to measure extra-pyramidal side effect. The participants medical charts were used to fill in clinically related variables like duration of illness, duration of treatment, number of admissions, presence of co-morbidity, type of antipsychotics, and presence of antipsychotics polypharmacy. The questioner had five parts. The first part contains socio-demographic characteristics of the study participants, such as sex, age, marital status, residence, religion, educational level, occupation, and income level. The second section consisted of clinical and medication related characteristics like duration of illness, presence of co-morbidity, individual’s medication record, duration of treatment, and number of admissions. The third section consisted of the current substance use assessment tool. ASSIST was used to briefly screen ' use of psychoactive substances. The tool was developed and validated by WHO [26]. The fourth section consisted of an extra-pyramidal side effect assessment tool. The Simpson-Angus Scale (SAS) was used to measure antipsychotic induced side effect on a 10-item rating scale. It has been commonly used in both clinical and research setups. It consists of one item measuring gait (hypokinesia), six items measuring rigidity, and three items measuring glabella tap, tremor, and salivation, respectively. The cut-off value for screening for neuroleptic induced parkinsonism is 0.65 or more [25]. It has been used in Ethiopia [24, 27, 28]. The fifth section consisted of an adherence measuring tool. Medication Adherence Rating Scale (MARS) was used to evaluate medication non-adherence, which is a ten-item yes/no self-report questionnaire [29]. The MARS was adopted as a measure of medication adherence in the Psychological Prevention of Relapse in Psychosis experiment [30]. MARS has been utilized in Ethiopia [16, 22, 31].
Data quality control
Data was collected by face-to-face interview using a structured and pretested questionnaire. Data was collected by three BSc psychiatric nurses in UoGCSH under supervision of one master’s degree in psychiatry, three BSc psychiatric nurses in FHCSH with supervision of one BSc psychiatric nurse and two BSc psychiatric nurses in TGCSH under supervision of one BSc psychiatric nurse. The supervisors distributed all the necessary items for data collectors on each data collection day and were tasked with checking the filled questionnaire for completeness and solving reported problems timely during the data collection period. In all study areas, the principal investigator facilitated all the necessary materials.
To assure the quality of the data, one day training was given by the principal investigator at each study area for data collectors and supervisors. A pretest was conducted on 22 of the 5% of peoples with schizophrenia at Dessie Comprehensive Specialized Hospital's outpatient department to identify potential problems with the data collection tool and check the consistency of the questionnaire. Some modifications, such as correction of typing errors and the rearranging of questionnaires were made. The internal consistency of ASSIST, SAS, and MARS was assessed, and the Cronbach’s alpha was 0.76, 0.88 and 0.75 respectively, which was acceptable.
Data processing and analysis
The collected data was cleaned, coded, and entered into Epi Data 4.6.0 and analyzed using Statistical Package for Social Studies (SPSS) version 24. In descriptive analysis, the mean with standard deviation (SD), frequency, and percentages were used to check the distribution of the data. Bivariable and multivariable binary logistic regression analysis were employed to identify factors associated with medication non-adherence. The odds ratio (OR) with a 95% confidence interval was computed for each variable for the corresponding p-value to see the strength of association. A P-value of < 0.05 was used as the cut-off for the significance of the association between the outcome and the predictor variables. The model fitness was tested, and the Hosmer and Lemeshow test result was 0.809. Multicollinearity was checked, and the maximum Variance Inflation Factor (VIF) reported was less than 5, which was within the acceptable level.
Results
Sociodemographic characteristics of study participants
From a total of 403 approached samples, 387 (with a response rate of 96.1%) eligible participants with schizophrenia were included in the study. The majority (58.9%) were male with a mean (± SD) age of 36.5 (± 11.7) years. Greater than half (52.7%) of participants were married, and more than two-third (70.0%) of them lived in urban areas. More than a quarter (27.4%) of the participants' educational level was high school, and around one-fifth (22.7%) of them were privately employed. More than three-quarters (76.5%) of participants had a monthly income above 1200 Ethiopian birr as shown below (Table 1).
