Abstract
Background
The underlying neurobiology of the complex autism phenotype remains obscure, although accumulating evidence implicates the serotonin system and especially the 5HT2A receptor. However, previous research has largely relied upon association or correlation studies to link differences in serotonin targets to autism. To directly establish that serotonergic signalling is involved in a candidate brain function our approach is to change it and observe a shift in that function.
We will use psilocybin as a pharmacological probe of the serotonin system in vivo. We will directly test the hypothesis that serotonergic targets of psilocybin – principally, but not exclusively, 5HT2A receptor pathways—function differently in autistic and non-autistic adults.
Methods
The ‘PSILAUT’ “shiftability” study is a case–control study autistic and non-autistic adults. How neural responses ‘shift’ in response to low doses (2 mg and 5 mg) of psilocybin compared to placebo will be examined using multimodal techniques including functional MRI and EEG. Each participant will attend on up to three separate visits with drug or placebo administration in a double-blind and randomized order.
Results
This study will provide the first direct evidence that the serotonin targets of psilocybin function differently in the autistic and non-autistic brain. We will also examine individual differences in serotonin system function.
Conclusions
This work will inform our understanding of the neurobiology of autism as well as decisions about future clinical trials of psilocybin and/or related compounds including stratification approaches.
Trial registration
NCT05651126.
Similar content being viewed by others
Background
Autism spectrum disorder (hereafter referred to as ‘autism’) is a neurodevelopmental condition characterised by differences in social interaction and communication, repetitive or restricted patterns of behaviour, and sensory differences [1]. Although the neurobiological underpinnings of the diverse autistic phenotype remain obscure, accumulating evidence strongly supports involvement of the serotonin system. Identifying differences in the serotonin system in autistic individuals may reveal novel mechanisms to be targeted pharmacologically to benefit those who seek support.
The serotonin system in autism
There is increasing evidence from association and/or correlation studies linking serotonin to autism. First, polymorphisms in genes for serotonin synthesis, transporters and receptors are associated with autism [2, 3]. Second, elevated whole blood serotonin levels are also reported in one-third of autistic individuals [4, 5]. Third, our team has previously reported that acutely elevating serotonin levels with a single dose of selective-serotonin reuptake inhibitor (SSRI) citalopram differentially affects autistic brain function. For example, citalopram produces sustained activation of brain regions associated with facial expression processing in autistic adults, but not in controls [6].
More specifically, there is also evidence implicating specific serotonin receptors in autism, especially the 5HT2A receptor. This receptor is involved in dendritic maturation, neuronal differentiation and the regulation of brain-derived neurotrophic factor levels during development [7]. At the circuit level, 5HT2A receptor signalling is thought to enhance neural plasticity [8] and increases cortical glutamate and thalamic GABA levels [9]. The receptor is expressed throughout the cortex but especially in regions related to sensorimotor integration [10] and the so-called default mode network responsible for “self” and “other” processing [11]. Thus, through these key processes that shape neuronal architecture and neurotransmission, serotonin influences lower-order systems (e.g. sensory) through to higher-order processes (e.g. whole-brain connectivity) as they emerge. As a result, early perturbations in the serotonin system, such as alterations in 5HT2A receptor-signalling, may influence subsequent brain developmental outcomes. Indeed the HT2RA gene is a candidate gene associated with autism [12,13,14,15]. However, although lower cortical 5HT2A receptor binding has been reported to correlate with social communication differences in autism [16], to date there have been no studies that have directly tested whether 5HT2A receptor pathways function differently in autistic and non-autistic people.
Measuring ‘Shift’ in the serotonin system in autism
To do this, we have developed a ‘“shiftability” paradigm [17] to examine how ‘foundational’ mechanisms of brain function such as neural responses to sensory stimuli or whole-brain network connectivity captured using electroencephalography (EEG) and functional magnetic resonance imaging (fMRI) are modulated by targeted pharmacological probes. These measures are biologically informative and may be used across a wide range of ages and, in many cases, also back-translate to animal models to inform future target identification and engagement studies [18,19,20,21,22,23].
The range of measures used to capture ‘shift’ and their target level of brain organisation is shown in Fig. 1.
The organisational levels of information processing in the brain and methodologies that probe each level. Methodologies used to detect ‘shift’ that are included in our ‘PSILAUT’ protocol and discussed here are shown in bold. Bidirectional arrows represent interaction between organisation levels (adapted from Ahmad & Ellis, 2022 [24])
Targeting 5HT2A receptor in autism using psilocybin
The only way to directly test if a neurosignalling system functions differently in one group of individuals compared to another is to experimentally manipulate it (for example using a pharmacological probe) and observe a ‘shift’ in function. In humans unlike preclinical model systems, it is of critical importance that the choice of pharmacological probe is safe and has minimal side effects. However, few (if any) neuropsychiatric drugs used in people are entirely specific in their biological effects. With this caveat in mind, in this protocol we selected psilocybin (4-phosphoryloxy-N.N-dimethyltryptamine), as a pharmacological probe of the 5HT2A receptor in autistic and non-autistic adults.
Psilocybin is a classic psychedelic compound produced by several species of mushrooms, including so-called “magic mushrooms”. Psilocybin is rapidly metabolised into its active component psilocin [25]. Psilocin is a 5HT2A receptor agonist but also binds several serotonin receptors, including 5HT7, 5HT2B, 5HT1D, 5HT6, 5HT5, 5HT2C & 5HT1B receptors in decreasing order of reported affinity [26]. Prior studies have used relatively high doses of psilocybin to explore the effects of psychedelics on the brain. However, in the planned study we will use lower doses (2 mg and 5 mg) in our “shiftability” protocol to assess brain responses so as not to cause a marked psychedelic experience. This dose range is expected to generate a ‘shift’ in brain function based on evidence using positron emission topography that similar doses of psilocybin engage 5HT2A receptors [27]; and low dose psilocybin has been shown to be sufficient to alter cognition and obsessive–compulsive behaviour [28, 29]. Low doses of the serotonergic psychedelic lysergic acid diethylamide (LSD) and psilocybin-containing mushrooms also acutely alter brain resting-state fMRI and EEG indices in the non-autistic population [30, 31], as well as neural responses to sensory stimuli [32]. Therefore, we expect that 2 mg and 5 mg of psilocybin will expose functional differences in the serotonin system targeted by psilocybin in autistic and non-autistic individuals using the experimental medicine approach outlined in this protocol.
