Abstract
Background
The Lothian Birth Cohort 1936 (LBC1936) is a longitudinal study of ageing with well-characterised assessments, but until now, it has relied on self-report or proxies for dementia such as cognitive tests. Our aims were twofold:
a) to describe a framework for identifying dementia in a cohort study.
b) to report the age-specific incidence and prevalence of all-cause dementia and dementia subtypes in 865 individuals in the LBC1936.
Methods
Electronic Health Records (EHR) of all participants were reviewed, and relevant information was extracted to form case vignettes for everyone with any record of cognitive dysfunction. The EHR data sources include hospital and clinic letters, general practitioner and hospital referrals, prescribed medications, imaging and laboratory results. Death certificate data were obtained separately. Clinician assessments were performed when there was concern about a participant's cognition. A diagnosis of probable dementia, possible dementia, or no dementia was agreed upon by a consensus diagnostic review board, comprised of a multidisciplinary team of clinical dementia experts who reviewed case vignettes and clinician assessment letters. For those with probable dementia, a subtype was also determined, where possible. We compared the agreement between our newly ascertained dementia diagnoses with the existing self-reported dementia diagnoses.
Results
Self-reported dementia diagnoses were positive in only 17.8% of ascertained dementia diagnoses. The EHR review identified 163/865 (18.8%) individuals as having cognitive dysfunction. At the consensus diagnostic review board, 118/163 were diagnosed with probable all-cause dementia, a prevalence of 13.6%. Age-specific dementia prevalence increased with age from 0.8% (65–74.9 years) to 9.93% (85–89.9 years). Prevalence rates for women were higher in nearly all age groups. The most common subtype was dementia due to Alzheimer disease (49.2%), followed by mixed Alzheimer and cerebrovascular disease (17.0%), dementia of unknown or unspecified cause (16.1%), and dementia due to vascular disease (8.5%).
Conclusions
We present a robust systematic framework and guide for other cohort teams wanting to ascertain dementia diagnoses. The newly ascertained dementia diagnosis provides vital data for further analyses of LBC1936 to allow exploration of lifecourse predictors of dementia.
Similar content being viewed by others
Introduction
Dementia is a major and growing global public health challenge [1]. Dementia research is crucial for informing present and future demand for dementia care services [2]. As the number of people with dementia increases globally, obtaining accurate dementia prevalence rates based on valid and robust dementia ascertainment is crucial to guide health system planning and to inform research decisions. Epidemiological studies require robust dementia diagnoses, ideally in well-characterised longitudinal cohorts, to allow the identification of lifecourse predictors of dementia, and to produce meaningful results to inform policy and clinical practice.
Using multiple and varied data sources when ascertaining dementia diagnoses is vital [3, 4]. Our dementia ascertainment method using a combination of existing data sources builds upon a previously validated approach that compared diagnoses extracted from existing data with diagnoses made on clinical review in an earlier LBC cohort (LBC1921) [3]. That study found that overall dementia diagnoses using data from multiple existing sources were confirmed by clinical review in 88% of cases [3]. A recent UK Biobank study found that using hospital admissions data alone unearthed 78% of dementia diagnoses, and general practitioner data alone captured only 52% of dementia diagnoses [5]. Ultimately, many dementias in the community remain undiagnosed as individuals affected do not attend health or social care services [6]. This makes it important that cohort studies have a system, like ours, of flagging individuals who merit clinical assessment for cognitive impairment, whether from concerns raised at the follow-up research waves, declining performance in cognitive tests, or some other warning sign.
The aims of this study are twofold:
-
a)
To outline a framework for robust, clinically-derived dementia ascertainment in an important longitudinal cohort study, the Lothian Birth Cohort 1936 (LBC1936).
-
b)
To describe prevalence and incidence rates of all-cause dementia and subtypes of 865 individuals in LBC1936 as they aged from 70 years to approximately 86 years old.
Methods
Participants
This study used data from the LBC1936 (https://www.ed.ac.uk/lothian-birth-cohorts), described in detail elsewhere [7,8,9]. In summary, participants living in the Lothian region of Scotland (which includes Edinburgh), most of whom had completed an intelligence test aged 11 years, were recruited in 2004, at mean age 69.5 years (n = 1091). At initial recruitment, none reported a diagnosis of dementia, this was a specific inclusion criterion of the LBC1936. They have been followed up every three years since, at mean ages 72.5 years (n = 866), 76.3 years (n = 697), 79.3 years (n = 550) and 82 years (n = 431). The sixth wave of data collection is complete, and a seventh is planned. LBC1936 participants were first asked for their consent to access medical records from wave 2 onwards, so participants who only attended wave 1 were excluded from our study. We also excluded one other participant who did not consent to data linkage to their medical records from wave 2 onwards.
