Abstract
Objectives
Electroconvulsive therapy (ECT) is one of the most effective treatments in mood disorders, mainly in major depressive episode (MDE) in the context of either unipolar (MDD) or bipolar disorder (BD). However, ECT remains a neglected and underused treatment. Older people are at high risk patients for the development of adverse drug reactions. In this context, we sought to determine the duration of MDEs and the number of lines of treatment before the initiation of ECT in patients aged 65 years or over according to the presence or absence of first-line indications for using ECT from international guidelines.
Methods
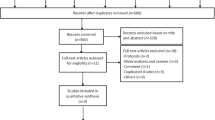
In this multicenter, retrospective study including patients aged 65 years or over with MDEs in MDD or BD who have been treated with ECT for MDEs, data on the duration of MDEs and the number of lines of treatment received before ECT were collected. The reasons for using ECT, specifically first-line indications (suicidality, urgency, presence of catatonic and psychotic features, previous ECT response, patient preference) were recorded. Statistical comparisons between groups used standard statistical tests.
Results
We identified 335 patients. The mean duration of MDEs before ECT was about 9 months. It was significantly shorter in BD than in MDD- about 7 and 10 months, respectively. The co-occurrence of chronic medical disease increased the duration before ECT in the MDD group. The presence of first-line indications for using ECT from guidelines did not reduce the duration of MDEs before ECT, except where there was a previous response to ECT. The first-line indications reduced the number of lines of treatment before starting ECT.
Conclusion
Even if ECT seems to be a key treatment in the elderly population due to its efficacity and safety for MDEs, the delay before this treatment is still too long.
Key points
• The mean duration of depression before ECT was 8.8 months.
• The duration before ECT for Bipolar Disorder (vs Major Depressive Disorder) is shorter.
• The co-occurrence of chronic medical disease increased the duration before ECT in the MDD group.
• Focusing on the first-line indications for using ECT, only a previous response reduces the duration of depression before ECT.
Similar content being viewed by others
Introduction
Electroconvulsive therapy (ECT) is one of most effective treatments in mood disorders, mainly in major depressive episode (MDE) in the context of either unipolar (MDD) or bipolar disorder (BD) [1, 2]. It is now well established that ECT is efficient and safe in the elderly population [3]. Moreover, a recent meta-analysis highlighted that ECT was particularly effective in elderly people with moderate and severe MDE [4, 5]. However, ECT remains a neglected and underused treatment [6,7,8]. In the elderly population, concerns regarding the side effects, mainly cognitive effects, may reduce its use [3]. Nevertheless, ECT should not be considered a "last line" treatment for the elderly population with MDE. It has been shown that its use is safe, with minimal side effects, when appropriate considerations are taken for this population [9].
Moreover, clinical guidelines do not limit the use of ECT for treatment-resistant depression (TRD) [10,11,12]. Indeed, ECT could be used as a first-line treatment when rapid clinical improvement is required, such as in the presence of psychotic or catatonic features, urgency (e.g. poor oral intake), high suicidality, or when patient preference or previous response to ECT are reported [10,11,12,13].
Recently, we highlighted in adult patients with MDE that, despite these recommendations, the mean duration of MDE before ECT was around 10 months and the mean number of lines of treatment before ECT was over 3 [14]. We also showed that the duration of MDE before ECT was longer for a single episode than for recurrent MDD and BD. Moreover, despite the fact that the presence of first-line indication for using ECT was associated with shorter duration of MDE and lower number of therapeutic sequences before ECT, this duration remained over 9 months and the number of lines of treatment over 3 [14].
Because of polypharmacy, multi-morbidity, and age-related changes in pharmacokinetics and pharmacodynamics, older people are high-risk patients for the development of adverse drug reactions (ADRs) [15]. Also, a problem can be the risk of drug interactions with other drugs taken due to chronic medical conditions [16]. Moreover, elderly patients with depression have a higher risk of suicide and more rapid life-threatening outcome. As a consequence, the use of ECT should occur earlier than in the younger population. However, to our knowledge, there is no study assessing delay before accessing ECT in this population.
In this context, we sought to determine the duration of MDEs and the number of lines of treatment before the initiation of ECT in patients aged 65 years or over depending on the presence or absence of first-line indications for using ECT from international guidelines.
