Abstract
Objective
Diabetes distress typically causes depressive symptoms; common comorbidity of diabetes unpleasantly affects patients’ medical and psychological functions. Psychotherapeutic interventions are effective treatments to treat depressive symptoms and to improve the quality of life in many chronic diseases including diabetes. The present study investigated the efficacy of cognitive behavior therapy (CBT) to treat depressive symptoms in patients with type 2 diabetes mellitus (T2DM) using experimental and waitlist control conditions.
Materials and Methods
A total of 130 diagnosed patients with T2DM were taken from outdoor patients services of different hospitals in Faisalabad. Ninety patients met the eligibility criteria and were randomly assigned to experimental (n = 45) and waitlist control (n = 45) conditions. All the patients completed clinical interviews and assessment measures at pre-and post-assessment stages (16 weeks intervals). Medical consultants at the respective hospitals diagnosed the patients on the base of their medical reports and then referred those patients to us. Then we used different scales to assess primary and secondary outcomes: Diabetes Distress Scale (DDS) and Patient Health Questionnaire (PHQ) to assess primary outcomes, and a Short Health Anxiety Inventory (SHAI), a Revised Version of the Diabetes Quality of Life Questionnaire (DQLQ), and a General Medication Adherence Scale (GMAS) were used to investigate secondary outcomes. Repeated measure ANOVA was used to analyze the results.
Results
The findings indicated that patients who received CBT got a significant reduction in their diabetes distress F(1,60) = 222.710, P < 0.001, η2 = .788), depressive symptoms F(1,60) = 94.436, P < 0.001, η2 = .611), health anxiety F(1,60) = 201.915, P < .0.001, η2 = 771), and a significant improvement in their quality of life F(1,60) = 83.352, P < 0.001, η2 = .581), treatment adherence F(1,60) = 67.579, P < 0.001, η2 = .566) and physical activity schedule F(1,60) = 164.245, P < .0.001, η2 = .736 as compared to the patients in waitlist control condition.
Conclusion
It is concluded that cognitive behavior therapy is an effective and promising intervention for depressive symptoms, diabetes distress, and health anxiety which also helps the person to promote quality of life, treatment adherence and physical activity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diabetes or diabetes mellitus is a metabolic disease that interferes with the human body’s ability to process and absorb glucose. It is the seventh leading cause of death, and about 422 million people live with diabetes worldwide (WHO 2020). The current scenario estimates that it will rise by 25% within 10 years to 454 million and 51% within 25 years to 548 million [1]. In Pakistan, the prevalence of type 2 diabetes is 13.7% higher in urban areas [2]. According to National Diabetes Federation (2019), about 19 million in Pakistan from age 20 to 79 have been suffering from diabetes. Type-II diabetes is the most commonly occurring type that accounts for up to 90% of the total [3].
Diabetes could be a reason of a variety of psychological disturbances in the people suffering from it. One such psychological disturbance is called diabetes distress (DD). DD is a big problem that accompanies emotional disturbances, stress, guilt feelings, and avoidance of treatment [4]. It is more frequent among patients with type II diabetes mellitus [5]. The prevalence of DD globally is around 45% which is quite high as it is a predictor of clinical outcomes among patients of T2DM [6] Poor self-care, poor self-management, and a reduced treatment adherence among patients with diabetes are some of the negative treatment outcomes associated with DD [7]. Depression is a mental state characterized by a pessimistic sense of inadequacy and lack of activity, usually occurring a i when the intensity of distress becomes high as frequent and unmanaged distress can sometimes lead to full-blown depression [8]. Many factors can lead to depression such as psychological, social, and biological and it can also present itself as a comorbid condition of chronic medical illnesses such as diabetes, [9]. Having a depressive disorder increases the risk of new-onset diabetes mellitus, and patients with diabetes mellitus also have a higher likelihood of developing depressive symptoms. Therefore, depression is an observed common factor among diabetic patients and it frequently co-occurs [10].
Health anxiety (HA) is another factor which causes distress; it occurs when an individual misinterprets his bodily sensations or changes as the indicators of a life-threatening illness (Asmundson & Taylor, [11]). HA is the core of many psychological illnesses, ranging from low to severe [7]. DD leads to HA because patients with chronic illnesses such as diabetes commonly experience fears of illness or symptoms recurring or worsening. It leads to lower adherence to treatment, fewer positive health behaviors, and increased medical costs [12]. HA is higher among patients with diabetes [13].
Treatment adherence is usually described as the patient’s compliance with the prescribed medication [14]. Treatment adherence is necessary to control diabetes and to foreclose death rate and severe morbidity. Adherence to treatment in diabetes helps maintain proper health and reduces diabetes-related complications. Albeit, some psychological factors may compromise compliance and adherence of patients with diabetes mellitus [14]. Quality of life (QOL) refers to how much an individual is healthy, comfortable, and can participate in different events of life or can enjoy life events. It is an important variable to be considered in any healthcare research as it measures life in terms of participation in life not in terms of lived years [15]. Individuals with high quality of life usually have an improved metabolic control of their disease as compared to those with lower quality of life, whereas, patients with higher blood glucose also have a lower health-related quality of life [16].