All LBC1936 participants are white, and the sex split is approximately equal. At each wave, participants undergo a core battery of cognitive testing, including measures of reasoning, processing speed, executive function, and memory. In addition, a detailed medical history, blood tests, physical measures, and structural magnetic resonance imaging (MRI; age 72.5 onwards) are collected at each wave. The neuropsychological battery performed as part of LBC1936 testing includes the Mini-Mental State Exam (MMSE), logical memory 1 & 2, verbal fluency, National Adult Reading Test, Weschler Test of Adult Reading, Test of Premorbid Functioning, digit symbol coding, backward digit span, simple and four-choice reaction time, block design, verbal paired associates, spatial span, symbol search, matrix reasoning, verbal paired associates delay, and inspection time [8]. Symptoms of depression and anxiety are measured using the Hospital Anxiety and Depression Screen.
Dementia ascertainment process
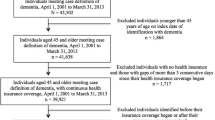
Our diagnostic procedure followed a previously validated process [3] with the additional step of a clinical assessment at home, where indicated, on a selection of our cohort. As illustrated in Fig. 1, there were three phases: (i) Electronic Health Record (EHR) review plus death certificate data, (ii) home visit clinician assessments, and (iii) consensus review board meeting.
Overview of the dementia diagnostic process. Note: EHR, Electronic Health Record. *only a small subsample of participants had information available at the consensus review meeting following a home visit assessment. Doctor home visits were requested for several reasons, explained in the section ‘Home visits’
Phase 1: Electronic Health Record (EHR) review
A team of psychiatrists specialising in Old Age Psychiatry (“EHR team”) reviewed the EHR of every consenting LBC1936 participant, including any information on their EHR dating before wave 2 collection. All information was accessed and stored within the secure National Health Service computer system. An EHR protocol was produced by the group to ensure a standardised and systematic approach for each participant (Additional file 1).
The EHR for each participant was located using the patient’s Community Health Index (CHI) number, a unique health identifier used in NHS Scotland. Since 2014, all healthcare records within NHS Lothian (the health board covering Edinburgh and surrounding areas) including psychiatric records have been stored on the EHR as full-text letters, records of referrals from primary to secondary/tertiary care services, hospital discharge letters including medications, and results of laboratory and radiological investigations. Before 2014, general and psychiatric records were held on separate systems, but all records were subsequently incorporated into the TrakCare system. Death certificate data is available for all deceased LBC1936 participants via record linkage. This was checked for each participant at the diagnostic review board (see Phase 3, below).
Case vignettes
The psychiatrist who reviewed the EHR created anonymised extracts of relevant information for the diagnostic review board meeting for any participant with evidence of cognitive dysfunction or a diagnosis of dementia. This work was completed on 17th April 2022.
Participants with upcoming NHS services investigations or assessments, such as brain imaging or memory clinic assessments, were flagged in the case vignettes to make the diagnostic review board aware. The EHRs of these flagged case vignettes were checked for updated information at the diagnostic review board.
Phase 2: Home visits
Doctor home visits were requested for several reasons: when cognitive impairment or decline was noted by LBC research staff during routine LBC1936 wave 6 testing (in comparison to test scores in prior waves); when a new diagnosis of dementia was self-reported to the LBC research team; or when the LBC researcher had concerns that the participant might have dementia. Wave 6 testing was ongoing at the time of our study. Before participating in Wave 6 of the study, LBC1936 participants were informed that they would be invited to have a home visit if there was a substantial decline in their cognitive scores or if they had already been diagnosed with dementia; participants provided written consent when attending their Wave 6 cognitive testing appointment.
During the home visit, an experienced Old Age psychiatrist performed a detailed clinical assessment. This included a thorough interview with the participant and, where available, an informant, to gather a complete medical history. Cognitive testing was completed using the Addenbrooke’s Cognitive Examination-III [10] and a physical examination, allowing the completion of the Modified Hachinski Ischaemic Scale [11]. The clinician also reviewed the participant’s medical records including investigations (laboratory results, brain imaging), clinic letters, and prescribed medications. They then wrote to the participant’s general practitioner detailing the outcome of the assessment and, if necessary, referred them for further assessment within the NHS. These letters were available for review by the consensus diagnostic review board and were considered alongside the case vignettes.
