Abstract
Background
Posttraumatic Stress Disorder (PTSD) could potentially increase the risk of mortality, and there is a need for a meta-analysis to quantify this association. This study aims to determine the extent to which PTSD is a predictor of mortality.
Methods
EMBASE, MEDLINE, and PsycINFO were searched systematically on 12th February 2020, with updated searches conducted in July 2021, and December 2022 (PROSPERO CRD42019142971). Studies involving community-dwelling participants with a diagnosis of PTSD or PTSD symptoms, and a comparator group of individuals without PTSD, and which assessed mortality risk, were included. A random-effects meta-analysis was conducted on studies reporting Odds Ratio (OR), Hazard Ratio (HR), and Risk Ratio (RR), and subgroup analysis was also performed by age, sex, type of trauma experienced, PTSD diagnosis, and cause of death.
Results
A total of 30 eligible studies of mostly good methodological quality were identified, with a total of more than 2.1 million participants with PTSD. The majority of studies involved male-dominated, veteran populations. PTSD was associated with a 47% (95% CI: 1.06–2.04) greater risk of mortality across six studies that reported OR/RR, and a 32% increased risk across 18 studies which reported time to death (HR: 1.32, 95% CI: 1.10–1.59). There was very high study heterogeneity (I2 > 94%) and this was not explained by the prespecified subgroup analysis.
Conclusion
PTSD is associated with increased mortality risk, however further research is required amongst civilians, involving women, and in individuals from underdeveloped countries.
Similar content being viewed by others
Introduction
Posttraumatic Stress Disorder (PTSD) is a chronic psychological disorder that can arise after exposure to a major traumatic event, such as during war, natural disasters, and serious assault [1, 2]. It is predicted that approximately 70% of adults worldwide have encountered at least one potentially traumatic event throughout their lifetime [3]. Previous estimates have reported that 5.6% of trauma-exposed individuals will develop PTSD during their lifetime [4], which can be diagnosed when individuals clinically present with symptoms including, but not limited to, flashbacks and recurring dreams of the event, avoidance behaviours, and negative alterations to cognition and arousal [5, 6]. The global prevalence of PTSD across 24 countries has been estimated to be 3.9% [4]. However, this rate is reportedly even higher in certain groups of individuals [7]. For example, PTSD is up to four times more prevalent in US combat veterans than in US civilians [8].
The pathophysiology of PTSD consists of neurochemical and neuroendocrine dysfunction [9, 10], including altered functioning of the hypothalamic-pituitary-adrenal (HPA) axis stress response [11,12,13].Dysregulation of the stress system may lead to deleterious consequences across a range of body systems, and contribute to the risk of comorbidities, such as cardiovascular, metabolic, autoimmune and inflammatory diseases [14,15,16,17,18,19].
To date, only one pooled analysis published in 2015 of 10 cohort studies has investigated the association between PTSD and the risk of all-cause mortality [20], and reported a 29% increased risk of mortality in individuals with PTSD, versus without PTSD. However, that review was not intended to be a formal meta-analysis, and may not have included all relevant studies.
Several studies have also indicated earlier cause-specific mortality in individuals with PTSD, including infection, cancer and cardiovascular-related death [21,22,23]. Increasing evidence suggests a relationship between PTSD and cardiovascular disease, with a meta-analysis of 402,274 participants published in 2013 revealing that PTSD was associated with a 55% increased risk of incident coronary heart disease or cardiac mortality [24].
Due to the number of more recent studies published in this field, there is a need for a more updated review. Thus, the primary aim of this systematic review and meta-analysis is to determine the extent to which PTSD predicts the risk of death (all-causes) at a given time, or the time to death, hereafter simply referred to as mortality risk. Sub-group analysis examined this association according to age, sex, type of trauma experienced (civilian or military environment), diagnosis or probable PTSD, type of PTSD symptoms experienced, and cause of death.
Methods
The systematic review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Statement [25], and the ‘PRISMA checklist for systematic reviews’ has been included in Supplementary Appendix 1. The protocol was registered with the International Prospective Register of Systematic Reviews (PROSPERO) (registration number CRD42019142971).
Inclusion/exclusion criteria
Types of studies
Studies were included if they were peer reviewed, original cohort or case-control studies. Reviews, case reports and series, and articles written in a language other than English were excluded.
Types of participants and exposures
Studies were included if they involved individuals with a PTSD diagnosis and a comparator group of individuals without a diagnosis of PTSD or PTSD symptoms. We also included participants with a probable diagnosis of PTSD, or PTSD symptoms, as measured by self-administered questionnaires. Subgroup analysis was later conducted to account for the differences between individuals with a formal and probable diagnosis of PTSD (see Sect. 2.5). Amendments to the protocol were made to exclude entire clinical samples with PTSD that met the criteria for another psychiatric diagnosis (e.g. a sample of patients with depression who also displayed PTSD symptoms) or another medical diagnosis (e.g. all PTSD patients who were undergoing coronary angiography). These targeted patient samples were excluded in order to limit the confounding influence of specific medical conditions, which could limit the external generalisability of the findings.
Types of outcome measures
The primary outcome of interest was mortality (all-cause as well as specific causes). Where stated, studies investigating only deaths due to suicide were excluded due to the already well-established link between PTSD and suicidal behaviour [26]. In addition, the neurobiological mechanisms underpinning PTSD and suicidal behaviour are likely to differ with that of somatic conditions. The protocol was amended to limit confounding and inflation of the pooled effect estimates because the association between PTSD and suicide is already well recognised [27]. However, studies that reported external causes of death, without distinguishing deaths due to unintentional overdoses, motor vehicle or other accidents, or suicide, were included. Deaths could be self-reported (family member, next-of-kin), from death certificates, medical records, or databases. Secondary outcomes included the cause of death. There were no restrictions regarding the length of follow-up to track mortality.