Clinical and substance related characteristics of participants
In terms of clinical characteristics, nearly half of the participants (47.8%) and nearly three-quarters (74.9%) had illness and treatment duration for less than 5 years respectively. One-quarter (25.3%) of patients had other co-morbid illnesses, from which hypertension (29.6%) and diabetes mellitus (21.4%) were predominant. One-quarter of respondents (25.1%) had two or more inpatient admissions, and 33.9% were substance users. More than two-fifths (44.3%) of those who used psychoactive substances used alcohol as shown below (Table 2).
Medication-related characteristics of participants
In this study, the prevalence of medication non-adherence was 51.2% (CI: 46.3, 56.3). More than one fifth (22.2%) of participants were on antipsychotic polypharmacy. About one-fourth (25.6%) of respondents took haloperidol and 26.4% of individuals received adjuvant medications, from which Amitriptyline was the predominant (35.3%). Roughly 15.0% of participants developed extra-pyramidal side effect (Table 3).
Factors associated with medication non-adherence
On multivariate analysis, longer duration of treatment, substance use, antipsychotic polypharmacy and extra-pyramidal side effect were significantly associated with medication non-adherence. Accordingly, participants who had treatment duration for more than ten years were 3.76 times more likely to be non-adherent compared with those who had treatment duration for less than five years (AOR = 3.76, 95% CI: 1.43, 9.89). Likewise, respondents who were psychoactive substance users were 1.92 times more likely to be non-adherent than those who were not substance users (AOR = 1.92, 95% CI: 1.17, 3.13).
Individuals who were on APP were 2.01 times more likely to be non-adherent than those who were on antipsychotic monotherapy (AOR = 2.01, 95% CI: 1.11, 3.63). Concerning extra-pyramidal side effect, those who developed EPS were 2.48 times more likely to be non-adherent than those who did not developed (AOR = 2.48, 95% CI: 1.24, 4.94) as shown below (Table 4).
Discussion
Despite the critical need of pharmacotherapy, it has been noted that non-adherence with suggested pharmacological therapies is a global issue and is possibly the most challenging aspect of treating people with schizophrenia [8]. Non-adherence to antipsychotics may increase the risk of symptomatic relapse, reduce the efficacy of therapy, increase the chance of suicidal thoughts or attempts, need frequent visits to the emergency department, increase treatment costs and consequently diminish quality of life [9,10,11]. Aiming at assessing medication non-adherence and associated factors in peoples with schizophrenia, the current study found that the overall prevalence of non-adherence was 51.2%. Duration of treatment, substance use, APP and extra-pyramidal side effect were significantly associated with medication non-adherence.
In this study, the prevalence of medication non-adherence was 51.2% (CI: 46.3, 56.3) which is comparable with studies in Ethiopia (48.4%) [17], Nigeria (54.2%) [15], and multi-continent survey (53%) [32]. However this finding is higher than that of study done in Mekelle (26.5%) [16] and Jimma 41.2% [33] Ethiopia. This variation could be due to differences in the types of adherence assessment tools and diverse inclusion criteria used. The study conducted in Mekelle reported relatively low rates of non-adherence, likely due to the differing approaches used to measure drug adherence. The lack of standardized criteria makes it challenging to categorize the extent of non-adherence among schizophrenia patients. For example, MARS used in Mekelle required 'yes/no' responses, with a score of 3 or above indicating adherence, and a score of 2 or below indicating non-adherence. This categorization differs from the current study, where adherence was defined as a MARS score of 6 or higher, and non-adherence as a score below 6. Additionally, the inclusion criteria varied, such as including only patients aged 18—65 and those who had been on continuous therapy for at least three months prior to the study [16], which may also have influenced the observed differences.
Studies conducted in Uganda 16.3% [34], China (20%) [35], Hong Kong 30% [36]indicated that the incidence of non-adherence were lower than the current study. On the contrary, study in Jordan (64.2%) [37], and India (88.16%) [38] were higher than the current study The inconsistencies in the prevalence of non-adherence may be explained by differences in clinical settings and methodological variations. These include diverse inclusion and exclusion criteria, such as requiring patients to have taken typical antipsychotics for at least six months [34], excluding patients who use psychoactive substance [35] and variations in study populations and sampling methods (convenience sampling) [38]. This finding suggests that appropriate interventions, such as developing awareness and implementing planned and continuous counseling programs, should be implemented to enhance their level of medication adherence.