Phase 3: consensus diagnostic review board
The consensus group consisted of experienced dementia experts from Old Age Psychiatry (AS, CG, DM, LS, TR), Geriatric Medicine (SS), and Neurology (TW). We agreed on whether the available evidence for each participant supported a diagnosis of one of probable dementia, possible dementia, or no dementia, and determined the subtype of dementia, where possible. Depending on the strength of the evidence, both the diagnosis and subtype were deemed either ‘probable’ or ‘possible’. The criteria used for probable and possible diagnoses are shown in Table 1 (derived from a validated process [3]). Any disagreement was resolved through discussion. Any individual identified as having dementia but where there was insufficient evidence to make a subtype diagnosis was classified as an ‘unclear’ subtype. Differential diagnoses were made according to the ICD-11 criteria [12]. The final date for this phase was 18th August 2022.
The earliest date of any diagnosis was recorded. When only the month was available, we selected the middle of the month. Where only the year was available, 2nd July was selected as the estimated middle of the year.
The EHR of participants flagged as having impending memory assessments or investigations, as described in Phase 1, were revisited at the consensus meeting, and any new information was considered. The consensus group were blinded to each participant’s self-report of dementia status to reduce the risk of bias in the assessment.
To minimise the risk of misclassification, any inconsistencies between data sources were considered on a case-by-case basis. If there was reliable and consistent evidence for dementia in one source (e.g., Psychiatry clinic letter), but not another (e.g., death certificate), it was assumed the participant had dementia. Where there was contradictory evidence of similar reliability from two sources, further evidence was sought from other sources, and a consensus was reached. If it was impossible to obtain further evidence, participants with contradictory evidence were classified as possible rather than probable dementia. We arranged NHS clinical follow-ups and post-diagnostic support for participants newly diagnosed with dementia in our study.
Person-hours calculation
We calculated the approximate number of person-hours required for each ascertainment phase, which can be a guide to researchers considering replicating our methods in other cohorts. Approximately 469 person-hours were required to ascertain dementia in this cohort (Additional file 2), the majority required for phase 1 (400 h).
Analysis
We compared the self-reported dementia diagnoses at each study wave to the cumulative ascertained dementia diagnoses. We recorded which sources contributed information for each ascertained probable dementia diagnosis. The information sources were categorised as EHR, clinical assessments at home, death certificates, and brain imaging. We noted if dementia was recorded on any part of the death certificate. For those participants who underwent more than one brain imaging modality, we noted the most detailed modality (e.g., MRI if the participant had had both CT and MRI brain scans). We considered brain imaging results from both NHS clinical settings and LBC1936 scans. We ensured clinical follow-up and post-diagnostic support for those where dementia was newly identified. Statistical analysis was performed using R version 4.0.2 [13]. Code is openly available on GitHub [14].
We calculated the prevalence of all-cause probable dementia, i.e., the proportion of the study sample that, at some point in their life or between the ages of approximately 70 and 86 years (if they are still alive), developed dementia. We formally quantified the trend for prevalence to i) increase linearly and ii) accelerate with age by performing a linear regression in which cumulative dementia cases were predicted by time in days as a linear and quadratic term (cumulative dementia ~ days + days2). We compared the basic characteristics of the participants with and without probable dementia. We calculated the age-stratified dementia prevalence by removing those with dementia from the numerator when they died and removing all those who died from the denominator. We calculated the age-stratified dementia incidence rate. We report five-year age groupings, but we pooled the two groups 65 to 69.9 years and 70 to 74.9 years to preserve anonymity due to sample distribution. We performed significance testing using a chi-squared test comparing the rate in men and women. Finally, we calculated the proportions of the probable dementia subtypes. For clarity, and as the number of people with possible dementia was small (N = 7), we focused on probable dementia when calculating prevalence and incidence rates – those with possible dementia were included in the ‘no dementia’ group for analysis.
Results
Participants
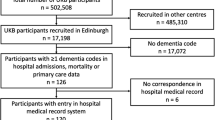
Wave 2 of the LBC1936 had 866 participants. One participant did not consent to their data being linked to their medical records. Accordingly, we included 865 participants in our analysis. Of these, 163 participants (18.8%) were flagged as having cognitive dysfunction following the EHR review and/or home visit. The anonymised case vignettes derived from the EHR, along with home visit clinical assessment letters for 10 participants, formed the basis of the discussion at the consensus group meeting. We illustrate the flow of participants, the data sources contributing to dementia diagnoses, and the consensus diagnostic review board outcomes in Fig. 2.
Dementia prevalence
In this cohort of older adults who were free from dementia at study inception, we found that 13.6% (118/865) of participants met the criteria for a diagnosis of probable all-cause dementia between the ages of approximately 70 and 86 years old. Participants’ demographics and IQ scores at age 11 are presented in Table 2.
In addition to the 118 people with probable dementia, seven participants were diagnosed with possible dementia. Of these seven, six were deceased making further testing impossible. To help preserve anonymity, their demographics are not included in Table 2.
