Abstract
Background
At present, there is not enough evidence to prove the relationship between blood lipid and electrocardiogram (ECG) abnormalities in common mental disorders (CMD). This study aimed to explore the relationship between them, to detect and prevent arrhythmia or sudden death.
Methods
We collected 272 CMD patients (maintained a fixed drug dose pattern for 1 year or more), including 95 schizophrenias (SC), 90 bipolar disorders (BD) and 87 major depressive disorders (MDD), and 78 healthy controls (HC) from the Third People’s Hospital of Foshan, China. We analyzed and compared their blood lipid and ECG indicators, to clarify the relationship between them.
Results
350 participants were included. There were no significant differences in age, gender, total cholesterol (TC), low density lipoprotein (LDL) and QTc (p > 0.05) among subjects. And there were significant differences in body mass index (BMI), triglyceride (TG), high density lipoprotein (HDL), heart rate, PR interval and QRS width (p < 0.05). Person correlation analysis showed that QRS width was positively correlated with BMI and TG. And negatively correlated with HDL. Meanwhile, QTc was positively correlated with BMI. Multiple linear regional analysis further proved that TG (B = 3.849, p = 0.007) and LDL (B = 11.764, p = 0.018) were the risk factors, and HDL (B = -9.935, p = 0.025) was the protective factor for QRS width increase.
Conclusion
Long term medication of CMD patients should strengthen weight management, and conduct regular blood lipid and ECG examinations to achieve early detection and intervention in order to promote their health.
Similar content being viewed by others
Introduction
Common mental disorders (CMD) include major depressive disorders (MDD), bipolar disorders (BD), schizophrenias (SC), and so on [1, 2]. Long-term use of psychotropic drugs may affect heart function and cause abnormal lipid metabolism [3,4,5].
Studies have shown the correlation between mental illnesses such as MDD, BD, SC and obesity [6, 7]. On one hand, mental illnesses may lead to poor lifestyle choices such as an unhealthy diet and lack of exercise, resulting in obesity [8, 9]. On the other hand, obesity itself may cause mental health issues as weight gain can lead to self-image problems and further increase psychological stress. In addition, some anti-psychotic medications can also cause weight gain and abnormal blood lipid levels [10, 11], which may result in abnormal cardiovascular changes and increase the risk of sudden death [12,13,14].
ECG is cheap, convenient, fast, ready-made and non-invasive, therefore, it is important to regularly test the blood lipids and ECG [15,16,17]. Among the common ECG indicators (heart rate, PR, QRS width and QTc), QTc was considered one of the monitoring indicators for prevention of sudden death in patients with mental disorders [18, 19]. However, other ECG indicators were not paid much attention.
Thus, we included patients with CMD who had taken drugs steadily for one year or more. Through venous blood testing, we learned about their blood lipids situation, compared with various ECG indicators, and tried to clarify the relationship between them, which provided reference for patients’ health monitoring and clinical intervention.
Methods
Participants
This was a prospective study. Subjects with SC, BD and MDD were included in this study, who met the diagnostic criteria of the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) from July 2017 to September 2022 in the Third People’s Hospital of Foshan, Guangdong, China. Their age was ≥ 18 and < 45 years old. They were required to maintain a fixed drug dose pattern for 1 year or more before blood testing.
Healthy controls (HC): volunteers recruited through advertising in Foshan from March 2020 to December 2021; ①18–45 years old; ②No history or family history of psychosis was confirmed through an interview with a psychiatrist; ③Gender and age were matched with the patient group.
Exclusion criteria: ①Comorbidity of other mental disorders, such as intellectual disability, anxiety disorders, personality disorders, or other cognitive impairment, was assessed and excluded using the Structured Clinical Interview for DSM-IV (SCID); ②Patients with severe and unstable physical diseases, including severe liver and kidney function damage, cardiac insufficiency, diabetes, etc.; ③Smoking habits (≥ 1 cigarette per day) or drinking habits (≥ 1 unit alcohol per week); 1 unit alcohol = 480 ~ 600 ml of beer = 350 ml of low alcohol liquor or red wine, yellow wine = 50 ml of high spirits (that is 40 degrees or more) [2]; ④Did not cooperate with venous blood drawing, such as phobia, etc.
