Abstract
Background
Previous studies suggested that childhood maltreatment is associated with poor health outcomes. While not everyone who experiences abuse as a child goes on to experience poor mental health, some traumatized people are grown to be more resilient than others. Few studies have examined the association between childhood maltreatment and adult resilience. This study aimed to determine different relationships between specific types and features of childhood maltreatment with adult resilience among Chinese with Major Depressive Disorder (MDD) and healthy controls (HCs).
Methods
A total of 101 patients with MDD and 116 participants in the healthy control (HC) group from Zhumadian Psychiatric Hospital and its nearby communities were included in this analysis. Childhood maltreatment was assessed retrospectively using Childhood Trauma Questionnaire (CTQ). Adults’ resilience was assessed by the Connor-Davidson Resilience Scale (CD-RISC). Generalized linear models were applied between childhood maltreatment (specific types and features) and resilience adjusting for covariates.
Results
The total score of CD-RISC and factor scores of strength, optimism, and tenacity in the HC group were higher than those in the MDD group. CTQ total score had a negative association with optimism score among participants in MDD (β=-0.087, P < 0.001) and HC (β=-0.074, P = 0.023) groups. Higher emotional neglect (EN) score (β=-0.169, P = 0.001) and physical neglect (PN) score (β=-0.153, P = 0.043) were related to a worse optimism score in MDD group. Emotional abuse (EA) score was associated with a worse tenacity score (β=-0.674, P = 0.031) in MDD group. For participants in HC group, higher EN and PN scores were related to worse resilience scores (tenacity, strength, and optimism).
Conclusions
Patients with MDD showed lower optimism than HCs. Childhood maltreatment, especially childhood negect, independently contributed to optimism, with more severe childhood maltreatment predictive of worse performance of optimism. EA in childhood was also linked to worse tenacity in adult patients with MDD.
Similar content being viewed by others
Background
Childhood maltreatment is regarded as the abuse and neglect of children under 16 years, including physical and emotional abuse and neglect, and sexual abuse, which are related to long-term physical and mental health outcomes across the life course. A study suggested that females with mental illness had a higher rate of childhood sexual abuse than those in the general group [1]. Representative studies from large national American samples [2, 3] showed that American children were exposed to various types of violence in their childhood, including maltreatment, bullying, property victimization, sexual victimization, and eye-witness experience. Childhood maltreatment is commonly reported in individuals from developing countries, such as China. A systematic review reported that 26.6% of children under 18 years of age had suffered from physical abuse, 8.7% from sexual abuse, 19.6% from emotional abuse, and 16% from neglect in China [4]. It is reported that 36.6% of Chinese experienced physical abuse in their childhood [5]. A total of 24.8% and 17.6% of male and female college students experience sexual abuse in their childhood [6]. Previous studies showed that childhood maltreatment had an association with later psychiatric symptomatology, including major depressive disorder [7], posttraumatic stress disorder [8], and bipolar disorder [1]. In this case, childhood maltreatment is a major public problem.
Many children are at high risk of exposure to violence and its negative outcomes, so it is important to recognize how many children could successfully navigate these adverse events [9]. However, not everyone who experiences abuse as a child goes on to experience poor mental health [10]. Some people are or grow to be more resilient than others [11]. This observation had led many researchers to test the specific protective factors, including individual capacity for resilience, or the ability to face adversities or challenges successfully [12]. Resilience is defined as the ability to bounce back from setbacks [13], learn from mistakes [14], find inspiration in obstacles, and have faith that you can get through any stress or struggle you face in life [15, 16]. Previous studies focused on resilience capacity at individual-level, which is defined as one’s degree of their personal qualities, including adaptability, self-confidence, and ability to endure stress [17, 18]. Resilience capacity might be one of the factors that contribute to the recovery process after experiencing adversity and could decrease the risk of developing negative consequences after adverse events [19, 20]. It is important to explore how childhood maltreatment may have effects on resilience and compare the differences between individuals with and without psychotic disorders, such as Major Depressive Disorder (MDD), and this could provide recommendations for future public health interventions and for promoting public mental health.
