Abstract
Background
Depression during pregnancy is a significant health concern that can lead to a variety of short and long-term complications for mothers. Unfortunately, there is a lack of information available on the prevalence and predictors of prenatal depression in rural eastern Ethiopia. This study assessed prenatal depression and associated factors among pregnant women attending public health facilities in the Babile district, Eastern Ethiopia.
Method
An institution-based cross-sectional study was conducted among 329 pregnant women attending Babile District Public Health Facilities from November 1 to December 30, 2021. Bivariable and multivariable logistic regression were used to identify factors associated with prenatal depression. The adjusted odds ratio (AOR) with a 95% confidence interval was used to report the association, and the significance was declared at a p-value < 0.05.
Results
The prevalence of prenatal depression was 33.1% (95% CI = 28.0%, 38.2%). A lower income (AOR = 3.85, 95% CI = 2.08, 7.13), contraceptive use (AOR = 0.53, 95% CI = 0.28, 0.98), unintended pregnancy (AOR = 2.24, 95% CI = 1.27, 3.98), history of depression (AOR = 5.09, 95% CI = 2.77, 9.35), poor social support (AOR = 5.08, 95% CI = 2.15, 11.99), and dissatisfied marriage (AOR = 2.37, 95% CI = 1.30, 4.33) were the factors associated with increased prenatal depression among pregnant women.
Conclusions
One in every three pregnant women in rural eastern Ethiopia had prenatal depression. Monthly income, contraceptive use, pregnancy intention, history of depression, social support, and marriage satisfaction status were the determinants of prenatal depression. Preventing unintended pregnancies by encouraging women to utilize modern contraceptive methods is essential for mitigating and controlling the risks and burdens of prenatal depression and its negative consequences.
Similar content being viewed by others
Introduction
Depression is a mood disorder characterized by persistent feelings of low self-worth, loss of interest, feelings of regret, restlessness, loss of appetite, fatigue, and poor concentration [1,2,3]. Prenatal depression is a depression that occurs during the time from conception to delivery and is a precursor of postpartum depression if it remains untreated or mismanaged [4]. It is the most prevalent psychiatric disorder experienced during pregnancy, and almost 25% of women experience depression at some point in their life, most commonly during childbearing age [5, 6].
Prenatal depression is a global burden of disease and affects approximately 10% of pregnant women each year [5]. The burden of prenatal depression is 25.5% in lower- and middle-income countries (LMICs) [7]. The burden is also higher than that in sub-Saharan Africa (SSA), which ranges from 10 to 47% [8,9,10], and the prevalence of prenatal depression ranges from 12 to 35% in Ethiopia [10,11,12,13,14].
Prenatal depressive disorders can lead to various short and long-term fetal and maternal negative consequences, including low birth weight, intrauterine growth restriction, preterm birth, and stillbirth, and can also contribute to maternal and neonatal disability, morbidity, and mortality [15,16,17]. In addition, it negatively influences social adjustment and marital relationships [18, 19] and affects maternal-infant interactions through its influence on the occurrence of postnatal depression [20, 21].
Prenatal depression has a significant potential effect on the economy, and it is more susceptible to adverse effects through its impact on healthcare costs and work absenteeism, which accounts for one-third of the work days missed and one-fifth of all primary healthcare appointments missed [22]. Although reports on prevalence rates lack consistency, substantially higher rates were reported in developing countries [5].
There are various factors affecting prenatal depression, but little is known about these factors in developing countries, including Ethiopia. The studies indicated that factors such as low economic status, previous history of psychiatric illness, abortion history, and previous stillbirth history were determinants of prenatal depression [23,24,25,26]. The government of Ethiopia launched and enforced a mental health strategy that aimed at providing mental health services in all health systems of the country [27]. However, there is a gap in providing mental health services in routine maternal health services. Even though investigating prenatal depression and its risk factors is essential for designing and monitoring the implementation of preventive and rehabilitative interventions designed to reduce the impacts of depression, the evidence regarding prenatal depression is inconsistent in Ethiopia.