We obtained written informed consent from patients or their legal guardians. This study was approved by the ethics committee of the Third People’s Hospital of Foshan, China and the experiments were conducted following the declaration of Helsinki.
Assessments
For the subjects who met the above conditions and were willing to participate in this study, after signed the informed consent, collected their names, gender and age through interviews. The height and weight of the subjects were evaluated by the nurses and the BMI (kg/m2) values of each subject were calculated.
Before drawing the venous blood of the subjects, they were required to be fasting for more than 8 h, and the nurses were required to complete the blood drawing from 7:30 to 10:00 in the morning. The night before blood drawing, they should maintain a normal diet, follow the previous work and rest, and should not drink alcohol or coffee after dinner. TC, TG, HDL and LDL were measured using the Mindray BS2000 Modular Analysis System (www.mindray.com/cn/products/laboratory-diagnostics/chemistry/modular-analysis-system/bs-2000 m) which Launched in 2013 and were recorded in the clinical data sheet of the subjects.
ECG measurement: ①Exposed the parts of the body that require electrodes, including both wrists and ankles. ②Limb leads were clamped to the corresponding limbs respectively, and the electrodes on the leads contacted the skin of the limbs. V1 was placed in the fourth intercostal space on the right edge of the sternum, V2 was located in the fourth intercostal space on the left edge of the sternum, V4 was located at the junction of the left clavicular midline and the fifth intercostal space, V3 was located between V2 and V4, V5 was located at the junction of the axillary front line and the fifth intercostal space, and V6 was located at the junction of the axillary midline and the fifth intercostal space. ③The ECG recorded the electrical activity of the heart for one minute, and the doctor in the ECG room read the chart and recorded the values of heart rate, PR interval, QRS width, and QTc.
Data analyses
Statistical Product and Service Solutions 21 software (SPSS 21, https://www.ibm.com/analytics/spss-statisticssoftware) was used to analyze the data. Chi-square test and one way ANOVA were used to compare the differences in general demographic, then Bonferroni post-hoc analyses were performed. The relationships between BMI and variable indexes were analyzed by Pearson correlation, which adjusted for age and gender. Next, the obtained p values were then corrected by false discovery rate (FDR) correction. Taking heart rate, PR interval, QRS width, and QTc as dependent variables (Y), BMI, TG, TC, HDL and LDL as independent variables (X), age and gender as covariates, stepwise multiple linear regression models were established to analyze the effects of blood index components on ECG index.
Results
Comparison of demographic characteristics, metabolic indexes and ECG indexes
363 subjects took part in this study, including SC (n = 95), BD (n = 90), MDD (n = 87), and HC (n = 78), while 13 subjects were excluded due to consumption of breakfast before drawing blood. There were no significant differences in age, gender, TC, LDL and QTc (p > 0.05) among subjects. And there were significant differences in BMI, TG, HDL, heart rate, PR interval and QRS width (p < 0.05). Bonferroni post-hoc analyses showed that compared the BMI and blood lipid indexes of CMD and HC, we found that the BMI of MDD (p = 0.002) was significantly lower than that of HC. We also found that the BMI of SC (p < 0.001) and BD (p < 0.001) was significantly higher than that of MDD. What’s more, TG of SC (p = 0.021) was significantly higher than that of MDD. Our results indicated that HDL of SC was significantly lower than BD (p = 0.013) / MDD (p < 0.001) / HC (p = 0.016).
