Abstract
Background
The aim of the study was to investigate functional impairment and its relationship to illness severity in a sample of patients with a diagnosis of mood or anxiety disorder during inpatient treatment and 1 year after discharge.
Methods
Two hundred thirty-nine inpatients with primary diagnoses of mood or anxiety disorders were assessed at baseline and at follow-up by a range of validated instruments. Mini-ICF-APP was used for the assessment of functional impairment, BDI-II for the assessment of clinical symptoms and remission. Sample characteristics and measures of impairment at baseline and at follow-up were analysed descriptively. Symptomatically remitted and non-remitted patients were compared with regard to capacity limitations.
Results
Initially, the sample showed considerable impairment in many capacities, particularly endurance, spontaneous activities, structuring of tasks, competency and flexibility. After 1 year, all capacities significantly improved. The level of impairment was correlated with employment status and severity of clinical symptoms. About 50% of the patients remitted in clinical symptomatology. Retrospectively, the remitted and the unremitted did not differ in functional impairment at baseline but there were considerable differences at follow-up.
Conclusions
Mini-ICF-APP is a useful instrument to monitor functional status and change in psychiatric samples, complementing the usual focus on symptom reduction.
Similar content being viewed by others
Background
People with mental disorders are often affected not only by symptoms but also by impairments in activities of daily living and social participation. The International Classification of Functioning, Disability and Health (ICF) of the World Health Organization [1] is a useful tool for systematically describing a person’s available functional capacities in reference to a standard environment, as opposed to recording performance in the actual environment. Regardless of the actual realisation of abilities (performance), the ICF provides a comprehensive record on the person’s capacities [2]. However, capacity impairment is not an absolute category but needs to be determined in reference to the requirements of a specific context. For example, communication problems due to social phobia may severely impair the capacity of a person to work as a teacher but not to have a job as a research assistant in a laboratory. In medical treatment settings, there is a vital interest in the assessment not only of symptoms but of functioning in order to get a detailed account of the person’s capacities affected by the disorder and draw conclusions with regards to therapy, needs for assistance and prognosis. To quantify the impairment of capacities according to ICF the “Mini-ICF Rating for Mental Disorders” (Mini-ICF-APP) was developed [2]. This rating instrument offers a set of 13 capacities that may be impaired by mental illness and are supposed to be judged in relation to the requirements of a defined context.
As already mentioned, a specific question concerns the relationship between symptoms and functioning. There is already a structural association between the diagnosis of a mental disorder and functional impairment, however. Making a diagnosis according to a standard diagnostic system like DSM-IV presupposes the presence of distinct symptoms (Criterion A) but also a marked distress or disability by the condition (Criterion B) [3]. Studies have repeatedly confirmed a positive correlation between the severity of symptoms and the degree of functional impairment [4,5,6]. Recently, Rosburg and colleagues [7] showed that patients with different psychiatric diagnoses also have different levels of functional limitations. In a mixed sample, capacity limitations increased with the severity of the symptoms, especially in patients with depressive disorders. Also the development of functional impairment during symptomatic remission has aroused interest: Collard and colleagues [8] found significant differences in functioning between remitted and non-remitted patients with depression 2 years after first diagnosis. Remarkably, functioning in remitted patients was still reduced compared to healthy controls. These results are consistent with the findings of Iancu et al. [9] who followed up a total of 914 participants with persistent, recurrent and fully remitted depression over a 6-year period. Initially, chronically depressed participants showed the most severe impairment, followed by those with recurrent and remitted depression, and all of them were more impaired than healthy controls. At follow-up, symptom improvement was associated with a reduction in impairment, but none of the diagnosed groups reached the level of the healthy controls, i.e., even in remission some impairments persisted. However, these two follow-up studies used self-reports on performance only (WHO DAS II); in contrast, the Mini-ICF-APP is an external rating of capacities that includes both self-reports and anamnestic data as well as observations during the examination situation.
For more than 10 years now, Mini-ICF-APP has proven to be a practicable, economic, reliable and valid assessment instrument for the assessment of capacity limitations. Nevertheless, literature providing detailed reports of the single items’ results in specific samples other research could refer to is sketchy. Some studies [4, 10] have rather small sample sizes (N = 120 and 74). With Rosburg et al. [7], for the first time the items’ results from a larger sample are available (n = 946), but information on long-term development of functional limitations is still missing. On the other hand, Egger et al. [5] reported data of a remarkable sample of over 3000 inpatients at admission and discharge, but he did not present the 13 single items’ results. An analysis of the single Mini-ICF-APP items with special attention to the long-term course of impairment and in relation to symptomatic remission seems to be overdue.