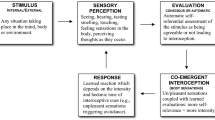
Cognitive Behavior therapy (CBT) is a form of psychological intervention which emphasizes the current state of affairs and, usually, it is a time-bound mode of therapy [17]. CBT uses the cognitive-behavioral model, which taps the thought patterns of an individual that are triggered by their behavioral and physiological reactions to different stimuli [18]. Cognitive behavior therapy does not merely work for the management of psychiatric disorders, recent decades of research have provided evidence of the effectiveness of CBT with many different chronic illnesses and their related psychological issues; CBT also helps reduce depression and anxiety among patients with diabetes [19, 20].
Recent studies show that, in Asian countries, there is a need for improved mental health screening and treatment in diabetes care (Karla et al., 2020). CBT works effectively with depression and increases treatment adherence in diabetes patients as CBT is an evidence-based treatment therapy for depression as a comorbid condition with diabetes [21].
CBT has the potential to addresses the emotional problems of patients with T2DMas it has been practiced with T2DM to reduce depressive symptoms [22]. CBT has been substantiated to be an effective treatment intervention for diabetes distress [23], reduction of emotional problems [24], improvement in adherence [25] and for control of glucose level through adherence [26].
This current study aimed to examine the effectiveness of CBT through experimental and waitlist control conditions with type 2 diabetes patients. We hypothesized that CBT will effectively reduce diabetes distress and other depressive symptoms, will effectively deal with health-related anxiety concerns and distress due to diabetes, and will improve the patients’ treatment adherence and quality of life.
Research design and methods
Study design
The current research is a prospective randomized control trial (RCT) in which we assessed the effectiveness of CBT using EXP and WLC conditions with T2DM patients using pre-and post-test measures. Outcome measures were obtained at the baseline and post-interventions. The participants were taken from different public and private hospitals of the district Faisalabad, Punjab, Pakistan. The study protocol was approved by the Institutional Review Board (IRB), Government College University, and Faisalabad, Pakistan (i.e., Ref.No. GCUF/ERC/2270). Furthermore, the protocol was also registered and approved by the Thai Clinical Trial Registry (i.e., TCTR20210703002 on 03 July, 2021) with the following URL: https://www.thaiclinicaltrials.org/show/TCTR20210703002).
Participants
Consultant medical doctors first diagnosed patients with T2DM after evaluating them using medical evaluations from reliable laboratories (i.e., Agha Khan University Laboratories & Shaukat Khanum Memorial Trust Laboratories) at outpatient settings of different hospitals. and. Then the diagnosed participants were referred to us for the inclusion in our study. These participants first went through our clinical psychologists for psychological assessment and evaluation. The number of needed participants was calculated through G-Power software using the effect size (f) = 0.20, α = 0.05, power (1-β error prob.) =0.95 with actual power = 0.96 which gave us the total required sample size of56 (experimental and waitlist control conditions combined) [27]. Therefore, in this RCT, 130 participants were initially enrolled for eligibility assessment, 90 patients qualified the inclusion criteria, and they were allocated to two different treatment conditions (i.e., EXP = 45 & WLC = 45) through random assignment (see Fig. 1). A total of 62 patients completed all the required procedures of the present study. Participants’ age range was 23 to 50 years.
Inclusion and exclusion criteria
In this RCT, people diagnosed with Type-II Diabetes Mellitus (T2DM) availing outpatient treatment facilities under consultant practitioners in different hospitals of Faisalabad were recruited. Participants who achieved mean item score of 3 or above (moderate distress) on DDS and were belonging to mild depressive symptoms category or higher on PHQ were included and allocated for two treatment conditions. Only those patients were included who had been diagnosed at-least 6-month ago (and at most 10 years ago) with T2DM and had been experiencing depressive symptoms for at-least two-weeks. Respondents who were suffering from major depressive disorder, persistent mood disorder and health anxiety disorder were excluded from the study as the protocol of their treatment was out of the scope of the present study. Patients were taken from all socioeconomic statuses. Participants with Type-I diabetes mellitus, duration of illness of less than 6 months and more than 10 years, not availing any medical treatment or receiving inpatient treatment were excluded from the study. Participants with any physical disability, severe physical/head injury, or undergoing any surgical treatment were also excluded from the study. Participants who did not sign the consent form or did not complete all the research procedures were also excluded from the study.
Assessment and screening
A clinical psychologists conducted in-depth clinical interviews with patients in one-on-one settings. In the interview, the central focus was given to exploring the current presenting complaints, duration of illness, nature of the problems, and symptoms severity in terms of psychiatric problems. In order to cross check, the symptoms severity baseline measures, i.e., DDS (for diabetes distress) and PHQ (for depressive symptoms severity) were administered. Moreover, patients under treatment and experiencing T2DM for the last 6 months and experiencing depressive symptoms more than 2 weeks were selected for this RCT. Structured Clinical Interview for Diagnosis (SCID) was used to screen out any patients suffering from major depressive disorder, persistent mood disorders and health anxiety disorder and such patients were excluded. They were excluded from this RCT because they were referred for further psychological evaluation and treatment (i.e., psychiatric medication if need and extensive psychotherapy along with T2DM treatment). Furthermore, participants who achieved mean item score of 3 or above (moderate distress) on DDS and were belonging to mild depressive symptoms category or higher on PHQ were considered eligible for this RCT because they had diabetes distress and depressive symptoms due to T2DM and they were coming for treatment on regular bases. They were then randomly assigned to the two different treatment conditions.