Compared the ECG indexes of CMD and HC, we found that the heart rate of CMD was increased, and PR interval of SC was significantly shorter than that of BD (p < 0.001) / MDD (p < 0.001) / HC (p < 0.001). Others, we found that QRS width increased significantly in SC. However, it is worth mentioning that the QTc of CMD patients was generally longer than HC, but there is no significant difference. (Table 1)
Pearson correlation between ECG and blood lipid
The results of Person correlation analysis showed that QRS width was positively correlated with BMI and TG. And negatively correlated with HDL. Meanwhile, QTc was positively correlated with BMI. (Table 2)
Multiple linear regression analysis of heart rate, PR interval, QRS width and QTc
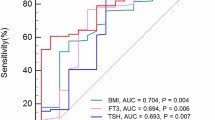
The stepwise multiple linear regression models (FHeart rate = 1.733, p = 0.126; F PR interval = 2.246, p = 0.051; FQRS width = 3.626, p = 0.003; FQTc = 0.986, p = 0.426) were established for analysis. Only the equation (taking QRs width as the dependent variable) passed the fitting requirement (p < 0.05). Finally, the elements entering the model were TG (B = 3.849, p = 0.007), HDL (B = -9.935, p = 0.025) and LDL (B = 11.764, p = 0.018). (Table 3)
Discussion
Our study determined that the blood lipid and ECG indicators of CMD patients were significantly different from HC. Abnormal blood lipid was closely related to the abnormality of ECG. Moreover, HDL was the protective factor of QRs width increase.
Comparing the BMI and blood lipid indexes of CMD and HC, we found that the BMI of MDD was significantly lower than that of HC. It is known to us that antidepressants can cause nausea [5, 20]. At the same time, no appetite is the core symptom of MDD [21], resulting in weight loss, which leads to a decline in BMI. We also found that the BMI of SC and BD was significantly higher than that of MDD. This was consistent with our previous research results. Generally, CMD who received regular medication were more likely to be obese [2, 22]. What’s more, TG of SC was significantly higher than that of MDD. TG synthesized in vivo is mainly in the liver, followed by adipose tissue. Its main function is to supply and store energy, and it can also fix and protect internal organs. However, the increase of TG is related to diet structure and is the risk factor for cardiovascular disease [23, 24]. Previous studies have shown that the diet structure and intestinal flora of SC have specific changes [25,26,27], which made the patient’s diet tend to be unhealthy and result in leading to abnormal TG [28]. HDL is composed of proteins, lipids and their regulatory factors. HDL protein components include apolipoproteins, enzymes, lipid transfer proteins, acute phase response proteins, complement components and other protein components. It can transport the excess cholesterol in the blood to the liver, process and decompose it into cholic acid salts, and excrete it through the bile duct, thus forming a special way of blood lipid metabolism. It can enhance the ability of blood lipid metabolism and keep the blood vessels unblocked [29, 30]. Our results indicated that HDL of SC was significantly lower than BD/MDD/HC, which was related to the use of antipsychotic drugs [31, 32]. Meanwhile, SC itself also had HDL anomalies [33], and Hannah et al. further verified the metabolic abnormalities of SC at the genetic level, which also explained our experimental results [34].