In the current study, socio-demographic variables were not associated with medication non-adherence, consistent with previous evidence [17]. However, other studies have reported correlations between medication non-adherence and factors such as age range [39], place of residence [40], marital status [41], and educational level [16]. These discrepancies could be due to variations in demographic data and sample size.
In terms of treatment duration, participants with treatment duration of more than ten years were more likely to be non-adherent compared with those who had treatment duration for less than five years. This is in line with various studies [42], [43]. This could be because of after starting treatment, these individuals may have interrupted their follow-up after achieving remission, and they may have had a poor outcome over time. Besides longer treatment course might predispose forgetfulness, carelessness and exposure for side effects may negatively influence medication adherence. Healthcare professionals need to follow and provide continuous counseling to improve adherence for patients having longer duration of treatment.
This study also showed that peoples who use psychoactive substance were more likely to be non-adherent than those who did not use. This finding is in line with studies from Ethiopia [42], Morocco [44] and Norway [45]. This might be due to a person's internal state can be negatively impacted by specific substance use, leading to worsened cognitive abnormalities and unpleasant withdrawal symptoms. There are a number of long-term social and clinical implications of drug and alcohol use in addition to the immediate bodily effects. In addition, substance users are more likely to experience tardive dyskinesia and report more extra-pyramidal symptoms than those who abstain from using drugs or alcohol. The higher likelihood of social rejection and eventual homelessness or a lack of family support is additional effects of those substances, both of which can lead to prescription non-adherence[17]. Hence individuals who use psychoactive substances require psychological support to withdraw from psychoactive substances in order to adhere to their medications.
In the current study, respondents who were on antipsychotic polypharmacy were more likely to be non-adherent than those who were on monotherapy. This finding goes with studies from Ethiopia [42], Nigeria [15] and Jordan [37]. This could be justified by being on APP, which may predispose to increased overall dose, increased utilization of concurrent anticholinergic medications, adverse drug reaction and drug interaction [46] which negatively influences medication adherence. Therefore people who were on APP need better antipsychotic utilization program and follow up to improve medication adherence.
This study also indicated that, those who developed EPS were more likely to be non-adherent than those who did not developed EPS. This finding is in line with studies from Ethiopia [17], Nigeria [3] and United states of America [28]. The possible explanation might be, developing side effect that hampers day-to-day activities, mobility, work capacity, and energy [47] might have its impact in reducing medication adherence. Consequently, individuals who developed EPS require better treatment of the side effect and improved selection of antipsychotics so as to enhance adherence to medications.
Limitation of the study
The current study has several limitations. Firstly, its results are only applicable to the study areas. Secondly, the study did not report the dosing of antipsychotics. Additionally, due to the inherent limitations of a cross-sectional design, it was unable to determine causal relationships between the independent and dependent variables. Self-reported adherence rates are known to overstate adherence prevalence, which may affect the findings. Furthermore, this study did not examine disease severity, and the assessment of substance use is subject to social desirability bias.
Conclusion and recommendation
In this study, half of the participants were found to be non-adherent. Critical follow-up is necessary for peoples who have been receiving treatment for a longer duration, substance users, those on antipsychotic polypharmacy and those who experience extra-pyramidal side effects. Healthcare personnel who work in hospitals should do routine substance use screenings and offer counseling on quitting psychoactive substances. To limit their detrimental impact on medication adherence, extra-pyramidal side effect should also be periodically monitored. Future studies could look at the relationship between medication non-adherence and potential predictive variables causally.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- AOR:
-
Adjusted Odds Ratio
- APP:
-
Antipsychotic Polypharmacy
- ASSIST:
-
Alcohol Smoking and Substance Involvement Screening Test
- CI:
-
Confidence Interval
- COR:
-
Crude Odds Ratio
- DM:
-
Diabetes Mellitus
- EPS:
-
Extra-pyramidal Side Effect
- FHCSH:
-
Felege-Hiwot Comprehensive Specialized Hospital
- HIV:
-
Human Immunodeficiency Virus
- MMAS:
-
Medication Adherence Scale
- MARS:
-
Medication Adherence Rating Scale
- OR:
-
Odds Ratio
- TGCSH:
-
Tibebe-Ghion Comprehensive Specialized Hospital
- SAS:
-
Simpson Angus Scale
- SD:
-
Standard Deviation
- SPSS:
-
Statistical Package for Social Studies
- UOGCSH:
-
University of Gondar Comprehensive Specialized Hospital
- VIF:
-
Variance Inflation Factor
- WHO:
-
World Health Organization
References
Guze SB. Diagnostic and statistical manual of mental disorders, (DSM-IV). American Journal of Psychiatry. 1995;152(8):1228-.