Hence, addressing the gaps in burdens and risk factors for prenatal depression among pregnant women is a top priority in reducing and preventing prenatal depression and its negative short- and long-term consequences. Previous studies have shown that the burden of prenatal depression is inconsistent in Ethiopia [11, 23], and there is limited information available concerning this topic in rural eastern Ethiopia. In addition, previous studies conducted in the country were performed in a one-site region of Ethiopia, and almost all the studies failed to evaluate the association between prenatal depression and the use of contraceptive methods. Overall, there is limited information on the prevalence and factors associated with prenatal depression among pregnant women in rural Eastern Ethiopia. Thus, this study aimed to assess the level of prenatal depression and associated factors among pregnant women attending public health facilities in the Babile district, eastern Ethiopia.
Materials and methods
Study design and setting
An institution-based cross-sectional study was conducted in the Babile district, eastern Ethiopia, from November 1 to December 30, 2021. The Babile district is one of 24 districts in the East Hararghe Zone, located 560 km, east of Addis Ababa (the capital city of Ethiopia). Administratively, the district had one urban and 23 rural kebeles, and based on the 2007 Central Statistical Agency population census, the district has a projected total population of 103,575, with 22,921 reproductive-age women and 3594 pregnant women. According to the Babile District Health Office annual report of 2020, there is one general hospital, four health centers, and 24 health posts, with two private drug shops providing routine healthcare services for the general public in the district. The annual antenatal care (ANC) attendance in the facilities of the district was 6780 in the Babile Health Center, 1020 in the Abdibuch Health Center, 1320 in the Erer Health Center, and 1500 in the Bisidimo General Hospital.
Population and sampling
All pregnant women attending public health facilities in the Babile district in Eastern Ethiopia were the source population. The study population included pregnant women attending selected public health facilities in the Babile district in Eastern Ethiopia during the study period. Married pregnant women aged 18 years and older who were permanent residents of the district and who attended public health facilities for antenatal care service were included in the study. Women who were unable to understand the local language (Afan Oromo), who were critically sick pregnant women, or who were urgently or immediately referred to a higher-level facility upon arrival at the interview were excluded from the study.
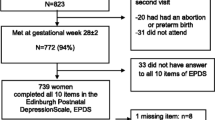
The sample size (n = 330) was calculated by Epi Info version 7.1 using the single population proportion formula. Considering the following assumptions, the average monthly ANC attendance in the district was 565, the confidence interval was 95%, the margin of error was 5%, the prevalence of prenatal depression was 26.6% in southern Ethiopia [28], and the nonresponse rate was 10%.
We selected purposefully all public health facilities (four health centers and one hospital) in the district. The projected sample size was proportionally allocated to each facility based on the average ANC attendance flows over the previous three months. The sample sizes were proportionally allocated to the Babile Health Center (n = 90), Abdibuch Health Center (n = 50), Erer Health Center (n = 64), Awsherif Health Center (n = 53), and Bisidimo General Hospital (n = 73). Then, a systematic random sampling technique was used to select the study participants, and every three eligible women who visited ANC facilities were selected from among the health facilities. After providing written informed consent, a face-to-face interview was conducted in a separate and quiet area.
Data collection procedures and tools
The data were collected through face-to-face interviews using a structured questionnaire adapted from validated scales and published literature [23, 25, 29,30,31,32,33,34,35]. The questionnaire included information on sociodemographic characteristics, obstetric-related characteristics, behavioral characteristics, mental health and psychosocial characteristics, and prenatal depression. Before data collection began, the questionnaire was pretested on 5% of the sample (17 pregnant women) in a separate health facility in the neighboring district to ensure its validity. The questionnaire was first prepared in English, subsequently translated to the local language (Afan Oromo), and returned to English by two experts who were in good command of both languages. Five trained diploma nurses collected the data through face-to-face interviews in a quiet private room. The overall data collection process was supervised by trained BSc nurses at each facility.
Measurements
Prenatal depression
The Edinburgh Postnatal Depression Scale (EPDS) was used to detect prenatal depression [32]. The EPDS is a validated scale with 10 Likert scale items, each rated from 0 (mild depression) to 3 (high depression), for detecting depression in antepartum and postpartum samples across the world; this scale includes information from Ethiopia (postpartum depression assessment in Addis Ababa with a sensitivity of 80.6% and a specificity of 77%) [29]. Similar to other studies conducted abroad and in Ethiopia, the cutoff point of the EPDS was 13 and above to identify pregnant women with depressive symptoms. The internal consistency of the index score was confirmed with a Cronbach’s α of 0.92. Pregnant women who scored 13 or above were categorized as depressed women, while those who scored less than 13 were categorized as not depressed women [25].