Overall design of the ‘PSILAUT’ study
The study is an Investigator-Initiated Study sponsored by King’s College London and co-Sponsored by South London and Maudsley NHS Foundation Trust (SLaM). It is part funded by COMPASS Pathfinder Ltd with infrastructure support from the NIHR-Maudsley Biomedical Research Centre at South London and Maudsley NHS Foundation Trust and King’s College London. COMPASS Pathfinder Ltd are donating psilocybin (as “COMP360”). The study is a case–control study with a pseudo-randomised, double-blind, placebo-controlled, cross-over design. We have capacity to recruit up to 70 adult participants to accommodate participant drop-out and/or data quality screening with the goal of n = 30 autistic adults (half female) and n = 30 non-autistic adults (half female), who will be matched by age and sex. All participants will provide written informed consent. Participants will be asked to attend 3 visits in total and on each visit they will receive either placebo or one of two single doses (2 mg or 5 mg) of oral synthetic COMP360 psilocybin. Participants and the researchers accompanying the visit will be blind to allocation. The order of administration of placebo and psilocybin will also be pseudo-randomised by the Chief Investigator using a randomisation tool to help generate a list (e.g. Random.org, Randomness and Integrity Services Ltd.) then modified manually to ensure a reasonable balance of individuals in each cell are allocated each of the 3 possible administration orders throughout the duration study (for example, to avoid a ‘run’ of placebo first visits, should different groups/sexes be harder to recruit and result in different cell sizes). Thus, there are 3 possible orders of administration allocated:
-
1.
Visit 1, placebo; Visit 2, 2 mg psilocybin; Visit 3, 5 mg psilocybin
-
2.
Visit 1, 2 mg psilocybin; Visit 2, 5 mg psilocybin; Visit 3, placebo
-
3.
Visit 1, 2 mg psilocybin; Visit 2, placebo; Visit 3 5 mg psilocybin
The lowest dose of psilocybin will always precede the higher dose. This allows us to unblind in the case of unwanted side effects (such as a significant increase in blood pressure) or unwanted experience and potentially omit the higher dose visit. We also explain that there will be more chance of side effects with the higher dose in our informed consent process and if a participant only wishes to attend for the placebo and lower dose visit, we can exclude the higher dose from the randomisation (i.e. they would attend a total of 2 visits only). Thus, a ‘drop-out’ would be considered a participant that did not attend all 3 visits and has missing data for at least one condition.
Ethical considerations
This study will take place at the Institute of Psychiatry, Psychology and Neuroscience (IoPPN) at De Crespigny Park, SE5 8AF, London, United Kingdom. Our study does not address safety or clinical efficacy and the UK Medicines and Health Regulatory Authority (MHRA) has confirmed that our protocol is therefore not a clinical trial of an Investigational Medicinal Product (IMP) as defined by the EU Directive 2001/20/EC.
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2013. All procedures involving human participants were approved by Dulwich Research Ethics Committee (Reference: 21/LO/0795) and the study protocol was peer reviewed during the ethical review process. As clinicaltrials.gov accepts a range of study designs, because definitions of study types using pharmacological probes differ in different jurisdictions, and in the interest of transparency, we have preregistered the study (Identifier: NCT05651126). We emphasize that in this study, to ensure individuals can provide full informed consent, we will be recruiting autistic and non-autistic adults without intellectual disability and the doses of psilocybin used will be low to limit likelihood of marked psychedelic experiences.
Community engagement
Community engagement was led by the Autism Research Centre at Cambridge University in 2019, prior to designing the study. Three hundred and thirty-one autistic adults were asked about their attitudes to psilocybin research in autism. It was made clear that the research team were not aiming to ‘treat’ autism itself and that the research would not proceed if there was not clear support for it from the autism community. The majority of respondents supported exploratory studies using psilocybin.
Of the 331 autistic adult respondents, 41% were ‘very interested’ and 28% were ‘somewhat interested’. For example: “I am very interested in helping with pioneering new approaches… and feel it is high time proper research was done in this area”. There was also caution however as 25% were ‘not interested’ or ‘not at all interested’. Therefore, rather than proceed immediately to a conventional clinical trial, this study was designed to provide further information on the brain functions targeted by low dose psilocybin and understand any differences between autistic and non-autistic adults. Our hope is that this study will establish a firmer neurobiological evidence base to inform potential opportunities for the development of psilocybin as a pharmacological support option.
Stakeholder engagement also included a press release by King’s College London, South London and Maudsley NHS Foundation Trust and COMPASS Pathways (https://ir.compasspathways.com/news-releases/news-release-details/compass-pathways-fund-study-comp360-psilocybin-autistic-adults), as well as articles and interviews across several platforms including The Economist (https://www.economist.com/psychedelics-pod), Psychology Today [33], Technology Networks [34] and The BBC (https://www.bbc.co.uk/programmes/m001j45x), which received positive feedback. Study findings will be continue to be widely disseminated in forums, publications and presentations involving stakeholders in the autistic community, study participants, researchers, industry and clinicians (Fig. 2).
'PSILAUT' recruitment and study procedures. Autistic and non-autistic participants will be recruited from existing local research databases, advertising on the King’s College London website and wider dissemination of study information. Participants are welcome to self-refer. Autistic participants will also be recruited from clinical contacts from South London and Maudsley NHS trust, local and national support groups and via the Cambridge Autism Research Database (CARD), managed by our collaborators at the Autism Research Centre, University of Cambridge. Interested participants will be sent an information sheet and screened via video call or phone for eligibility according to the inclusion and exclusion criteria prior to the first visit. Written consent will be sought after inclusion criteria are confirmed and the participant is then assigned to a study schedule. Participants will be provided with login details to an online platform (Delosis Ltd., London) to complete a battery of questionnaires remotely. Participants will visit the study site on three separate occasions. A blood sample will be collected on one of the three visits for quantification of whole blood serotonin levels. Each participant will complete an MRI scan session to acquire a structural, resting-state functional MRI scan and a face emotion processing task. The EEG paradigm will include resting-state and functional activation during a face processing, auditory oddball and visual processing. Psychophysical tasks will be collected prior to a cognitive battery which will include the ‘reading the mind in the eyes’ (RMET), probabilistic reversal learning (PRT), both of which will be delivered using PsyTools (Delosis Ltd., London) and a semantic verbal fluency task. The 5-dimensional altered states of consciousness (5D-ASC) questionnaire will then be completed to quantify any subjective effects experienced by participants
‘PSILAUT’ protocol measures
Each study visit will last approximately 4–5 h in total. Although given the number of measures, the data collected is time permitting and cognitive tasks at the end of the protocol may be omitted, for example. We will aim to collect spectroscopy and resting-state MRI at 60min and 70min post-dose at Tmax [27], respectively; EEG at ~ 2 h post-dose & psychophysics at ~ 3 h post-dose. We have established the tolerability and feasibility of this study design in autistic adults as we have conducted similar studies previously with several different pharmacological probes [6, 21, 35,36,37,38]. Indeed, many of our participants have also attended our studies in the past and are well-informed about the visit procedures.