Comparing the ECG indexes of CMD and HC, we found that the heart rate of CMD was increased, and PR interval of SC was significantly shorter than that of BD/MDD/HC. The heart is doubly innervated by sympathetic and parasympathetic nerves. The sympathetic nerve fiber terminals release norepinephrine (NE) and act on myocardial cells’ β1 adrenergic receptors (β1 receptors). Acetylcholine (Ach) released from parasympathetic nerve fiber terminals acts on cholinergic receptors (M receptors) in cardiomyocytes. Psychotropic drug receptors overlap with heart related receptors to some certain extent, thus affecting the change of heart rate and PR interval [35,36,37]. Others, we found that QRS width increased significantly in SC. In clinical practice, in order to better control the psychiatric symptoms of SC, patients need to take sufficient antipsychotic drugs during treatment, which seems to affect the cardiac function inevitably, thus increasing the risk of sudden death of SC [38]. However, it is worth mentioning that the QTc of CMD patients was generally longer than HC, but there is no significant difference. Previous studies showed that the QTc of SC was significantly prolonged [39], which was not completely consistent with our results. With the standardization of diagnosis and treatment for mental disorders, the first-line antipsychotic drugs for clinicians according to the International Clinical Guidelines for psychiatric related diseases are the second-generation antipsychotic drugs [40, 41], and SSRIS drugs were commonly used as antidepressants [42, 43], which have relatively little impact on patients’ heart QT interval. QTc prolongation can be reversible, depending on the underlying cause. The patients selected for this study were those who had been taking medication regularly in a stable phase. After long-term medication use, the heart can tolerate the effects of the medication, resulting in partial recovery of the QTc interval [41, 43, 44]. In addition, the subjects in this study had a long course of illness (≥ 1 year), regular medication treatment, and were mostly in stable stage of the disease. The risk of QTc prolongation in such patients is relatively low [45]. Therefore, these differences may be the reasons for the lack of significant differences in our results.
When we performed Pearson correlation analysis on blood lipid indicators and ECG indicators, the results showed that QRS width was positively correlated with BMI and TG, negatively correlated with HDL, and QTc was positively correlated with BMI. Multiple linear regional analysis determined that TG and LDL were the risk factors, and HDL was the protective factor for QRS width increase. QRS complex reflects changes in depolarization potential and time of left and right ventricles. The time from the starting point of QRS complex to its end point is the QRS time limit. Generally, the time limit of QRS complex is 0.06 ~ 0.10s [46]. The prolongation of QRS duration can be seen in ventricular hypertrophy, bundle branch block, preexcitation syndrome, and intraventricular differential conduction. Our results were consistent with previous studies. TG and LDL were recognized to damage the vascular environment [47], and HDL has a protective effect on cardiovascular system [48].
However, we know that there are many factors affecting blood lipid and ECG, including smoking, drinking, age, race, eating habits, etc. What’s more, our subjects were only from the South China, so we still need to be cautious when generalizing the conclusions.
Above all, long term medication of CMD patients is easy to lead to abnormal blood lipid and ECG. They should strengthen weight management, and conduct regular blood lipid and ECG examinations to achieve early detection and promote their health.
Data Availability
The datasets generated and/or analyzed during the current study are not publicly available due to confidentiality but are available from the corresponding author on reasonable request.
References
Auerbach RP, Mortier P, Bruffaerts R, Alonso J, Benjet C, Cuijpers P, Demyttenaere K, Ebert DD, Green JG, Hasking P, et al. Prevalence and distribution of mental disorders. J Abnorm Psychol. 2018;127(7):623–38. WHO World Mental Health Surveys International College Student Project.
Li X, Shi X, Tan Y, Yu Y, Tang C, Xu G, Zhang X, Liao H, Mai X, Chen W, et al. Metabolic indexes of obesity in patients with common mental disorders in stable stage. BMC Psychiatry. 2022;22(1):91.
Pillinger T, Osimo EF, de Marvao A, Berry MA, Whitehurst T, Statton B, Quinlan M, Brugger S, Vazir A, Cook SA, et al. Cardiac structure and function in patients with schizophrenia taking antipsychotic drugs: an MRI study. Translational psychiatry. 2019;9(1):163.
De Hert M, Detraux J, van Winkel R, Yu W, Correll CU. Metabolic and cardiovascular adverse effects associated with antipsychotic drugs. Nat reviews Endocrinol. 2011;8(2):114–26.
Solmi M, Fornaro M, Ostinelli EG, Zangani C, Croatto G, Monaco F, Krinitski D, Fusar-Poli P, Correll CU. Safety of 80 antidepressants, antipsychotics, anti-attention-deficit/hyperactivity medications and mood stabilizers in children and adolescents with psychiatric disorders: a large scale systematic meta-review of 78 adverse effects. World psychiatry: official journal of the World Psychiatric Association (WPA). 2020;19(2):214–32.