Previous research suggested that childhood maltreatment could have detrimental effects on self-reported resilience in adulthood. A study conducted in the USA showed that childhood maltreatment had a relationship with worse resilience capacity among individuals in the community [21]. Another study from America revealed that exposure to violence in childhood was related to lower resilience capacity, however, this association was no longer statistically significant after adjusting for the symptoms of depression and anxiety [9]. A recent study using Atlanta’s large community-based sample reported that childhood emotional abuse and co-occurrence of childhood maltreatment might be deleterious to resilience in adulthood [22]. Most previous studies were conducted on data from high-income countries, including the USA. Few studies explored the association between childhood maltreatment and adult resilience in developing countries like China. There is value in conducting an analysis of relationships of childhood maltreatment to adult resilience in a new cultural and social setting. Besides, comparing the differences of associations between childhood maltreatment and adult resilience among patients with and MDD and healthy controls (HCs) might help to find the specific interventions among patients to promote their mental health.
In this study, we aim to investigate the association between childhood maltreatment and adult resilience capacity and compare differences among patients with MDD and HCs. Specifically, we intended to test whether the following childhood maltreatment features were related to worse resilience capacity (certain types of resilience capacity, including tenacity, strength, and optimism) in adulthood: (a) overall childhood maltreatment; (b) specific types of childhood maltreatment; (c) number of specific types of childhood maltreatment.
Methods
Sample and procedure
The data in this analysis was derived from the baseline data from a longitudinal project conducted in Zhumadian Psychiatric Hospital (Henan, China) and its nearby communities, and the project aimed to scrutinize the biological and psychological mechanisms of MDD. The enrolment procedure was set up in January 2013 and ended in December 2018. Two well-trained psychiatrists supervised the whole process and an eligibility criterion was set for the procedure for the two groups separately. The investigation was carried out following the latest version of the Declaration of Helsinki. The study design was reviewed and approved by the Medical Ethics Committees of the Second Xiangya Hospital of Central South University (S238) and the Zhumadian Psychiatric Hospital (S002). This clinical research has been registered at the Chinese Clinical Trial Registry, and the Registration number is ChiCTR1800014591.
The inclusion criteria for the two groups in the longitudinal study at baseline were as follows. For participants included in the MDD group, they (1) aged 18–60 years old, (2) diagnosed with MDD which was confirmed by two well-trained psychiatrists using the Structured Clinical Interview for the fourth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV), (3) were medication free for ≥ 14 days, (4) currently had at least moderate depression severity, with a score \(\ge\)20 in the 24-item Hamilton Depression Rating Scale (HAMD24), (5) with no other psychiatric disorders in the past or present (except generalized anxiety disorder). For participants included in the HC group, they (1) aged 18–60 years old, (2) scored < 8 in the HAMD24, (3) had no current or lifetime substance abuse or diagnosis of any psychiatric disorders. For any participants, if they (1) had a history of systemic medical condition, neurological disorders or head injury, (2) are pregnant or breastfeeding, (3) had any other DSM-IV psychiatric disorder or alcohol/drug dependence, (4) had completed any similar neurocognitive assessments last year, (5) had color-blindness, or (6) had suicide ideation or suicidal behaviors, they were excluded from the Zhumadian longitudinal project. Any participants who had not completed childhood maltreatment or resilience measurements were not included in the current study. After excluding ineligible participants, a total of 101 patients with MDD and 116 participants in the HC group were included in this analysis. Informed consent of the participants was obtained after the nature of the procedures had been fully explained.
Measures
Resilience
Resilience was assessed using the Chinese version of Connor-Davidson resilience scale (CD-RISC), which showed good validity and reliability among Chinese [23]. The Cronbach’s α for CD-RISC in this study was 0.902, indicating good internal consistency. The self-report questionnaire includes 25 items that could be grouped into three factors: tenacity, strength, and optimism [24]. Participants’ responses to each item ranged from 0 (completely disagree) to 4 (completely agree).
Childhood maltreatment
Childhood maltreatment was assessed by the Childhood Trauma Questionnaire (CTQ). CTQ consists of five factors (emotional abuse, EA; physical abuse; PA, sexual abuse, SA; emotional neglect, EN; physical neglect, PN) of maltreatment with 28 items in the questionnaire. The questionnaire is a retrospective assessment tool for assessing maltreatment before the age of 16 years old. The Chinese version of CTQ had shown good validity and reliability among the Chinese population [25]. The Cronbach’s α for CTQ in this study was 0.704, indicating good internal consistency. According to previous studies [26], we set the cutting scores of CTQ’s five factors to distinguish the participants with positive CTQ factors (exceeding the cutting scores) as follows: PA > 9, PN > 9, EA > 12, EN > 14, and SA > 7. The summary and factor scores of CTQ and the counts of CTQ factors exceeding the cutting scores were used for analysis.