Inclusion & exclusion criteria
A comprehensive baseline characterisation will be obtained. An expert clinical diagnosis of autism from a recognised UK assessment service will be accepted. This may be supported by the Autism Diagnostic Interview-Revised [39] where an appropriate informant is available. An Autism Diagnostic Observation Schedule [40] will be used to support diagnosis, but if it has already been used to inform the diagnostic assessment in adulthood, it will not be repeated. Participants with ASD of a known genetic cause (e.g. Fragile X syndrome) were excluded. Other inclusion criteria include being over 18 years old; the ability to provide informed consent; no cooccurring psychiatric illness such as major mood disorder or psychotic illness; no history of seizures or diagnosis of epilepsy and no physical illness such as high blood pressure. Participants taking medications known to affect serotonin (such as selective serotonin-reuptake inhibitors) will be excluded. Those taking stimulants will be eligible and asked to ideally exclude on the day of testing or else ensure they take it the same way on each visit. These and any other potential medication use will be included as covariates in analyses and/or statistical analyses rerun excluding data from individuals taking medication to establish the extent to which medication use drives any potential findings.
Baseline characterisation
Additional baseline questionnaires will quantify autistic traits (e.g. social behaviour or sensory differences), relevant cognitive domains (e.g. intolerance of uncertainty and behavioural flexibility) and the symptomology of co-occurring psychiatric conditions.
Neurometabolites
Magnetic Resonance Spectroscopy (MRS)
An MRS Hadamard Encoding and Reconstruction of MEGA-Edited Spectroscopy (HERMES) sequence [41] will be collected during the MRI scan for the dorsal medial prefrontal cortex region. HERMES permits the quantification of levels of metabolites in the living brain and is focused on estimating GABA and Glutamate-glutamine markers of E/I balance. For the purposes of our study, given the evidence that E-I pathways are modulated by 5HT2A receptor action in animal models [9], we will be able to examine the impact of psilocybin on these tissue level measures of E-I balance.
Local circuits
EEG
Resting-state
High-density (64-channel) EEG data will be collected during the resting-state, metrics from which local circuit activity can be derived such as beta and gamma band power/frequency [24]. Oscillations in the beta frequency band at rest, for example, are associated with inhibitory neurotransmitter levels in sensorimotor cortex [42]. This, and other EEG-derived metrics such as aperiodic activity, are considered a proxy measure for E/I balance in vivo [24]. Hence, we will be able to examine the impact of psilocybin on these dynamic measures of E/I balance.
Passive sensory tasks
Visual domain
A visual processing task (contrast saturation) in which steady-state evoked potentials (SSVEPs) are elicited by passive surround suppression stimuli will be conducted. We have shown that SSVEPs during this task are altered in autism [21]. 5HT2A receptors are particularly highly expressed in the primary visual cortex [11], and their agonism alters visual response amplitudes and surround suppression in mouse primary visual cortex [43]. In humans, we expect visual processing to be altered by 5HT2A receptor activation given that the marked visual perceptual changes robustly induced with higher doses of psychedelics are blocked by pretreatment with the 5HT2 receptor antagonist, ketanserin [44].
Auditory domain
A conventional auditory oddball paradigm of mismatch negativity (MMN) [45] will be used to passively measure ‘repetition suppression’ (or habituation) to repetitive auditory stimuli and response to an unexpected ‘deviant’ stimulus (the event-related mismatch negativity MMN response). We and others have observed less repetition suppression in both eight-month-old infants who go on to receive a diagnosis or autism, and adults with a diagnosis of autism [19, 46]. Thus, this signal appears linked to autism across infancy to maturity. The impact of autism on the event-related MMN is less consistent and varies with age [47,48,49]. The latter may in part be due to differences in the serotonin system, as the MMN response can be modulated by acute elevation of serotonin levels by the highly selective SSRI escitalopram [50]. In this study we will test the prediction that psilocybin alters both sensory suppression and MMN in autism differently compared to controls.
Global networks
Resting-state
EEG
Oscillatory power will be assessed across multiple frequency bands during the resting-state. This will include electrodes over key brain regions implicated in autism such as those belonging to the default mode network (DMN) [51]. Reduced oscillatory power over DMN regions using electrophysiological approaches following 5HT2A receptor activation by psilocybin has been reported previously [52]. Functional connectivity analyses (e.g. within and between brain networks) can also be derived from EEG, and this will complement connectivity analyses from resting-state fMRI.
MRI
Participants will undergo a structural and functional MRI scan. Scans will be acquired on a 3.0 Tesla MR Scanner (General Electric Premier). A fMRI scan with a multiband 4 sequence will be acquired during the resting-state, multiband 4 is preferable for connectivity analyses [53]. In addition, multiband sequences will considerably reduce the repetition time (TR), therefore they have the advantage of allowing dynamic functional connectivity analyses. Autistic differences in both ‘averaged’ functional connectivity and dynamic functional connectivity have been reliably reported across different datasets [20, 54]. Functional connectivity of brain networks in neurotypical individuals has also be shown to be acutely modulated by 5HT2A receptor activation [55]. Notably, psilocybin alters dynamic functional connectivity, mediated by 5HT2A receptor agonism [56]. It facilitates state transitions and more temporally diverse brain activity in neurotypical individuals[57]. Our study will be the first to examine the effects of psilocybin on conventional and dynamic functional metrics in autistic individuals.