Level of social support
Social Support was measured using the Oslo Social Support Scale-3 item (OSSS-3). The OSSS-3 contains three items: the number of close intimates, the perceived level of concern from others, and the perceived ease of getting help from neighbors. The composite index score was computed from three items ranging from 3 to 14, and OSSS-3 scores were categorized into three categories of social support. The internal consistency of the index score was confirmed with a Cronbach’s α of 0.76. The scores were subsequently assigned as 3–8 for ‘poor social support’, 9–11 for ‘moderate social support’, and 12–14 for ‘strong social support’ [30].
Marital satisfaction
This was measured using the Kansas Marital Satisfaction Scale (KMSS), which contains three Likert scale items. The marriage satisfaction scale included three items, each of which had a 7-point scale ranging from 1 (extremely dissatisfied) to 7 (extremely satisfied); the composite index score was computed from three items ranging from 3 to 21. The internal consistency of the index score was confirmed with a Cronbach’s α of 0.83. A cutoff point of 17 and above was used to indicate that women were satisfied with their current marital relations, while a cutoff point less than 17 was used to indicate that women were dissatisfied with their current marital relations [31, 33].
Substance use was assessed using a self-report of exposure to at least one of the three substances (alcohol, khat, or tobacco) during the current pregnancy. A pregnant woman was considered to use a substance when she used at least one type of substance during her current pregnancy, regardless of the dose and frequency [36].
Data quality control
The data quality was maintained using standard questionnaires adapted from validated scales and relevant published literature. The questionnaires were first written in English and subsequently translated into the local language (Afan Oromo) and returned to English by two experts with good mastery of both languages. The data collectors and supervisors trained for one day on the objective of the study and the data collection technique. Before starting the statistical analysis, several composite index scores were computed and used accordingly, which improved the validity of the measurements and respective computed indices and estimates used in the study.
Data processing and analysis
After checking for completeness and consistency, the data were entered into EpiData version 3.1 and analyzed using SPSS version 24. Descriptive statistics such as frequency, a measure of central tendency, and dispersion were used to characterize pregnant women accordingly. Before analysis, the internal consistency of the items was checked for each composite index score using reliability analysis (Cronbach’s α). We observed high internal consistency across all the composite indices of the EPDS use items (Cronbach’s α = 0.92), the KMSS use items (Cronbach’s α = 0.83), and the OSSS use items (Cronbach’s α = 0.76). Bivariable and multivariable logistic regression analyses were also conducted to identify factors associated with prenatal depression among pregnant women. Variables with a p-value < 0.25 in the bivariable analysis were selected as candidate predictors for multivariable logistic regression analysis. A multivariable logistic regression analysis was conducted to identify the significant risk factors for prenatal depression using the backward stepwise likelihood ratio method for model building. The Hosmer and Lemeshow goodness-of-fit test was employed to determine the overall adequacy of the model, with a p-value of 0.65 indicating an adequate fit. The adjusted odds ratio (AOR) with its 95% confidence interval (CI) was used to report the strength of an association, and a p-value < 0.05 indicated statistical significance.
Results
Participants sociodemographic characteristics
A total of 330 eligible pregnant women were invited to participate in the study, and 329 (99.7%) participated in the study. The mean age of the participants was 29.2 (± 5.6) years, and the majority (65.5%) of them were in 25–34 years age group, followed by 27.4% in the 18–24 years age group and 26.1% in the ≥ 35 years age group. More than half (55.0%) of the participants were from rural residences. Approximately half (49.5%) of the participants had an education level of primary school, followed by being unable to read and write (36.8%), secondary school (9.7%), and college and above (4.0%). Among occupational status, the majority (63.5%) of the participants were housewives, followed by merchants (18.2%) and government employees (13.1%). Regarding average monthly income, a majority (54.1%) of the participants had a monthly income less than or equal to 2000 Ethiopian Birr (ETB), and their median average monthly income was 2000 ETB (quartile 1 = 1200 ETB, quartile 3 = 3200 ETB) (Table 1).