Procedure
Participant enrollment started on the 10th of July 2021, and trial completed on the 31st of December 2021, at different hospitals in the Faisalabad. Initially, participants’ baseline assessment was completed in the hospital’s outpatient setting. After qualifying the eligibility criteria, participants were interviewed and were invited for intake at the psychoogical clinic. Participants who met the study criteria and gave written informed consent to participate in the study were registered for this randomized clinical trial. Participants assigned to treatment conditions were assessed (pre-assessment), and at treatment completion, they were again assessed (post-assessment) with the duration of 4 months between the two assessments. We provided 8 to 10 CBT-based therapeutic sessions based on a particular agenda and goal (see interventions). Participants allocated to waitlist control were also assessed at pre-and post-assessment stages with the same time interval allocated for the experimental group.
Randomization
We randomly assigned participants to treatment conditions so that both conditions were with similar and matchable group characteristics. Furthermore, all the patients were blinded with respect to the identification of the group they were assigned to. We told the participants that they were being randomized to receive psychological treatment, and its goal was to reduce their level of distress and depressive symptoms.
Interventions
During the initial briefing, the participants were guided about the advantages of adherence and disadvantages of non-adherence, the importance of quality of life [23], reduced depression and anxiety [28], and also about improving their problem-solving abilities [29] to improve physiological functioning and to reduce stress and mood disturbance [30]. Then CBT was administered. CBT is an evidence-based intervention designed to address cognitive and behavioral problems efficiently. The CBT-based treatment plan was structured and delivered individually to each patient. Treatment was completed in 16 weeks, and therapeutic session frequency was one session in 10–12 days intervals with 45–60 minutes. In the initial sessions of the treatment, the therapist discussed about the process of treatment sessions, frequency, duration, the role of the therapist and client, the significance of patients’ active participation, and homework assignments. CBT protocol was structured according to Beck [31], Hilliard et al. [32] and Hood et al. [33]. The main components of the CBT were psychoeducation, cognitive conceptualization, adherence training, activity scheduling, problem-solving, improving coping strategies, muscle relaxation and imagery, and, lapse and relapse prevention (see supplementary material). The therapist asked the patients to come with a diary to write down important notes, daily homework assignments, and activity schedules and to write the current issues for discussion in the upcoming session. We received written feedback after each session. Almost all the patients easily understood the therapeutic process, therapy concept, content, and the mechanism for change.
Waitlist control condition
Participants allocated to the waitlist control condition received no treatment for 16 weeks. Their pre-and post-assessment was completed with the same time interval as that of the experimental group.
Assessment measures
Demographic information
The demographic form that was used comprised of personal information from patients; such as age, education, socioeconomic status, family system, total family members, marital status, duration of illness, and the hospital name. In addition, the information related to their illness such as glucose level, duration of treatment, type of treatment, the dose of insulin, hypertension, obesity family history, was also asked in the demographic form. This form was used for further analysis and to tabulate results.
Primary outcomes measures
Diabetes distress scale (DDS-17) [34]
Diabetes Distress Scale DDS-17 is an instrument used to assess the level of distress among diabetes patients. It consists of 17 items. It has a six-point Likert scale where 1 means no problem and 6 indicates serious issues or problems. It has four subscales emotional-related distress, physician-related distress, regimen-related distress, and interpersonal-related distress. A mean item score of 3 or above is considered worthy of clinical attention (moderate distress). Its reliability was reported at 0.87.
The patient health questionnaire-9 (PHQ) [35]
The PHQ is a nine-item depression scale. It is based directly on the diagnostic criteria for major depressive disorders in the Diagnostic and Statistical Manual Fifth Edition. The PHQ scores range from 0 to 3 from not at all to nearly every day, respectively. It has five ranges of severity, i.e., minimal depressive symptoms, mild depressive symptoms, moderate depressive symptoms, moderately severe depressive symptoms, and severe depressive symptoms. The scores on this self-report measure do not provide a diagnosis on their own as a diagnosis necessitates a detailed clinical investigation. PHQ reliability estimation is 0.89.
Secondary outcomes measures
Short health anxiety inventory (SHAI) [36]
The SHAI is an instrument widely used to assess anxiety about the health status of a person. It consists of 18 items. Items assess the worries about health, awareness of bodily sensations or changes, and feared consequences of having an illness. The SHAI has demonstrated good reliability 0.86 and criterion validity 0.8.
Revised version of diabetes quality of life questionnaire (RV-DQOL) [37]
The RV-DQOL instrument is used to measure the quality of life among diabetes patients. It consists of 13 items and has three domains: satisfaction, impact, and worry. It has a 5-point Likert scale from “no impact/no worries” to “always satisfied/always affected.” The reliability of DQOL is 0.92 and 0.84, for worry, 0.98 and 0.60, for faction and, for “impact,” 0.99 and 0.57, respectively.
General medication adherence scale (GMAS) [38]
The GMAS is widely used to determine adherence among patients with chronic illness and is used for diabetes patients. This scale has three subscales; and each subscale measures a specific dimension of non-adherence., patient behavior-related non-adherence, additional diseases and pill burden-related non-adherence, and, cost-related non-adherence. It measures the overall adherence to medication as well. It has reliability estimation of 0.84, and test-re-test reliability of 0.99 and content validity of 0.80.