Search methods
A systematic search of EMBASE (1947-present), MEDLINE (1946-present), and PsycINFO (1806-present) was conducted through Ovid software. Relevant studies were identified using a combination of subject headings and keywords, which were adapted using truncations and Boolean operators (Supplementary Appendix 2 A-2 C). The population was identified using the following search terms: [posttraumatic stress disorder; (posttraumatic or post traumatic) adj stress; PTSD]. The outcome was identified using the following search terms: [mortality; all-cause mortality; cardiovascular mortality; hospital mortality; mortality rate; mortality rate; premature mortality; accidental death; cause of death; heart death; sudden death; mortalit*; death*]. Searches were conducted on February 12th, 2020 following consultation with a Senior Librarian. An updated search was conducted on the 17th July, 2021, and 9th December, 2022.
Data collection
Following the initial search, duplicate research articles were removed by one reviewer (DN). The articles were exported to Covidence systematic review software (www.covidence.org) for subsequent reference management. Four reviewers (DN, AP, AT, HH) independently assessed the articles by title and abstract, to determine eligibility for full-text review. Final inclusion for data extraction were determined by four reviewers (DN, AP, AT, HH), with a third reviewer (JR) involved in cases of conflicting verdicts.
One reviewer (DN) extracted the following information from the final set of included articles. Data were first extracted on 27/04/2020 using a standardised data extraction form:
-
1.
Study details (author, year, country, study design, database, baseline, and follow-up years).
-
2.
Participant characteristics (sample size, eligibility crietria, mean age, percentage of women participants).
-
3.
PTSD assessment.
-
4.
Mortality risk estimate (Odds Ratio (OR), Relative Risk (RR), Hazard Ratio (HR), or Survival Ratio (SR)), or descriptive statistics if the risk estimate was not available; and the cause of death.
-
5.
Factors adjusted for in the analysis.
Two reviewers (AP and JW) independently verified extracted data.
Quality assessment
The quality and risk of bias of the included articles were independently evaluated by four reviewers (DN,JW, AT, HH) using The Joanna Briggs Institute Critical Appraisal Checklist [28] for the relevant study design. Any discrepancies in quality assessment were resolved through discussion, and if consensus could not be reached, by a third reviewer (JR). Ten components of study quality were assessed, including whether: the PTSD and comparator groups were from the same population, PTSD was assessed in both groups, PTSD was measured in a valid and reliable way, confounding factors (age, sex, depression) were identified, strategies to deal with confounding factors were stated, participants were not deceased at the time of diagnosis, mortality was measured in a valid and reliable way, follow-up time was at least one year, follow-up time was complete for at least 80% of participants, and appropriate statistical analysis was used. Articles were scored out of ten, with a score of one to four indicating poor quality, five to seven indicating fair quality, and eight to ten indicating good quality.
The Grading of Recommendations Assessment, Development and Evaluation (GRADE) framework was used to evaluate the quality of evidence in which the following were assessed: risk of bias, inconsistency (based on heterogeneity), indirectness (population differences), imprecision (summary estimate CIs), publication bias (funnel plots and Egger’s test), and pooled effect sizes (OR/RR and HR) [29].
Data syntheses and meta-analyses
Meta-analyses were conducted with the final included studies using Stata statistical software, version 16.0 (StataCorpLP, College Station, TX, USA). The risk estimates of interest were Odds Ratio (OR) and Risk Ratio (RR), in addition to Hazard Ratio (HR) which provided information regarding time to death. A random-effects approach was used to report the overall mortality risk estimates (OR/RR, HR, 95% CI), to be displayed as forest plots. The risk estimates of OR and RR were combined in the one meta-analysis, as OR can be used to approximate RR when the outcomes are relatively rare [30]. For studies in which more than one estimate was provided, we endeavoured to extract the effect size which would be the most generalisable (e.g. using results from all-cause mortality rather than cause-specific death), adjusted for the covariates of interest (age, sex, depression), and from the largest sample provided.
Heterogeneity was assessed using I² statistics, with the results of this analysis interpreted according to the Cochrane guidelines (0–40% = might not be important; 30–60% = may represent moderate heterogeneity; 50–90% = may represent substantial heterogeneity; and 75–100% = considerable heterogeneity) [31]. Statistical significance was set at P < 0.05. Publication biases were assessed using funnel plots and Egger’s test. Additional subgroup analyses were conducted to investigate factors that may account for heterogeneity in the association between PTSD and mortality. This included according to age, sex, whether participants were military veterans or civilians, follow-up years, whether PTSD diagnoses or a probable diagnosis (based on cut-points from continuous symptom severity scores) was assessed, type of PTSD symptom experienced, cause of death, and risk of bias assessment.
Results
Search results
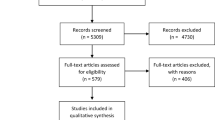
The search of EMBASE, MEDLINE and PsycINFO yielded 9,945 articles (Fig. 1). Duplicates were removed (n = 2,883), resulting in 7,062 papers included for subsequent screening. Upon screening by title and abstract, a further 6,882 articles were excluded, as these studies either did not investigate human populations, were not in English, or were nonprimary research articles. One hundred and eighty articles underwent a full-text review. Of these articles, 146 papers were excluded as they did not meet the eligibility criteria. A further four studies were excluded as they utilised the same participants, or a subsample [32,33,34,35]. To avoid repeating participants in the meta-analysis, only one study that utilised the same participants was selected [36], and this was based on having a completed sample, and a variety of outcomes (all-cause, external, cardiovascular (CVD) and cancer-related deaths). An additional search of Google Scholar revealed 13 articles, and citation searching yielded 102 articles, however none of these studies proceeded to full-text screening. A total of 30 articles were thus included in this systematic review, with 24 articles included in the primary meta-analysis.