Obstetrics and psychosocial-related characteristics
The means (± SD) gravidity and parity were 4.8 (± 2.4) and 3.9 (± 2.1), respectively. Almost one in every five (21.1%) women had at least one abortion history, and one in every four (25.3%) participants had at least one stillbirth history. The majority (59.6%) of the women had never used modern contraceptive methods before their current pregnancies, and approximately 38.9% of the current pregnancies were unintended pregnancies. The majority (58.7%) of women were in the second trimester, followed by the third trimester (33.1%) and the first trimester (8.2%). Approximately 15.5% of pregnant women used at least one type of substance during their current pregnancy. About 31.6% of the pregnant women were violated by their partners, and approximately 32.8% of the pregnant women had a history of depression. Regarding social support, 41.6%, 41.0%, and 17.3% of the pregnant women had poor, moderate, and strong social support, respectively. Almost seven out of ten pregnant women (69.3%) were satisfied with their marriage relationship (Table 2).
Prevalence of prenatal depression
In this study, the internal consistency of the prenatal depression (EPDS) tool was acceptable, with Cronbach’s α = 0.92. The overall prevalence of prenatal depression (EPDS score ≥ 13) among pregnant women was 33.1% (95% CI = 28.0%, 38.2%) in the Babile district, eastern Ethiopia.
Factors associated with prenatal depression
The bivariable logistic regression analysis showed that average monthly income, gravidity, current pregnancy intentions, trimester, substance use, parental violence, history of depression, level of social support, and marriage satisfaction status were factors significantly associated with prenatal depression. However, in the multivariable logistic regression analysis, average monthly income, use of contraceptives, pregnancy intention, history of depression, level of social support, and marriage satisfaction status were the main predictors of prenatal depression among pregnant women.
Women who had an average monthly income less than or equal to 2000 ETB were almost four times more likely to be depressed during pregnancy (AOR = 3.85, 95% CI: 2.08, 7.13) than those who had an average monthly income greater than 2000 ETB. The women who used contraceptive methods before their current pregnancy were almost 50% less likely to develop prenatal depression during pregnancy (AOR = 0.53; 95% CI = 0.28, 0.98). The odds of prenatal depression were approximately two times greater among women with unintended pregnancies than among those with planned pregnancies (AOR = 2.24, 95% CI = 1.27, 3.98). Women who had a history of previous depression were five times more likely (AOR = 5.09, 95% CI = 2.77, 9.35) to develop prenatal depression than those who had no previous history of depression. Pregnant women who had poor social support were five times more likely to develop prenatal depression than those who had strong social support (AOR = 5.08, 95% CI = 2.15, 11.99). The odds of prenatal depression were approximately two times greater (AOR = 2.37, 95% CI: 1.30, 4.33) among women dissatisfied with their marriage than among women who were satisfied with their marriage (Table 3).
Discussion
This study assessed the prevalence and associated factors of prenatal depression among pregnant women attending public health facilities in the Babile district, eastern Ethiopia. We found that the prevalence of prenatal depression was 33.1% among pregnant women attending public health facilities in Babile district, eastern Ethiopia.
This finding is consistent with previous studies conducted in Arba Minch, southern Ethiopia (35.4%) [14], west Showa, central Ethiopia (32.3%) [37], Bale, southeast Ethiopia (31.5%) [17], Adama, central Ethiopia (31.2%) [11], and northern Tanzania (33.8%) [38]. However, this finding is higher than those of studies conducted in east Gojam, northwest Ethiopia (17.8%) [39], Addis Ababa, central Ethiopia (24.9%) [25], Hawasa, southern Ethiopia (21.5%) [26], Gondar, northwest Ethiopia (23.0%) [13], Nigeria (24.5%) [35], and Bangladesh (18.0%) [40]. This variation might be due to sociodemographic differences: almost all the study subjects in comparable studies were urban residents [25], while more than half of our study subjects were rural residents. This difference might also be due to differences in the reproductive characteristics of the study subjects. For instance, the rate of contraceptive use was higher in Addis Ababa but lower in our study, which may have resulted in a higher burden of unintended pregnancy associated with prenatal depression. In addition, geographical, cultural, and economic variations may contribute to the higher prevalence of this disease.