Task-dependent MRI and EEG
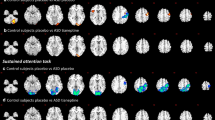
MRI
fMRI studies of face emotion processing in autism have produced inconsistent results. In the largest study to date, no differences between autistic and non-autistic individuals in fMRI response to facial expressions of emotion were observed [58]. However, we have recently examined the fMRI response to facial expressions of emotion in a social brain network before and after administration of the SSRI, citalopram. We reported that the dynamics of the response to faces is different in autism, in that serotonin reuptake inhibition slows habituation [6]. Consistent with this, blockade of 5HT2A receptors causes an ‘opposite’ effect and reduces neural responses to emotional faces during fMRI in neurotypical individuals [59]. Therefore, we expect that psilocybin will alter the dynamics of face emotion processing, but differently in autistic individuals.
EEG
Event-related potentials (ERPs) in response to face stimuli will also be assessed during EEG. The N170 component, a neural response present at 170ms following the presentation of facial stimuli and can be modulated by 5HT2A receptor activation [44, 60, 61]. An altered N170 response is associated with social communication differences in autism and may have utility as a stratification marker that is amenable to support [62]. It is also going to be the first prognostic biomarker for autism (or any neurodevelopmental or psychiatric condition) to be approved by regulatory agencies [62]. The incorporation of this task in our protocol therefore will be an important test of whether an autism biomarker can be modified pharmacologically.
Perception
Psychophysical approaches are structured approaches in which stimulus characteristics are tightly controlled, and they provide robust, objective measures of sensory sensitivity by estimating perceptual metrics [63, 64]. Serotonin has been directly implicated in tactile perception, such as in affective touch, by studies using tryptophan depletion (which acutely reduces central serotonin levels) alongside psychophysical approaches [65]. Tactile detection threshold and amplitude discrimination will be assessed, as differences in tactile thresholds have already been reported in autism and are associated with outcomes [66]. As processing of tactile stimuli is also known to be perturbed by 5HT2A receptor agonism with psilocybin [67], we also expect to elicited functional differences following psilocybin in autistic and non-autistic individuals in this paradigm.
Additional measures
Questionnaires
The 5-dimensional altered states of consciousness (5D-ASC) questionnaire [68] will be completed on each visit following the completion of study procedures to quantify the subjective effects of psilocybin, which are primarily mediated by the 5HT2A receptor [69].
Cognitive battery
‘Theory of mind’ (i.e. cognitive empathy, the ability to understand and take into account the mental state of another individual) can be investigated using the ‘reading the mind in the eyes’ (RMET) task [70]. Other cognitive processes in which differences are observed in autism such as language and executive and reward-related functioning (e.g. flexible choice behaviour) will be assessed with a verbal fluency task and probabilistic reversal learning task, respectively [71, 72].
Peripheral biochemistry
Participants will be asked to provide a blood sample on one visit prior to placebo/drug administration (their preference). Whole blood serotonin levels will be determined for each individual, given that elevated levels are present in one-third of individuals with autism [4, 5]. This will allow us to explore whether any ‘shift’ in brain function in response to psilocybin depends on overall serotonin ‘tone’ as indexed by proxy.
Data analyses
The overarching goal of our analyses is to assess whether we see a ‘shift’ by psilocybin in autistic and non-autistic individuals for each modality. Both parametric and nonparametric statistical analyses will be used to test hypotheses that the serotonergic targets of psilocybin functioning differently in autistic individuals. Given the heterogeneity of the autistic population and our prior observations that there is a wide range of pharmacological responses in both autistic and non-autistic individuals, we will calculate individual ‘shift’ for each modality, and what characteristics (e.g. clinical scores, questionnaire responses, whole blood serotonin) these are associated with. Although we will generate and analyse data from single modalities, post-hoc we will also explore multimodal metrics (i.e. associations between modalities) to understand how ‘shifts’ detected across multiple organisational levels are inter-related.
Power analyses
We will use a within-subject, repeated-measures design with a placebo condition so that each subject is their own control, thus increasing statistical power. Results from our prior neuroimaging studies using pharmacological challenge were successful in detecting group differences in MRI metrics with sample sizes of n = < 20 [6, 35,36,37,38, 73,74,75]. This implies an effects size (expressed as Cohen’s d) in excess of 1.2. In sensory tasks a sample size of n = 16 per cell is estimated to achieve 80% power to detect a medium effect (0.5) at a = 0.05; this has been achieved even in mixed sex groups of 20 participants or fewer. This reflects the literature in which significant group differences are evident even in mixed sex groups of 20 participants or fewer (e.g. n = 16) [76,77,78]. Nevertheless, we aim for n = 30 per group (approximately half female in both groups). Our design relies upon participants attending for repeat test sessions. Thus, there is a chance that participants may ‘drop-out’ and need to be replaced, this is accommodated with our ethically approved total sample size of n = 70.
Limitations
Our protocol requires active participation despite the passive nature of several of our tasks. For example, participants will wear an EEG cap and will be asked to remain focused on the screen during the presentation of sensory stimuli. This may limit generalisability across ages or to autistic individuals with higher support needs.
Even in the proposed adult cohort, participants may get restless or become distracted. Hence, we have included concurrent eye tracking during EEG to control for the potential confound of participant variability in fixation on the screen. However, many of our tasks require minimal or no response from participants and so they are less likely to be impacted by confounds such as individual cognitive difficulties. We hope that this way, should our indices prove worthy of further investigation and/or incorporation in (for example) clinical trials, they will be more accessible for individuals who may otherwise be excluded from drug development studies.
Discussion
Our “shiftability” paradigm aims to determine how different organisational scales of brain function are modulated by the serotonin system, in particular the 5HT2A receptor pathway when activated by psilocybin. It will test the hypothesis that the serotonin system targeted by psilocybin is different in autistic and non-autistic people. The results will expand our understanding of brain biology in autistic and non-autistic individuals.