Avila C, Holloway AC, Hahn MK, Morrison KM, Restivo M, Anglin R, Taylor VH. An overview of links between obesity and Mental Health. Curr Obes Rep. 2015;4(3):303–10.
Perry C, Guillory TS, Dilks SS. Obesity and Psychiatric Disorders. Nurs Clin N Am. 2021;56(4):553–63.
Salvador Robert M, Porras-Segovia A, Peñuelas-Calvo I, Baca-Garcia E. Physical comorbidity and use of healthcare services in people with schizophrenia: protocol for a systematic review. BMJ open. 2021;11(12):e053324.
Neumann NU, Frasch K. [The significance of regular physical exercise for health and well-being]. Dtsch Med Wochenschr. 2007;132(45):2387–91.
Uguz F, Sahingoz M, Gungor B, Aksoy F, Askin R. Weight gain and associated factors in patients using newer antidepressant drugs. Gen Hosp Psychiatry. 2015;37(1):46–8.
Himmerich H, Minkwitz J, Kirkby KC. Weight gain and metabolic changes during treatment with Antipsychotics and Antidepressants. Endocr Metab Immune Disord Drug Targets. 2015;15(4):252–60.
Timour Q, Frassati D, Descotes J, Chevalier P, Christé G, Chahine M. Sudden death of cardiac origin and psychotropic drugs. Front Pharmacol. 2012;3:76.
Wu CS, Tsai YT, Tsai HJ. Antipsychotic drugs and the risk of ventricular arrhythmia and/or sudden cardiac death: a nation-wide case-crossover study. J Am Heart Association 2015, 4(2).
Bernardo M, Rico-Villademoros F, García-Rizo C, Rojo R, Gómez-Huelgas R. Real-World Data on the adverse metabolic Effects of Second-Generation Antipsychotics and their potential determinants in adult patients: a systematic review of Population-Based Studies. Adv therapy. 2021;38(5):2491–512.
Lambert TJ, Chapman LH. Diabetes, psychotic disorders and antipsychotic therapy: a consensus statement. Med J Australia. 2004;181(10):544–8.
Philip AB, Dratcu L. Psychotic disorders and electrocardiogram abnormalities in the acute psychiatric setting: more than the metabolic syndrome alone. Int J psychiatry Clin Pract. 2021;25(1):103–5.
Antoniou CK, Bournellis I, Papadopoulos A, Tsiachris D, Arsenos P, Dilaveris P, Diakogiannis I, Sideris S, Kallikazaros I, Gatzoulis KA, et al. Prevalence of late potentials on signal-averaged ECG in patients with psychiatric disorders. Int J Cardiol. 2016;222:557–61.
Carrà G, Crocamo C, Bartoli F, Lax A, Tremolada M, Lucii C, Martinotti G, Nosè M, Bighelli I, Ostuzzi G, et al. First-generation antipsychotics and QTc: any role for mediating variables? Human Psychopharmacol. 2016;31(4):313–8.
Ali Z, Ismail M, Nazar Z, Khan F, Khan Q, Noor S. Prevalence of QTc interval prolongation and its associated risk factors among psychiatric patients: a prospective observational study. BMC Psychiatry. 2020;20(1):277.
Alonso-Pedrero L, Bes-Rastrollo M, Marti A. Effects of antidepressant and antipsychotic use on weight gain: a systematic review. Obes reviews: official J Int Association Study Obes. 2019;20(12):1680–90.
Otte C, Gold SM, Penninx BW, Pariante CM, Etkin A, Fava M, Mohr DC, Schatzberg AF. Major depressive disorder. Nat reviews Disease primers. 2016;2:16065.
Liang J, Cai Y, Xue X, Li X, Li Z, Xu C, Xie G, Yu Y. Does Schizophrenia itself cause obesity? Front Psychiatry. 2022;13:934384.