Study and participant characteristics
The characteristics of the 30 included studies [22, 23, 36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63], encompassing at least 2.1 million participants with a confirmed or probable diagnosis of PTSD are shown in Table 1. All studies were cohort studies, except for one case-control [56]. The period of follow-up ranged from one to 70 years, and the majority of studies (n = 22) had a follow-up of ≤ 10 years. Nineteen studies were conducted in the US, seven in Europe, two in the Middle East, and two in East-Asia. The majority of the included studies focused specifically on veteran military populations, and only 12 studies analysed civilian populations. Of the civilian studies, two involved participants exposed to war trauma [38, 49], two terrorist attacks [41, 51], one a natural disaster [44], and seven included participants exposed to any type of trauma [22, 23, 45, 58,59,60,61].
The majority of samples were male-dominated, with six studies involving only men, and only one study with women exclusively [45]. Amongst the studies that included both sexes, the percentage of women ranged from 0.5 to 64.6%. One study did not specify the proportion of each sex [60], and one study did not specify if both sexes were included [55].
The percentage of participants with PTSD varied between 0.74% and 69%. PTSD was most frequently diagnosed using the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) [64]. A total of nine studies [38, 41, 44,45,46, 51,52,53,54] investigated a probable diagnosis of PTSD.
All but seven studies [22, 23, 37, 51, 56, 58, 62] investigated all-cause mortality. While we have excluded studies that focused specifically on suicide, four studies [36, 48, 60, 62] reported findings for all external causes of death (which included suicide, homicide and accidental deaths). Four studies analysed CVD-related deaths [23, 36, 41, 55], three studies reported deaths by cancer [22, 36, 48], and one study investigated infection-related deaths [58].
Risk of bias assessment
The risk of bias scores assessing methodological quality of the included studies is shown in Supplementary Appendix 3 A-3B. Fifteen articles were rated as good quality (score 8–10), 14 as fair [4,5,6,7], and one only as poor quality (≤ 3) [55]. The most common sources of potential bias were participants without PTSD not having undergone PTSD assessment (due to many studies obtaining diagnoses via medical records rather than performing an assessment in the entire sample), failure to identify and deal with potential confounding factors (in particular depression), and lack of information regarding whether follow-up was complete. Quality of evidence was assessed by GRADE criteria. Of the five categories, the only serious issue was inconsistency, due to high unexplained heterogeneity (Supplementary Appendix 4). However, given all studies were observational, thus initially classified as ‘low’ overall anyway, this rating was further downgraded to ‘very low’ [65].
Meta-analyses
Twenty-four cohort studies provided the estimates used in the meta-analyses. All-cause mortality was used as the outcome in all but three studies that only provided estimates for external causes of death [37, 51, 62], and one study which only provided an estimate for cardiovascular-related cause of death [23]. One study [39] provided a survival ratio (SR = 1.37 (1.34–1.40), that was converted into a risk estimate (estimate = 0.63 (0.6–0.66)). Two studies that showed a positive association between PTSD and mortality were excluded from meta-analyses as they did not provide any comparable statistics [53, 55] (Table 1). The one case-control study [56] was too heterogenous (in terms of study design and temporal sequence) to include in the meta-analyses. However, that study demonstrated a 2.8-fold increased risk of mortality amongst soldiers with PTSD. Amongst the studies that measured symptoms or severity of PTSD, two (which presented null findings) were based on a dimensional metric [52, 54] (rather than a 0 vs. 1 determination to indicate probable PTSD diagnosis), and were excluded from analyses. An additional article was also excluded from the main meta-analyses [22] as it utilised the same participants as another study [61], but was later included in the subgroup analyses investigating causes of death.
Meta-analyses were conducted to investigate the overall association between PTSD and mortality. Across the six studies that provided estimates for odds and risk ratios, there was a 47% (95% CI: 1.06–2.04, P = 0.02) greater risk of mortality (Fig. 2). However, substantial heterogeneity was also observed (I2 = 94.96%). There was also some evidence of publication bias, as observed by asymmetry in the funnel plots (Supplementary Appendix 5 A), however this was not significant after conducting Egger’s test (P = 0.30).
Similarly, a positive association was observed between PTSD and time-to-death across the 18 studies reporting hazard ratios (HR: 1.32, 95% CI: 1.10–1.59, P = 0.00). (Fig. 3). Very high heterogeneity was observed (I2 = 99.17%), with no strong evidence of publication bias (Supplementary Appendix 5B) (Egger’s test, P = 0.53).
Subgroup analyses
Subgroup analyses were performed to investigate potential sources of heterogeneity and to see whether the association between PTSD and mortality differed according to specific study characteristics.
Civilian vs. veteran: Among four studies of civilians [49, 51, 59, 60] PTSD was associated with an 70% greater risk (OR/RR 95% CI: 1.51–1.91, I2 = 0.00%, k (number of studies) = 4) (Supplementary Appendix 6 A). Likewise, seven studies investigating time to death showed that risk was 55% greater in civilians (HR 95% CI: 1.41–1.71, I2 = 39.82%, k = 7). No significant association was found for the subgroup of studies in veteran populations (k = 11) (Supplementary Appendix 6B).
Diagnosis vs. probable PTSD: There was a 55% greater risk (HR 95% CI: 1.27–1.87, I2 = 39.68%, k = 5) of mortality in studies that measured probable PTSD, whilst no significant association was found for studies that included a diagnosis of PTSD (k = 13) (Supplementary Appendix 7).
PTSD symptoms: Among the studies which included PTSD symptoms, only one article provided an effect size for mortality risk within individual symptom categories (intrusion, avoidance, arousal) [38], thus no subgroup analysis was undertaken.
Cause of death: PTSD was associated with an increased risk of external causes of death (HR: 2.03, 95% CI: 1.50–2.74, I2 = 94.07%, k = 5) [36, 37, 40, 41, 62], cancer-related deaths (HR 95% CI: 1.14–1.66, I2 = 0.00%, k = 2) [22, 36] and CVD-related deaths (HR 95% CI: 1.30–1.81, I2 = 32.66%, k = 3) [23, 36, 41] (Supplementary Appendix 8 A). Likewise, similar results were observed in studies that provided OR/RR estimates (Supplementary Appendix 8B).