Our work will inform a more personalized medicine approach to autism. Not everyone in our study will respond the same way to psilocybin. Whilst our study design may reveal differences in the response to psilocybin at the group-level, crucially, our prior studies have shown that its constituents are also sensitive to the potential variability at the individual-level. For example, we have been able to plot individual ‘shifts’ in GABA and glutamate spectroscopy, task-dependent and resting-state fMRI measures in response to several drug challenges [6, 36,37,38, 74], and calculated an individual ‘sensitivity index’ across the different sensory modalities examined in response to a GABA challenge [21, 46]. Thus, by investigating individual biology in both autistic and non-autistic people, this experimental medicine approach may help identify autistic individuals whose serotonin system functions no differently from non-autistic people, and who might therefore not be expected to show a clinical response in a clinical trial. And vice versa; those who respond biologically to psilocybin challenge might ultimately benefit clinically. To date, all clinical trials for the core features of autism have failed to reach their primary endpoint. This is in large part because they have included participants based on diagnosis alone and measured outcomes, often without evaluating mechanisms in the same cohort. Existing pharmacological options available for autistic people that target the serotonin system are mainly selective serotonin reuptake inhibitors (reviewed in Howes et al., 2017 [79]). These show limited efficacy in core domains. For example, there is some evidence for their utility in addressing repetitive behaviours in adults, as assessed using obsessive compulsive symptom outcome measures [80]. They have also been used to manage co-occurring mental health conditions such as anxiety and depression. Unfortunately, these medications can be poorly tolerated [81], highlighting the need for novel options, and the importance of identifying serotonergic mechanisms to target in the autistic brain specifically prior to clinical trials. Therefore, in depth pharmacological ‘profiling’ adopting some of the methods described here may help avoid the unnecessary expense and likely failure of clinical trials and facilitate the discovery of novel pharmacological support options for those who would like that choice.
Availability of data and materials
No datasets were generated or analysed during the current study.
Abbreviations
- 5D-ASC:
-
5-Dimensional altered states of consciousness
- 5HT:
-
5-Hydroxytryptamine
- DMN:
-
Default mode network
- EEG:
-
Electroencephalography
- E/I:
-
Excitation/Inhibition
- ERP:
-
Event-related potential
- GABA:
-
Gamma-aminobutyric acid
- HERMES:
-
Hadamard Encoding and Reconstruction of MEGA-Edited Spectroscopy
- EEG:
-
Electroencephalography
- MRI:
-
Magnetic resonance imaging
- MRS:
-
Magnetic Resonance Spectroscopy
- RMET:
-
Reading the mind in the eyes test
- SSRI:
-
Selective-serotonin reuptake inhibitor
- SSVEP:
-
Steady-state evoked potential
References
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. text rev. 2022. https://doi.org/10.1176/appi.books.9780890425787.
Devlin B, Cook EH, Coon H, Dawson G, Grigorenko EL, McMahon W, et al. Autism and the serotonin transporter: the long and short of it. Mol Psychiatry. 2005;10(12):1110–6.
Anderson BM, Schnetz-Boutaud NC, Bartlett J, Wotawa AM, Wright HH, Abramson RK, et al. Examination of association of genes in the serotonin system to autism. Neurogenetics. 2009;10(3):209–16.
Aaron E, Montgomery A, Ren X, Guter S, Anderson G, Carneiro AMD, et al. Whole blood serotonin levels and platelet 5-HT2A binding in autism spectrum disorder. J Autism Dev Disord. 2019;49(6):2417–25.
Veenstra-VanderWeele J, Muller CL, Iwamoto H, Sauer JE, Owens WA, Shah CR, et al. Autism gene variant causes hyperserotonemia, serotonin receptor hypersensitivity, social impairment and repetitive behavior. Proc Natl Acad Sci USA. 2012;109(14):5469–74.
Wong NML, Findon JL, Wichers RH, Giampietro V, Stoencheva V, Murphy CM, et al. Serotonin differentially modulates the temporal dynamics of the limbic response to facial emotions in male adults with and without autism spectrum disorder (ASD): a randomised placebo-controlled single-dose crossover trial. Neuropsychopharmacol. 2020;45(13):2248–56.
Zafeiriou D, Ververi A, Vargiami E. The serotonergic system: its role in pathogenesis and early developmental treatment of autism. CN. 2009;7(2):150–7.
Carhart-Harris R, Nutt D. Serotonin and brain function: a tale of two receptors. J Psychopharmacol. 2017;31(9):1091–120.
Wojtas A, Bysiek A, Wawrzczak-Bargiela A, Szych Z, Majcher-Maślanka I, Herian M, et al. Effect of psilocybin and ketamine on brain neurotransmitters, glutamate receptors, DNA and rat behavior. IJMS. 2022;23(12):6713.
Ishii T, Kimura Y, Ichise M, Takahata K, Kitamura S, Moriguchi S, et al. Anatomical relationships between serotonin 5-HT2A and dopamine D2 receptors in living human brain. Chen K, editor. PLoS One. 2017;12(12):e0189318.
Beliveau V, Ganz M, Feng L, Ozenne B, Højgaard L, Fisher PM, et al. A high-resolution In Vivo Atlas of the human brain’s serotonin system. J Neurosci. 2017;37(1):120–8.
Gong P, Liu J, Blue PR, Li S, Zhou X. Serotonin receptor gene (HTR2A) T102C polymorphism modulates individuals’ perspective taking ability and autistic-like traits. Front Hum Neurosci. 2015;9:575. Available from: http://journal.frontiersin.org/Article/10.3389/fnhum.2015.00575/abstract. [cited 2022 Dec 6].
Smith RM, Banks W, Hansen E, Sadee W, Herman GE. Family-based clinical associations and functional characterization of the serotonin 2A receptor gene (HTR2A) in autism spectrum disorder: clinical and functional genetics of HTR2A. Autism Res. 2014;7(4):459–67.
Cieslinska A, Fiedorowicz E, Jarmolowska B, Kordulewska N, Kostyra E, Moszynska M, et al. Polymorphisms rs6313 and rs6314 in serotonin receptor gene (HTR2A) and serotonin concentration in autistic children. Neuropsychiatry. 2019;9(1):2021–28. Available from: http://www.jneuropsychiatry.org/peer-review/polymorphisms-rs6313-and-rs6314-in-serotonin-receptor-gene-htr2a-and-serotonin-concentration-in-autistic-children-12913.html. [cited 2022 Dec 6].