On the other hand, the prevalence of depression in this study is lower than that in studies conducted in South Africa (47.0%) [9], Pakistan (81.0%) [41], and Koria (40.5–61.4%) [41]. These variations in prenatal depression could be attributable to differences in the study setting and verification tools used to screen for symptoms of depression and cutoff points for prenatal depression. For instance, the study in Koria used the EPDS with a cutoff point greater than or equal to a score of 9 to diagnose prenatal depression, while our study used a cutoff point greater than or equal to a score of 13.
This study indicated that women with an average monthly income of less than or equal to 2000 ETB were almost four times more likely to develop prenatal depression than women with an income greater than 2000 ETB. These findings imply that lower household income increases the risk of incidental mental disorders. These findings are supported by those of a previous study, which indicated that pregnant women with lower incomes were more likely to develop depression and anxiety [42, 43]. Given that thriving during a healthy pregnancy requires access to adequate nutrition, a safe and reliable place to rest, and other sources of social support.
Women who used contraceptive methods before their current pregnancy were almost 50% less likely to develop prenatal depression during pregnancy than women who did not use contraceptive methods. This finding implies that the use of contraceptives indirectly reduces prenatal depression by reducing the burden of unintended pregnancies. On the other hand, the odds of prenatal depression were greater among women with unintended pregnancies. This could be due to the presence of women who missed opportunities to use modern contraceptive methods for preventing and reducing unintended pregnancy; only a few women may have intended to become pregnant. These women may develop prenatal depression as a result of stress, which is associated with perceiving unintended motherhood with poor social support [44, 45]. It is worrisome that unintended pregnancy could increase the risk of prenatal depression during pregnancy. Reducing the burden of unintended pregnancy through improving the utilization of modern contraceptive methods at the community level is essential for reducing and preventing prenatal depression and its negative consequences.
The odds of prenatal depression were higher among women who had a previous history of depression. This finding is supported by studies conducted in northwestern and central Ethiopia [25, 39]. The risk of depression recurrence is high during pregnancy due to physiological changes. In addition, physical and hormonal changes that occur during pregnancy may precipitate earlier depression, increasing susceptibility to recurrence [23, 25, 46].
Pregnant women who had poor social support were five times more likely to develop prenatal depression than those who had strong social support. This finding is supported by the findings of a study conducted in Hawassa, southern Ethiopia. A poor social life may reduce women’s interaction with others, and it can lead to stress and cause mood changes. This finding is also supported by the findings of previous studies indicating that depression and anxiety are less common among pregnant women who perceive a greater degree of social support [47, 48].
Marriage satisfaction status was significantly associated with prenatal depression. The odds of prenatal depression were about two times higher among women who were dissatisfied with their marriage than among women who were satisfied with their marriage. Marital dissatisfaction leads to marital instability, which may aggravate psychosocial stress and precipitate depression disorder. During pregnancy, women need their husbands’ psychological, physical, and financial support; however, if their marital status is dissatisfied during critical times, they may miss mandatory support and may develop mood instability [49].
As a strength, the study used standard validated instruments for data collection; these instruments can be generalized to pregnant women attending public health facilities in urban and rural settings. However, because of the cross-sectional study design, the study may not have shown a temporal relationship between prenatal depression and the predictors. In addition, because this study was conducted among pregnant women who received antenatal care at health facilities, the findings may not apply to women who did not receive antenatal care.
Conclusions
This study concluded that one in every three pregnant women attending ANC visits at public health facilities in the Babile district had prenatal depression. Having a lower income, not using contraceptives, unintended pregnancy, a history of previous depression, poor social support, and dissatisfied marriage relations were found to be independent predictors of prenatal depression. Prevention of unintended pregnancies by encouraging women to utilize modern contraceptive methods is essential for mitigating and controlling the risks and burdens of prenatal depression and its negative consequences. In addition, strengthening and building strong social support and healthy marital relationships are paramount for reducing the burden of prenatal depression and its adverse effects.
Data availability
Data that support the findings are available and will be provided by the correspondence author on a reasonable request.