Covariates
Potential confounders requiring adjustment were demographic factors (age, sex, and educational years), clinical information (total history of MDD and episode counts), and participants’ depression and anxiety rating scores.
The participants’ depression was assessed using HAMD24 which is a generally used clinician-rated scale [27]. HAMD24 had shown good reliability and validity in the Chinese population. A total of 12 items were rated from 0 to 4, three items were rated from 0 to 3, and nine items were scored from 0 to 2. The total score of the questionnaire ranges from 0 to 75 with a cutoff score of 20. Participants with a score of HAMD24\(\ge\)20 were regarded as having moderate depression [28].
We used a clinician-rated 14-item Hamilton Anxiety Rating Scale (HAMA14) to assess the participants’ anxiety symptoms [29]. HAMA14 presented good reliability and validity among the Chinese community population [30]. Each item of the questionnaire was rated from 0 to 4, and the total score ranges from 0 to 56.
Statistical analysis
Mean (standard deviation) was used to summarize participants’ age and other continuous factors. Number (percentage) was reported to summarize participants’ sex. χ2 tests were used to test the group difference for categorical variables. t-test and Mann-Whitney test were used for examining the difference for continuous variables. With the adjustment of age, sex, and education years, we applied a 2 × 2 analysis of covariance (ANCOVA) of the diagnosis of MDD and childhood maltreatment on summary and factor scores of CD-RISC. Generalized linear models (GLMs) were applied to analyze the relationships between childhood maltreatment and resilience by adjusted models 1–2. The adjusted model 1 with adjustment of age, sex, and education, and adjusted model 2 was adjusted for age, sex, education, HAMD24, HAMA14, total history, and episode counts. The GLMs were applied separately for participants in MDD and HC groups. Statistical analyses were tested by SPSS 22.0. Two-tail P values < 0.05 were considered statistically significant in the analyses.
Results
Descriptive statistics
The demographics and clinic information of included participants were presented in Table 1. The educational years of the MDD group (11 years) are shorter than that of the HC group (12 years). For participants in the MDD group, 7 (6.9%) experienced EA in their childhood, 10 (9.9%) experienced SA in their childhood, 32 (31.7%) were exposed to EN in their childhood, 48 (47.5%) experienced PN in their childhood, and 7 (6.9%) experienced PA in their childhood, according to the results of CTQ. According to the CTQ scores, 46 (45.5%) participants in MDD did not experience any childhood maltreatment, 21 (20.8%) experienced one type of childhood maltreatment, 26 (25.7%) experienced two types of childhood maltreatment, 5 (5.0%) were exposed to three types of childhood maltreatment, and 3 (3.0%) experience four types of childhood maltreatment. For participants in the HC group, 6 (5.2%) experienced EA in their childhood, 7 (6.0%) were exposed to PA in their childhood, 43 (37.1%) experienced PN in their childhood, 27 (23.3%) experienced EN in their childhood, and 10 (8.6%) experienced SA in their childhood. According to the results of CTQ, 61 (52.6%) participants in the HC group did not experience any childhood maltreatment, 29 (25.0%) experienced one type of childhood maltreatment, 18 (15.5%) experienced two types of childhood maltreatment, 5 (4.3%) experienced three types of childhood maltreatment, 2 (1.7%) experienced four types of childhood maltreatment, and 1 (0.9%) experienced five types of childhood maltreatment. Table 2 showed the differences in CTQ scores and CD-RISC scores between MDD and HC groups. Factor scores of EA and PN in the MDD group were higher than those in the HC group. The total score of CD-RISC and factor scores of strength, optimism, and tenacity in the HC group were higher than those in the MDD group.
Effects of diagnosis of MDD and childhood maltreatment on CD-RISC total and factor scores
Table 3 showed the results of a 2 × 2 ANCOVA (factor 1: diagnosis of MDD and factor 2: childhood maltreatment) on CD-RISC total and factor scores with the adjustment of age, gender, and educational years. There is no significant two-way interaction effect of a diagnosis of MDD and childhood maltreatment found for CD-RISC total and factor scores. Different main effects of a diagnosis of MDD were tested on CD-RISC total and factor scores. As for the main effect of childhood maltreatment, it presented a statistically significant difference in optimism scores, the difference was 7.179 (P = 0.006).