Methods
Study design and recruiting characteristics
This multicenter, retrospective, cross-sectional study included patients recruited by the French national network of 12 experts [FondaMental Foundation (www.fondation-fondamental.org)] [17, 18] and collaborative centres hosted by academic departments of psychiatry (Besançon, Brest, Clermont-Ferrand, Créteil, Grenoble, Lyon, Marseille, Montpellier, Nantes, Paris, Toulouse, Tours).
Ethics approval and consent to participate
The assessment protocol was approved by the relevant ethical review board (CPP Sud-Est VI, 2016 / CE 07). This a retrospective study. All data were collected anonymously.
Population
This study of 335 individuals included all patients over 65 years with MDD or BD who have received ECT as acute treatment for an MDE according to DSM-IV-TR criteria from 1 January 2009 to 1 January 2014. Exclusion criteria were schizophrenia or schizoaffective disorder and autistic spectrum diagnosis (according to DSM-IV-TR criteria).
Measures
As previously described [14], the following data were extracted from the computerised or paper clinical records: sociodemographic data (age, sex), number of previous MDEs, lifetime diagnosis (MDD single episode, recurrent MDD, BD type 1 and 2), substance use disorders (tobacco, alcohol, cannabis, opioids, psychostimulants) and chronic physical disease comorbidities (cardiovascular, respiratory, neurologic, neoplastic, infectious, systemic, endocrinal, and metabolic). Duration of MDE (delay between the onset of the episode and the first day of ECT) and the number of lines of treatment received consecutively (in monotherapy or in combination) before the initiation of ECT were collected. The reasons for using ECT as previously described, specifically first-line indications, based on international guidelines, were also recorded rating retrospectively the charts of the 335 patients [10,11,12,13]. We chose the first line indications as suggested in Canadian [12] and Australian / New Zealand [11, 13] guidelines and confirmed in a review focusing on different mood disorder guidelines [10].
Statistical analysis
Sociodemographic and clinical data are presented as the mean (SD) for continuous variables and frequency distribution for categorical variables (n, %).
Statistical comparisons between groups of patients were done by using standard statistical tests: the Chi-square test for categorical variables and Student t test, Anova test or Mann–Whitney test, depending on the number and distribution of continuous variables. The distribution was tested with Kernel estimation (Supplementary Fig. 1 and 2).
Analyses were conducted using SAS 9.3 (SAS Statistical Institute, Cary, North Carolina). All statistical tests were 2-tailed, with the α level set at 0.05.
Results
We identified 335 patients aged 65 year or over who commenced ECT for treatment of MDE (MDD or BD) according to DSM-IV-TR criteria. Age, sex and clinical characteristics are presented in Table 1.
The mean duration of MDE before ECT was 8.88 (12.03) months. We found a significant shorter duration of MDE in patients with BD compared to MDD (p = 0.005) (Table 2). In addition, it seemed that the occurrence of single MDE in MDD increases the duration of MDE before ECT (mean duration = 13.75 months, SD = 13.77) in comparison with recurrent MDE (mean duration = 8.67 months, SD = 11.00) or BD (mean duration = 6.90, SD = 8.88; F = 7.4213, p < 0.001). The previous number of MDEs reduces the duration before ECT in the whole sample (p < 0.001) and mainly, in the MDD group (p < 0.01). Moreover, the co-occurrence of other chronic medical diseases increased the duration before ECT in the MDD group (Table 2).
The presence of first-line indications for using ECT from guidelines did not reduce the duration of MDE before ECT (Table 3), except for previous response to ECT (p < 0.001). However, the first-line indications reduced the number of lines of treatment before starting ECT (Fig. 1).
Discussion
To our knowledge, this is the first study focusing on the adherence to guidelines for using ECT in the elderly population focusing on the duration of MDE and the number of treatments before ECT. In this population, the mean duration of MDEs before ECT was 9 months. This duration is in line with data on adult patients with MDE [14]. Unlike this study, the presence of first-line indications for using ECT from guidelines, such as the presence of psychotic or catatonic features, urgency (e.g., poor oral intake), high suicidality, or patient preference did not reduce the delay before ECT in our elderly population. However, a previous response to ECT reduced the delay before ECT. The lack of difference between the presence and the absence of first-line indications for using ECT, in elderly population, could be explained by the fact that the delay in case of the absence of the first line indications seems shorter in this population compared to the adult population [14].