Sex: Given that most studies involved a majority of men (with many only involving men), it was not possible to investigate subgroups defined by sex (Supplementary Appendix 9).
Follow-up period: The majority of studies had a follow-up period of ≤ 10 years but there were no clear differences observed in the subgroup analysis (Supplementary Appendix 10). [59].
Methodological quality of the studies: Similar trends were observed across all methodological quality subgroups (Supplementary Appendix 11 A and B).
Discussion
Summary of evidence
This systematic review summarises the findings of 30 longitudinal studies examining the association between PTSD and mortality. Studies were of fair-good methodological quality and included at least 2.1 million participants with a PTSD diagnosis or probable PTSD, who were primarily male military veteran populations. Meta-analyses indicated that PTSD increased mortality risk by approximately 47% in six studies reporting OR/RR, and 32% in 18 studies examining time to death, when compared to individuals without PTSD. However, it is important to acknowledge the very high heterogeneity in the interpretation of the meta-analyses, and subgroup analyses did not account for this heterogeneity.
There was a significantly increased risk of mortality with PTSD among civilian populations, but not among the veteran subgroup. Civilian traumas, including natural disasters and sexual assault are generally unexpected, compared to military personnel who are trained and prepared for the trauma-exposure. Some research suggests that a combination of accessibility to treatment and awareness of the disorder within veteran groups promotes greater management of PTSD than in the general population [7]. Of note however, the heterogeneity remained high in the veteran subgroup, but was much lower for the civilians. [66]. When investigating subgroups according to cause of death, the largest effect size was observed for external causes of death. While the focus of this review was on unintentional causes of death, studies investigating external causes of death did not distinguish suicide from other external causes (e.g. homicide). Thus, it is possible that suicides partly account for our finding that PTSD had a stronger association with external causes of death. We also found that PTSD was associated with cancer-related and CVD-related death, with previous studies also describing a relationship between PTSD and incidence of these diseases [67,68,69]. It has been hypothesised that an overactivity of the sympathetic nervous system in individuals with PTSD, could increase basal heart rate and cause endothelial dysfunction, and subsequently lead to cardiac events. However, it is possible that health problems, including acute cardiovascular events [70] are sufficient to precipitate PTSD in patients, hence it is sometimes difficult to establish whether they lie on the causal pathway with PTSD, or an independent risk factor for mortality.
Comparison with literature
These findings are largely consistent with a previous pooled analysis [20] that found that participants with PTSD have a 29% greater risk of mortality than those without PTSD. Unlike the present study, that analysis only consisted of 10 papers that excluded hazard ratio information and extensive subgroup analysis. Thus, our findings based on 30 studies conducted using a thorough systematic review, substantially adds to this previous work. In contrast, five independent studies (included in this review) found PTSD to be associated with a reduced mortality risk [39, 43, 47, 50, 57]. These results may be attributed to psychological resilience, as evidence suggesting that experiencing a traumatic event may provide resilience to physical morbidity and mortality, with reduced dementia incidence observed in a France cohort who had undergone lifetime trauma [71]. Thus, it is possible that the populations in studies showing reverse associations may have unique resilience factors, which could also account for the very high heterogeneity observed in our pooled meta-analysis.
Survivorship effects may also explain negative associations between PTSD and mortality, and are supported by our subgroup analyses which did not show excess mortality in studies ≥ 20 years. Specifically, those who survive to older age may be in greater physical and mental health, and be utilising more healthcare services that may be beneficial for longevity. The lack of excess mortality in older-aged adults (60 years and above) by three included studies [39, 50, 57] supports this theory. However, due to the large age ranges included, we were unable to investigate subgroups according to age.
Potential confounders
While various morbidities may lie on the causal pathway in the association between PTSD and mortality, they may also have a confounding effect independent of shared pathogenesis with PTSD. It has been suggested that people with PTSD are more likely to experience more severe service-connected comorbidities, which may independently be associated with up to a 2.5-fold increased risk of one-year mortality [72].The presence of PTSD may increase patients’ risk of morbidities such as cancer, diabetes, neurodegeneration, gastrointestinal disease, and autoimmune disorders, which may subsequently increase mortality [73]. One explanation may be due to elevated proinflammatory cytokines (e.g., tumour necrosis factor-α and interleukin-6), and reactive oxygen species, which can occur with neuroendocrine changes in PTSD [14, 74], and may be associated with the pathologies of the aforementioned chronic diseases. Nine studies included in this review [22, 43, 45, 50, 57, 58, 61,62,63] adjusted for physical comorbidities, and four of these studies were not able to indicate excess mortality with PTSD [43, 45, 50, 57]. Mild traumatic brain injury (mTBI) is one possible illness driving the PTSD/mortality association as this is a common occurrence with PTSD [75]. However, despite this, mTBI was adjusted by only two eligible studies [56, 62]. Thus, it is difficult to establish whether it is PTSD, or such other morbidities, that are responsible for increasing mortality risk in our results.
Psychiatric comorbidities are highly prevalent in PTSD affected individuals, with more than 90% of people with PTSD also having another lifetime mental disorder [76]. However, only four studies [57, 58, 61, 62] considered all psychiatric comorbidities in their analyses, and only one of these studies did not demonstrate an increased risk of mortality [57]. Major Depressive Disorder (MDD) or depressive symptoms, which many of the included studies did not adjust for, may explain the strong association observed with external causes of death, as suicidality risk is increased combined with PTSD [77]. Adjusting for psychiatric disorders in a study investigating PTSD as an exposure is a challenge, as other conditions may also share trauma as a common aetiology [78]. However, adjusting for these factors may be unnecessary in the possibility that PTSD may precipitate the formation of other psychiatric disorders, leading to subsequent mortality.