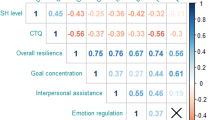
Association between CTQ total score and CD-RISC factor scores
The results of adjusted GLMs were presented in Tables 4 and 5. In adjusted model 1, CTQ total score had a negative association with optimism score (β=-0.081[95%CI,-0.129 to -0.033], P = 0.001) among participants in the MDD group, and similar results were found in adjusted model 2. For participants in the HC group, CTQ total score had a negative association with tenacity score (β=-0.005[95%CI,-0.008 to -0.002], P = 0.001) and optimism score (β=-0.007[95%CI,-0.012 to -0.002], P = 0.010) in adjusted model 1. After adjusting for age, sex, educational years, HAMD24, and HAMA14, similar associations were found in adjusted model 2 in Table 5.
Association between CTQ factor scores and CD-RSIC factor scores
In Table 4, among participants in the MDD group, adjusted model 1 showed negative associations between factor scores of EA and tenacity score (β=-0.643[95%CI,-1.262 to -0.024], P = 0.042), higher EN score was related to worse optimism score (β=-0.169[95%CI,-0.259 to -0.079], P = 0.001), and higher PN score was associated with worse optimism score (β=-0.153[95%CI,-0.301 to -0.005], P = 0.043). The associations which were found in adjusted model 1 among patients with MDD were statistically significant in adjusted model 2. For participants in the HC group, a higher EN score was associated with a worse tenacity score (β=-0.016 [95%CI,-0.022 to -0.009], P < 0.001), strength score (β=-0.011 [95%CI,-0.019 to -0.004], P = 0.004), and optimism score (β=-0.017 [95%CI,-0.029 to -0.006], P = 0.003) with the adjustment of age, sex, and educational years. Negative associations were also found between factor scores of PN and tenacity score (β=-0.019 [95%CI,-0.028 to -0.010], P < 0.001), strength score (β=-0.014 [95%CI,-0.02 5to -0.003], P = 0.012), and optimism score (β=-0.025 [95%CI,-0.042 to -0.008], P = 0.003) in adjusted model 1. The associations which were found in adjusted model 1 were statistically significant in adjusted model 2.
Association between counts of positive CTQ factors and CD-RISC factor scores
For patients with MDD, a negative association between counts of positive CTQ factors and optimism scores was significant in both adjusted model 1 (β=-0.489[95%CI,-0.970 to -0.009], P = 0.046) and adjusted model 2 (β=-0.579[95%CI,-1.057 to -0.100], P = 0.018). However, negative associations between counts of positive CTQ factors and tenacity scores (β=-0.037[95%CI,-0.065 to -0.010], P = 0.008) and optimism scores (β=-0.053[95%CI,-0.104 to -0.002], P = 0.040) were only statistically significant in adjusted model 1.
Discussion
Previous studies conducted in China focused on testing the mediating roles of resilience on the relationship between childhood maltreatment and depression [31,32,33], mainly among youth [34] and adolescents [35]. Our study focused on the relationship between childhood maltreat and resilience among patients with MDD and HCs in adulthood by using baseline data of a longitudinal study. This study found that the specific features of childhood maltreatment had different associations with resilience capacity in adult patients with MDD and HCs. Participants in the HC group had higher overall and factor scores of CTQ than participants in the MDD group. Child neglect had detrimental effects on tenacity, strength, and optimism among participants in the HC group, however, a negative association was found between optimism and child neglect for patients with MDD. EA was negatively associated with tenacity for patients with MDD. This study provides evidence for further understanding of the relationship between CM and adult resilience in patients with MDD and HCs.
We found that participants in the MDD group showed lower optimism scores than those in the HC group. Previous studies suggested that the interactive association between optimism and depression, individuals experiencing high levels of depression symptoms reduced their optimism bias when they met with a life event [36], meanwhile, people with low levels of dispositional optimism would have more harmful or dysfunctional expectations about their future [37]. This may suggest that optimism could have a protective function against adverse mental health outcomes, and the underlying mechanism could be that individuals with high optimism were more likely to exert efforts to manage stress actively and less likely to disengage in the face of adversities [38]. Childhood maltreatment was associated with worse optimism among individuals in both MDD and HC groups. This is along with previous studies [39, 40] showing that childhood maltreatment was linked to low dispositional optimism. One possible explanation might be that childhood maltreatment changes children’s cognitive beliefs and even their ability to have positive mental imagery of the future [39]. Besides, the effect size of the relationship between childhood maltreatment and optimism among participants in the MDD group is higher than that in the HC group. Childhood neglect, including PN and EN, was linked to adults’ worse optimism, tenacity, and strength for participants in the HC group. But for patients with MDD, a negative association was only found between child neglect and adults’ optimism. This is different from the conclusion of Chen’s study [41], in which they suggested that neglect is often unintentional and may not have deleterious effects on optimism as abuse. This is probably because Chen’s study was conducted on data from the PTSD population, which have differences from participants in our analysis. Besides, the possible explanation on the results that the negative associations between EN and PN, and tenacity disappeared in patients with MDD were the genetic effects on resilience [42], patients with MDD might be with lower tenacity capacity with the cause of some genetic reasons, instead of the effects of childhood maltreatment. Our results suggested that promotion optimism might be an effective way to lessen the likelihood of MDD development and severity in people with childhood maltreatment experience.