The aim of this study was to explore capacity impairment degrees according to the mean values of the 13 Mini-ICF-APP items in a sample of 320 psychiatric inpatients with a diagnosis of mood or anxiety disorders. In particular, we were interested in the functional impairment at admission and 1 year after discharge. Finally, we wanted to investigate possible differences in the different capacity dimensions between the symptomatically remitted and non-remitted patients.
Methods
The study was part of a comprehensive research project on Treatment Pathways of Patients with Anxiety and Depression (PfAD study) [11,12,13] that had started in 2012. Data collection ended in 2015. The overall projects’ aim was to explore the long-term development of former inpatients with comparable psychiatric diagnoses up to 1 year after discharge from different treatment settings.
Sample
For the PfAD study, 320 inpatients with an admitting primary diagnosis of the categories mood (F3) or anxiety disorders (including neurotic, stress-related and somatoform disorders) (F4) according to ICD-10 were assessed. Recruitment took place in four different psychiatric inpatient treatment settings: day clinic, two specialized units for crisis intervention and for the treatment of depression, and a psychosomatic clinic, all situated in Southern Germany. Patients diagnosed with comorbid organic, including symptomatic mental disorders (F0), schizophrenia, schizotypal and delusional disorders (F2) or mental retardation (F7) (ICD-10) were excluded. All consecutively admitted adult patients meeting the inclusion criteria were asked for participation and included in the study after given written informed consent. The recruitment stopped in each setting when a number of 80 participants has been reached. The study was approved by the ethics committee of Ulm University (number 284/11). A detailed account of the methodology of the PfAD study is provided in [13].
Design
The general framework of the PfAD study was designed to investigate the clinical course and future service use of patients with a diagnosis of mood or anxiety disorder [11]. The prospective longitudinal design of the overall study included four assessments: at the beginning and at the end of the index hospitalisation as well as 6 months and 12 months after discharge. Data gathering included self-assessments and interviews. For the present study’s aim of examining the long-term course of functional impairment in our sample, we decided to use the data assessed during index hospitalisation (baseline) and at 12 months follow-up (follow-up) (Fig. 1).
Instruments
Socio-demographic, disease-related and treatment-related data were collected using both self- and external assessments. They included age, sex, living in a partnership, less than 9 years of education, supported living, and having a job. We assessed the following clinical characteristics: age at onset of disorder, highest GAF value in the year before admission [3], duration of index hospitalisation, primary diagnosis at discharge, number of co-occurring psychiatric disorders according to the Mini International Neuropsychiatric Interview (M.I.N.I [14].) and the Structured Clinical Interview for DSM-IV, axis II Personality disorders (SCID-II [15]). Additionally, we recorded the use of outpatient and inpatient services in the year after index hospitalisation. In order to assess severity of symptoms we used the global severity index in the Brief Symptom Inventory (GSI; mean value [16]) and Beck Depression Inventory II (BDI-II; sum score [17]).
Outcome 1: functional impairment
As primary outcome, the level of functional impairment in activities and participation at baseline and at follow-up was assessed using Mini-ICF-APP [2]. This rating instrument consists of 13 items that cover a wide variety of capacities that can be affected by the mental disorder, such as adherence to regulations or flexibility, but also self-care or mobility [2]. Each item is rated on a 5-point scale: 0 = no impairment, 1 = subjective impairment, 2 = observable impairment, 3 = need for assistance, 4 = full impairment, no activity possible in this capacity. A total score can be calculated adding up the ratings of all 13 items. There are versions in German [2, 18], English [19], French [18] and Italian [4, 10]. Several studies have proved its reliability and validity in patients with various mental disorders [4, 10, 19]. The assessments were made by independent study workers not involved in the treatment of the patients. They were trained to rate the items using all available information on the participant (which included a semi-structured interview by the raters) as well as observations during the interview. The rating aimed at assessing the individual’s capacities of general social participation. Accordingly, it was conducted with reference to the individual’s general living context.