Generalisability of the findings
A large proportion of participants were US veterans and men, and the current evidence may thus not be widely generalisable to women in the general community. As US veterans have access to specialised healthcare through the Veterans Health Administration [79], our findings may not be applicable to the large majority of the US population who don’t have access to this service or have private insurance. Healthcare utilisation could improve survival and may partially explain the negative association observed in three US veteran studies [39, 43, 50]. In addition to healthcare utilisation, PTSD may be better diagnosed in veterans, due to being an at-risk population. The included studies may have also misrepresented the true number of PTSD patients in the population, due to the challenges in diagnosing PTSD. As PTSD diagnoses were obtained through medical records in the majority of studies, it is possible that there may be undiagnosed participants, which could dilute the true association with mortality. It is likely that the stigma associated with mental illness would be a barrier in diagnosing PTSD, particularly within military environments [80]. Misdiagnoses may have also occurred, as PTSD has overlapping symptoms with other psychiatric disorders [81].
Strengths
This review was conducted in adherence with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement. Our searches were conducted across three electronic databases, including a grey literature search. Studies were also screened and extracted independently by multiple reviewers. All included studies were longitudinal, were of mostly good methodological quality, and had follow-up periods of at least one year, with only a few studies with follow-up time of less than two years. We included studies with diagnoses and symptoms of PTSD, and the majority of studies also had a valid measure of mortality from nationwide death registries, as opposed to self-report by relatives.
Limitations
Despite the aforementioned strengths of this review, there was substantial heterogeneity between studies (I2 > 94%), which contributed to the ‘very low’ rating in the GRADE assessment. Thus, the unexplained heterogeneity limits the overall conclusions that can be drawn. It is likely that the heterogeneity of our analyses was increased due to our primary outcome being all-cause mortality, which also included studies that investigated any cause of mortality. However, we also performed subgroup analysis where we examined specific cause of death, and variation in length of follow-up may also be a source of heterogeneity in our analyses. We were also unable to perform subgroup analysis based on type of PTSD assessment (e.g. interview or self-report), as many of the included studies did not specify the delivery of this assessment, due to PTSD status being ascertained from chart review. It is likely that structured diagnostic interview assessments, such as the Clinician-Administered PTSD Scale for DSM-5, would provide more reliable and valid determinations of PTSD [82]. Additionally, only some studies adjusted for depressive symptoms and disorders, which may explain the strong associations observed with death by external causes. It is also possible that not all of the included studies were independent, especially studies analysing databases of US veterans, in which the same participant may be included across multiple studies. This is of concern, as overlapping participants could lead to underestimated standard errors and confidence intervals, thus overestimating the precision of our overall estimates [83]. Furthermore, a major source of bias affecting the methodological quality of the studies included not measuring PTSD in the comparator group. Thus, these studies are likely to have a higher percentage of individuals affected by PTSD, thus the provided estimates may be diluted. As we only included three databases in our search strategy, it is possible we may have excluded relevant articles in our analyses. Therefore, the conclusions should be considered within the constraints of these limitations.
Future directions and conclusion
Our systematic review and meta-analysis is the first comprehensive systematic review and meta-analysis to provide evidence of PTSD increasing the risk of mortality. However, the high unexplained heterogeneity of our findings, should be considered in the interpretation of these results.
The findings of our review also highlight several gaps in the literature which need to be addressed. Prior literature suggests that PTSD disproportionately affects more women than men [7], however only eight included articles included a greater than 50% representation from women [21,22,23, 44, 45, 49, 59, 61]. While half of these articles have been published in the last two years, suggesting a shift towards equal gender representation in contemporary research, there is still a need for more studies with women. A possible future research question could also be to request female-only data or sex split data from the samples in this review, to ascertain whether a sex difference may be occurring with these results. Furthermore, only 12 included studies analysed civilians, with seven of those articles reporting associations with non-specific traumas [22, 23, 45, 58,59,60,61]. While PTSD has historically been referred to as a military disorder, it is increasingly becoming more prevalent among civilians, especially after the COVID-19 pandemic [84]. Thus, further research is required within civilian populations, particularly in countries outside of the US.
Findings from this review highlight the long-term implications of PTSD and may be beneficial in promoting prevention and treatment strategies for this highly debilitating disorder. This review provides preliminary evidence to precipitate future studies, that could investigate whether treating PTSD could reverse premature mortality and aid longevity.
Data Availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
Abbreviations
- CI:
-
Confidence Interval
- CVD:
-
Cardiovascular Disease
- GRADE:
-
Grading of Recommendations Assessment Development and Evaluation
- HR:
-
Hazard Ratio
- ICD-9-CM:
-
International Classification of Diseases Ninth Revision Clinical Modification
- MDD:
-
Major Depressive Disorder
- mTBI:
-
Mild Traumatic Brain Injury
- OR:
-
Odds Ratio
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- PROSPERO:
-
International Prospective Register of Systematic Reviews
- PTSD:
-
Posttraumatic Stress Disorder
- RR:
-
Risk Ratio
- SR:
-
Survival Ratio
References
Kilpatrick DG, Resnick HS, Milanak ME, Miller MW, Keyes KM, Friedman MJ. National estimates of exposure to traumatic events and PTSD prevalence using DSM-IV and DSM-5 criteria. J Trauma Stress. 2013;26(5):537–47.
Al Jowf GI, Ahmed ZT, An N, Reijnders RA, Ambrosino E, Rutten BPF et al. A Public Health Perspective of Post-Traumatic Stress Disorder.Int J Environ Res Public Health. 2022;19(11).
Benjet C, Bromet E, Karam EG, Kessler RC, McLaughlin KA, Ruscio AM, et al. The epidemiology of traumatic event exposure worldwide: results from the World Mental Health Survey Consortium. Psychol Med. 2016;46(2):327–43.
Koenen KC, Ratanatharathorn A, Ng L, McLaughlin KA, Bromet EJ, Stein DJ, et al. Posttraumatic stress disorder in the World Mental Health surveys. Psychol Med. 2017;47(13):2260–74.
Sareen J. Posttraumatic stress disorder in adults: impact, comorbidity, risk factors, and treatment. Can J Psychiatry. 2014;59(9):460–7.