Oikonomou EK, Antoniades C. The role of adipose tissue in cardiovascular health and disease. Nat reviews Cardiol. 2019;16(2):83–99.
Esan O, Wierzbicki AS. Triglycerides and cardiovascular disease. Curr Opin Cardiol. 2021;36(4):469–77.
Cryan JF, O’Riordan KJ, Cowan CSM, Sandhu KV, Bastiaanssen TFS, Boehme M, Codagnone MG, Cussotto S, Fulling C, Golubeva AV, et al. The Microbiota-Gut-Brain Axis. Physiol Rev. 2019;99(4):1877–2013.
Dickerson F, Severance E, Yolken R. The microbiome, immunity, and schizophrenia and bipolar disorder. Brain Behav Immun. 2017;62:46–52.
Zhuang Z, Yang R, Wang W, Qi L, Huang T. Associations between gut microbiota and Alzheimer’s disease, major depressive disorder, and schizophrenia. J Neuroinflamm. 2020;17(1):288.
Pu Z, Sun Y, Jiang H, Hou Q, Yan H, Wen H, Li G. Effects of Berberine on Gut Microbiota in patients with mild metabolic Disorders Induced by Olanzapine. Am J Chin Med. 2021;49(8):1949–63.
Jackson AO, Meng J, Tang H, Yin K. High-density lipoprotein-mediated cardioprotection in heart failure. Heart Fail Rev. 2021;26(4):767–80.
Jia C, Anderson JLC, Gruppen EG, Lei Y, Bakker SJL, Dullaart RPF, Tietge UJF. High-density lipoprotein anti-inflammatory capacity and Incident Cardiovascular events. Circulation. 2021;143(20):1935–45.
Pillinger T, McCutcheon RA, Vano L, Mizuno Y, Arumuham A, Hindley G, Beck K, Natesan S, Efthimiou O, Cipriani A, et al. Comparative effects of 18 antipsychotics on metabolic function in patients with schizophrenia, predictors of metabolic dysregulation, and association with psychopathology: a systematic review and network meta-analysis. The lancet Psychiatry. 2020;7(1):64–77.
Zhang Y, Wang Q, Reynolds GP, Yue W, Deng W, Yan H, Tan L, Wang C, Yang G, Lu T et al. Metabolic Effects of 7 antipsychotics on patients with Schizophrenia: a Short-Term, randomized, Open-Label, Multicenter, Pharmacologic Trial. J Clin Psychiatry 2020, 81(3).
Douglas J, Nasrallah HA. Low high-density lipoprotein and psychopathology: a review. Annals of clinical psychiatry: official journal of the American Academy of Clinical Psychiatrists. 2019;31(3):209–13.
Jones HJ, Borges MC, Carnegie R, Mongan D, Rogers PJ, Lewis SJ, Thompson AD, Zammit S. Associations between plasma fatty acid concentrations and schizophrenia: a two-sample mendelian randomisation study. The lancet Psychiatry. 2021;8(12):1062–70.
Behlke LM, Lenze EJ, Carney RM. The Cardiovascular Effects of newer Antidepressants in older adults and those with or at High Risk for Cardiovascular Diseases. CNS Drugs. 2020;34(11):1133–47.
Zhu J, Hou W, Xu Y, Ji F, Wang G, Chen C, Lin C, Lin X, Li J, Zhuo C, et al. Antipsychotic drugs and sudden cardiac death: a literature review of the challenges in the prediction, management, and future steps. Psychiatry Res. 2019;281:112598.
Polcwiartek C, Kragholm K, Hansen SM, Atwater BD, Friedman DJ, Barcella CA, Graff C, Nielsen JB, Pietersen A, Nielsen J, et al. Electrocardiogram characteristics and their Association with psychotropic drugs among patients with Schizophrenia. Schizophr Bull. 2020;46(2):354–62.
