Abstract
Background
Common mental disorders are severe and frequent co-morbid psychiatric illnesses with epilepsy. Different study findings across the world showed that patients with epilepsy have a higher burden of mental disorders than the general population. However, these issues in patients with epilepsy have been consistently undiagnosed.
Objectives
The study aimed to screen common mental disorders and the determinants among patients with epilepsy attending at Fenote Selam hospital.
Methods
An institutional-based cross-sectional study was conducted among patients with Epilepsy from March 10 to May 15, 2019. Patients were assessed for the risk of common mental disorders using a pretested, structured, self-reporting questionnaire (SRQ-20). The collected data were entered into Epi-data version 3.1 software and analyzed using R version 4.0 software. Descriptive statistics were computed using frequency, percent, mean, and standard deviations. A simple logistic regression model was fit to identify the association and strength of exploratory variables and common mental disorders at a 95% confidence interval and p-value < 0.05.
Results
The study included 202 patients diagnosed with epilepsy and yielded a response of 91.4%. About 53% of the patients were males. The magnitude of common mental disorders among patients with epilepsy was 57.9% (95% CI: 44.56, 71.24). Being more than one substance user (AOR = 5.7; 95%CI: 1.6, 20.7) and Not having social support (AOR = 4.3; 95%CI: 1.5, 11.9) were the identified determinants of common mental disorders.
Conclusion
The magnitude of common mental disorders among patients with epilepsy were high. Not having social support and khat chewing were the identified risk factors significantly associated with common mental disorders. Early screening and treatments are the key interventions to prevent complications and deaths from common mental disorders.
Similar content being viewed by others
Background
Mental health is the crucial aspect of health closely allied with the physical and physiological changing aspects of the human body [1]. A clinically important impairement in a person’s cognition, emotion control, or behavior caused by a failure in the biological, psychological or developmental processes underpinning mental functioning is known as a mental disorder [2]. As well as insomnia, fatigue, irritability, forgetfulness, difficulty concentrating, substantial distress, impairment of social, or occupational activities, and somatic complaints, mental disorders encompass a wide range of mental disorders that do not fit into standard diagnostic criteria [3,4,5].
The World Health Organization reported that mental disorder is the direct risk factor for mortality and morbidity [6, 7]. Psychiatric comorbidities occur in about one-third of patients with epilepsy during the lifespan, and the risk of these comorbidities are much higher in patients with treatment-resistant seizures [8, 9].
Mental disorders have a vital negative impact on the quality of life and living standards of patients with epilepsy. Risk factors for common mental disorders among epileptic patients were being female, young age, marital status, lower-income, unemployment, low educational status, worse QOLIE-89 scores, lack of social support, frequent seizures attacks, side effects of antiepileptic drugs, medication non-adherence, nicotine dependence, alcohol misuse, family history of psychiatric illness, comorbidity of medical condition, duration of illness, and poly-pharmacy [10,11,12,13,14,15,16].
Despite the high burden of common mental disorders among patients with epilepsy, they remain under-investigated and inappropriately treated [18]. Better understanding and treatment of common mental disorders can assist early complication management and better health outcomes for people living with epilepsy. However, the magnitude and determinants of common mental disorders in patients with epilepsy are not determined well in low income countries, including Ethiopia in general and the study area in particular. Therefore, this study aimed to assess the magnitude of common mental disorders and the determinants among patients with epilepsy attending at the Fenote Selam hospital.
Methods
Study design, setting, and period
This institutional-based cross-sectional study was conducted at the Fenote Selam hospital from March 10 to May 15, 2019. The hospital is situated 378 km from Ethiopia’s capital city of Addis Ababa in the Amhara region. It is the only public hospital in Fenote Selam town.
Population
The source population for this study was all patients with epilepsy (N = 521) attending at the Fenote Selam hospital for epilepsy treatment, while the study population was those patients 18 years and older. Those patients who dropped out the treatment, missed the appointment, or transferred out to other health institutions during the data collection period were excluded.
Sample size determination and sampling procedure
The sample size was determined using the single population proportion formula by considering a 95% confidence level, a 5% margin of error, and a 50% proportion of common mental disorders. Taking the 10% non-response rate and the correction formula (N < 10, 000), the final sample size was 202. A simple random sampling technique was applied using their medical record numbers. The patients were interviewed and their medical records reviewed.