International physical activity questionnaire (IPAQ) [39]
The IPAQ measures the amount of physical activity performed over the past 7-day period. The IPAQ includes questions about the time spent engaging in vigorous physical activities, moderate physical activities, and walking. The IPAQ is a reliable (p = 0.76) and valid measure (concurrent = 0.58; criterion = 0.30).
Statistical analysis
Descriptive statistics (Mean & SD) was used to calculate sample demographic characteristics, whereas, group characteristics were compared at pre-test using χ2 and t-test to compare variables. A repeated measures ANOVA statistic was used for the assessment time (pre- versus post-test) to evaluate the effects and benefits of the interventions (within-group effects). Frequency distribution statistics were used to find out the severity of the symptoms. An alpha of .05 was used for all analyses, and p-value <.01was submitted to Bonferroni correction using IBM SPSS Statistics (Version 25).
Results
Recruitment and attrition
A total of 130 participants were recruited, and n = 90 met the inclusion criteria. Participants were equally divided into experimental (EXP) = 45(50%) and waitlist control (WLC) = 45(50%), and they were statistically analyzed (see Fig. 1). There were no significant differences found between EXP vs. WLC among the demographic characteristics; such as age, gender, education, glucose level, family system, occupation, socioeconomic status, duration of illness, types of treatment, duration of treatment, checkup, hypertension, BMI, family history and obesity respectively (see Table 1).
Primary and secondary outcomes
We found a significant mean difference between EXP and WLC conditions in post-testing scores on PHQ which indicates CBT substantially decreased depressive symptoms among patients with T2DM. Findings indicate that significant mean differences were found between EXP and WLC groups on SHAI which indicates that the CBT played a 77% role in reducing the level of health anxiety in the experimental group. Furthermore, significant mean differences were found between baseline and post-testing scores on the scale of EBS, PDS, RDS, IDS and overall DDS between EXP and WLC which indicates CBT reduced 63% emotional burden, 68% physician burden, 66% of regimen distress, 53% of interpersonal distress and 76% of overall diabetes distress of EXP group. Similarly, EXP group was found to be significantly different as compared to WLC on PBNA, ADPB, CRNA and overall GMAS which shows that CBT also improved adherence to treatment; such as: 48% patient behavior related non-adherence, 42% additional disease and pill burden describe non-adherence, 51% cost related non adherence and 57% over all general medication adherence to treatment. Analysis reveals a significant difference between EXP and WLC after CBT on SATS, IMPS, WORS, and overall DQLS which shows CBT sessions improved satisfaction to the degree of 41%, impact to the degree of 43%, non-worried behavior to the degree of 41%, and, overall diabetes patients’ quality of life to the degree of 58%. Furthermore, findings show that CBT produced a significant difference in changing lifestyle as compared to WLC on WALS, MPAS, VPAS and IPAQ which shows that patients with T2DM improved their quality of life after getting CBT sessions; such as: walking activities to the degree of 69%, moderate physical activities to the degree of 23%, vigorous physical activities to the degree of 33%, and overall daily physical activities to the degree of 73% (see Table 2).
The analysis reveals that scores significantly decreased throughout the treatment among the experimental group on PHQ, HAI, and DDS, and the group’s scores enhanced on MAS. CBT played an influential role in addressing depressive symptoms, health-related anxiety, and diabetes distress. On the other hand, CBT played a supportive role in increasing treatment adherence (see Fig. 2).
Findings showed a significant improvement in symptoms of depression in the EXP group. The score in the pre-vs. post of the EXP group is as follows: minimal depressive symptoms 0% vs. 3.7%, mild depressive symptoms 7.4% vs.37.1%, moderate depressive symptoms 40.8% vs. 59.3%; this indicates that CBT significantly reduced depressive symptoms. Similarly, at pre-assessment, the moderate-severe depressive symptoms were in 33.4% of the participants, and severe depressive symptoms were in 18.5% of the participants which got reduced due to CBT at post-assessment, while no significant change was observed in the waitlist control group (see Table 3).
Findings show that CBT significantly improved adherence to treatment among individuals with T2DM. Post-testing analysis reveals that the individuals from the EXP group got an improvement in their treatment adherence considerably. For example, high adherence, which was at 2(7.41%) at baseline, increased 10(37.04%), good adherence, which was at 3(11.12%) at baseline, improved to 12(44.45%), partial adherence, which was at 13(46.15%) at the baseline, shrank to 3(11.12%) as people moved to higher categories, and, low adherence, which was at 6(22.23%) at baseline, again shrank to 2(7.41%) as people moved to higher categories. In the case of WLC, no significant difference was observed, such as, high adherence at baseline had 3(8.57%) participants and at post-analysis stage there were 2(5.71%); good adherence at baseline had 6(17.14%) participants and at post-analysis stage there were 5(14.29%); partial adherence at baseline had 15(42.86%) participants and at post-analysis stage there were 18(51.43%); low adherence at baseline had 9(25.71%) participants and at post-analysis stage there were 6(17.14%); whereas, poor adherence at baseline had 2(5.71%) participants and at post-analysis stage there were 4(11.43%) (see Table 4).
Discussion
Our findings present the effectiveness of CBT for patients with T2DM in order to produce substantial improvement on multiple psychophysiological health outcomes. CBT has been widely used to treat patients’ psychological problems with diabetes [23]. Overall findings of our study show substantial improvement in diabetes distress, health anxiety, depression, quality of life, and medication adherence among the experimental group. Whereas, no difference was found in the pre- and post-testing in the control group.