EA in childhood had an association with worse tenacity among patients with MDD. This finding is similar to two previous studies, one of which reported that EA had the highest magnitude of impact on resilience after adjusting for psychological distress; and another study [43] presented that associations between EA and higher levels of negative traits and lower levels of positive traits. The possible explanations were as follows: EA is known to disrupt individuals’ development of self-concept, impairing emotion regulation, and leading to negative self-perceptions [44], and this psychological impact might be harmful to long-term adjustment, reducing their confidence when facing challenges [22]. Since EA might be more chronic than other kinds of maltreatment, which could be more deleterious for future psychological function [22].
Along with the results of studies among the general population, our analysis showed that childhood maltreatment was related to tenacity only in the HC group. Poole et al. 2017 [45] suggested that a stronger relationship between childhood maltreatment and depression existed among individuals with low resilience than among those with high resilience. Resilience could be regarded as a dynamic personality trait that may be enhanced through practice and training. It is important to figure out the high risk of the population with low resilience, such as adults with childhood maltreatment, and provide resilience-training programs (e.g. The Penn Resiliency Program) for these target individuals. It was reported that resilience-training programs could foster personal characteristics [46] and had been shown to improve the rate of depressive symptoms [47].
The number of positive CTQ factors was only significantly associated with lower optimism among patients with MDD. Besides, counts of positive CTQ factors were no longer significantly related to optimism after controlling for current depression and anxiety severity in the general population. Results from previous cross-sectional studies showed that the negative associations between the number of childhood maltreatment types [48] or adverse childhood events [45] and resilience capacity were small among the general population. The general population included in our analysis was small, and it is possible that no significant association was tested in this small general sample. Unlike the previous study’s findings [22], our results did not suggest that the complexity of childhood maltreatment exposure with multiple types might be specifically noxious for adults’ resilience. Our results may indicate that cumulative adversity models are limited since the models assumed that adverse effects across childhood maltreatment types were additive and equal. The assumption may not be appropriate [49]. More research with a larger sample should be conducted to examine the cumulative adversity models.
Our study has some clinical and practical implications. First, this study revealed that childhood maltreatment was a risk for poor performance of resilience in adult patients with MDD, suggesting the importance of identifying childhood maltreatment and assessments of resilience in the clinical management of MDD. Second, resilience training may be a promising and viable intervention for patients with MDD who exposures to childhood maltreatment when established treatment strategies. Additionally, general adults with childhood maltreatment should also be advised to take some resilience training in the community, in order to cope with the adverse impacts associated with childhood adversity. According to previous studies [50, 51], CBT can effectively increase resilience. When administering medication to patients with MDD, particularly those who have a history of childhood maltreatment, CBT may also be an alternative option to enhance resilience.
Strengths and limitations.
Previous research on the relationship between childhood trauma and resilience has focused on adolescents, with very little research on adults with MDD. The present study provides further evidence on the relationship between childhood trauma and resilience by including medication-free patients with MDD and HCs. To be more specific, based on a Chinese sample, this study explored the associations between various features of childhood maltreatment and summary and factor scores of resilience capacity in adulthood. Besides, this study compared the different relationships between patients with MDD and HCs to better understand the impacts of childhood maltreatment on resilience. However, there were several limitations in the present study. Firstly, this analysis was based on baseline data from a longitudinal study, inference on the causal relationship between childhood maltreatment and resilience could not be made. Further exploration based on longitudinal data was needed to examine these relationships. Second, the participants’ childhood maltreatment and resilience were self-reported, and recall bias may influence our results and conclusion. Third, the conclusion derived from this analysis was based on data that was from a psychiatric hospital and nearby community, which was not a representative sample of the whole Chinese population, it is unclear yet whether the findings could be proved in other population.