Age-stratified dementia prevalence
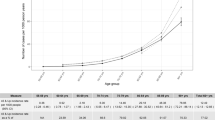
The prevalence of dementia for the age group 65 to 74.9 years was 0.8% rising to 9.47% for the age group 80–84.9 years. There was only a slight increase to 9.93% in the 85–89.9 years age group as the mean age of dementia diagnosis in this group was only 85.49 years. We pooled the two groups 65 to 69.9 years and 70 to 74.9 years to preserve anonymity due to sample distribution. The prevalence rates for women were higher in nearly all age groups. At the time of the consensus meeting, 321 of 865 participants had died; 64 of these had dementia. Thus, 54 participants with dementia were alive at the time of our study. They had a mean (SD) age of 86 (0.8) years, and the sex divide was approximately even. As individuals with dementia died, they were removed from our prevalence calculation for later age groups. Table 3 presents the age-stratified dementia prevalence in our study, both pooled and grouped by sex. When modelling prevalence as a continuous trend, regression indicated there was a significant increase in dementia prevalence over time (p < 0.001); a significant quadratic term indicated that there was also significant acceleration in the prevalence rate (p < 0.001).
Age-stratified dementia incidence
Table 4 presents the incident dementia diagnoses over five years, distributed across age and sex categories.
Dementia subtypes
The distribution of the 118 probable dementia diagnoses by subtype was as follows: dementia due to Alzheimer disease (49.2%), mixed Alzheimer and cerebrovascular disease (17.0%), vascular disease (8.5%), Lewy body disease (3.4%), dementia due to psychoactive substances (1.7%), diseases classified elsewhere (e.g., Creutzfeldt-Jakob Disease, Parkinson’s; 4.2%), and dementia of unknown or unspecified cause (16.1%). Table 5 presents the subtype diagnoses in detail. Figure 3 illustrates the main subtype groupings.
Distribution of main dementia subtype groups. Note: “Other dementias” contains those due to Lewy Body Disease, psychoactive substances, and diseases classified elsewhere (precise proportions are presented in Table 5)
Comparing self-reported and ascertained dementia diagnoses
Figure 4 illustrates the large difference between the number of self-reported and ascertained dementia diagnoses. Of the 118 ascertained dementia diagnoses, only 21 had ever self-reported dementia. One participant who self-reported dementia did not have dementia ascertained. The self-reported dementia diagnosis in LBC1936, therefore, has a sensitivity of 17.8% and a specificity of 98.9%, when assigning the ascertained dementia diagnoses as the gold standard.
Comparison of the cumulative number of self-reported dementias with the ascertained dementia diagnoses over the timespan of the LBC1936. Note: due to attrition, the number tested (i.e., asked about their dementia status) reduces at each wave, whereas access to electronic health records is not affected by attrition
Data sources contributing to probable dementia diagnoses
Of the 118 probable dementia diagnoses, 43 had an MRI brain scan (37%), 53 had a CT brain scan (45%), and three (2.5%) had another scan such as single-photon emission computerised tomography (SPECT) scan, Dopamine Transporter (DaT) Scan, or Positron emission tomography (PET). Nineteen (16%) of those with a dementia diagnosis did not have any brain imaging. As stated in the methods, we recorded only the most detailed scan a participant received, as this was given precedence during the consensus group meeting. Of the 64 participants with dementia who died, a diagnosis of dementia was recorded on the death certificate of 47 (73.4%). Information from home visits contributed to 10/118 dementia diagnoses. This information is illustrated in Fig. 2.
Discussion
We have ascertained dementia diagnoses in the LBC1936 using a robust systematic approach that closely aligns with diagnosing dementia in practice. Our methods go far beyond those used by many research studies, which lack the detailed medical data required to ascertain dementia in such a robust clinical manner. Previously, the best method available for determining dementia in the LBC1936 dataset was self-reported dementia status. Over the course of the LBC1936 study, this self-reported measure has been used as an exclusion criterion, the basis of sensitivity analyses or a covariate to control for the potential that those results are not heavily driven by an apparently small number of clinical cases. Our results indicate that the prevalence within the LBC1936 was a substantial underestimate leading to the inclusion of those with dementia who had previously been treated as non-demented. Whereas prior work suggested that the results of some types of analyses may not have been unduly biased by unrecognised dementia [4], optimal characterisation of the sample under study is critical in refining our understanding of the nature and mechanisms of cognitive ageing across a spectrum of severities and may vary as a function of the exposures being studied.. Given the pre-clinical phase of dementia, though variable between persons, is likely to precede a clinical diagnosis by many years, it is likely that some participants at recruitment (none of whom had a diagnosis of dementia) were in the preclinical phase. This is substantiated by the relatively short time for a small number of participants between recruitment and dementia – our ascertainment protocol thus further highlights the value of having identified individuals who might otherwise have been considered ‘healthy agers’.