Abbreviations
- AOR:
-
Adjusted odds ratio
- ANC:
-
Antenatal care
- EPDS:
-
Edinburgh Postnatal Depression Scale
- LMIC:
-
Low middle-income country
- SSA:
-
Sub-Saharan Africa
- WHO:
-
World Health Organization
References
Figueiredo B, Pacheco A, Costa RJA. Depression during pregnancy and the postpartum period in adolescent and adult Portuguese mothers. Arch Women Ment Health. 2007;10(3):103–9.
Freitas CJ, Williams-Reade J, Distelberg B, Fox CA, Lister Z. Paternal depression during pregnancy and postpartum: an international Delphi study. J Affect Disord. 2016;202:128–36.
Marcus M, Yasamy MT, van Ommeren Mv, Chisholm D, Saxena S. Depression: A global public health concern. 2012.
Becker M, Weinberger T, Chandy A, Schmukler SJC. Depression during pregnancy and postpartum. Curr Psychiatry Rep. 2016;18(3):32.
Woody C, Ferrari A, Siskind D, Whiteford H. Harris MJJoad: a systematic review and meta-regression of the prevalence and incidence of perinatal depression. J Affect Disord. 2017;219:86–92.
Alderdice F, McNeill J, Lynn F. A systematic review of systematic reviews of interventions to improve maternal mental health and well-being. Midwifery. 2013;29(4):389–99.
Roddy Mitchell A, Gordon H, Lindquist A, Walker SP, Homer CS, Middleton A, Cluver CA, Tong S, Hastie R. Prevalence of Perinatal Depression in Low-and Middle-Income countries: a systematic review and Meta-analysis. JAMA Psychiatry 2023, 80(5).
Habtamu Belete A, Alemayehu Assega M, Alemu Abajobir A, Abebe Belay Y, Kassahun Tariku M. Prevalence of antenatal depression and associated factors among pregnant women in Aneded Woreda, North West Ethiopia: a community based cross-sectional study. BMC Res Notes. 2019;12:1–6.
Rochat TJ, Tomlinson M, Bärnighausen T, Newell M-L, Stein A. The prevalence and clinical presentation of antenatal depression in rural South Africa. J Affect Disord. 2011;135(1–3):362–73.
Mossie TB, Sibhatu AK, Dargie A, Ayele AD. Prevalence of antenatal depressive symptoms and associated factors among pregnant women in Maichew, North Ethiopia: an institution based study. Ethiop J Health Sci. 2017;27(1):59–66.
Sahile MA, Segni MT, Awoke T, Bekele D. Prevalence and predictors of antenatal depressive symptoms among women attending Adama Hospital Antenatal Clinic, Adama, Ethiopia. Int J Nurs Midwifery. 2017;9(5):58–64.
Getinet W, Amare T, Boru B, Shumet S, Worku W, Azale T. Prevalence and risk factors for antenatal depression in Ethiopia: systematic review. Depression research and treatment 2018, 2018.
Ayele TA, Azale T, Alemu K, Abdissa Z, Mulat H, Fekadu A. Prevalence and associated Factors of Antenatal Depression among women attending Antenatal Care Service at Gondar University Hospital, Northwest Ethiopia. PLoS ONE. 2016;11(5):e0155125.
Beketie ED, Kahsay HB, Nigussie FG, Tafese WT. Magnitude and associated factors of antenatal depression among mothers attending antenatal care in Arba Minch town, Ethiopia, 2018. PLoS ONE. 2021;16(12):e0260691.
Baumgartner JN, Parcesepe A, Mekuria YG, Abitew DB, Gebeyehu W, Okello F, Shattuck D. Maternal mental health in Amhara region, Ethiopia: a cross-sectional survey. Global Health: Sci Pract. 2014;2(4):482–6.
Belay YA, Moges NA, Hiksa FF, Arado KK, Liben ML. Prevalence of antenatal depression and associated factors among pregnant women attending antenatal Care at Dubti Hospital: a case of pastoralist region in Northeast Ethiopia. Depression research and treatment 2018, 2018.
Tefera TB, Erena AN, Kuti KA, Hussen MA. Perinatal depression and associated factors among reproductive aged group women at Goba and Robe Town of Bale Zone, Oromia Region, South East Ethiopia. Maternal Health Neonatology Perinatol. 2015;1(1):1–9.
