Abstract
Background
Because they are prevalent, persistent, and have substantial negative effects on physical health, psychological well-being, and economic implications, common mental illnesses like depression, anxiety, and somatic complaints are major public health problems. Patients with mental illness are devoted to religious therapy including holy water as a coping mechanism for their illnesses. The aim of this study was to investigate the magnitude and associated factors of common mental illness among adult holy water users.
Methods
Facility-based cross-sectional study design was conducted in Amhara regional state orthodox Tewahido churches. A simple random sampling techinque was used to select participants. Data were collected by using the Brief Psychiatric Rating Scale for mental illnesses symptoms and a structured interviewer administered questionnaire was used. Data were entered into EpiData version 4.6 and exported to SPSS version 25 for analysis. Variables with a p-value of 0.25 in the bivariable logistic regression were entered into multivariable logistic regression.
Result
Three hundred eighty-two participants were involved in the study. The magnitude of Common mental illnesses among holy water users was 58.9%. Unemployed, using more than one substance, having Poor and moderate social support, current daily alcohol drinker and past history of mental illness were significantly associated with common mental illness.
Conclusion
The magnitude of common mental illness among adult holy water users was high. Giving special attention to decreasing unemployment, establishing social support services, and decreasing substance utilization are the keys to preventing common mental illnesses.
Similar content being viewed by others
Introduction
Back ground
Mental illnesses are health conditions involving changes in emotion, thinking or behavior or a combination of these which leads to distress and problems of functioning in social, work or family activities [1]. Many people who have a mental illness do not want to talk about it [2]. Mental health conditions are treatable which can affect anyone regardless of age, gender, geography, income, social status, race/ethnicity, religion/spirituality, background or other aspect of cultural identity [3].
Neuropsychiatric disorders account for 13% of the total Disability Adjusted Life Years (DALYs) lost due to all diseases and injuries in the world and were estimated to increase to 15% by the year 2020. Worldwide, five of the ten leading causes of disability and premature death are psychiatric illnesses [4]. According to global burden of diseases 2010 among 291 diseases, injuries, and risks from 187 countries indicated that common mental illness (depressive disorder 41% and anxiety disorder 15%) are the third cause of Disability-adjusted life years (DALYs) next to circulatory and cancer diseases [5].
Common mental illnesses like depression, anxiety, and somatic complaints are global health concerns which have substantial negative effects on physical health, psychological well-being, and economic implications because of high prevalence and chronicity [6]. Recent statistics showed that one in five people experienced common mental illnesses in the past year, and 29.2% of people have experienced episodes of common mental disorders throughout their lives [6]. The overlaps of somatic, anxious and depressive syndromes are frequent in the general population [7].
Various studies showed that the magnitude of common mental illnesses varied across the world. In Great Britain (England, Wales and Scotland) 24.6% of the study participants were suffered from common mental illnesses [8]. Another study conducted in Brazil reported that the magnitude of common mental illnesses was 29.3 %[9]. Evidence conducted in China showed that about 34.4% of the respondants were had common mental illnesses [10]. In Africa, the estimated magnitude of common mental illnesses in Tanzania was 24–28.8 %[11, 12]. The magnitude of common mental illnesses was 10.3% in Kenya and 27% in South Africa respectively [13, 14]. Studies done in Ethiopia showed that the magnitude of common mental illnesses was ranged from 14.9 to 33.6% [15,16,17,18].
Mental illnesses have great impact on the economical aspect of the population. It directly costs actual expenditures for the care of the mentally ill by public and private agencies [19]. It has also indirect costs based on the annual loss of production, annual earnings, and work years by patients [20]. In addition, mental health ilnesses meaningfully adds to a cycle of poverty where people who experiences social suffering and poverty are at augmented risk of mental illness, and on the other hand, those with mental illnesses are at amplified the threat of poverty [21].
According to a study conducted in Ethiopia, most people were considered that mental disorders are results from sprites and evil forces. For these reasons they prefer religious institutions than mental treatment for curative practices habitually using holy water sites [22]. Another study done in Ethiopia supported that most Ethiopians blames supernatural forces for mental health issues. As a result, the majority of people were seen turning to supernatural remedies such as prayer, fasting, holy water sprinkles, and meeting with those who were believed to possess special abilities for curing mental health issues [23]. The most popular method of treating mental illnesses in Ethiopia is holy water, which is used by Orthodox Christian who think it has healing properties that embody the spirit of Christ [24]. People of Orthodox Christian religion (43.5% of the population )[25] and the wider public [26] both used holy water because of a widely held cultural and interreligious belief.