Ressler KJ, Berretta S, Bolshakov VY, Rosso IM, Meloni EG, Rauch SL, et al. Post-traumatic stress disorder: clinical and translational neuroscience from cells to circuits. Nat reviews Neurol. 2022;18(5):273–88.
Lehavot K, Katon JG, Chen JA, Fortney JC, Simpson TL. Post-traumatic stress disorder by gender and veteran status. Am J Prev Med. 2018;54(1):e1–e9.
Richardson LK, Frueh BC, Acierno R. Prevalence estimates of combat-related post-traumatic stress disorder: critical review. Aust N Z J Psychiatry. 2010;44(1):4–19.
Sherin JE, Nemeroff CB. Post-traumatic stress disorder: the neurobiological impact of psychological trauma. Dialogues Clin Neurosci. 2011;13(3):263–78.
Aliev G, Beeraka NM, Nikolenko VN, Svistunov AA, Rozhnova T, Kostyuk S et al. Neurophysiology and Psychopathology Underlying PTSD and Recent Insights into the PTSD Therapies-A Comprehensive Review.J Clin Med. 2020;9(9).
Meewisse M-L, Reitsma JB, De Vries G-J, Gersons BPR, Olff M. Cortisol and post-traumatic stress disorder in adults: systematic review and meta-analysis. Br J Psychiatry. 2007;191(5):387–92.
Ancelin ML, Scali J, Norton J, Ritchie K, Dupuy AM, Chaudieu I, et al. The effect of an adverse psychological environment on salivary cortisol levels in the elderly differs by 5-HTTLPR genotype. Neurobiol Stress. 2017;7:38–46.
Speer KE, Semple S, Naumovski N, D’Cunha NM, McKune AJ. HPA axis function and diurnal cortisol in post-traumatic stress disorder: a systematic review. Neurobiol Stress. 2019;11:100180.
Neigh GN, Ali FF. Co-morbidity of PTSD and immune system dysfunction: opportunities for treatment. Curr Opin Pharmacol. 2016;29:104–10.
Dedert EA, Calhoun PS, Watkins LL, Sherwood A, Beckham JC. Posttraumatic stress disorder, cardiovascular, and metabolic disease: a review of the evidence. Annals of behavioral medicine: a publication of the Society of Behavioral Medicine. 2010;39(1):61–78.
Sun Y, Qu Y, Zhu J. The relationship between inflammation and post-traumatic stress disorder. Front Psychiatry. 2021;12:707543.
Bookwalter DB, Roenfeldt KA, LeardMann CA, Kong SY, Riddle MS, Rull RP. Posttraumatic stress disorder and risk of selected autoimmune diseases among US military personnel. BMC Psychiatry. 2020;20(1):23.
Vidal C, Polo R, Alvarez K, Falgas-Bague I, Wang Y, B LC, et al. Co-occurrence of posttraumatic stress disorder and Cardiovascular Disease among Ethnic/Racial groups in the United States. Psychosom Med. 2018;80(7):680–8.
Lihua M, Tao Z, Hongbin M, Hui W, Caihong J, Xiaolian J. Metabolic syndrome risk in relation to posttraumatic stress disorder among trauma-exposed civilians in Gansu Province, China.Medicine (United States). 2020;99 (1) (no pagination)(e18614).
Lohr JB, Palmer BW, Eidt CA, Aailaboyina S, Mausbach BT, Wolkowitz OM, et al. Is post-traumatic stress disorder associated with premature senescence? A review of the literature. Am J Geriatric Psychiatry. 2015;23(7):709–25.
Song H. Stress related disorder and risk of inflammation-related conditions: evidence from Population-Based sibling controlled Cohort Studies. Biol Psychiatry. 2020;87(9 Supplement):49.
Tian F, Fang F, Shen Q, Ye W, Valdimarsdottir UA, Song H. Stress-related disorders and subsequent cancer risk and mortality: a population-based and sibling-controlled cohort study in Sweden. Eur J Epidemiol. 2022;37(9):947–58.
Kim K, Tsai AC, Sumner JA, Jung SJ. Posttraumatic stress disorder, cardiovascular disease outcomes and the modifying role of socioeconomic status. J Affect Disord. 2022;319:555–61.
Edmondson D, Kronish IM, Shaffer JA, Falzon L, Burg MM. Posttraumatic stress disorder and risk for coronary heart disease: a meta-analytic review. Am Heart J. 2013;166(5):806–14.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev. 2021;10(1):89.
Krysinska K, Lester D. Post-traumatic stress disorder and suicide risk: a systematic review. Arch Suicide Res. 2010;14(1):1–23.
Fox V, Dalman C, Dal H, Hollander AC, Kirkbride JB, Pitman A. Suicide risk in people with post-traumatic stress disorder: a cohort study of 3.1 million people in Sweden. J Affect Disord. 2021;279:609–16.
Institute TJB. Joanna Briggs Institute Reviewers’ Manual: 2014 edition / Supplement. 2014.
Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336(7650):924–6.
Akobeng AK. Understanding systematic reviews and meta-analysis. Arch Dis Child. 2005;90(8):845.
Higgins J, Thomas J, Chandler J, Cumpston M, Li T, Page M et al. Cochrane Handbook for Systematic Reviews of Interventions version 6.2. 2021.
Boscarino JA. A prospective study of ptsd and early-age heart disease mortality among vietnam veterans: implications for surveillance and prevention. Psychosom Med. 2008;70(6):668–76.
Boscarino JA. Psychobiologic predictors of disease mortality after psychological trauma: implications for research and clinical surveillance. J Nerv Mental Disease. 2008;196(2):100–7.
Boscarino JA. External-cause mortality after psychologic trauma: the effects of stress exposure and predisposition. Compr Psychiatr. 2006;47(6):503–14.
Boscarino JA, Figley CR. The impact of repression, hostility, and post-traumatic stress disorder on all-cause mortality: a prospective 16-year follow-up study. J Nerv Mental Disease. 2009;197(6):461–6.