We have illustrated in our comparison of self-reported and ascertained dementia diagnoses that most participants with dementia dropped out or did not communicate their dementia diagnosis to LBC1936 researchers during follow-up wave testing. Previous LBC1936 analysis has found that those more likely to drop out were at higher risk of dementia and ill-health [7]. This includes those who dropped out after wave 1, who were all excluded from our study as they had not been asked to consent to medical data linkage. Therefore, our prevalence and incidence rates are likely to be conservative. Nevertheless, the addition of this new dementia diagnosis using medical data linkage adds great value to the LBC1936 dataset.
In total, 118/865 (13.6%) participants met the criteria for a diagnosis of probable dementia between the ages of 69 and 85.5 years. The prevalence of dementia increased with age, and women had higher rates in nearly all age groups. The most common subtype was dementia due to Alzheimer disease (49.2%), followed by mixed Alzheimer and cerebrovascular disease (17.0%), dementia of unknown or unspecified cause (16.1%), and dementia due to vascular disease (8.5%).
Comparison to literature
Our study’s all-cause dementia prevalence rates are comparable with other similar studies (community-based, similar demographics). For example, the prevalence rate for 75–79.9-year-olds in LBC1936 is 4.5% compared to the Framingham (3.6%) [15] and the Cognitive Function and Ageing Studies (CFAS) II (5.2% [males] and 6.2% [females]) [2], the male-only Caerphilly Prospective Study (3.9%) [16] from Wales, a cohort from Sweden (5.7%) [17], and a meta-analysis (5.6%) [18]. It is worth highlighting, though, that participants in LBC1936 were all white and a recent study comparing the incidence of dementia among ethnic groups in the UK found that black people had a higher incidence of dementia (25—28% higher) and Asian people had a lower incidence (12—18% lower), when compared with white people [19]. As such, our framework and estimates of the discrepancy between self-report and ascertained prevalence may not apply to samples with more diverse ancestries. Additional file 3 presents the age-specific all-cause dementia prevalence rates across similar community cohorts from neighbouring countries.
Our finding of increasing prevalence with age and higher prevalence in women is common in most dementia prevalence studies [2, 20,21,22]. While the dementia rates in LBC1936 in the younger age groups (65–74.9 years) are low, the absolute numbers of dementia diagnoses are small, so these prevalence rates should be interpreted cautiously. Similarly, we advise caution when interpreting the prevalence rate of our 85–89.9 years age group. At the time of our study, the mean age of participants with dementia in the 85–89.9 years group is only 85.49 years old. Previous meta-analyses found that dementia rates double every five years [18, 20, 23], so it is reasonable to expect a large increase in dementia prevalence as the participants in the 85–89.9 years age group move towards the older end of the group over the next four to five years. Repeating this dementia ascertainment work in four of five years (with August 2022 as the start date, thus substantially reducing the workload) for the participants who have, until now, survived dementia-free, will likely yield many new dementia diagnoses. It is not only invaluable for research purposes but also aids understanding of the changing needs of participants for forthcoming LBC1936 study appointments, some of whom are keen to still attend with dementia. The higher prevalence in women makes it critical that large prospective clinical trials with dementia as the primary outcome include women and men in numbers adequate for the assessment of sex effects.
Exploring variation
There are many difficulties with comparing prevalence rates in different studies using different methodological approaches. The diagnostic criteria for dementia and dementia subtypes have evolved since dementia population cohorts proliferated in the 1980s, making it especially difficult to compare estimates before this with newer ones [24]. Other methodological differences between studies also influence prevalence estimates. For example, in the Framingham study, only those scoring below set cut-off scores on the MMSE were called back for further evaluation, thus increasing the likelihood that they will have dementia [15].
The slightly lower prevalence rates in our study may be partly explained by a trend towards reduced rates in later-born cohorts. In two landmark studies in cognitive ageing from England, CFAS I and II, there was a marked reduction in dementia prevalence rates over the 20 years between data collection instances [2]. Later-born populations had a lower risk of prevalent dementia than those born earlier in the twentieth century. This finding was replicated in a representative panel study, the English Longitudinal Study of Ageing (ELSA), which found a decrease in age-specific prevalence [21]. Despite this, the ELSA study reported that the number of people with dementia in England and Wales is projected to increase by 57% from 2016 to 2040, mainly due to improved life expectancy [21].