Eventhough the burden of common mental illnesses are higher in low and middle-income countries; including Ethiopia, the health services delivery setting (primary health care setting) for clients who are suffering from mental illnesses is extremely limited. So due to these reasons, instead of visiting health care services; most clients are forced to visit holy water sites. So far, no study was conducted to assess the magnitude of common mental disorder and its associated factors among adults holy water user in the study setting. Therefore, this study was intended to assess the magnitudeof common mental illness and its associated factors among adults holy water user. More over, the result will give significant information to policymakers, important for early interventions which help to reduce the magnitude of common mental illness and to improve the clients’ quality of life. It will be used for the researchers as a baseline data.
Methods
Study design, period and setting
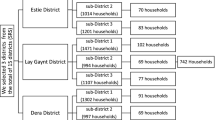
Institutional based cross-sectional study was conducted from November 28 –December 28, 2021, in Amhara regional state Orthodox Tewahido churches, Ethiopia. The study was conducted in Amhara nationalregional state Orthodox churches, which have holy water users for different purposes like the healing of mental illness. Amhara Region is a regional state in Northwest Ethiopia, and its capital city is Bahir Dar. Iaccording to central statistical agency Ethiopia (CSA), 2017 the total population were 21,134,98 8[27]. The study was conducted in five randomly selected churches, namely Wonkshet Gebreal, Gono Gebreal, Megendi Giorgis, Andasa Giorgis, and Tsadikane Maryam. Wonkshet Gebreal and Gono Gebreal located in South Gondar district, Megendi Giorgis and Andasa Giorgis in west Gojjam district, and Tsadikane Maryam located in North Shewa district.
Source population
All clients who used Orthodox Tewahido churches holy water in Amhara region.
Study population
All adults who used Orthodox Tewahido churches holy water in Amhara region during the study period.
Inclusion criteria and exclusion criteria
People, who use Orthodox Tewahido churches holy water in the Amhara region and age of 18 and beyond were involved in the study. On the other hand individuals who had problem of communication, and holy water user who interrupted the interview were excluded from the study.
Sample size determination
The single population proportion formula was used to determine the required sample size by considering a 50% estimated proportion of mental illness among holy water user adults, since no study was done on this problem in Ethiopia.
By considering 95% confidence interval (CI) and 5% as margin of error, sample was calculated as follows:
Then total sample size = 384 + 10% non-response rate (39) = 423.
Sampling techniques
First, permission was obtained from the selected church administrators. Then, lists of holy water users at selected churches were taken from the registration books. After listing, the selection of participants has conducted by the lottery method. The number of samples in each selected churches was distributed proportionally based on the total number of holy water users in individually selected churches.
Dependent variable
Common mental illness.
Independent variable
Socio demographic variables and psychosocial factor
Sex, Age, Ethnicity, Religion, Marital status, Educational status, Occupation, Residence, Social support
Behavioral factors
Alcohol, Tobacco, and Khat.
Clinical factors
Previous mental disorder, Family history of mental illness, known medical/surgical disease.
Operational definitions
Common mental illness
Those participants who had self-report somatic illness, anxiety and depression by using Brief Psychiatric Rating Scale (BPRS) [28, 29].
Current and ever use of substance
Using a specific substance for non-medical purpose in the last 3 months and using of a particular substance for non-medical purpose once in lifetime respectively [30].
Data collection tools
Data collection was conducted by using an interviewer-administered structured questionnaire, interview and observation by Brief Psychiatric Rating Scale (BPRS) for mental illness symptoms. Data were collected by four BSc psychiatric nurses and supervised by two MSc psychiatry nurses. BPRS has 24 items with seven scale measurements ranging from “not present” to “extremely severe, the first three items were used to asess common mental illnesses (somatic concern, anxiety and depression) [29, 30]. The Extent of soscial support was assessed by using three-item Oslo social support scale with a range of between 3 and 14. “scoring of 12–14 = strong social support”, “score of 9–11 = moderate social support and”, “score of 3–8= poor social support” scale [31].
Data quality assurance
The questionnaire was first prepared in English and translated to Amharic language for data collection and back re-translated to English language by fluent speaker language experts to maintain its concistency. The training was given to data collectors and supervisors on BPRS. The pre-test was done on 5% of holy water users at Recha Gebreal church; 2 weeks before the start of actual data collection and revision was made accordingly. Reliability was checked and Cronbach’s alpha was 0.921. The supervisors and principal investigator have checked the completeness and consistency of the filled questionnaires daily.