Conclusion
In conclusion, the present study investigated the influence of childhood maltreatment on resilience in patients with MDD and HCs. We found that childhood maltreatment were the risk factors for lower optimism, and EA might be responsible for the poor performance of tenacity in patients with MDD. These findings highlight the importance of early identification of childhood maltreatment and specific training on resilience in the treatment course of MDD.
Data Availability
All data generated or analyzed during this study are included in this article.
References
Etain B, Mathieu F, Henry C, Raust A, Roy I, Germain A, et al. Preferential association between childhood emotional abuse and bipolar disorder. J Trauma Stress. 2010;23(3):376–83.
Finkelhor D, Ormrod R, Turner H, Hamby SL. The victimization of children and youth: a comprehensive, national survey. Child Maltreat. 2005;10(1):5–25.
Finkelhor D, Turner H, Ormrod R, Hamby SL. Violence, abuse, and crime exposure in a national sample of children and youth. Pediatrics. 2009;124(5):1411–23.
Fang X, Fry DA, Ji K, Finkelhor D, Chen J, Lannen P, et al. The burden of child maltreatment in China: a systematic review. Bull World Health Organ. 2015;93(3):176–85c.
Ji K, Finkelhor D. A meta-analysis of child physical abuse prevalence in China. Child Abuse Negl. 2015;43:61–72.
Chen J-Q, Han P, Lian G-L, Dunne MP. Prevalence of childhood sexual abuse among 2508 college students in 6 provinces of China. Zhonghua liu Xing Bing xue za zhi. 2010;31(8):866–9.
Mueller-Pfeiffer C, Moergeli H, Schumacher S, Martin-Soelch C, Wirtz G, Fuhrhans C, et al. Characteristics of child maltreatment and their relation to dissociation, posttraumatic stress symptoms, and depression in adult psychiatric patients. J Nerv Ment Dis. 2013;201(6):471–7.
Breslau N, Koenen KC, Luo Z, Agnew-Blais J, Swanson S, Houts RM, et al. Childhood maltreatment, juvenile disorders and adult post-traumatic stress disorder: a prospective investigation. Psychol Med. 2014;44(9):1937–45.
Howell KH, Miller-Graff LE. Protective factors associated with resilient functioning in young adulthood after childhood exposure to violence. Child Abuse Negl. 2014;38(12):1985–94.
Green JG, McLaughlin KA, Berglund PA, Gruber MJ, Sampson NA, Zaslavsky AM, et al. Childhood adversities and adult psychiatric disorders in the national comorbidity survey replication I: associations with first onset of DSM-IV disorders. Arch Gen Psychiatry. 2010;67(2):113–23.
Meng X, Fleury MJ, Xiang YT, Li M, D’Arcy C. Resilience and protective factors among people with a history of child maltreatment: a systematic review. Soc Psychiatry Psychiatr Epidemiol. 2018;53(5):453–75.
Cicchetti D, Rogosch FA. Adaptive coping under conditions of extreme stress: multilevel influences on the determinants of resilience in maltreated children. New Dir Child Adolesc Dev. 2009;2009(124):47–59.
Sweetman D, Luthans F, Avey JB, Luthans BC. Relationship between positive psychological capital and creative performance. 2011;28(1):4–13.
Artuch-Garde R, González-Torres MDC, de la Fuente J, Vera MM, Fernández-Cabezas M, López-García M. Relationship between Resilience and Self-regulation: a study of Spanish Youth at Risk of Social Exclusion. Front Psychol. 2017;8:612.
Davydov DM, Stewart R, Ritchie K, Chaudieu I. Resilience and mental health. Clin Psychol Rev. 2010;30(5):479–95.
Chmitorz A, Kunzler A, Helmreich I, Tüscher O, Kalisch R, Kubiak T, et al. Intervention studies to foster resilience - A systematic review and proposal for a resilience framework in future intervention studies. Clin Psychol Rev. 2018;59:78–100.
Choi KW, Stein MB, Dunn EC, Koenen KC, Smoller JW. Genomics and psychological resilience: a research agenda. Mol Psychiatry. 2019;24(12):1770–8.
Mancini AD, Bonanno GA. Resilience in the face of potential trauma: clinical practices and illustrations. J Clin Psychiatry. 2006;62(8):971–85.