Geography and socioeconomic status may also partly explain our slightly lower prevalence rates. The LBC1936 is a relatively healthy self-selecting cohort from a more affluent area than most in Scotland; their early life cognitive ability was higher, on average, than the general population [8], and it may be that dementia rates are lower in Lothian than in other areas of the country [7, 8]. The CFAS I and II studies detailed important analyses of the effect of geography on dementia incidence and prevalence and found that prevalence varies according to deprivation indices in English localities [2].
Using multiple and varied data sources
The proportion of Alzheimer disease among dementia diagnoses in our study (49.2%) is comparable to the Framingham (55.6%) [15] and Kungsholmen (53.7%) [17] studies.
Brain imaging results were available for 84% of the participants diagnosed with dementia. This was particularly important to subtyping vascular dementia, when brain imaging is especially helpful [12]. Dementia was noted on the death certificates of 73.4% of those with dementia who had died. This is similar to a previous Scottish study that found dementia was noted on the death certificates of 71.5% of patients who died with dementia [25].
Strengths and limitations
A major strength of this study is the limited attrition bias as we reviewed the EHR of all participants from wave 2 till the present (or their death). This is important, especially with an outcome like dementia, as participants with poorer cognitive ability are at a greater risk of loss to follow-up [26]. Several specialists were involved in reviewing the EHR and performing the home visits, and inter-rater variability was limited by having a clear protocol and a multidisciplinary consensus meeting including at least two people who had completed the EHR reviews. Our thorough EHR reviews combined with our system for flagging for home visit any participant presenting at wave 6 testing with evidence of cognitive dysfunction makes it very likely we captured anyone with concerns raised to the health service, or at LBC testing.
A limitation of the study was the inability to accurately provide subtypes for all those (n = 118) who were diagnosed with dementia. This was mostly due to inadequate information recorded in the EHR for people who subsequently died (i.e., could not be assessed further by the study team). This reflects clinical practice in Scotland in the early 2000s, where subtypes were not always routinely recorded. Of note, no participants were diagnosed with frontotemporal dementia (FTD), whereas in recent dementia cohorts, FTD diagnoses have accounted for 1.6% to 6% of dementia diagnoses [27, 28]. However, these cohorts tended to include relatively younger adults (mean age 64 years [28]). A further limitation is that the home visits were only for a small selection of our cohort based on a specific set of criteria (outlined in methods section) applied to those who attended the latest follow-up wave.
Implications
Our multidisciplinary approach to ascertaining dementia using multiple varied sources can serve as a framework and guide for other cohort teams wanting to ascertain dementia diagnoses. The estimated person-hours calculation (Additional file 2) will inform those involved in resourcing such future undertakings. This newly ascertained clinically robust dementia diagnosis will be invaluable for future research identifying risk factors and associations with dementia in this well-characterised cohort, and should be used instead of the self-report dementia diagnoses. The LBC1936 has five waves (sixth is underway, seventh is planned) of consistently measured cognitive, brain imaging, biomedical, psychosocial, and lifestyle data covering the ages of 70 – 86 years. It has, uniquely, a measure of intelligence at age 11. The latest data types in LBC1936 include: whole-genome sequencing, longitudinal DNA methylation, longitudinal gene expression, lipidomics, post-mortem brain tissue, induced pluripotent stem cells, inflammatory markers, oxidative stress markers, life course geographical information, objectively measured physical activity and sedentary behaviour [7]. This ensures a vast range of possibilities for future dementia research.
Conclusion
These dementia diagnoses for the well-characterised LBC1936 can be a foundation for future studies to confirm existing, and assess novel risk factors for dementia, and contribute to the rational basis for the development of new interventions to reduce incident dementia.
Availability of data and materials
All data are available on reasonable request here: https://www.ed.ac.uk/lothian-birth-cohorts/data-access-collaboration
Abbreviations
- CFAS:
-
Cognitive Function and Ageing Studies
- CI:
-
Confidence Interval
- CT:
-
Computerised Tomography
- DSM-5:
-
Diagnostic and Statistical Manual of Mental Disorders—Fifth Edition
- DaT:
-
Dopamine Transporter
- EHR:
-
Electronic Health Records
- ELSA:
-
English Longitudinal Study of Ageing
- FTD:
-
Frontotemporal Dementia
- ICD-11:
-
International Classification of Diseases-11
- LBC1936:
-
Lothian Birth Cohort 1936
- MRI:
-
Magnetic Resonance Imaging
- MMSE:
-
Mini-Mental State Exam
- NHS:
-
National Health Service
- SPECT:
-
Single-Photon Emission Computerised Tomography
- SD:
-
Standard Deviation
References
Nichols E, Steinmetz JD, Vollset SE, et al. Estimation of the global prevalence of dementia in 2019 and forecasted prevalence in 2050: an analysis for the Global Burden of Disease Study 2019. Lancet Public Heal. 2022;7:e105–25.