Data processing and analysis
Data were coded, filtered, and entered into EpiData version 4.6 and then exported to SPSS version 25 for analysis. Binary logistic regression analysis was used to determine the association between the dependent and independent variables. Firstly, bivariable logistic regression was performed and all variables with P ≤ 0.25 in the bivariable analysis were included in the final model of multivariable analysis in order to control all possible confounders. The goodness of fit was tested by Hosmer-Lemeshow statistic and the data fitted to the model. The direction and strength of statistical association were measured by the odds ratio with 95% CI. The adjusted odds ratio along with 95% CI were estimated to identify factors associated with complications by using multivariable analysis in binary logistic regression. Finally, P-value ≤0.05 was considered to declare as a statistically significant.
Results
Socio demographic characteristics
Three hundred eighty-two participants were involved in the study with a response rate of 90.3%. Among respondents, 253 (56.3%) were females and about half (47.9%) of them were in the age group of 26–40 with a mean age of 35.69 (SD ± 12.43). Of the total respondents, 184 (48.2%) were separated. Regarding social support conditions, 175 (45.8%) were had poor social support. In relation to occupational status, 66% of them were unemployed (Table 1).
Behavioral factors
About 101 (26.4%) of the respondents were used two or more substance in their lifetime (Table 2).
Clinical related factors
Of 382 respondents, 194 (50.6%) had a past history of psychiatric illness and 53 (13.9%) had a family history of mental illness. Ninety-two (24.1%) of the study participants had a history of known medical or surgical condition (Table 3).
Magnitude of common mental illness
Among 382 study participants, 225(58.9%) had a BPRS score of > 31. Therefore, the magnitude of common mental illness was 58.9% with 95% CI (53.9–63.6).
Among mentally ill individuals, 133 (59.1%) were females and 121 (53.7%) were separated. Of mentally ill individuals, 79 (35.1%) were using more than one substance in their lifetime and 39.1% of them had a previous history of mental illness.
Factors associated with common mental illness
Being unemployed holy water users were 1.71 times (AOR = 1.71, 95% CI = (1.002–2.92)) more likely to had common mental illness (Table 4).
Discussion
The main aim of this study was to assess the magnitude and associated factors of common mental illness among adults holy water user in Amhara regional state Orthodox Tewahido churches, Ethiopia.
The magnitude of common mental illness among adults holy water user in the Amhara region Orthodox Tewahido churches holy water users was 58.9% (95% CI, 53.9–63.6). The finding is higher than the study done in Great Britain 24.6 %[8], Brazil 29.3 %[9], China, Bangladesh 52.5 %[32], 34.4 %[10], South Africa 27 %[13], Kenya 10.3 %[14], and Ethiopia 29.7 %[18]. This difference is mainly due to the study setting. Because our study setting were holy water sites the chance of getting large number of common mental illnesses is high compared with community based setting. This high magnitude of common mental illness can be due to the reason that, mentally illpeople prefer religious places than psychiatric institutions due to their thought, sprit, and possession that supernatural are the cause of mental illnesses [33]. The other reason is misunderstanding of population around the study area that is mental illness is not treatable by psychomedications rather they believed that the illness is due to punishment from God or creatures [18].
This study revealed that common mental illness is more likely in unemployed individuals as compared to those who were employed. This is supported by studies done in Australia [34], South Africa [13], Tanzania [12], and Ethiopia [18, 35]. This can be explained by common mental illnesses among unemployed may result from tension due to the incapability to accomplish economic and social costs. Unemployed is also at risk for substance dependence tributary to desperateness, and difficulties in managing social and familial needs, which all lead to common mental illness.
Holy water users who used more than one substance were more likely to have common mental illnesses as compared to those who do not have a substance use history. This result is supported by the study [36]. This is due to the interactions between mental illnesses and substance use that leads to physiological, economic, and social functioning impairment on an individual [37].
The result in this study showed that those who have a previous history of mental illness were more likely to have common mental illness. The finding is similar with the studies done in Ethiopia [18, 35]. This is due to those who had previous history of psychiatric illnesses either they might not got psychiatric treatmentor not taken their medication properlyand the root cause of illnesses might not be managed; the chance of relapsing is high.