Our findings show that CBT effectively addresses patients’ psychological problems with diabetes mellitus. These findings are consistent with the findings of the previous studies. CBT-based interventions help patients by bringing about psycho-education, development of better understanding and upping the motivation to of overcome and manage negative automatic thoughts, by regulating emotions, and rectifying negative beliefs [40, 41]. In our findings, CBT effectively reduced psychological distress and improved emotional and behavioral outcomes as well as medication adherence [42]. Significant difference between baseline and outcomes assessment scores in the experimental group report that CBT was found an evidence-based treatment intervention to reduce diabetes distress and depressive symptoms among patients with T2DM [40].
Moreover, the analysis reveals that CBT effectively helped the patients to develop a positive attitude toward life and promoted their functional outcomes through skill training [43, 44]. This reflects that CBT is an effective intervention to address depressive symptoms among T2DM [41]. Depression is a ubiquitous affliction that affects patients with diabetes. That’s why it is necessary to encounter this, and for this purpose, CBT is a strong and reliable treatment option to follow [43].
Furthermore, our analysis reveals that CBT significantly decreases health anxiety among T2DM patients in our study [45]. Health anxiety is common among patients with diabetes. Patients with DM have a propensity for developing apprehension about their illness, that’s why it was reported in our sample that after receiving the intervention, participants’ level of anxiety was reduced [46]. This maybe so because the intervention was aimed to change the thought pattern into adaptive thinking pattern in T2DM patients.
In our study. CBT was tested to improve the quality of life among patients with T2DM because diabetes negatively affects quality of life [47]. There was a significant difference between pre- and post- test scores; participants in the experimental group showed higher quality of life. The experimental group’s post-testing was remarkably different from the control group as their quality of life improved after the intervention. However, the control group didn’t significantly differ because they didn’t receive the intervention [48].
The study findings also indicate that CBT improved medication adherence. Medication adherence was focused upon because it is strongly associated with many complications of T2DM [49]. In our study, medication adherence was low at baseline screening because many patients were not taking medication appropriately. They were less likely to seek medication and held an unhealthy diet plan that led to poor glycmeic control. Hence, we used CBT to manage medication adherence to overcome this issue of the patients with T2DM, and substantial improvement was reported in the experimental group. However, no difference was found in the control group.
Our findings indicate that patients with diabetes mellitus showed more physical activity after having CBT; these findings are consistent with the existing research [26]. Physical activity accounts for maximum improvement in diabetic patients because it enhances self-care behavior, diminishes glucose levels, and improves health status. It is important to address the physical activity among T2DM to improve their lifestyle and to balance their glucose and insulin levels to prevent them from facing damaging health outcomes. For this, researchers can use CBT and other different motivational programs to reduce the level of inactivity among diabetes patients [50].
Conclusion
It is concluded that CBT produced substantial improvement among patients with T2DM having diabetes distress and depressive symptoms. It has also been supported that CBT is an effective and evidence-based treatment to address diabetes distress, depressive symptoms, and health-related anxiety. CBT also improves treatment adherence and quality of life among diabetic patients. This also helps the patients to manage daily routines, sustain motivation for treatment and develop a positive attitude toward life. Finally, CBT increases treatment adherence in patients with T2DM helping being about a rapid recovery process.
Limitations of the study
The current study has some limitations. First, only patients with Type II diabetes mellitus were taken in the study. Second, patients were taken only from outpatient departments. Third, major focus was given only to diabetes distress, depressive symptoms, health anxiety, medication adherence and physical activities; many other factors; such as, patients’ coping mechanisms, social and emotional support systems, and others comorbid medical conditions, diagnosed psychiatric disorders and aging factors, were not investigated in this study. Fourth, the cognitive behavior therapy session was mainly designed for patients with T2DM having psychiatric problems, not psychiatric disorders. Fifth point I that we could not enroll a large-enough number of participants (due to Covid-19) in this RCT that come from different age groups, especially above age 50, who might have more diabetes problems. Lastly, this RCT does not say anything about the patients who have a history of chronic diabetes greater than 10 years. Nonetheless, if future researches target the aforesaid areas, it will be a helpful contribution to the literature as well as to the generalizability of the results.
Recommendation and implication of the study
This paper provides contributions to fill the knowledge gap in this ignored area of research. This paper also recommends that future researchers should check the effectiveness of CBT for patients with T1DM and T2DM having severe depressive and anxiety-related disorders. This study provides valuable background for mental health practitioners to treat and develop the guidelines and protocol for patients with diabetes mellitus and other chronic illnesses such as diabetes, cancer, HIV/AIDS. Cognitive behavior therapy played a substantial role in developing patient insight and motivation, so, it is also recommended that other practitioners should carry out qualitative studies on the variables of this research in order to know the qualities and limitations of this strategy and give even more suitable strategies to deal with the problems faced with T2DM within the field of cognitive behavior therapy.
Availability of data and materials
The dataset generated and/or analyzed during the present study are not publicly available because no permission was taken from the participants and the hospital administration where the study was conducted. The datasets are available from the corresponding authors on a special request.