Veenstra-VanderWeele J, Kim SJ, Lord C, Courchesne R, Akshoomoff N, Leventhal BL, et al. Transmission disequilibrium studies of the serotonin 5-HT2A receptor gene (HTR2A) in autism. Am J Med Genet. 2002;114(3):277–83.
Murphy DGM, Daly E, Schmitz N, Toal F, Murphy K, Curran S, et al. Cortical serotonin 5-HT 2A receptor binding and social communication in adults with Asperger’s syndrome: an in Vivo SPECT Study. AJP. 2006;163(5):934–6.
Whelan TP, Daly E, Puts NA, Malievskaia E, Murphy DGM, McAlonan GM. Editorial Perspective: Bridging the translational neuroscience gap in autism - development of the 'shiftability' paradigm. J Child Psychol Psychiatry. 2023. Online ahead of print.
França LGS, Ciarrusta J, Gale-Grant O, Fenn-Moltu S, Fitzgibbon S, Chew A, et al. Neonatal brain dynamic functional connectivity in term and preterm infants and its association with early childhood neurodevelopment. Nature Communications. 2024; 15(16).
Kolesnik A, Begum Ali J, Gliga T, Guiraud J, Charman T, Johnson MH, et al. Increased cortical reactivity to repeated tones at 8 months in infants with later ASD. Transl Psychiatry. 2019;9(1):46.
Holiga Š, Hipp JF, Chatham CH, Garces P, Spooren W, D’Ardhuy XL, et al. Patients with autism spectrum disorders display reproducible functional connectivity alterations. Sci Transl Med. 2019;11(481):eaat9223.
Huang Q, Pereira AC, Velthuis H, Wong NML, Ellis CL, Ponteduro FM, et al. GABA B receptor modulation of visual sensory processing in adults with and without autism spectrum disorder. Sci Transl Med. 2022;14(626):eabg7859.
Carey C, Singh N, Dunn JT, Sementa T, Mendez MA, Velthuis H, et al. From bench to bedside: the mGluR5 system in people with and without Autism Spectrum Disorder and animal model systems. Transl Psychiatry. 2022;12(1):395.
Janz P, Bainier M, Marashli S, Schoenenberger P, Valencia M, Redondo RL. Neurexin1α knockout rats display oscillatory abnormalities and sensory processing deficits back-translating key endophenotypes of psychiatric disorders. Transl Psychiatry. 2022;12(1):455.
Ahmad J, Ellis C, Leech R, Voytek B, Garces P, Jones E, et al. From mechanisms to markers: novel noninvasive EEG proxy markers of the neural excitation and inhibition system in humans. Transl Psychiatry. 2022;12(1):467.
Dinis-Oliveira RJ. Metabolism of psilocybin and psilocin: clinical and forensic toxicological relevance. Drug Metab Rev. 2017;49(1):84–91.
Halberstadt AL, Geyer MA. Multiple receptors contribute to the behavioral effects of indoleamine hallucinogens. Neuropharmacology. 2011;61(3):364–81.
Madsen MK, Fisher PM, Burmester D, Dyssegaard A, Stenbæk DS, Kristiansen S, et al. Psychedelic effects of psilocybin correlate with serotonin 2A receptor occupancy and plasma psilocin levels. Neuropsychopharmacol. 2019;44(7):1328–34.
Prochazkova L, Lippelt DP, Colzato LS, Kuchar M, Sjoerds Z, Hommel B. Exploring the effect of microdosing psychedelics on creativity in an open-label natural setting. Psychopharmacology. 2018;235(12):3401–13.
Moreno FA, Wiegand CB, Taitano EK, Delgado PL. Safety, Tolerability, and efficacy of psilocybin in 9 patients with obsessive-compulsive disorder. J Clin Psychiatry. 2006;67(11):1735–40.
Cavanna F, Muller S, de la Fuente LA, Zamberlan F, Palmucci M, Janeckova L, et al. Microdosing with psilocybin mushrooms: a double-blind placebo-controlled study. Transl Psychiatry. 2022;12(1):307.
Bershad AK, Preller KH, Lee R, Keedy S, Wren-Jarvis J, Bremmer MP, et al. Preliminary report on the effects of a low dose of LSD on resting-state Amygdala functional connectivity. Biol Psychiatry. 2020;5(4):461–7.
Murray CH, Tare I, Perry CM, Malina M, Lee R, de Wit H. Low doses of LSD reduce broadband oscillatory power and modulate event-related potentials in healthy adults. Psychopharmacology. 2022;239(6):1735–47.
McAlonan G. Psilocybin may reveal the role serotonin plays in autism. Psychology Today. 2022. Available from: https://www.psychologytoday.com/gb/blog/pathways-progress/202205/psilocybin-may-reveal-the-role-serotonin-plays-in-autism.
Whelan S. Psilocybin study to investigate the serotonin system in autism. Technology Networks. 2022. Available from: https://www.technologynetworks.com/neuroscience/blog/psilocybin-study-to-investigate-the-serotonin-system-in-autism-365462#:~:text=Why%20use%20COMP360%20psilocybin%20in,acts%20on%20the%20serotonin%20system.
Pretzsch CM, Voinescu B, Lythgoe D, Horder J, Mendez MA, Wichers R, et al. Effects of cannabidivarin (CBDV) on brain excitation and inhibition systems in adults with and without Autism Spectrum Disorder (ASD): a single dose trial during magnetic resonance spectroscopy. Transl Psychiatry. 2019;9(1):313.
Pretzsch CM, Floris DL, Voinescu B, Elsahib M, Mendez MA, Wichers R, et al. Modulation of striatal functional connectivity differences in adults with and without autism spectrum disorder in a single-dose randomized trial of cannabidivarin. Molecular Autism. 2021;12(1):49.
Wichers RH, Findon JL, Jelsma A, Giampietro V, Stoencheva V, Robertson DM, et al. Modulation of atypical brain activation during executive functioning in autism: a pharmacological MRI study of tianeptine. Mol Autism. 2021;12(1):14.
Ajram LA, Horder J, Mendez MA, Galanopoulos A, Brennan LP, Wichers RH, et al. Shifting brain inhibitory balance and connectivity of the prefrontal cortex of adults with autism spectrum disorder. Transl Psychiatry. 2017;7(5):e1137–e1137.