This study revealed that having poor and moderate social supports were more risk for the occurrence of common mental illness. This finding is inline with the studies done in Ethiopia [18, 33]. The possible explanation for this is those individuals who are poor, and moderate social support may exposed to certain harmful things, stressors or substances like alcohol drinking and might be developed or susceptible for common mental illness.
Limitation of study
The study did not analyze the effect of a specific medical illness and undiagnosed medical illness on common mental illnesses.
Conclusion
The magnitude of common mental illness among adults holy water user was high. The reasons for this figure reflect that the insight of community towards mental illnesses entirly depends on religious sites. To minimize the magnitude of common mental illness; stakeholders should work together with religious fathers or leaders to bring these patients to mental clinics. Different factors were identifed which contributed for common mental illness. Giving special attention to decreasing unemployment, establishing social support services, decreasing substance utilization by providing substance rehabiltation centers in health services and early management of mental illness helps to decrease common mental illness.
Availability of data and materials
All data are available with in the manuscript and supplementary files.
References
American Psychiatric Associations. https://www.psychiatry.org/patients-families/what-is-mental-illness. online updated on November 2022.
High Watch Recovery Center. https://highwatchrecovery.org/. Why-dont-people-seek-help-for-mental-illness/. January 15, 2019.
Association AP. Diagnostic and statistical manual of mental disorders: DSM-IV-TR®: American Psychiatric Pub; 2000.
WHO: World health report 2004.
Murray CJLE, Flaxman AD, Lim S, Lozano R, Michaud C, et al. GBD 2010: design, definitions, and metrics. Lancet. 2012;380:2063–6.
Steel Z, Marnane C, Iranpour C, Chey T, Jackson JW, Patel V, et al. The global prevalence of common mental disorders: a systematic review and meta-analysis 1980–2013. Int J Epidemiol. 2014;43(2):476–93.
Kohlmann S, Gierk B, Hilbert A, Brähler E, Löwe B. The overlap of somatic, anxious and depressive syndromes: a population-based analysis. J Psychosom Res. 2016;90:51–6.
Weich S, Lewis G. Poverty, unemployment, and common mental disorders: population based cohort study. Bmj. 1998;317(7151):115–9.
Rocha SV, de Almeida MMG, de Araújo TM, Virtuoso Júnior JS. Prevalence of common mental disorders among the residents of urban areas in Feira de Santana, Bahia. Rev Bras Epidemiol. 2010;13:630–40.
Zhong B-L, Liu T-B, Chan S, Jin D, Hu C-Y, Dai J, et al. Common mental health problems in rural-to-urban migrant workers in Shenzhen, China: prevalence and risk factors. Epidemiol Psychiatr Sci. 2018;27(3):256–65.
Uriyo JG, Abubakar A, Swai M, Msuya SE, Stray-Pedersen B. Prevalence and correlates of common mental disorders among mothers of young children in Kilimanjaro region of Tanzania. PLoS One. 2013;8(7):e69088.
Jenkins R, Mbatia J, Singleton N, White B. Common mental disorders and risk factors in urban Tanzania. Int J Environ Res Public Health. 2010;7(6):2543–58.
Havenaar JM, Geerlings MI, Vivian L, Collinson M, Robertson B. Common mental health problems in historically disadvantaged urban and rural communities in South Africa: prevalence and risk factors. Soc Psychiatry Psychiatr Epidemiol. 2008;43(3):209–15.
Jenkins R, Othieno C, Ongeri L, Sifuna P, Ongecha M, Kingora J, et al. Common mental disorder in Nyanza province, Kenya in 2013 and its associated risk factors–an assessment of change since 2004, using a repeat household survey in a demographic surveillance site. BMC Psychiatry. 2015;15(1):1–12.
Hunduma G, Girma M, Digaffe T, Weldegebreal F, Tola A. Prevalence and determinants of common mental illness among adult residents of Harari regional state, eastern Ethiopia. Pan Afr Med J. 2017;28(1):262.
Kerebih H, Soboka M. Prevalence of common mental disorders and associated factors among residents of Jimma town, South West Ethiopia. Population. 2016;8:6–8.
Yimam KKY, Azale T. Prevalence of common mental disorders and associated factors among adults in Kombolcha town. Northeast Ethiopia. J Depress Anxiety S. 2014;1:2167–1044.
Legas G, Beyene GM, Asnakew S, Belete A, Shumet S, Selomon Tibebu N, et al. Magnitude and predictors of common mental disorders among residents in South Gondar zone, Northwest Ethiopia: a community-based, cross-sectional study. BMC Psychiatry. 2022;22(1):1–8.