Matthews FE, Arthur A, Barnes LE, et al. A two-decade comparison of prevalence of dementia in individuals aged 65 years and older from three geographical areas of England: results of the Cognitive Function and Ageing Study I and II. Lancet (London, England). 2013;382:1405.
Sibbett RA, Russ TC, Deary IJ, et al. Risk factors for dementia in the ninth decade of life and beyond: A study of the Lothian birth cohort 1921. BMC Psychiatry; 17. Epub ahead of print 2 June 2017. https://doi.org/10.1186/s12888-017-1366-3.
Sibbett RA, Russ TC, Deary IJ, et al. Dementia ascertainment using existing data in UK longitudinal and cohort studies: a systematic review of methodology. BMC Psychiatry; 17. Epub ahead of print 3 July 2017. https://doi.org/10.1186/S12888-017-1401-4.
Wilkinson T, Schnier C, Bush K, et al. Identifying dementia outcomes in UK Biobank: a validation study of primary care, hospital admissions and mortality data. Eur J Epidemiol. 2019;34:557–65.
Aldus CF, Arthur A, Dennington-Price A, et al. Undiagnosed dementia in primary care: a record linkage study. Heal Serv Deliv Res. 2020;8:1–108.
Taylor AM, Pattie A, Deary IJ. Cohort profile update: the lothian birth cohorts of 1921 and 1936. Int J Epidemiol. 2018;47:1042–1042r.
Deary IJ, Gow AJ, Taylor MD, et al. The Lothian Birth Cohort 1936: A study to examine influences on cognitive ageing from age 11 to age 70 and beyond. BMC Geriatr. 2007;7:1–12.
Deary IJ, Gow AJ, Pattie A, et al. Cohort profile: The lothian birth cohorts of 1921 and 1936. Int J Epidemiol. 2012;41:1576–84.
Hsieh S, Schubert S, Hoon C, et al. Validation of the addenbrooke’s cognitive examination iii in frontotemporal Dementia and Alzheimer’s Disease. Dement Geriatr Cogn Disord. 2013;36:242–50.
Hachinski VC, Iliff LD, Zilhka E, et al. Cerebral blood flow in dementia. Arch Neurol. 1975;32:632–7.
World Health Organization. International Statistical Classification of Diseases Eleventh Revision (ICD-11). 11th ed. Geneva: WHO, https://icd.who.int/en (2022).
R Core Development Team. A Language and Environment for Statistical Computing. R Foundation for Statistical Computing 2020; 2: https://www.R-project.org.
Mullin D. Dementia prevalences in LBC1936 code. Epub ahead of print 2022. https://doi.org/10.5281/zenodo.7327567.
Bachman DL, Wolf PA, Linn R, et al. Prevalence of dementia and probable senile dementia of the Alzheimer type in the Framingham Study. Neurology. 1992;42:115–9.
Fish M, Bayer AJ, Gallacher JEJ, et al. Prevalence and pattern of cognitive impairment in a community cohort of men in south wales: methodology and findings from the caerphilly prospective study. Neuroepidemiology. 2008;30:25–33.
Fratiglioni L, Grut M, Forsell Y, et al. Prevalence of Alzheimer’s disease and other dementias in an elderly urban population. Neurology. 1991;41:1886–1886.
Jorm AF, Korten AE, Henderson AS. The prevalence of dementia: a quantitative integration of the literature. Acta Psychiatr Scand. 1987;76:465–79.
Pham TM, Petersen I, Walters K, et al. Trends in dementia diagnosis rates in UK ethnic groups: analysis of UK primary care data. Clin Epidemiol. 2018;10:949.
Wu Y-T, Beiser AS, Breteler MMB, et al. The changing prevalence and incidence of dementia over time — current evidence. Nat Publ Gr. Epub ahead of print 2017. https://doi.org/10.1038/nrneurol.2017.63.
Ahmadi-Abhari S, Guzman-Castillo M, Bandosz P, et al. Temporal trend in dementia incidence since 2002 and projections for prevalence in England and Wales to 2040: Modelling study. BMJ; 358. Epub ahead of print 2017. https://doi.org/10.1136/bmj.j2856.
Fiest KM, Jetté N, Roberts JI, et al. The prevalence and incidence of dementia: a systematic review and meta-analysis. Can J Neurol Sci. 2016;43:S3–50.
Cao Q, Tan CC, Xu W, et al. The prevalence of dementia: a systematic review and meta-analysis. J Alzheimers Dis. 2020;73:1157–66.