Lord C, Rutter M, Le Couteur A. Autism diagnostic interview-revised: a revised version of a diagnostic interview for caregivers of individuals with possible pervasive developmental disorders. J Autism Dev Disord. 1994;24(5):659–85.
Bastiaansen JA, Meffert H, Hein S, Huizinga P, Ketelaars C, Pijnenborg M, et al. Diagnosing autism spectrum disorders in adults: the use of Autism Diagnostic Observation Schedule (ADOS) module 4. J Autism Dev Disord. 2011;41(9):1256–66.
Chan KL, Puts NAJ, Schär M, Barker PB, Edden RAE. HERMES: Hadamard encoding and reconstruction of MEGA-edited spectroscopy: HERMES. Magn Reson Med. 2016;76(1):11–9.
Baumgarten TJ, Oeltzschner G, Hoogenboom N, Wittsack HJ, Schnitzler A, Lange J. Beta peak frequencies at rest correlate with endogenous GABA+/Cr concentrations in sensorimotor cortex areas. Johnson B, editor. PLoS One. 2016;11(6):e0156829.
Michaiel AM, Parker PRL, Niell CM. A hallucinogenic serotonin-2A receptor agonist reduces visual response gain and alters temporal dynamics in mouse V1. Cell Rep. 2019;26(13):3475-3483.e4.
Kometer M, Schmidt A, Jancke L, Vollenweider FX. Activation of serotonin 2A receptors underlies the psilocybin-induced effects on oscillations, N170 visual-evoked potentials, and visual hallucinations. J Neurosci. 2013;33(25):10544–51.
Garrido MI, Kilner JM, Stephan KE, Friston KJ. The mismatch negativity: a review of underlying mechanisms. Clin Neurophysiol. 2009;120(3):453–63.
Huang Q, Velthuis H, Pereira AC, Ahmad J, Cooke SF, Ellis CL, et al. Exploratory evidence for differences in GABAergic regulation of auditory processing in autism spectrum disorder. Transl Psychiatry. 2023;13(1):320.
Dunn MA, Gomes H, Gravel J. Mismatch negativity in children with autism and typical development. J Autism Dev Disord. 2008;38(1):52–71.
OramCardy JE, Flagg EJ, Roberts W, Roberts TPL. Delayed mismatch field for speech and non-speech sounds in children with autism. NeuroReport. 2005;16(5):521–5.
Vlaskamp C, Oranje B, Madsen GF, Møllegaard Jepsen JR, Durston S, Cantio C, et al. Auditory processing in autism spectrum disorder: mismatch negativity deficits: auditory processing in autism spectrum disorder. Autism Res. 2017;10(11):1857–65.
Wienberg M, Glenthoj B, Jensen K, Oranje B. A single high dose of escitalopram increases mismatch negativity without affecting processing negativity or P300 amplitude in healthy volunteers. J Psychopharmacol. 2010;24(8):1183–92.
Padmanabhan A, Lynch CJ, Schaer M, Menon V. The default mode network in autism. Biol Psychiatry. 2017;2(6):476–86.
Muthukumaraswamy SD, Carhart-Harris RL, Moran RJ, Brookes MJ, Williams TM, Errtizoe D, et al. Broadband cortical desynchronization underlies the human psychedelic state. J Neurosci. 2013;33(38):15171–83.
Risk BB, Murden RJ, Wu J, Nebel MB, Venkataraman A, Zhang Z, et al. Which multiband factor should you choose for your resting-state fMRI study? Neuroimage. 2021;234:117965.
Watanabe T, Rees G. Brain network dynamics in high-functioning individuals with autism. Nat Commun. 2017;8(1):16048.
Carhart-Harris RL, Erritzoe D, Williams T, Stone JM, Reed LJ, Colasanti A, et al. Neural correlates of the psychedelic state as determined by fMRI studies with psilocybin. Proc Natl Acad Sci USA. 2012;109(6):2138–43.
Kringelbach ML, Cruzat J, Cabral J, Knudsen GM, Carhart-Harris R, Whybrow PC, et al. Dynamic coupling of whole-brain neuronal and neurotransmitter systems. Proc Natl Acad Sci USA. 2020;117(17):9566–76.
Singleton SP, Luppi AI, Carhart-Harris RL, Cruzat J, Roseman L, Nutt DJ, et al. Receptor-informed network control theory links LSD and psilocybin to a flattening of the brain’s control energy landscape. Nat Commun. 2022;13(1):5812.
the EU-AIMS LEAP group, Moessnang C, Baumeister S, Tillmann J, Goyard D, Charman T, et al. Social brain activation during mentalizing in a large autism cohort: the Longitudinal European autism project. Mol Autism. 2020;11(1):17.
Hornboll B, Macoveanu J, Rowe J, Elliott R, Paulson OB, Siebner HR, et al. Acute serotonin 2A receptor blocking alters the processing of fearful faces in the orbitofrontal cortex and amygdala. J Psychopharmacol. 2013;27(10):903–14.
Bernasconi F, Schmidt A, Pokorny T, Kometer M, Seifritz E, Vollenweider FX. Spatiotemporal brain dynamics of emotional face processing modulations induced by the serotonin 1A/2A receptor agonist psilocybin. Cereb Cortex. 2014;24(12):3221–31.
Schmidt A, Kometer M, Bachmann R, Seifritz E, Vollenweider F. The NMDA antagonist ketamine and the 5-HT agonist psilocybin produce dissociable effects on structural encoding of emotional face expressions. Psychopharmacology. 2013;225(1):227–39.
Mason L, Moessnang C, Chatham C, Ham L, Tillmann J, Dumas G, et al. Stratifying the autistic phenotype using electrophysiological indices of social perception. Sci Transl Med. 2022;14(658):eabf8987.
Puts NAJ, Wodka EL, Tommerdahl M, Mostofsky SH, Edden RAE. Impaired tactile processing in children with autism spectrum disorder. J Neurophysiol. 2014;111(9):1803–11.
Cascio C, McGlone F, Folger S, Tannan V, Baranek G, Pelphrey KA, et al. Tactile perception in adults with autism: a multidimensional psychophysical study. J Autism Dev Disord. 2008;38(1):127–37.