Abbreviations
- CBT:
-
Cognitive Behavior Therapy
- T2DM:
-
Type 2 Diabetes Mellitus
- PHQ:
-
Patient Health Questionnaire-9
- SHAI:
-
Short Health Anxiety Inventory
- DD:
-
Diabetes Distress
- HA:
-
Health Anxiety
- QOL:
-
Quality of Life
- EXP:
-
Experimental group
- WLC:
-
Waitlist Control
- EBS:
-
Emotional Burden Subscale
- PDS:
-
Physician Distress Subscale
- RDS:
-
Regimen Distress Subscale
- IDS:
-
Interpersonal Distress Subscale
- DDS:
-
Diabetes Distress Scale
- PBNA:
-
Patient Behavior related Non-Adherence
- ADPB:
-
Additional Disease and Pill Burden Related Non-Adherence
- CRNA:
-
Cost Related Non-Adherence
- GMAS:
-
General Medication Adherence Scale
- SATS:
-
Satisfaction Subscale
- IMPS:
-
Impact Subscale
- WORS:
-
Worry Subscale
- DQLSL:
-
Diabetes Quality of Life Scale
- WALS:
-
Walking Subscale
- MPAS:
-
Moderate Physical Activity Subscale
- VPAS:
-
Vigorous Physical Activity Subscale
- IPAQ:
-
International Physical Activity Questionnaire.
References
Saeedi P, Petersohn I, Salpea P, Malanda B, Karuranga S, Unwin N, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the international diabetes federation diabetes atlas. Diabetes Res Clin Pract. 2019;157:107843.
Aamir AH, Ul-Haq Z, Mahar SA, Qureshi FM, Ahmad I, Jawa A, et al. Diabetes prevalence survey of Pakistan (DPS-PAK): prevalence of type 2 diabetes mellitus and prediabetes using HbA1c: a population-based survey from Pakistan. BMJ Open. 2019;9:e025300.
Mustapha S, Mohammed M, Azemi AK, Jatau AI, Shehu A, Mustapha L, et al. Current status of endoplasmic reticulum stress in type II diabetes. Molecules. 2021;26:4362.
Fisher L, Polonsky WH, Hessler D. Addressing diabetes distress in clinical care: a practical guide. Diabet Med. 2019;36:803–12.
Lee AA, Heisler M, Trivedi R, Obrosky DS, Mor MK, Piette JD, et al. Diabetes distress among dyads of patients and their health supporters: links with functional support, metabolic outcomes, and cardiac risk. Ann Behav Med. 2021;55:949–55.
Parsa S, Aghamohammadi M, Abazari M. Diabetes distress and its clinical determinants in patients with type II diabetes. Diabetes Metab Syndr. 2019;13:1275–9.
Bozkurt E, Kurtses Gürsoy B, Atay E, Bilir A, Kaynarca Ö. Perceived stress level and health anxiety during COVID-19 pandemic period in patients with diabetes mellitus and hypertension: A prospective cross-sectional study. J Surg Med. 2021;5:785–90.
Kaur H, Scholl JC, Owens-Gary M. Depression and diabetes in workers across the life span: addressing the health of America’s workforce—behavioral risk factor surveillance system, 2014–2018. Diabetes Spectr. 2021;35(2):198–206. https://doi.org/10.2337/ds21-0022.
Gold SM, Köhler-Forsberg O, Moss-Morris R, Mehnert A, Miranda JJ, Bullinger M, et al. Comorbid depression in medical diseases. Nat Rev Dis Primer. 2020;6:1–22.
Khan ZD, Lutale J, Moledina SM. Prevalence of depression and associated factors among diabetic patients in an outpatient diabetes clinic. Psychiatry J. 2019;2019:1–6.
Asmundson GJG, Taylor S. How health anxiety influences responses to viral outbreaks like COVID-19: what all decision-makers, health authorities, and health care professionals need to know. J Anxiety Disord. 2020;71:102211.
Lebel S, Mutsaers B, Tomei C, Leclair CS, Jones G, Petricone-Westwood D, et al. Health anxiety and illness-related fears across diverse chronic illnesses: A systematic review on conceptualization, measurement, prevalence, course, and correlates. PLoS One. 2020;15:e0234124.
Sharma K, Dhungana G, Adhikari S, Bista Pandey A, Sharma M. Depression and anxiety among patients with type II diabetes mellitus in Chitwan medical college teaching hospital. Nepal Nurs Res Pract. 2021;2021:e8846915.
AlShayban DM, Naqvi AA, Alhumaid O, AlQahtani AS, Islam MA, Ghori SA, et al. Association of Disease Knowledge and Medication Adherence among out-Patients with Type 2 diabetes mellitus in Khobar, Saudi Arabia. Front Pharmacol. 2020;11:60.
Abdollahi L, Mirghafourvand M, Babapour JK, Mohammadi M. Effectiveness of cognitive-behavioral therapy (CBT) in improving the quality of life and psychological fatigue in women with polycystic ovarian syndrome: a randomized controlled clinical trial. J Psychosom Obstet Gynecol. 2019;40:283–93.
Chen Q, Yang G, Lin S, Li M, Liu Z, Fu Y, et al. The effects of mindfulness-based stress reduction therapy combined with intensive education on the effectiveness of the care and the awareness rate in patients with arthritis and diabetes. Am J Transl Res. 2021;13:3190–7.
Purba JM, Empraninta HE. The effect of cognitive behavioral therapy on self-management and self-care behaviors of type 2 diabetes mellitus patients. J Keperawatan Soedirman. 2021;16;20–4.
Chand SP, Kuckel DP, Huecker MR. Cognitive behavior therapy. In: StatPearls. Treasure Island. FL: StatPearls Publishing; 2021.