Boscarino JA. Posttraumatic stress disorder and mortality among U.S. Army veterans 30 years after military service. Ann Epidemiol. 2006;16(4):248–56.
Bohnert AS, Ilgen MA, Ignacio RV, McCarthy JF, Valenstein M, Blow FC. Risk of death from accidental overdose associated with psychiatric and substance use disorders. Am J Psychiatry. 2012;169(1):64–70.
Bramsen I, Deeg DJH, van der Ploeg E, Fransman S. Wartime stressors and mental health symptoms as predictors of late-life mortality in World War II survivors. J Affect Disord. 2007;103(1–3):121–9.
Cho J, Copeland LA, Stock EM, Zeber JE, Restrepo MI, MacCarthy AA, et al. Protective and risk factors for 5-Year survival in the Oldest Veterans: data from the Veterans Health Administration. J Am Geriatr Soc. 2016;64(6):1250–7.
Flood AM, Boyle SH, Calhoun PS, Dennis MF, Barefoot JC, Moore SD, et al. Prospective study of externalizing and internalizing subtypes of posttraumatic stress disorder and their relationship to mortality among Vietnam veterans. Compr Psychiatr. 2010;51(3):236–42.
Giesinger I, Li J, Takemoto E, Cone JE, Farfel MR, Brackbill RM. Association between Posttraumatic stress disorder and mortality among responders and Civilians following the September 11, 2001. Disaster JAMA network open. 2020;3(2):e1920476.
Kimbrell T, Pyne JM, Kunik ME, Magruder KM, Petersen NJ, Yu H-J, et al. The impact of purple heart commendation and PTSD on mortality rates in older veterans. Depress Anxiety. 2011;28(12):1086–90.
Kinder LS, Bradley KA, Katon WJ, Ludman E, McDonell MB, Bryson CL. Depression, posttraumatic stress disorder, and mortality. Psychosom Med. 2008;70(1):20–6.
Li X, Aida J, Hikichi H, Kondo K, Kawachi I. Association of Postdisaster Depression and Posttraumatic Stress Disorder with Mortality among Older Disaster Survivors of the 2011 Great East Japan Earthquake and Tsunami.JAMA Network Open. 2019;2 (12) (no pagination)(e1917550).
Roberts AL, Kubzansky LD, Chibnik LB, Rimm EB, Koenen KC. Association of Posttraumatic stress and depressive symptoms with mortality in women. JAMA Netw Open. 2020;3(12):e2027935.
Schlenger WE, Corry NH, Williams CS, Kulka RA, Mulvaney-Day N, DeBakey S, et al. A prospective study of mortality and trauma-related risk factors among a nationally Representative Sample of Vietnam Veterans. Am J Epidemiol. 2015;182(12):980–90.
Zohar J, Fostick L. Mortality rates between treated post-traumatic stress disorder israeli male veterans compared to non-diagnosed veterans. Eur Neuropsychopharmacol. 2014;24(1):117–24.
Bullman TA, Kang HK. Posttraumatic stress disorder and the risk of traumatic deaths among Vietnam veterans. J Nerv Mental Disease. 1994;182(11):604–10.
Mollica RF, Sarajlic N, Chernoff M, Lavelle J, Sarajlic Vukovic I, Massagli MP. Longitudinal study of psychiatric symptoms, disability, mortality, and emigration among bosnian refugees. JAMA: J Am Med Association. 2001;286(5):546–54.
Trivedi RB, Post EP, Sun H, Pomerantz A, Saxon AJ, Piette JD, et al. Prevalence, Comorbidity, and prognosis of Mental Health among US Veterans. Am J Public Health. 2015;105(12):2564–9.
Welch AE, Zweig KC, Liao T, Yip J, Davidson A, Jordan H, et al. Alcohol and drug-related mortality among enrollees in the world trade center health registry (WTCHR), 2004 to 2012. J Occup Environ Med. 2018;60(10):875–9.
Wolf EJ, Logue MW, Stoop TB, Schichman SA, Stone A, Sadeh N, et al. Accelerated DNA methylation age: Associations with posttraumatic stress disorder and mortality. Psychosom Med. 2018;80(1):42–8.
Vaillant GE, Highum Vaillant D, US. The effects of combat and posttraumatic stress disorder on longevity. Spiro, Avron III [Ed]; Settersten, Richard A Jr, editor; Aldwin, Carolyn M, editor (2018) Long-term outcomes of military service: The health and well-being of aging veterans (pp 245–255) xviii, 306 pp Washington, DC, US: American Psychological Association;. 2018:245 – 55.
Solomon Z, Levin Y, Crompton L, Ginzburg K. Is acute stress reaction a risk factor for early mortality? Health Psychol. 2019;38(7):606–12.
Kilbourne AM, Ignacio RV, Kim HM, Blow FC. Are VA patients with serious mental illness dying younger? Psychiatric Serv. 2009;60(5):589.
Lewandowski-Romps L, Schroeder HM, Berglund PA, Colpe LJ, Cox K, Hauret K, et al. Medical-encounter mental health diagnoses, non-fatal injury and polypharmacy indicators of risk for accident death in the US Army enlisted soldiers, 2004–2009. Prev Medicine: Int J Devoted Pract Theory. 2018;111:299–306.
Chwastiak LA, Rosenheck RA, Desai R, Kazis LE. Association of psychiatric illness and all-cause mortality in the national department of veterans affairs health care system. Psychosom Med. 2010;72(8):817–22.
Song H, Fall K, Fang F, Erlendsdóttir H, Lu D, Mataix-Cols D, et al. Stress related disorders and subsequent risk of life threatening infections: population based sibling controlled cohort study. BMJ. 2019;367:l5784.
Gradus JL, Antonsen S, Svensson E, Lash TL, Resick PA, Hansen JG. Trauma, comorbidity, and mortality following diagnoses of severe stress and adjustment disorders: a nationwide cohort study. Am J Epidemiol. 2015;182(5):451–8.