Kahn R, Sommer I, Murray R, Meyer-Lindenberg A. Weinberger D. CannonT, et al.Schizophrenia Nat Rev Dis Primers. 2015;1:15067.
Effiong JH, Umoh KA. Medication non adherence in schizophrenia: Prevalence and correlates among outpatients in a tertiary healthcare facility in Uyo. South-South Nigeria Clin Med Diagn. 2015;5(6):107–13.
Deegan PE, Drake RE. Shared decision making and medication management in the recovery process. Psychiatr Serv. 2006;57(11):1636–9.
Kishimoto T, Agarwal V, Kishi T, Leucht S, Kane JM, Correll CU. Relapse prevention in schizophrenia: a systematic review and meta-analysis of second-generation antipsychotics versus first-generation antipsychotics. Mol Psychiatry. 2013;18(1):53–66.
Takeuchi H, Kantor N, Sanches M, Fervaha G, Agid O, Remington G. One-year symptom trajectories in patients with stable schizophrenia maintained on antipsychotics versus placebo: meta-analysis. Br J Psychiatry. 2017;211(3):137–43.
Terkelsen KC, Menikoff A. Measuring the costs of schizophrenia: implications for the post-institutional era in the US. Pharmacoeconomics. 1995;8:199–222.
Organization WH. Schizophrenia. Geneva: World Health Organization; 2011.
Adelufosi AO, Adebowale TO, Abayomi O, Mosanya JT. Medication adherence and quality of life among Nigerian outpatients with schizophrenia. Gen Hosp Psychiatry. 2012;34(1):72–9.
Farooq S, Naeem F. Tackling nonadherence in psychiatric disorders: current opinion. Neuropsychiatric disease and treatment. 2014;1069–77.
Sun SX, Liu GG, Christensen DB, Fu AZ. Review and analysis of hospitalization costs associated with antipsychotic nonadherence in the treatment of schizophrenia in the United States. Curr Med Res Opin. 2007;23(10):2305–12.
Lacro JP, Dunn LB, Dolder CR, Leckband SG, Jeste DV. Prevalence of and risk factors for medication nonadherence in patients with schizophrenia: a comprehensive review of recent literature. J Clin Psychiatry. 2002;63(10):892–909.
Dassa D, Boyer L, Benoit M, Bourcet S, Raymondet P, Bottai T. Factors associated with medication non-adherence in patients suffering from schizophrenia: a cross-sectional study in a universal coverage health-care system. Aust N Z J Psychiatry. 2010;44(10):921–8.
Mert DG, Turgut NH, Kelleci M, Semiz M. Perspectives on reasons of medication nonadherence in psychiatric patients. Patient preference and adherence. 2015;87–93.
Ibrahim A, Pindar S, Yerima M, Rabbebe I, Shehu S, Garkuwa H, et al. Medication-related factors of non adherence among patients with schizophrenia and bipolar disorder: outcome of a cross-sectional survey in Maiduguri. North-eastern Nigeria J Neurosci Behav Health. 2015;7(5):31–9.
Eticha T, Teklu A, Ali D, Solomon G, Alemayehu A. Factors associated with medication adherence among patients with schizophrenia in Mekelle, Northern Ethiopia. PLoS ONE. 2015;10(3): e0120560.
Girma S, Abdisa E, Fikadu T. Prevalence of Antipsychotic Drug Non Adherence and Associated Factors Among Patients with Schizophrenia Attending at Amanuel Mental Specialized Hospital, Addis Ababa, Ethiopia: Institutional Based Cross Sectional Study. Health Science Journal. 2017;11(4).
Yaegashi H, Kirino S, Remington G, Misawa F, Takeuchi H. Adherence to oral antipsychotics measured by electronic adherence monitoring in schizophrenia: a systematic review and meta-analysis. CNS Drugs. 2020;34:579–98.