However, these first-line indications reduced the number of treatments tested before ECT.
Unexpectedly, the delay before ECT was significantly longer for MDD patients with comorbid chronic physical diseases. This could be explained, in part, by psychiatrists’, anaesthetists’, and geriatric practitioners’ concerns about the safety of ECT in these patients. The management of these physical comorbidities may also have delayed the management of MDE in hospitals providing ECT.
Although there is an important delay before management of BD after the onset of the disease [19], we highlighted a difference focusing on the delay before ECT between MDD and BD. In our elderly population, it seems that once correctly diagnosed, patients with BD access ECT more quickly than patients with MDD. Moreover, it seems that patients with recurrent episodes benefit from ECT earlier than those with a single episode. Indeed, the occurrence of previous MDE reduces the duration before ECT. However, we did not find these results in the BD group, probably due to the small number of patients in our cohort with a late life onset episode (only one). Therefore, it seems difficult to interpret these analyses. Better knowledge of the disorder and, in case of a similar episode, a lack of the need for further examination (in order to search for a neurological disorder such as dementia) could explain this difference.
However, the reasons for the long delay before ECT are more difficult to explain in the elderly population except by three points: i) the uncertain or negative attitudes of patients towards ECT [20], ii) the choice/practice of the psychiatrist, and mainly, the difficulties of changing prescription habits despite recommendations, whatever the type of treatment [21] and iii) the difficulties of access to this therapeutic strategy [22, 23] and the lack of relevant training of health professionals [22]. Indeed, a recent meta-analysis showed that old age was a predictor of response and remission focusing on ECT [5]. Moreover, despite the stigma, it is now well established that ECT is safe and well tolerated, especially in the elderly population [24]. It is a safe alternative to pharmacotherapy (which can generate side effects leading to early discontinuation) [24]. Moreover, ECT does not worsen the course of dementia, and is indicated for comorbid depression and agitation in dementia [3]. Therefore, ECT should be used more quickly, mainly in this population, because MDE can lead to death by suicide [25], particularly in the elderly population and it is the first cause of functional disability and poor quality of life [26, 27].
There are some limitations to this work. First, not all health care facilities practicing ECT in France participated in this study. This could limit the extrapolation of results. Second, this is a retrospective study in which data may potentially be missing from medical files. Moreover, it is difficult to assess urgency criteria retrospectively.
Conclusion
Even if ECT seems to be a key treatment in the elderly population due to its efficacy and safety for MDEs, the delay before this treatment might be too long, probably due to factors such as the capacity for ECT that is very sparse in France and the uncertain or negative attitudes of patients towards ECT. MDEs can, firstly, lead to death by suicide, particularly in the elderly population and, secondly, it is the first cause of functional disability and poor quality of life. Therefore, improving knowledge of the practice of ECT of psychiatrists and facilitating accessibility to ECT, especially in the elderly population, should represent a major public health concern.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
References
Pagnin D, de Queiroz V, Pini S, Cassano GB. Efficacy of ECT in depression: a meta-analytic review. J ECT. 2004;20:13–20.
UK Ect Review Group. Efficacy and safety of electroconvulsive therapy in depressive disorders: a systematic review and meta-analysis. Lancet. 2003;361:799–808.
Meyer JP, Swetter SK, Kellner CH. Electroconvulsive therapy in geriatric psychiatry: a selective review. Clin Geriatr Med. 2020;36:265–79.
Østergaard SD, Speed MS, Kellner CH, Mueller M, McClintock SM, Husain MM, et al. Electroconvulsive therapy (ECT) for moderate-severity major depression among the elderly: data from the pride study. J Affect Disord. 2020;274:1134–41.
van Diermen L, van den Ameele S, Kamperman AM, Sabbe BCG, Vermeulen T, Schrijvers D, et al. Prediction of electroconvulsive therapy response and remission in major depression: meta-analysis. Br J Psychiatry J Ment Sci. 2018;212:71–80.