Kazi A, Fatmi Z, Hatcher J, Kadir MM, Niaz U, Wasserman GA. Medicine: social environment and depression among pregnant women in urban areas of Pakistan: importance of social relations. Soc Sci Med. 2006;63(6):1466–76.
Hart R, McMahon C. Mood state and psychological adjustment to pregnancy. Arch Women Ment Health. 2006;9(6):329–37.
Sawyer A, Ayers S, Smith HJJ. Pre-and postnatal psychological wellbeing in Africa: a systematic review. J Affect Disord. 2010;123(1–3):17–29.
Koubovec D, Geerts L, Odendaal H, Stein DJ, Vythilingum BJCPR. Effects of psychologic stress on fetal development and pregnancy outcome. Curr Psychiatry Rep. 2005;7(4):274–80.
Portugal FB, Campos MR, Goncalves DA, Mari Jd, Fortes SLCL. Quality of life of primary care patients in Rio De Janeiro and SãoPaulo, Brasil: associations with stressful life events and mental health. Ciencia Saude Coletiva 2016, 21(2).
Bisetegn TA, Mihretie G, Muche T. Prevalence and predictors of depression among pregnant women in Debretabor Town, Northwest Ethiopia. PLoS ONE. 2016;11(9):e0161108.
Hartley M, Tomlinson M, Greco E, Comulada W, Stewart J. Roux Iea: depressed mood in pregnancy: prevalence and correlates in two Cape Town peri-urban settlements. Reprod Health. 2011;8:9.
Biratu A, Haile D. Prevalence of antenatal depression and associated factors among pregnant women in Addis Ababa, Ethiopia: a cross-sectional study. Reproductive Health. 2015;12(99):1–8.
Duko B, Ayano G, Bedaso A. Depression among pregnant women and associated factors in Hawassa City, Ethiopia: an institution-based cross-sectional study. Reprod Health 2019, 16(25).
Federal Ministry of Health (FMOH): Federal Democratic Republic of Ethiopia Ministry of Health: National Mental Health Strategy. (2012/13–2015/16). In. Edited by Health M; 2012.
Gemta WA. Prevalence and factors associated with antenatal depression among women following antenatal care at Shashemane health facilities, South Ethiopia. Annals Global Health. 2015;81(1):90–90.
Hanlon C, Medhin G, Alem A, Araya M, Abdulahi A, Hughes M, Tesfaye M, Wondimagegn D, Patel V, Prince M. Detecting perinatal common mental disorders in Ethiopia: validation of the self-reporting questionnaire and Edinburgh postnatal depression scale. J Affect Disord. 2008;108(3):251–62.
Oslo social support scale (OSSS-. 3) [http://www.stakes.fi/pdf/mentalhealth].
Grover KJ, Paff-Bergen LA, Russell CS, Schumm WR. The Kansas marital satisfaction scale: a further brief report. Psychol Rep. 1984;54(2):629–30.
Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression: development of the 10-item Edinburgh postnatal depression scale. Br J Psychiatry. 1987;150(6):782–6.
Green RG, Woody D, Maxwell S, Mercer R, Williams S. Reliability and validity of the Kansas Marital Satisfaction Scale in a sample of African-American husbands and wives. Psychol Rep. 1998;82(1):255–8.
Priscila PK, Lovisi GM, Pilowsky DL, Lima LA, Legay LF. Depression during pregnancy: prevalence and risk factors among women attending a public health clinic in Rio De Janeiro, Brazil. 2009, 25(12):2725–36.
Thompson O, Ajayi I. Prevalence of Antenatal Depression and Associated Risk Factors among Pregnant Women Attending Antenatal Clinics in Abeokuta North Local Government Area, Nigeria. Depression research and treatment 2016, 2016:e4518979.
World Health Organization. Guidelines for the identification and management of substance use and substance use disorders in pregnancy. 2014.
Tiki T, Taye K, Duko B. Prevalence and factors associated with depression among pregnant mothers in the West Shoa Zone, Ethiopia: a community-based cross-sectional study. BMC Annals Gen Psychiatry 2020, 19(24).