Trotter PD, Smith SA, Moore DJ, O’Sullivan N, McFarquhar MM, McGlone FP, et al. Acute tryptophan depletion alters affective touch perception. Psychopharmacology. 2022;239(9):2771–85.
He JL, Wodka E, Tommerdahl M, Edden RAE, Mikkelsen M, Mostofsky SH, et al. Disorder-specific alterations of tactile sensitivity in neurodevelopmental disorders. Commun Biol. 2021;4(1):97.
Duerler P, Brem S, Fraga-González G, Neef T, Allen M, Zeidman P, et al. Psilocybin induces aberrant prediction error processing of tactile mismatch responses—a simultaneous EEG–FMRI study. Cereb Cortex. 2021;32(1):186–96.
Dittrich A. The standardized psychometric assessment of Altered States of Consciousness (ASCs) in Humans. Pharmacopsychiatry. 1998;31(S2):80–4.
Vollenweider FX, Vollenweider-Scherpenhuyzen MFI, Bäbler A, Vogel H, Hell D. Psilocybin induces schizophrenia-like psychosis in humans via a serotonin-2 agonist action. NeuroReport. 1998;9(17):3897–902.
Baron-Cohen S, Wheelwright S, Hill J, Raste Y, Plumb I. The ‘Reading the Mind in the Eyes’ Test revised version: a study with normal adults, and adults with Asperger syndrome or high-functioning autism. J Child Psychol Psychiatry. 2001;42(2):241–51.
den Ouden HEM, Daw ND, Fernandez G, Elshout JA, Rijpkema M, Hoogman M, et al. Dissociable effects of dopamine and serotonin on reversal learning. Neuron. 2013;80(4):1090–100.
Begeer S, Wierda M, Scheeren AM, Teunisse JP, Koot HM, Geurts HM. Verbal fluency in children with autism spectrum disorders: Clustering and switching strategies. Autism. 2014;18(8):1014–8.
Wong NM, Dipasquale O, Turkheimer F, Findon JL, Wichers RH, Dimitrov M, et al. Differences in social brain function in autism spectrum disorder are linked to the serotonin transporter: a randomised placebo-controlled single-dose crossover trial. J Psychopharmacol. 2022;36(6):723–31.
Pretzsch CM, Voinescu B, Mendez MA, Wichers R, Ajram L, Ivin G, et al. The effect of cannabidiol (CBD) on low-frequency activity and functional connectivity in the brain of adults with and without autism spectrum disorder (ASD). J Psychopharmacol. 2019;33(9):1141–8.
Pretzsch CM, Freyberg J, Voinescu B, Lythgoe D, Horder J, Mendez MA, et al. Effects of cannabidiol on brain excitation and inhibition systems; a randomised placebo-controlled single dose trial during magnetic resonance spectroscopy in adults with and without autism spectrum disorder. Neuropsychopharmacol. 2019;44(8):1398–405.
Robertson CE, Kravitz DJ, Freyberg J, Baron-Cohen S, Baker CI. Tunnel vision: sharper gradient of spatial attention in autism. J Neurosci. 2013;33(16):6776–81.
Foss-Feig JH, Tadin D, Schauder KB, Cascio CJ. A substantial and unexpected enhancement of motion perception in autism. J Neurosci. 2013;33(19):8243–9.
Karaminis T, Lunghi C, Neil L, Burr D, Pellicano E. Binocular rivalry in children on the autism spectrum: binocular rivalry in autism. Autism Res. 2017;10(6):1096–106.
Howes OD, Rogdaki M, Findon JL, Wichers RH, Charman T, King BH, et al. Autism spectrum disorder: consensus guidelines on assessment, treatment and research from the British Association for Psychopharmacology. J Psychopharmacol. 2018;32(1):3–29.
Hollander E, Soorya L, Chaplin W, Anagnostou E, Taylor BP, Ferretti CJ, et al. A double-blind placebo-controlled trial of fluoxetine for repetitive behaviors and global severity in adult autism spectrum disorders. AJP. 2012;169(3):292–9.
King BH, Hollander E, Sikich L, McCracken JT, Scahill L, Bregman JD, et al. Lack of efficacy of citalopram in children with autism spectrum disorders and high levels of repetitive behavior: citalopram ineffective in children with autism. Arch Gen Psychiatry. 2009;66(6):583.
Funding
The PSILAUT study is an Independent Investigator Study (G.M.M.) funded in part by Compass Pathfinder Ltd. The authors also receive support from EU-AIMS (European Autism Interventions)/EU AIMS-2-TRIALS, an Innovative Medicines Initiative Joint Undertaking under Grant Agreement No. 777394. In addition, this paper represents independent research part funded by the infrastructure of the National Institute for Health Research (NIHR) Mental Health Biomedical Research Centre (BRC) at South London and Maudsley NHS Foundation Trust and King’s College London, and the Medical Research Council Centre for Neurodevelopmental Disorders. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health and Social Care.
Author information
Authors and Affiliations
Contributions
T.P.W. contributed to study design, supported community engagement, prepared Figs. 1 and 2 and drafted the manuscript. E.D. contributed to study design and helped draft the manuscript; N.A.P. contributed to study design and helped draft the manuscript; P.S., C.A. and S.B-C. led community engagement and helped draft the manuscript; E.M. contributed to study design, supported community engagement and helped draft the manuscript; D.G.M.M. contributed to study design and helped draft the manuscript. G.M.M. conceived the idea for the study; contributed to study design and drafted the manuscript. All authors reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
T.P.W. is an employee of COMPASS Pathfinder Ltd., T.P.W. and E.M. hold shares in the company. P.S. and C.A. have no conflicts to declare, S-B.C. is co-editor-in-chief of Molecular Autism. N.A.P. has consulted for Deerfield Discovery and Research. D.G.M.M. has consulted for Jaguar Gene Therapy LLC. G.M.M. has received funding for investigator-initiated studies from GW Pharmaceuticals and COMPASS Pathfinder Ltd.. G.M.M. has consulted for Greenwich Biosciences, Inc.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Whelan, T.P., Daly, E., Puts, N.A. et al. The ‘PSILAUT’ protocol: an experimental medicine study of autistic differences in the function of brain serotonin targets of psilocybin. BMC Psychiatry 24, 319 (2024). https://doi.org/10.1186/s12888-024-05768-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12888-024-05768-2