Daniels JK, Hegadoren KM, Coupland NJ, Rowe BH, Densmore M, Neufeld RW, et al. Neural correlates and predictive power of trait resilience in an acutely traumatized sample: a pilot investigation. J Clin Psychiatry. 2011;72(3):12580.
Hourani L, Bender RH, Weimer B, Peeler R, Bradshaw M, Lane M, et al. Longitudinal study of resilience and mental health in marines leaving military service. J Affect Disord. 2012;139(2):154–65.
Campbell-Sills L, Forde DR, Stein MB. Demographic and childhood environmental predictors of resilience in a community sample. J Psychiatr Res. 2009;43(12):1007–12.
Nishimi K, Choi KW, Davis KA, Powers A, Bradley B, Dunn EC. Features of Childhood Maltreatment and Resilience Capacity in Adulthood: results from a large community-based sample. J Trauma Stress. 2020;33(5):665–76.
Wu L, Tan Y, Liu Y. Factor structure and psychometric evaluation of the Connor-Davidson resilience scale in a new employee population of China. BMC Psychiatry. 2017;17(1):49.
Yu X, Zhang J, Yu XN, Zhang JX, FACTOR ANALYSIS AND PSYCHOMETRIC EVALUATION OF, THE CONNOR-DAVIDSON RESILIENCE SCALE (CD-RISC) WITH CHINESE PEOPLE. Social Behav Personality: Int J. 2007;35(1):19–30.
Fu W, Yao S. Initial reliability and validity of Childhood Trauma Questionnaire (CTQ-SF) applied in chinese college students. Chin J Clin Psychol. 2005;13:40–2.
Bernstein DP, Stein JA, Newcomb MD, Walker E, Pogge D, Ahluvalia T, et al. Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse Negl. 2003;27(2):169–90.
Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23(1):56.
Yuhua T, Mingyuan Z. Hamilton depression scale (HAMD). Shanghai Psychiatry. 1984;2:61–4.
Hamilton M. The assessment of anxiety states by rating. Br J Med Psychol. 1959.
Wang C, Chu Y, Zhang Y, Zhang N, Zhang J, Yang H. Study on factor structure of hamilton rating scale for anxiety. J Clin Psychiatry. 2011;21:299–301.
Zheng K, Chu J, Zhang X, Ding Z, Song Q, Liu Z, et al. Psychological resilience and daily stress mediate the effect of childhood trauma on depression. Child Abuse Negl. 2022;125:105485.
Wang H, Liao Y, Guo L, Zhang H, Zhang Y, Lai W, et al. Association between childhood trauma and medication adherence among patients with major depressive disorder: the moderating role of resilience. BMC Psychiatry. 2022;22(1):644.
Cao H, Zhang R, Li L, Yang L. Coping Style and Resilience Mediate the Effect of Childhood Maltreatment on Mental Health Symptomology. Children (Basel, Switzerland). 2022;9(8).
Wang YC, Moya Guerola M, Lin YC, Hsieh YP, Strong C, Tsai MC, et al. Effects of childhood adversity and resilience on taiwanese youth health behaviors. Pediatr Neonatol. 2019;60(4):368–76.
Wei J, Shi J, Zhang M, Ding H, Kang C, Wang K, et al. Childhood trauma and its correlation with resilience among primary and middle school students in Wuhan city in 2015. Wei Sheng yan jiu = Journal of Hygiene Research. 2019;48(5):717–27.
Hobbs C, Vozarova P, Sabharwal A, Shah P, Button K. Is depression associated with reduced optimistic belief updating? Royal Soc open Sci. 2022;9(2):190814.
Uribe FAR, de Oliveira SB, Junior AG, da Silva Pedroso J. Association between the dispositional optimism and depression in young people: a systematic review and meta-analysis. Psicologia, reflexao e critica: revista semestral do Departamento de Psicologia da UFRGS. 2021;34(1):37.
Conversano C, Rotondo A, Lensi E, Della Vista O, Arpone F, Reda MA. Optimism and its impact on mental and physical well-being. Clin Pract Epidemiol Mental Health. 2010;6:25.
Broekhof R, Rius-Ottenheim N, Spinhoven P, van der Mast RC, Penninx BW, Zitman FG, et al. Long-lasting effects of affective disorders and childhood trauma on dispositional optimism. J Affect Disord. 2015;175:351–8.
Mersky JP, Topitzes J. Comparing early adult outcomes of maltreated and non-maltreated children: a prospective longitudinal investigation. Child Youth Serv Rev. 2010;32(8):1086–96.