Chisholm D, Saxena S, Van Ommeren M. Dollars, DALYs and decisions: economic aspects of the mental health system: World Health Organization; 2006.
Doran CM, Kinchin I. Economics of mental health: providing a platform for efficient mental health policy: Springer; 2020.
WHO: WHO. Mental Health. world health report. 2007.
Jacobsson L. Traditional treatment of mental and psychosomatic disorders in Ethiopia. Int Congr Ser. 2002;1241:265–9.
Hailemariam KW. Perceived causes of mental illness and treatment seeking behaviors among people with mental health problems in Gebremenfes Kidus holy water site. Am J Appl Psychol. 2015;3(2):34–42.
Hannig A. The pure and the pious: corporeality, flow, and transgression in Ethiopian orthodox Christianity. J Relig Afr. 2013;43(3):297–328.
World Health O. Mental health atlas 2017. Geneva: World Health Organization; 2018.
Teshome-Bahire W. Initiation of healers in Ethiopia: a case study. Collegium antropologicum. 2000;24(2):555–63.
Population projection of Ethiopia for all regions at Wereda level from 2014 – 2017. In.; June 2018. https://web.archive.org/web/20180606103106/http://www.csa.gov.et/ehioinfo-internal.
Lukoff D, Liberman RF, Nuechterlein K. H: symptom monitoring in the rehabilitation of schizophrenic patients. Schizophrenic Bull. 1986;12:578–602.
Leucht S, Kane JM, Kissling W, Hamann J, Etschel E, Engel R. Clinical implications of brief psychiatric rating scale scores. Br J Psychiatry. 2005;187(4):366–71.
Henrique I, De Micheli D, Lacerda R, Lacerda L, Formigoni M. Validation of the Brazilian version of alcohol, smoking and substance involvement screening test (ASSIST). Rev Assoc Med Bras (1992). 2004;50(2):199–206.
Dalgard OSDC, Lehtinen V, Vazquez-Barquero JL, Casey P, Wilkinson G, et al. Negative life events, social support and gender difference in depression. Soc Psychiatry Psychiatr Epidemiol. 2006;41(6):444.
Islam FMA. Psychological distress and its association with socio-demographic factors in a rural district in Bangladesh: a cross-sectional study. PLoS One. 2019;14(3):e0212765.
Legas G, Asnakew S, Belete A, Beyene GM, Wubet GM, Bayih WA, et al. Magnitude and correlates of alcohol use disorder in south Gondar zone, northwest Ethiopia: A community based cross-sectional study. PLoS One. 2021;16(9):e0257804.
Scutella R, Wooden M. The effects of household joblessness on mental health. Soc Sci Med. 2008;67(1):88–100.
Mekonnen E, Esayas S. Correlates of mental distress in Jimma town, Ethiopia. Ethiop J Health Sci. 2016;13,1:2003.
Drake RE. T MUESER K, Brunette MF: management of persons with co-occurring severe mental illness and substance use disorder: program implications. World Psychiatry. 2007;6(3):131.
Pepper B, Kirshner MC, Ryglewicz H. The young adult chronic patient: overview of a population. Psychiatr Serv. 1981;32(7):463–9.
Acknowledgments
We would like to express our heartfelt gratitude to Debre Tabor University and all selected study site officials whom we have communicated, and indorsed as to conduct this study. Our special thanks also extended to the study participants, data collectors, and supervisors.
Funding
No fund received; all costs were covered by the authors.
Author information
Authors and Affiliations
Contributions
All authors have made substantial contributions to this study. The corresponding author conceived and designed the study, did the literature search, coordinated the write-up, participated in data analysis, editing, and submission of the article. All co-authors participated in literature search, analysis, and interpretation of data, drafting the article and revising it for important intellectual content, and approve the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All methodological procedures have been performed in accordance with the declaration of Helsinki and ethical approval was obtained from the ethical review committee of Debre Tabor University. The official letter was submitted to the selected churches. Then, permission was obtained from the selected church administrators. Informed consent was obtained from the study participants. The participants were fully informed about the purpose and objectives of the study.
Consent for publication
Not applicable.
Competing interests
The authors declared that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Belete, A., Abate, M.W., Nigat, A.B. et al. The magnitude of common mental illness and associated factors among adult holy water users in Amhara regional state Orthodox Tewahido churches, Ethiopia, 2021. BMC Psychiatry 23, 53 (2023). https://doi.org/10.1186/s12888-023-04524-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12888-023-04524-2