Operational definitions
Common Mental disorder
The patient was screened for common mental disorder using the SRQ-20 dichotomous items (Yes = 1, No = 0). The likelihood of a common mental disorder was considered when he/she responded to nine or more positive (yes) answers out of the total. Otherwise, the patient was considered not at risk of common mental disorder [19].
Social support
Patients with Epilepsy who scored mean or above of the social support assessing questions (got counseling, financial aid, and or physical support from family, friends) correctly were considered as getting social support. Otherwise didn’t get social support [20].
Data collection tool
Data were collected using a pre-tested structured questionnaire, adapted from a standardized self-reporting questionnaire (SRQ-20) with a 30-day recall period [21, 22]. The questionnaire comprised social-demographic, somatic, depressive/anxiety, and cognitive [23] and the multidimensional scale of perceived social support [20] assessing characteristics. It was translated into the Amharic (the indigenous) language by the independent translator (Ph.D. in linguistics) and then back to English to check for consistency. The five-day training was given to two enumerators (BSc in nursing) and one supervisor (MSc in psychiatry). The enumerators conducted a role-plays before the actual data collection period. Finally, the data was collected using the Amharic version of the questionnaire. Each questionnaire was examined for completeness and consistency by the supervisor and the principal investigator daily, and appropriate feedback was given to the data collectors.
Data management and analysis
Data entry, cleaning, and coding were performed using Epi-data version 3.1 software, and the analysis was done using R version 4.0 software. Descriptive statistics were computed using frequency, percent, mean, and standard deviation. Bivariate and multivariate logistic regression analyses were employed to assess the association between the exploratory variables and mental disorders. The strength of the association was measured using the adjusted odds ratio (AOR) and 95% confidence interval (CI). A p-value < 0.05 was considered a statistically significant predictor of common mental disorders.
Results
Socio-demographic characteristics of the study participants
A total of 202 patients with epilepsy participated in the study, with a response rate of 91.4%. About 52% and 54% of the patients were males and single. About 20% of the patients were unable to read and write. About one-third of the patients were students. Almost 40% of them were living in rural areas and had a monthly income of fewer than 700 Birrs (Table 1).
Seizure characteristics of patients with epilepsy
About 52% of the current and ever substance-using patients were at risk of common mental disorders. Of 35.3% of multi-substance users, 72% were at risk of common mental disorders. Of 20.3% of phenytoin drug users, 76% were at risk of common mental disorders. Similarly, out of 20.3% of patients who had a seizure during treatment, 76% were at risk of having a common mental disorders (Table 2).
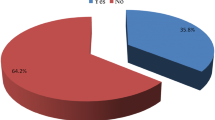
The magnitude of common mental disorders among patients with epilepsy
The magnitude of common mental disorders among patients with epilepsy was 57.9% (95% CI: 44.56, 71.24).
Factors associated with a diagnosable mental disorder
On bivariate analysis, occupational status, social support, types of substances used, types of anti-epileptic drugs used, and seizures during treatment were factors associated with common mental disorders at 20% of level of significance. Whereas in the multivariable analysis, only social support and types of substances used showed a significant association with common mental disorders.
For those patients who hadn’t received social support, the odds of developing common mental disorders were about four (AOR = 4. 3; 95%CI: 1.5, 11.9) times higher compared to those who had. Similarly, for those patients abused by more than one substance, the odds of common mental disorders were about six (AOR = 5. 7; 95%CI: 1.6, 20.7) times higher compared to those khat chewers (Table 3).
Discussion
This study identified the magnitude of common mental disorders and the determinants among patients with epilepsy attending the Fenote Selam hospital. The study revealed that 57.9% (95% CI: 44.56, 71.24) of the patients had common mental disorders. This finding was higher than the studies done in northwest Ethiopia (45.2%), Addis Ababa, Ethiopia (27.1%), Mexico (36.6%), Sudan (45.5%), the systematic review (32.71%), Hawassa, Ethiopia (34.2%), and Nigeria (31–37%) [17, 24,25,26,27,28,29], respectively. However, it was lower compared to the studies from Burkina Faso (67.3%) and Nigeria (37%) [30, 31]. The possible reasons for the difference might be due to differences in the study period, study area, and socio-cultural practice.