Novick D, Montgomery W, Treuer T, Aguado J, Kraemer S, Haro JM. Relationship of insight with medication adherence and the impact on outcomes in patients with schizophrenia and bipolar disorder: results from a 1-year European outpatient observational study. BMC Psychiatry. 2015;15(1):1–8.
Melkam M, Kassew T. Mental healthcare services satisfaction and its associated factors among patients with mental disorders on follow-up in the University of Gondar Comprehensive Specialized Hospital. Northwest Ethiopia Frontiers in Psychiatry. 2023;14:1081968.
Abate AW, Menberu M, Belete H, Ergetie T, Teshome AA, Chekol AT, et al. Perceived compassionate care and associated factors among patients with mental illness at Tibebe Ghion specialized and Felege Hiwot comprehensive specialized hospital, Northwest Ethiopia. BMC Health Serv Res. 2023;23(1):650.
Endale Gurmu A, Abdela E, Allele B, Cheru E, Amogne B. Rate of nonadherence to antipsychotic medications and factors leading to nonadherence among psychiatric patients in Gondar University Hospital, Northwest Ethiopia. Advances in Psychiatry. 2014.
Kasteridis P, Ride J, Gutacker N, Aylott L, Dare C, Doran T, et al. Association between antipsychotic polypharmacy and outcomes for people with serious mental illness in England. Psychiatr Serv. 2019;70(8):650–6.
Tesfaye S, Debencho N, Kisi T, Tareke M. Prevalence of antipsychotic polypharmacy and associated factors among outpatients with schizophrenia attending Amanuel mental specialized hospital, Addis Ababa, Ethiopia. Psychiatry journal. 2016;2016.
Janno S, Holi MM, Tuisku K, Wahlbeck K. Validity of Simpson-Angus Scale (SAS) in a naturalistic schizophrenia population. BMC Neurol. 2005;5(1):1–6.
Group WAW. The alcohol, smoking and substance involvement screening test (ASSIST): development, reliability and feasibility. Addiction. 2002;97(9):1183–94.
Taye H, Awoke T, Ebrahim J. Antipsychotic medication induced movement disorders: the case of Amanuel specialized mental hospital, Addis Ababa. Ethiopia Am J Psychiatry Neurosci. 2014;2(5):76–82.
Ayehu M, Shibre T, Milkias B, Fekadu A. Movement disorders in neuroleptic-naïve patients with schizophrenia spectrum disorders. BMC Psychiatry. 2014;14(1):1–7.
Thompson K, Kulkarni J, Sergejew A. Reliability and validity of a new Medication Adherence Rating Scale (MARS) for the psychoses. Schizophr Res. 2000;42(3):241–7.
Fialko L, Garety PA, Kuipers E, Dunn G, Bebbington PE, Fowler D, et al. A large-scale validation study of the Medication Adherence Rating Scale (MARS). Schizophr Res. 2008;100(1–3):53–9.
Moges S, Belete T, Mekonen T, Menberu M. Lifetime relapse and its associated factors among people with schizophrenia spectrum disorders who are on follow up at Comprehensive Specialized Hospitals in Amhara region, Ethiopia: a cross-sectional study. Int J Ment Heal Syst. 2021;15(1):42.
Olivares JM, Alptekin K, Azorin J-M, Cañas F, Dubois V, Emsley R, et al. Psychiatrists’ awareness of adherence to antipsychotic medication in patients with schizophrenia: results from a survey conducted across Europe, the Middle East, and Africa. Patient preference and adherence. 2013:121–32.
Tesfay K, Girma E, Negash A, Tesfaye M, Dehning S. Medication non-adherence among adult psychiatric out-patients in Jimma University specialized hospital, Southwest Ethiopia. Ethiop J Health Sci. 2013;23(3):227–36.
Kule M, Kaggwa MM. Adherence to Typical Antipsychotics among Patients with Schizophrenia in Uganda: A Cross-Sectional Study. Schizophrenia Research and Treatment. 2023;2023.
Wang X, Zhang W, Ma N, Guan L, Law SF, Yu X, et al. Adherence to antipsychotic medication by community-based patients with schizophrenia in China: a cross-sectional study. Psychiatr Serv. 2016;67(4):431–7.
Bressington D, Mui J, Gray R. Factors associated with antipsychotic medication adherence in community-based patients with schizophrenia in Hong Kong: A cross sectional study. Int J Ment Health Nurs. 2013;22(1):35–46.