Eranti SV, McLoughlin DM. Electroconvulsive therapy - state of the art. Br J Psychiatry J Ment Sci. 2003;182:8–9.
Leiknes KA, Jarosh-von Schweder L, Høie B. Contemporary use and practice of electroconvulsive therapy worldwide. Brain Behav. 2012;2:283–344.
Sienaert P, Falconieri T, Obbels J, van den Ameele H, Bouckaert F. Improving practice in electroconvulsive therapy: a nationwide survey in Belgium. J ECT. 2016;32:29–32.
Chatham AN, Shafi H, Hermida AP. The use of ECT in the elderly-looking beyond depression. Curr Psychiatry Rep. 2022;24:451–61.
Bayes AJ, Parker GB. Comparison of guidelines for the treatment of unipolar depression: a focus on pharmacotherapy and neurostimulation. Acta Psychiatr Scand. 2018;137:459–71.
Malhi GS, Bassett D, Boyce P, Bryant R, Fitzgerald PB, Fritz K, et al. Royal Australian and New Zealand College of Psychiatrists clinical practice guidelines for mood disorders. Aust N Z J Psychiatry. 2015;49:1087–206.
Milev RV, Giacobbe P, Kennedy SH, Blumberger DM, Daskalakis ZJ, Downar J, et al. Canadian Network for Mood and Anxiety Treatments (CANMAT) 2016 Clinical Guidelines for the Management of Adults with Major Depressive Disorder: Section “Discussion”. Neurostimulation Treatments. Can J Psychiatry Rev Can Psychiatr. 2016;61:561–75.
Weiss A, Hussain S, Ng B, Sarma S, Tiller J, Waite S, et al. Royal Australian and New Zealand College of Psychiatrists professional practice guidelines for the administration of electroconvulsive therapy. Aust N Z J Psychiatry. 2019;53:609–23.
Samalin L, Yrondi A, Charpeaud T, Genty JB, Blanc O, Sauvaget A, et al. Adherence to treatment guidelines in clinical practice for using electroconvulsive therapy in major depressive episode. J Affect Disord. 2020;264:318–23.
Mallet L, Spinewine A, Huang A. The challenge of managing drug interactions in elderly people. Lancet Lond Engl. 2007;370:185–91.
Dominiak M, Antosik-Wójcińska AZ, Wojnar M, Mierzejewski P. Electroconvulsive therapy and age: effectiveness, safety and tolerability in the treatment of major depression among patients under and over 65 years of age. Pharm Basel Switz. 2021;14:582.
Henry C, Etain B, Mathieu F, Raust A, Vibert J-F, Scott J, et al. A French network of bipolar expert centres: a model to close the gap between evidence-based medicine and routine practice. J Affect Disord. 2011;131:358–63.
Yrondi A, Bennabi D, Haffen E, Garnier M, Bellivier F, Bourgerol T, et al. Significant need for a French network of expert centers enabling a better characterization and management of treatment-resistant depression (Fondation FondaMental). Front Psychiatry. 2017;8:244.
Dagani J, Signorini G, Nielssen O, Bani M, Pastore A, de Girolamo G, et al. Meta-analysis of the interval between the onset and management of bipolar disorder. Can J Psychiatry. 2017;62:247–58.
Griffiths C, O’Neill-Kerr A. Patients’, Carers’, and the Public’s perspectives on electroconvulsive therapy. Front Psychiatry. 2019;10:304.
Gallini A, Andrieu S, Donohue JM, Oumouhou N, Lapeyre-Mestre M, Gardette V. Trends in use of antipsychotics in elderly patients with dementia: Impact of national safety warnings. Eur Neuropsychopharmacol J Eur Coll Neuropsychopharmacol. 2014;24:95–104.
Delva NJ, Graf P, Patry S, Gosselin C, Milev R, Gilron I, et al. Access to electroconvulsive therapy services in Canada. J ECT. 2011;27:300–9.
Lin Y, Tootoo J, Allen MK, Pinjari OF, Soares JC, Selek S. Geographical access to electroconvulsive therapy services in Texas. J Affect Disord. 2019;245:1135–8.