Tunsuchart K, Lerttrakarnnon P, Srithanaviboonchai K, Likhitsathian S, Skulphan S. Benefits of brief group cognitive behavioral therapy in reducing diabetes-related distress and HbA1c in uncontrolled type 2 diabetes mellitus patients in Thailand. Int J Environ Res Public Health. 2020;17:5564–74.
Zhang ZP, Premikha M, Luo M, Venkataraman K. Diabetes distress and peripheral neuropathy are associated with medication non-adherence in individuals with type 2 diabetes in primary care. Acta Diabetol. 2021;58:309–17.
Bukhsh A, Khan TM, Nawaz MS, Ahmed HS, Chan KG, Lee L-H, et al. Association of diabetes-related self-care activities with glycemic control of patients with type 2 diabetes in Pakistan. Patient Prefer Adherence. 2018;12:2377–85.
Abbasi Asl M, Rahmati-Najarkolae F, Dowran B. Comparison of the effectiveness of acceptance and commitment therapy (ACT) and cognitive-behavioral therapy (CBT) on psychological hardiness, caring behavior and coping strategies in patients with type 2 diabetes. J Mil Med. 2020:22.
Andreae SJ, Andreae LJ, Richman JS, Cherrington AL, Safford MM. Peer-delivered cognitive behavioral training to improve functioning in patients with diabetes: A cluster-randomized trial. Ann Fam Med. 2020;18:15–23.
Ciharova M, Furukawa TA, Efthimiou O, Karyotaki E, Miguel C, Noma H, et al. Cognitive restructuring, behavioral activation and cognitive-behavioral therapy in the treatment of adult depression: A network meta-analysis. J Consult Clin Psychol. 2021;89:563–74.
Yang X, Li Z, Sun J. Effects of Cognitive Behavioral Therapy–Based Intervention on Improving Glycaemic, Psychological, and Physiological Outcomes in Adult Patients With Diabetes Mellitus: A Meta-Analysis of Randomized Controlled Trials. Front Psychiatry. 2020;11:711.
Pan X, Wang H, Hong X, Zheng C, Wan Y, Buys N, et al. A group-based community reinforcement approach of cognitive behavioral therapy program to improve self-care behavior of patients with type 2 diabetes. Front Psychiatry. 2020;11:719.
Faul F, Erdfelder E, Buchner A, Lang A-G. Statistical power analyses using G* power 3.1: tests for correlation and regression analyses. Behav Res Methods. 2009;41:1149–60.
Xu C, Dong Z, Zhang P, Chang G, Xiang Q, Zhang M, et al. Effect of group cognitive behavioural therapy on psychological stress and blood glucose in people with type 2 diabetes mellitus: A community-based cluster randomized controlled trial in China. Diabet Med. 2021;38:e14491.
Izgu N, Gok Metin Z, Karadas C, Ozdemir L, Metinarikan N, Corapcıoglu D. Progressive muscle relaxation and mindfulness meditation on neuropathic pain, fatigue, and quality of life in patients with type 2 diabetes: A randomized clinical trial. J Nurs Scholarsh. 2020;52:476–87.
Anaabawati MA, Rumahorbo H, Pujiastuti RSE. Effectiveness of cognitive behavioral therapy and muscle relaxation on fasting blood sugar levels among type 2 diabetes mellitus: A systematic review. Int J Nurs Health Serv IJNHS. 2021;4:153–61.
Beck JS. Cognitive behavior therapy. 3rd ed: Basics and Beyond. Guilford Publications; 2020.
Hilliard ME, Riekert KA, Ockene JK, Pbert L. The handbook of health behavior change: Springer Publishing Company; 2021.
Hood KK, Raymond JK, Adams RN, Tanenbaum ML, Harris MA. Diabetes management behaviors: the key to optimal health and quality of life outcomes: Springer Publishing Company; 2021.
Polonsky WH, Fisher L, Earles J, Dudl RJ, Lees J, Mullan J, et al. Assessing psychosocial distress in diabetes: development of the diabetes distress scale. Diabetes Care. 2005;28:626–31.
Ahmad S, Hussain S, Akhtar F, Shah FS. Urdu translation and validation of PHQ-9, a reliable identification, severity and treatment outcome tool for depression. J Pak Med Assoc. 2018;68:5.
Salkovskis PM, Rimes KA, Warwick HMC, Clark DM. The health anxiety inventory: development and validation of scales for the measurement of health anxiety and hypochondriasis. Psychol Med. 2002;32:843–53.
Bujang MA, Adnan TH, Mohd Hatta NKB, Ismail M, Lim CJ. A revised version of diabetes quality of life instrument maintaining domains for satisfaction, impact, and worry. J Diabetes Res. 2018;2018:e5804687.
Naqvi AA, Hassali MA, Rizvi M, Zehra A, Iffat W, Haseeb A, et al. Development and validation of a novel general medication adherence scale (GMAS) for chronic illness patients in Pakistan. Front Pharmacol. 2018;9:1124.
Craig CL, Marshall AL, Sjöström M, Bauman AE, Booth ML, Ainsworth BE, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35:1381–95.
Li C, Xu D, Hu M, Tan Y, Zhang P, Li G, et al. A systematic review and meta-analysis of randomized controlled trials of cognitive behavior therapy for patients with diabetes and depression. J Psychosom Res. 2017;95:44–54.