The present study showed that patients who had no social support were about fourfold more likely to have common mental disorders (AOR = 4. 3; 95%CI: 1.5, 11.9) compared to those who had social support. This finding was consistent with a study done in Ethiopia [27]. This could be explained by the fact that lack of social support might deteriorate the patient’s health and quality of life due to fear of lacking support in the future when he/she gets sick.
The study also identified the use of addiction-inducing substances while on anti-epilepsy treatment was significantly associated with common mental disorders. For patients who used more than one substance, the odds of common mental disorders (AOR = 5. 7; 95%CI: 1.6, 20.7) were 6 times higher compared to those who used chat. This was supported by a study done in central Ethiopia [32]. The possible justification for this typical finding might be that the content of chemicals in more substance users might bring a higher risk of common mental disorders than only chat users when taken along with anti-epileptic drugs.
The findings of this study indicate that common mental disorders are common co-morbidities in patients with epilepsy. Healthcare professionals should assess and treat psychiatric and physical co-morbidities among patients with a history of seizures to improve patient health outcomes. The families of patients with epilepsy should be made aware of the disorders and their related psychological co-morbidities so that the patients can receive sufficient support from their families.
Limitations of the study
The difficulty of distinguishing the temporal relationships. There might also be a potential for recall bias. It is difficult to investigate why the effect of khat chewing is a potential risk factor for common mental disorders. Therefore, a strong evidenced study should be done to ascertain the impact of khat on mental disorders.
Conclusion
The risk of common mental disorders among patients with epilepsy was high. Social support and the type of substances used were the identified factors significantly associated with the risk of common mental disorders.
Recommendations
The authors recommended that the health care workers should give great attention to counseling on the reduction of substance use of the patients with epilepsy. In addition, the study suggests arranging social support and creating awareness about the consquences of taking substances (non medication) are important to reduce the common mental disorders.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Abbreviations
- AOR:
-
Adjusted Odds Ratio
- BSc:
-
Bachelor in Science
- CI:
-
Confidential Interval
- COR:
-
Crude Odds Ratio
- Epi-data:
-
Epidemiological Data
- Ph.D:
-
Doctor of Philosophy
- SRQ:
-
Self-Reporting Questionnaire
- MSc:
-
Masters of Science
References
Tawar S, Bhatia SS, Ilankumaran M. Mental health, are we at risk? Indian J community medicine: official publication Indian Association Prev Social Med. 2014;39(1):43.
Edition F. Diagnostic and statistical manual of mental disorders. Am Psychiatric Assoc. 2013;21(21):591–643.
Aderibigbe Y, Gureje O, Omigbodun O. Postnatal emotional disorders in Nigerian women: a study of antecedents and associations. Br J Psychiatry. 1993;163(5):645–50.
Kreutzer JS, Seel RT, Gourley E. The prevalence and symptom rates of depression after traumatic brain injury: a comprehensive examination. Brain Injury. 2001;15(7):563–76.
Robles R, et al. Removing transgender identity from the classification of mental disorders: a Mexican field study for ICD-11. The Lancet Psychiatry. 2016;3(9):850–9.
Whiteford HA, et al. Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010. The Lancet. 2013;382(9904):1575–86.
Ferrari AJ, et al. Burden of depressive disorders by country, sex, age, and year: findings from the global burden of disease study 2010. PLoS Med. 2013;10(11):e1001547.
Keezer MR, Sisodiya SM, Sander JW. Comorbidities of epilepsy: current concepts and future perspectives. Lancet Neurol. 2016;15(1):106–15.
Mula M. Treatment issues for psychiatric comorbidities of epilepsy. Clin Pract. 2013;10(3):293–300.
Bifftu BB, et al. Depression among people with epilepsy in Northwest Ethiopia: a cross-sectional institution based study. BMC Res Notes. 2015;8(1):1–8.
Ettinger A, Reed M, Cramer J. Depression and comorbidity in community-based patients with epilepsy or asthma. Neurology. 2004;63(6):1008–14.
Schmitz EB, Robertson MM, Trimble MR. Depression and schizophrenia in epilepsy: social and biological risk factors. Epilepsy Res. 1999;35(1):59–68.
Tareke M, et al. Common mental illness among epilepsy patients in Bahir Dar city, Ethiopia: a cross-sectional study. PLoS ONE. 2020;15(1):e0227854.