Geduldig ET, Kellner CH. Electroconvulsive therapy in the elderly: new findings in geriatric depression. Curr Psychiatry Rep. 2016;18:40.
Beghi M, Butera E, Cerri CG, Cornaggia CM, Febbo F, Mollica A, et al. Suicidal behaviour in older age: a systematic review of risk factors associated to suicide attempts and completed suicides. Neurosci Biobehav Rev. 2021;127:193–211.
McCall WV, Cohen W, Reboussin B, Lawton P. Effects of mood and age on quality of life in depressed inpatients. J Affect Disord. 1999;55:107–14.
McCall WV, Reboussin D, Prudic J, Haskett RF, Isenberg K, Olfson M, et al. Poor health-related quality of life prior to ECT in depressed patients normalizes with sustained remission after ECT. J Affect Disord. 2013;147:107–11.
Acknowledgements
Fondation Fondamental’s team
Funding
This work was supported by the French Society for Biological Psychiatry and Neuropsychopharmacology (AFPBN, www.afpbn.org).
The funders had no further role in design study, data collection analysis and interpretation, writing of the report, and the decision to submit the paper for publication.
Author information
Authors and Affiliations
Contributions
AY, LS: Formal analysis, Investigation, Methodology, Validation, Visualization, Writing—original draft, Writing—review & editing. OB: Formal analysis, Investigation, Methodology, Validation, Visualization, Writing-review & editing. LA, PML: Investigation, Methodology, Validation, Visualization, Writing-review & editing, CA, LB, MCP, AA, TC, JBG, RA, MR, RR, BA, DB, WEH, BE, JH, ML, FM, RMR, FS, GV, AS, EP, EH, PC, PF: Investigation, Validation, Visualization, Writing-review & editing.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The assessment protocol was approved by the relevant ethical review board (CPP Sud-Est VI, 2016 / CE 07). This a retrospective study. All data were collected anonymously.
All patients who were hospitalized, are informed and consent that their data could be used retrospectively for research.
Consent for publication
All patients who were hospitalized, are informed and consent that their data could be used retrospectively for research.
Competing interests
Pr. Samalin has received personal fees and/or non-financial support from Janssen, Lundbeck and Otsuka.
Pr Yrondi has received speaker's honoraria (AstraZeneca, Janssen, Lundbeck, Otsuka, Servier), carried out clinical studies in relation to the.
development of a medicine (Janssen) unrelated to this work.
Dr Genty has received speaker's honoraria from Servier.
Pr Sauvaget has received personal fees and/or non-financial support from Janssen, and Lundbeck.
Pr Poulet has received personal fees and/or non-financial support from Janssen, EISAI, Otsuka and Lundbeck.
Dr Holtzmann has received personal fees and/or non-financial support from Janssen and Lundbeck.
Pr Richieri has received speaker's honoraria from Otsuka and Janssen-Cilag. She has served on advisory boards for LivaNova.
Pr El-Hage has received speaker's honoraria from CHUGAI, EISAI, Lundbeck, Janssen-Cilag, and UCB unrelated to this work. He served on advisory boards for Janssen-Cilag and Lundbeck.
Pr Aouizerate has received speaker's honoraria from Lundbeck,Lilly, and Janssen-Cilag. He has served on advisory boards for Janssen-Cilag.
Pr Haffen acted in advisory capacities, carried out clinical studies inrelation to the development of a medicine, received personal researches,studies or travel allowance, gave presentations at meetings, and received remuneration for input from the following pharmaceutical organisations: AstraZeneca, BMS, Cellgene, Euthérapie—Servier, Janssen, Elli Lilly, Lundbeck, LivaNova, Otsuka, Pfizer, Sanofi.
Pr Llorca has received grants, honoraria, or consulting fees fromESAI, Gedeon Richeter, Janssen, Lundbeck, Otsuka and Sanofi.
No potential conflict of interest was reported by the other authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yrondi, A., Blanc, O., Anguill, L. et al. Adherence to clinical practice guidelines for using electroconvulsive therapy in elderly depressive patients. BMC Psychiatry 24, 487 (2024). https://doi.org/10.1186/s12888-024-05933-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12888-024-05933-7