Rwakarema M, Premji SS, Nyanza EC, Riziki P, Palacios-Derflingher L. Antenatal depression is associated with pregnancy-related anxiety, partner relations, and wealth in women in Northern Tanzania: a cross-sectional study. BMC Womens Health. 2015;15(1):1–10.
Bantie A, Kassa GM, Zeleke H, Zeleke LB, Aynalem BY. Prevalence of depression and associated factors among pregnant women attending antenatal care in public health institutions of Awabale Woreda, East Gojjam Zone, Northwestern Ethiopia: a cross-sectional study. PLoS ONE. 2022;17(10):e0271876.
Nasreen HE, Kabir ZN, Forsell Y, Edhborg M. Prevalence and associated factors of depressive and anxiety symptoms during pregnancy: a population based study in rural Bangladesh. BMC Womens Health. 2011;11(1):1–9.
Park J-h, Karmaus W, Zhang H. Prevalence of and risk factors for depressive symptoms in Korean women throughout pregnancy and in postpartum period. Asian Nurs Res. 2015;9(3):219–25.
Fellenzer JL, Cibula DA. Intendedness of pregnancy and other predictive factors for symptoms of prenatal depression in a population-based study. Matern Child Health J. 2014;18:2426–36.
Fisher J, Tran T, Tran TD, Dwyer T, Nguyen T, Casey GJ, Simpson JA, Hanieh S, Biggs B-A. Prevalence and risk factors for symptoms of common mental disorders in early and late pregnancy in Vietnamese women: a prospective population-based study. J Affect Disord. 2013;146(2):213–9.
Rahman A, Fisher J, Bower P, Luchters S, Tran T, Yasamy MT, Saxena S, Waheed W. Interventions for common perinatal mental disorders in women in low-and middle-income countries: a systematic review and meta-analysis. Bull World Health Organ. 2013;91:593–I601.
Fisher J, Mello MCd, Patel V, Rahman A, Tran T, Holton S, Holmes W. Prevalence and determinants of common perinatal mental disorders in women in low-and lower-middle-income countries: a systematic review. Bull World Health Organ. 2012;90:139–49.
Yanikkerem E, Ay S, Mutlu S, Goker A. Antenatal depression: prevalence and risk factors in a hospital based Turkish sample. J Pak Med Assoc. 2013;63(4):472–7.
Agostini F, Neri E, Salvatori P, Dellabartola S, Bozicevic L, Monti F. Antenatal depressive symptoms associated with specific life events and sources of social support among Italian women. Matern Child Health J. 2015;19:1131–41.
Bayrampour H, McDonald S, Tough S. Risk factors of transient and persistent anxiety during pregnancy. Midwifery. 2015;31(6):582–9.
Zelalem ED, Asaye MM, Mihret MS. Antenatal depression and its correlates on northwestern Ethiopian women: community-based cross-sectional study. Pan Afr Med J 2020, 36(239).
CIOMS. WHO: International Ethical Guidelines for Biomedical Research Involving Human Subjects. 1st edition; 2008.
Acknowledgements
We thank all the study participants, data collectors and supervisors. We also want to thank the Babile Health Office and the respective facilities for facilitating the study.
Funding
None.
Author information
Authors and Affiliations
Contributions
SJA, MM, DE, AAU, HAA, MT, AS, AA, AE and MY participated in the conception of the idea, development, and amendment of the proposal, data collection, and analysis, and write up the results. SJA, MM, DE, AAU and HAA analyzed the data. AAU drafted the manuscript with continuous input from SJA, MM, DE, AAU, HAA, MT, AS, AA, AE and MY reviewed the manuscript for intellectual content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The study was conducted in accordance with the Helsinki Declaration of Studies involving Human Subjects [50]. The study was also approved by the Institutional Health Research Ethical Review Committee of the College of Health and Medical Sciences, Haramaya University, Ethiopia (Ref.no: IHRERC/172/2021). Written informed consent was obtained from all participants after the purpose and benefits of the study were explained.
Consent for publication
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ahmed, S.J., Merid, M., Edessa, D. et al. Prenatal depression among pregnant women attending public health facilities in Babile district, Eastern Ethiopia: a cross-sectional study. BMC Psychiatry 24, 339 (2024). https://doi.org/10.1186/s12888-024-05732-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12888-024-05732-0