Taylor DC. Factors influencing the occurrence of schizophrenia-like psychosis in patients with temporal lobe epilepsy. Psychol Med. 1975;5(3):249–54.
Tsegabrhan H, et al. Co-morbidity of depression and epilepsy in Jimma University specialized hospital, Southwest Ethiopia. Neurol India. 2014;62(6):649.
Wubie MB, Alebachew MN, Yigzaw AB. Common mental disorders and its determinants among epileptic patients at an outpatient epileptic clinic in Felegehiwot Referral Hospital, Bahirdar, Ethiopia: cross-sectional study. Int J Mental Health Syst. 2019;13(1):1–10.
Bifftu BB, et al. Depression among people with epilepsy in Northwest Ethiopia: a cross-sectional institution based study. BMC Res Notes. 2015;8(1):585.
Fiest KM, Patten SB, Jetté N. Screening for depression and anxiety in epilepsy. Neurol Clin. 2016;34(2):351–61.
Carmo MBBd, et al. Screening for common mental disorders using the SRQ-20 in Brazil: what are the alternative strategies for analysis? Brazilian J Psychiatry. 2018;40:115–22.
Zimet GD, et al. The multidimensional scale of perceived social support. J Pers Assess. 1988;52(1):30–41.
Beusenberg M, Orley JH, Organization WH. A User’s guide to the self reporting questionnaire (SRQ. Geneva: World Health Organization; 1994.
Abou-Saleh M, Ghubash R, Daradkeh T. Al Ain community psychiatric survey. I. Prevalence and socio-demographic correlates. Soc Psychiatry Psychiatr Epidemiol. 2001;36(1):20–8.
Harpham T, et al. Measuring mental health in a cost-effective manner. Health Policy Plann. 2003;18(3):344–9.
Domínguez-Aguilera M, Muñiz-Landeros C. Prevalence of psychiatric disorders in patients with epilepsy in a tertiary level care hospital: Detection through the MINI PLUS International Structured Interview. Med Universitaria. 2017;19(74):3–6.
Duko B, et al., Depressive Symptoms among Patients with Epilepsy Attending Adare General Hospital, Hawassa Ethiopia: Cross-sectional Study 2018.
Saadalla A, Elbadwi A. Depression among Sudanese epileptic patients. Age. 2016;5(5):18–25.
Seid S, et al., Prevalence and Associated Factors of Mental Distress among Caregivers of Patients with Epilepsy in Ethiopia: A Cross-Sectional Study Design Psychiatry journal, 2018. 2018.
Adewuya AO, Ola BA. Prevalence of and risk factors for anxiety and depressive disorders in Nigerian adolescents with epilepsy. Epilepsy Behav. 2005;6(3):342–7.
Dessie G, et al., Prevalence of Depression among Epileptic Patients and its Association with Drug Therapy: A Systematic Review and Meta-Analysis BioRxiv, 2018: p. 387571.
Gureje O. Interictal Psychopathology in Epilepsy Prevalence and Pattern in a Nigerian Clinic. Br J Psychiatry. 1991;158(5):700–5.
Dabilgou AA, et al. Symptoms of Depression and Associated Risk Factors in Patients with Epilepsy in Burkina Faso. Open J Depress. 2019;8(1):29–40.
Chaka A, et al. Determinants of depression among people with epilepsy in Central Ethiopia. Ann Gen Psychiatry. 2018;17(1):27.
Acknowledgements
We would like to thank our study participants, data collectors, supervisor, and Fenote Selam hospital staff for their cooperation and support during the data collection.
Funding
No fund was received.
Author information
Authors and Affiliations
Contributions
All authors have an equal contribution.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Research Ethics Committee of Alkan Health Science Business and Technology College approved the study with reference number: AHSC/RCS/28/2019. The support letter was received from Fenote Selam hospital. Written informed consent was obtained from the study participants before commencing the data collection. The authors confirm that all methods were in accordance with the Declaration of Helsinki.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Bantie, G.M., Woya, A.A., Ayenew, G.M. et al. Magnitude of common mental disorders and associated factors among patients with Epilepsy in Amhara regional state, Northwest Ethiopia. BMC Psychiatry 22, 674 (2022). https://doi.org/10.1186/s12888-022-04314-2
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12888-022-04314-2