Blom MT, Cohen D, Seldenrijk A, Penninx BW, Nijpels G, Stehouwer CD, Dekker JM, Tan HL. Brugada syndrome ECG is highly prevalent in schizophrenia. Circulation Arrhythmia and electrophysiology. 2014;7(3):384–91.
Cao H, Zhou Y, Li T, Yao C, Yang W, Kong S, Wang Y, Yu B, Jiao Q, Sun Y, et al. The prevalence, risk factors and clinical correlates of QTc prolongation in chinese hospitalized patients with chronic Schizophrenia. Front Psychiatry. 2021;12:704045.
Stępnicki P, Kondej M, Kaczor AA. Current concepts and treatments of Schizophrenia. Molecules 2018, 23(8).
Beach SR, Celano CM, Noseworthy PA, Januzzi JL, Huffman JC. QTc prolongation, torsades de pointes, and psychotropic medications. Psychosomatics. 2013;54(1):1–13.
Feng Y, Xiao L, Wang WW, Ungvari GS, Ng CH, Wang G, Xiang YT. Guidelines for the diagnosis and treatment of depressive disorders in China: the second edition. J Affect Disord. 2019;253:352–6.
Beach SR, Kostis WJ, Celano CM, Januzzi JL, Ruskin JN, Noseworthy PA, Huffman JC. Meta-analysis of selective serotonin reuptake inhibitor-associated QTc prolongation. J Clin Psychiatry. 2014;75(5):e441–449.
Preda A, Shapiro BB. A safety evaluation of aripiprazole in the treatment of schizophrenia. Exp Opin Drug Saf. 2020;19(12):1529–38.
Czekalla J, Beasley CM Jr, Dellva MA, Berg PH, Grundy S. Analysis of the QTc interval during olanzapine treatment of patients with schizophrenia and related psychosis. J Clin Psychiatry. 2001;62(3):191–8.
Sousa PA, Pereira S, Candeias R, de Jesus I. The value of electrocardiography for differential diagnosis in wide QRS complex tachycardia. Revista portuguesa de cardiologia: orgao oficial da Sociedade Portuguesa de Cardiologia = Portuguese journal of cardiology : an official journal of the Portuguese Society of Cardiology. 2014;33(3):165–73.
Rao ACA, Ng ACC, Sy RW, Chia KKM, Hansen PS, Chiha J, Kilian J, Kanagaratnam LB. Electrocardiographic QRS duration is influenced by body mass index and sex. Int J Cardiol Heart vasculature. 2021;37:100884.
Türe M, Akin A, Unal E, Kan A, Balik H, Feryal Taş F, Haspolat YK. The association between electrocardiographic data and obesity in children and adolescents. Minerva Pediatr 2021.
Acknowledgements
Not applicable.
Funding
This study was supported by the project of Foshan Science and Technology Bureau (2220001004473, 2220001004736, 2220001004879) and the Foshan “14th five-year plan” medical high level key psychiatric specialty construction project (FSGSP145069).
Author information
Authors and Affiliations
Contributions
Jiaquan Liang, Yan Li, Chaohua Tang, and Guojun Xie have made great contributions to the conception, design and writing of the works; Weibo Wu, Zhijian Li, Xuesong Li, Wei Huang and Wensheng Chen have provided assistances in the acquisition, analysis or interpretation of the data. Xiancong Mai, Xiaoling Li and Caixia Xu made contributions to the recording of experimental data and the measurement of blood lipids and electrocardiograms.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
We obtained written informed consent from patients or their legal guardians. This study was approved by the ethics committee of the Third People’s Hospital of Foshan, China and the experiments were conducted following the declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors have no potential or actual conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Li, Y., Tang, C., Wu, W. et al. Abnormal blood lipid and electrocardiogram characteristics in common mental disorders. BMC Psychiatry 23, 465 (2023). https://doi.org/10.1186/s12888-023-04965-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12888-023-04965-9