George DR, Whitehouse PJ, Ballenger J. The evolving classification of dementia: placing the DSM-V in a meaningful historical and cultural context and pondering the future of ‘Alzheimer’s.’ Cult Med Psychiatry. 2011;35:417–35.
Russ TC, Batty GD, Starr JM. Cognitive and behavioural predictors of survival in Alzheimer disease: results from a sample of treated patients in a tertiary-referral memory clinic. Int J Geriatr Psychiatry. 2012;27:844–53.
Matthews FE, Chatfield M, Freeman C, et al. Attrition and bias in the MRC cognitive function and ageing study: An epidemiological investigation. BMC Public Health. 2004;4:1–27.
Religa D, Fereshtehnejad SM, Cermakova P, et al. SveDem, the Swedish Dementia Registry - A tool for improving the quality of diagnostics, treatment and care of dementia patients in clinical practice. PLoS One; 10. Epub ahead of print 19 February 2015. https://doi.org/10.1371/JOURNAL.PONE.0116538.
Van Der Flier WM, Scheltens P. Amsterdam dementia cohort: performing research to optimize care. J Alzheimer’s Dis. 2018;62:1091–111.
Acknowledgements
The authors are very grateful to the LBC1936 participants past and present, and the LBC research team who recruited participants, obtained data linkage permissions and collected data. Their commitment and contributions have made this work and many other important studies possible. Dr Mullin is very grateful for the support of his funders, supervisors, and academic mentors. For the purpose of open access, the authors have applied a CC-BY public copyright licence to any Author Accepted Manuscript version arising from this submission.
Funding
The present manuscript received no direct funding. DSM is undertaking a PhD Clinical Fellowship funded by the Masonic Charitable Foundation and the Royal College of Psychiatrists, United Kingdom. TCR is a member of the Alzheimer Scotland Dementia Research Centre, funded by Alzheimer Scotland. SRC is supported by a Sir Henry Dale Fellowship jointly funded by Wellcome and the Royal Society (221890/Z/20/Z) and receives grant support as core LBC funding from Age UK (The Disconnected Mind), UK’s Biotechnology and Biological Sciences Research Council (BBSRC) and the Economic and Social Research Council (BB/W008793/1), and the University of Edinburgh. He also receives funding from the NIH (1RF1AG073593; R01AG054628), MRC (MR/X003434/1) and ESRC (ES/T003669/1). ID receives funding from the UK’s Biotechnology and Biological Sciences Research Council (BBSRC) and the Economic and Social Research Council (BB/W008793/1), and NIH (1RF1AG073593; R01AG054628). The Lothian Birth Cohort 1936 study acknowledges the financial support of NHS Research Scotland (NRS) through the Edinburgh Clinical Research Facility. All researchers are independent of their funders.
Author information
Authors and Affiliations
Contributions
DSM and TCR generated the ideas behind the present manuscript. SRC, DP, and AT contributed to protocol design and collected and supplied non-ascertainment data. ID designed the cognitive test battery and other aspects of the assessment in the LBC1936. DSM analysed the data, drafted the manuscript, and is the guarantor. CG, ER, AS, CC, HG, and GW formed the Electronic Health Records review team. HG, EB, ER, DP, AT, and DSM formed the Home Visits team. DSM, LES, CG, AS, HG, ER, TCR, TW, and SS formed the Diagnostic Review Board team. All authors edited the manuscript and gave final approval of the version to be published. The corresponding author attests that all listed authors meet authorship criteria and that there has been no omission of others meeting the criteria.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Ethics permission for the Lothian Birth Cohort 1936 protocol was obtained from the Multi-Centre Research Ethics Committee for Scotland (Wave 1: MREC/01/0/56), the Lothian Research Ethics Committee (Wave 1: LREC/2003/2/29), and the Scotland A Research Ethics Committee (Waves 2–6: 07/MRE00/58). The research was carried out in compliance with the Helsinki Declaration. Written informed consent was obtained from all participants when data linkage permissions were sought (Wave 2). Where participants reported a diagnosis of dementia, informed consent was obtained from a welfare guardian or nearest relative (N = 2).
Consent for publication
Written informed consent for publication was obtained from all participants.
Conflicts of interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Dementia ascertainment protocol - Lothian Birth Cohort 1936 Study.
Additional file 2.
Approximate number of person-hours required for each ascertainment phase.
Additional file 3.
Comparable prevalence rates for all-cause dementia.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Mullin, D.S., Stirland, L.E., Buchanan, E. et al. Identifying dementia using medical data linkage in a longitudinal cohort study: Lothian Birth Cohort 1936. BMC Psychiatry 23, 303 (2023). https://doi.org/10.1186/s12888-023-04797-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12888-023-04797-7