Mukattash TL, Alzoubi KH, Abu El-Rub E, Jarab AS, Al-Azzam SI, Khdour M, et al. Prevalence of non-adherence among psychiatric patients in Jordan, a cross sectional study. Int J Pharm Pract. 2016;24(3):217–21.
Ghosh P, Balasundaram S, Sankaran A, Chandrasekaran V, Sarkar S, Choudhury S. Factors associated with medication non-adherence among patients with severe mental disorder-A cross sectional study in a tertiary care centre. Exploratory Research in Clinical and Social Pharmacy. 2022;7: 100178.
Gebeyehu DA, Mulat H, Bekana L, Asemamaw NT, Birarra MK, Takele WW, et al. Psychotropic medication non-adherence among patients with severe mental disorder attending at Bahir Dar Felege Hiwote Referral hospital, north west Ethiopia, 2017. BMC Res Notes. 2019;12(1):102.
Tareke M, Tesfaye S, Amare D, Belete T, Abate A. Antipsychotic medication non-adherence among schizophrenia patients in Central Ethiopia. The South African journal of psychiatry : SAJP : the journal of the Society of Psychiatrists of South Africa. 2018;24:1124.
Mohammed F, Geda B, Yadeta TA, Dessie Y. Antipsychotic medication non-adherence and factors associated among patients with schizophrenia in eastern Ethiopia. BMC Psychiatry. 2024;24(1):108.
Tareke M, Tesfaye S, Amare D, Belete T, Abate A. Antipsychotic medication non-adherence among schizophrenia patients in Central Ethiopia. South African Journal of Psychiatry. 2018;24.
Lacro JP, Dunn LB, Dolder CR, Jeste DV. Prevalence of and risk factors for medication nonadherence in patients with schizophrenia: a comprehensive review of recent literature. J Clin Psychiatry. 2002;63(10):15489.
El Ammouri A, Kisra H. Predictors of medication non-adherence among a Moroccan sample of patients with schizophrenia: A cross sectional study. L’encephale. 2016;43(6):522–7.
Jónsdóttir H, Opjordsmoen S, Birkenaes A, Simonsen C, Engh J, Ringen P, et al. Predictors of medication adherence in patients with schizophrenia and bipolar disorder. Acta Psychiatr Scand. 2013;127(1):23–33.
Goh Y-L, Seng KH, Chuan ASH, Chua HC. Reducing antipsychotic polypharmacy among psychogeriatric and adult patients with chronic schizophrenia. The Permanente Journal. 2011;15(2):52.
Rekhi G, Tay J, Lee J. Impact of drug-induced Parkinsonism and tardive dyskinesia on health-related quality of life in schizophrenia. J Psychopharmacol. 2022;36(2):183–90.
Acknowledgements
We would like to acknowledge UoGCSH, FHCSH and TGCSH for facilitating the data collection. Also, we would like to express our deep gratitude to data collectors for their admirable commitment, as well as to study participants for their willingness to participate in this research.
Funding
The study was funded by University of Gondar.
Author information
Authors and Affiliations
Contributions
'FB wrote the protocol, designed the study, facilitated data collection, analyzed the data, and drafted the manuscript. AM and SA revised the manuscript and critically reviewed the article. AK participated in the analysis and interpretation of the results. EA and KG were involved in the facilitation of the data collection and critical review parts'.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval was obtained from the ethical review committee of the School of Pharmacy of the University of Gondar, with a reference number of SOPS/206/2014. Authorization was secured from all hospital authorities to perform this study. All study participants were informed about the purpose of the study, and their participation was voluntary. The participants were informed that a lack of desire to engage in the research would not affect the service they obtained. The participants were informed that a lack of desire to engage in the research would not affect the service they obtained. Written informed consent was gathered from individual participants. The privacy of participants was guaranteed, and any personal identifiers were not used. All the data was synonymized. The study was conducted based on the Declaration of Helsinki.
Consent for publication
NA.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Tamene, F.B., Mihiretie, E.A., Mulugeta, A. et al. Medication non-adherence and associated factors among peoples with schizophrenia: multicenter cross-sectional study in Northwest Ethiopia. BMC Psychiatry 24, 567 (2024). https://doi.org/10.1186/s12888-024-06004-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12888-024-06004-7