Meier SM, Mattheisen M, Mors O, Mortensen PB, Laursen TM, Penninx BW. Increased mortality among people with anxiety disorders: total population study. Br J Psychiatry. 2016;209(3):216–21.
Tian F, Shen Q, Hu Y, Ye W, Valdimarsdóttir UA, Song H, et al. Association of stress-related disorders with subsequent risk of all-cause and cause-specific mortality: a population-based and sibling-controlled cohort study. Lancet Reg health Europe. 2022;18:100402.
Clark R, Kuffel RL, Neylan TC, Maguen S, Li Y, Boscardin WJ et al. Posttraumatic stress disorder, suicide, and unintended overdose death in later life: A national cohort study of veterans aged 50 and older.Journal of the American Geriatrics Society. 2022;n/a(n/a).
Szymanski BR, Hein TC, Schoenbaum M, McCarthy JF, Katz IR. Facility-level excess mortality of VHA patients with mental health or substance use disorder diagnoses. Psychiatric Serv. 2021;72(4):408–14.
Control CfD. International Classification of Diseases-9-CM 2007 [Available from: http://www.cdc.gov/nchs/icd.htm
Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011;64(4):383–94.
Olff M. Sex and gender differences in post-traumatic stress disorder: an update. Eur J Psychotraumatology. 2017;8(sup4):1351204.
Edmondson D, von Känel R. Post-traumatic stress disorder and cardiovascular disease. Lancet Psychiatry. 2017;4(4):320–9.
Kaster TS, Sommer JL, Mota N, Sareen J, El-Gabalawy R. Post-traumatic stress and cancer: findings from a cross-sectional nationally representative sample. J Anxiety Disord. 2019;65:11–8.
Roberts AL, Huang T, Koenen KC, Kim Y, Kubzansky LD, Tworoger SS. Posttraumatic stress disorder is Associated with increased risk of ovarian Cancer: a prospective and retrospective longitudinal cohort study. Cancer Res. 2019;79(19):5113–20.
Jacquet-Smailovic M, Alla F, Denis I, Kirche A, Tarquinio C, Brennstuhl MJ. Posttraumatic stress disorder following myocardial infarction: a systematic review. J Trauma Stress. 2021;34(1):190–9.
Nilaweera D, Freak-Poli R, Ritchie K, Chaudieu I, Ancelin ML, Ryan J. The long-term consequences of trauma and posttraumatic stress disorder symptoms on later life cognitive function and dementia risk. Psychiatry Res. 2020;294:113506.
Maynard C, Nelson K, Fihn SD. Disability rating and 1-Year Mortality among Veterans with Service-Connected Health Conditions. Public Health Rep. 2018;133(6):692–9.
Brudey C, Park J, Wiaderkiewicz J, Kobayashi I, Mellman TA, Marvar PJ. Autonomic and inflammatory consequences of posttraumatic stress disorder and the link to cardiovascular disease. Am J Physiol Regul Integr Comp Physiol. 2015;309(4):R315–R21.
Kim TD, Lee S, Yoon S. Inflammation in post-traumatic stress disorder (PTSD): a review of potential Correlates of PTSD with a neurological perspective. Antioxid (Basel). 2020;9(2):107.
Bryant R. Post-traumatic stress disorder vs traumatic brain injury. Dialog Clin Neurosci. 2011;13(3):251–62.
Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995;52(12):1048–60.
Stevens D, Wilcox HC, MacKinnon DF, Mondimore FM, Schweizer B, Jancic D, et al. Posttraumatic stress disorder increases risk for suicide attempt in adults with recurrent major depression. Depress Anxiety. 2013;30(10):940–6.
Yen S, Shea MT. Recent developments in research of trauma and personality disorders. Curr Psychiatry Rep. 2001;3(1):52–8.
Oliver A. The Veterans Health Administration: an american success story? Milbank Q. 2007;85(1):5–35.
Mittal D, Drummond KL, Blevins D, Curran G, Corrigan P, Sullivan G. Stigma associated with PTSD: perceptions of treatment seeking combat veterans. Psychiatr Rehabil J. 2013;36(2):86–92.
Flory JD, Yehuda R. Comorbidity between post-traumatic stress disorder and major depressive disorder: alternative explanations and treatment considerations. Dialog Clin Neurosci. 2015;17(2):141–50.
Lancaster CL, Teeters JB, Gros DF, Back SE. Posttraumatic stress disorder: overview of evidence-based Assessment and Treatment. J Clin Med. 2016;5(11):105.
Cheung MW. A guide to conducting a Meta-analysis with non-independent effect sizes. Neuropsychol Rev. 2019;29(4):387–96.
Yunitri N, Chu H, Kang XL, Jen HJ, Pien LC, Tsai HT, et al. Global prevalence and associated risk factors of posttraumatic stress disorder during COVID-19 pandemic: a meta-analysis. Int J Nurs Stud. 2022;126:104136.
Acknowledgements
We would like to thank Ms. Lorena Romero from the Ian Potter Library, Alfred Hospital, Melbourne for guidance in finalising the search strategy.
Funding
This study received no specific grant from any funding agency, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
DN conducted the initial literature search, screened articles for eligibility and risk of bias, extracted and synthesised data, and wrote the manuscript. AP, AT, DN, HH screened articles for eligibility, and AP, AT, DN HH and JW assessed risk of bias. AP and JW also independently verified the extracted data. To resolve discrepancies, JR was the third reviewer during article screening, and risk of bias assessment. CG, JR, and RFP reviewed draft manuscripts. All authors read and gave final approval to the submitted manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Nilaweera, D., Phyo, A.Z., Teshale, A.B. et al. Lifetime posttraumatic stress disorder as a predictor of mortality: a systematic review and meta-analysis. BMC Psychiatry 23, 229 (2023). https://doi.org/10.1186/s12888-023-04716-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12888-023-04716-w