Zakhour S, Nardi AE, Levitan M, Appolinario JC. Cognitive-behavioral therapy for treatment-resistant depression in adults and adolescents: a systematic review. Trends Psychiatry Psychother. 2020;42:92–101.
Tunsuchart K, Lerttrakarnnon P, Srithanaviboonchai K, Likhitsathian S, Skulphan S. Benefits of brief group cognitive behavioral therapy in reducing diabetes-related distress and HbA1c in uncontrolled type 2 diabetes mellitus patients in Thailand. Int J Environ Res Public Health. 2020;17:5564.
Feltz-Cornelis C van der, Allen SF, Holt RIG, Roberts R, Nouwen A, Sartorius N. Treatment for comorbid depressive disorder or subthreshold depression in diabetes mellitus: systematic review and meta-analysis. Brain Behav 2021;11:e01981.
Lu X, Yang D, Liang J, Xie G, Li X, Xu C, et al. Effectiveness of intervention program on the change of glycaemic control in diabetes with depression patients: A meta-analysis of randomized controlled studies. Prim Care Diabetes. 2021;15:428–34.
Newby JM, McElroy E. The impact of internet-delivered cognitive behavioural therapy for health anxiety on cyberchondria. J Anxiety Disord. 2020;69:102150.
Axelsson E, Hedman-Lagerlöf E. Cognitive behavior therapy for health anxiety: systematic review and meta-analysis of clinical efficacy and health economic outcomes. Expert Rev Pharmacoecon Outcomes Res. 2019;19:663–76.
Wu C, Ge Y-L, Zhang X-Y, Liu M-C, Heng C-N, Zhang L-Y, et al. The influence of hypoglycemia on the specific quality of life in type 2 diabetes mellitus: a comparative cross-sectional study of diabetics with and without hypoglycemia in Xi’an. China Health Qual Life Outcomes. 2021;19:151.
Taherpour R, Hatami H-R, Ahadi H, Zakeripour G-R, Kalhorniya GM. The impact of cognitive-behavioral group therapies and positive treatment on the psychological hardiness and quality of life in women suffering from T. Women Fam Cult-Educ. 2021;15:151–68.
Al-Qerem W, Jarab AS, Badinjki M, Hyassat D, Qarqaz R. Exploring variables associated with medication non-adherence in patients with type 2 diabetes mellitus. PLoS One. 2021;16:e0256666.
Huffman JC, Golden J, Massey CN, Feig EH, Chung W-J, Millstein RA, et al. A positive psychology-motivational interviewing program to promote physical activity in type 2 diabetes: the BEHOLD-16 pilot randomized trial. Gen Hosp Psychiatry. 2021;68:65–73.
Acknowledgments
We thank the participants who participated in the study and spent precious time. We also thank the hospital staff and medical professionals who support us during the study.
Disclosure
None.
Funding
There was no funding for this study.
Author information
Authors and Affiliations
Contributions
Q.A. conceptualized, designed and supervised the manuscript, as well as reviewed and edited the final draft of the manuscript. S.L. prepared the study protocol, collected data, scrutinized the data, and conducted therapeutic sessions. H.A.H. helped in trial registration, analyzed the data, interpreted the results, and planned treatment. S.S. helped with data arrangement, manuscript write-up, and edited the manuscript. U. S, collected data, prepared SPSS sheet, M.S. helped in patients’ scrutiny, allocation, and care. Z.R. and W.W. helped in data collection, preparation, and therapeutic sessions. All authors reviewed the manuscript. The author(s) read and approved the final manuscript.
Authors’ information
Q.A- Assistant Professor-Clinical Psychology, Department of Applied Psychology, Government College University Faisalabad, Pakistan. S.L-Final year MS Clinical Psychology student, Department of Applied Psychology, Government College University Faisalabad, Pakistan. H.A.H- Assistant Professor, Institute of Clinical Psychology, University of Karachi, S.S- Associate Professor, Institute of Clinical Psychology, University of Karachi, Pakistan, U.S. Lecturer, Department of Psychology, Government College Women University Sialkot, M.S- PhD Scholar at Department of Applied Psychology, Government College University Faisalabad, Pakistan. Z. R and W. W- Assistant Professor of psychiatry, Dow university of medical sciences.
Corresponding author
Ethics declarations
Ethics approval and informed consent
The study protocol was approved by the Institutional Review Board (IRB), Government College University, and Faisalabad, Pakistan (i.e., Ref.No. GCUF/ERC/2270). Furthermore, the protocol was also registered and approved by the Thai Clinical Trial Registry (i.e., TCTR20210703002 on 03 July, 2021, with URL: https://www.thaiclinicaltrials.org/show/TCTR20210703002). Moreover, informed consent was obtained from all the participants. Participants who read and then signed the consent form were enrolled in the study. All procedures including participant enrollment, screening, data collection, data scrutiny and analysis were performed in accordance with relevant guidelines.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplementary Table 1.
Therapeutic sessions details with designed agenda and content for the patients withT2DM.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Abbas, Q., Latif, S., Ayaz Habib, H. et al. Cognitive behavior therapy for diabetes distress, depression, health anxiety, quality of life and treatment adherence among patients with type-II diabetes mellitus: a randomized control trial. BMC Psychiatry 23, 86 (2023). https://doi.org/10.1186/s12888-023-04546-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12888-023-04546-w