Chen J, Christ NM, Shih C-H, Xie H, Grider SR, Lewis C, et al. Dispositional optimism mediates relations between childhood maltreatment and PTSD symptom severity among trauma-exposed adults. Child Abuse Negl. 2021;115:105023.
Maul S, Giegling I, Fabbri C, Corponi F, Serretti A, Rujescu D. Genetics of resilience: implications from genome-wide association studies and candidate genes of the stress response system in posttraumatic stress disorder and depression. Am J Med Genet Part B Neuropsychiatric Genetics: Official Publication Int Soc Psychiatric Genet. 2020;183(2):77–94.
Sudbrack R, Manfro PH, Kuhn IM, de Carvalho HW, Lara DR. What doesn’t kill you makes you stronger and weaker: how childhood trauma relates to temperament traits. J Psychiatr Res. 2015;62:123–9.
Cecil CA, Viding E, Fearon P, Glaser D, McCrory E. Disentangling the mental health impact of childhood abuse and neglect. Child Abuse Negl. 2017;63:106–19.
Poole JC, Dobson KS, Pusch D. Childhood adversity and adult depression: the protective role of psychological resilience. Child Abuse Negl. 2017;64:89–100.
Schulz A, Becker M, Van der Auwera S, Barnow S, Appel K, Mahler J, et al. The impact of childhood trauma on depression: does resilience matter? Population-based results from the study of Health in Pomerania. J Psychosom Res. 2014;77(2):97–103.
Brunwasser SM, Gillham JE, Kim ES. A meta-analytic review of the Penn Resiliency Program’s effect on depressive symptoms. J Consulting Clin Psychol. 2009;77(6):1042.
Edwards KM, Probst DR, Rodenhizer-Stämpfli KA, Gidycz CA, Tansill EC. Multiplicity of child maltreatment and biopsychosocial outcomes in young adulthood: the moderating role of resiliency characteristics among female survivors. Child Maltreat. 2014;19(3–4):188–98.
Lanier P, Maguire-Jack K, Lombardi B, Frey J, Rose RA. Adverse childhood experiences and child health outcomes: comparing cumulative risk and latent class approaches. Maternal Child Health Journal. 2018;22(3):288–97.
Zhang P, Mo L, Torres J, Huang X. Effects of cognitive behavioral therapy on psychological adjustment in chinese pediatric cancer patients receiving chemotherapy: a randomized trial. Medicine. 2019;98(27):e16319.
Brandalise MH, de Araujo Filho GM, Centeno RS, Yacubian EMT, Jackowski AP. Effects of a brief psychotherapeutic intervention on resilience and behavior in patients with drug-resistant mesial temporal lobe epilepsy and late seizure recurrence after surgery. Epilepsy & Behavior: E&B. 2019;100(Pt A):106512.
Acknowledgements
The authors thank all the participants for participating in this study.
Funding
This work was supported by the National Science and Technologic Program of China (2015BAI13B02), the Defense Innovative Special Region Program (17-163-17-XZ-004-005-01), the National Natural Science Foundation of China (81171286, 91232714 and 81601180), the STI2030-Major Projects (2021ZD0202000). The funders had no role in study design, data collection, and analysis, decision to publish, or manuscript preparation.
Author information
Authors and Affiliations
Contributions
Prof. Lingjiang Li, Prof. Yan Zhang and Dr. Bangshan Liu co-conceptualized and co-designed the study. Dr. Liu (Bangshan) reviewed and supervised the analysis and the manuscript. Dr. Liu (Jin) reviewed the manuscript and supervised the review and revision process. Miss Guanyi Lv and Dr. Yumeng Ju, Mi Wang, Jinrong Sun, Xiaowen Lu, Qiangli Dong, Liang Zhang, Ping Wan, Hua Guo and Futao Zhao recruited participants and collected data. Miss Li carried out the initial analysis, and drafted and revised the manuscript. Miss Guanyi Lv critically contributed important intellectual contents to the manuscript. All authors have read and approved the manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All methods were carried out following the Declaration of Helsinki. Written informed consent was provided by each participant, and the study design was reviewed and approved by the Medical Ethics Committees of the Second Xiangya Hospital of Central South University and the Zhumadian Psychiatric Hospital.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Li, C., Lv, G., Liu, B. et al. Impact of childhood maltreatment on adult resilience. BMC Psychiatry 23, 637 (2023). https://doi.org/10.1186/s12888-023-05124-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12888-023-05124-w