Outcome 2: symptomatic remission
Remission was defined with a cut-off value below 14 points in the BDI-II sum score [13, 17]. BDI-II sum score was chosen as outcome of remission because our assessments showed that patients with primary diagnoses of mood or anxiety disorder did not considerably differ in their baseline BDI-II scores. Regardless of the primary diagnosis, BDI-II sum scores indicated clinically relevant depressive symptoms in the entire sample.
Statistical analysis
All analyses were performed with SPSS for windows version 27. Initially, we analysed the baseline and follow-up data descriptively, and we tested for a possible attrition bias by comparing study completers (both assessments) with study non-completers. Then we analysed the difference between baseline and follow-up in the various Mini-ICF-APP dimensions (only study completers). Afterwards, we investigated possible correlations between level and quality of impairment and specific sociodemographic and clinical variables. In particular, we were interested in the associations of symptom severity (BDI-II), symptom burden (GSI) and functional impairment (Mini-ICF-APP). We examined them using correlations within and between assessment time points. We compared the mean values of the different capacity limitations in remitted and non-remitted patients. Because of multiple comparisons, we used Bonferroni adjusted p-values in all analyses.
Results
Sample characteristics
At baseline, a total of 320 inpatients participated in the study. Their mean age was 40.7 years (SD = 12.41), 60.6% were female, 42.2% lived in a partnership, and 67.4% were having a job. About 70% had a primary diagnosis of F3, 30% of F4. On average, inpatient index hospitalisation lasted 48.81 days (SD = 27.23). At admission, the mean BDI-II sum score was 30.07 (SD = 11.59), the mean GSI score was 1.61 (SD = 0.75) (Table 1).
A total of 241 participants (75%) took part in the follow-up assessment. Attrition bias was examined by comparing the socio-demographic and clinical characteristics of study completers and non-completers. Only mean age differed significantly (U = 6688.00; p < 0.001). There was no indication of an attrition bias with regard to clinical severity or other characteristics [13].
Outcome 1: Mean values of functional impairment at baseline and follow-up
The means of the total score and the 13 capacities at baseline and follow-up are displayed in Table 2. All capacities showed a significant improvement at follow-up. The items indicating the least impairment at both measurement points were self-care, mobility and adherence to regulations. The most impaired capacities at baseline (B) and follow-up (FU) included endurance (MB = 1.98 (SD = 0.96), MFU = 0.94 (SD = 0.96)), spontaneous activity (MB = 1.96 (SD = 1.09), MFU = 0.94 (SD = 1.00)), structuring of tasks (MB = 1.88 (SD = 1.04), MFU = 0.92 (SD = 0.97)), competency (MB = 1.87 (SD = 1.16), MFU = 0.84 (SD = 0.93)), and flexibility (MB = 1.82 (SD = 1.09), MFU = 0.91 (SD = 0.98)), with only minor changes in the ranks of impairment over time. At the same time, these five areas showed the greatest improvement over time. Table 2 also shows the mean changes in the completers in the Mini-ICF-APP total score and in the 13 individual items. It has to be noted that 1 year after discharge, nearly 25% (n = 53) of the sample showed no more impairment in any of the single capacities.
Correlations of Mini-ICF-APP and other characteristics
At baseline and at follow-up, there were no significant correlations of Mini-ICF-APP total score and any socio-demographic characteristics, except from employment status. At follow-up, unemployed participants showed a greater impairment score (r = − 0.319; p < 0.001; n = 238). We also examined correlations of Mini-ICF-APP total score at baseline and follow-up and the following clinical characteristics: primary diagnosis F3, total number of co-occurring diagnoses, duration of index hospitalisation, use of outpatient or inpatient services in the year after index hospitalisation. The number of comorbid diagnoses at index treatment correlated with impairment at baseline, but also at follow-up (rB = 0.208, p < 0.001, n = 319; rFU = 0.294, p < 0.001, n = 239). Participants who had used outpatient services more intensely (r = 0.209; p < 0.001; n = 228) or who had spent more days in another inpatient treatment after discharge from index hospitalisation (r = 0.364; p < 0.001; n = 229) showed higher Mini-ICF-APP scores at follow-up. Symptom severity and symptom burden were moderately associated with functioning on average (Table 3). GSI and BDI-II scores correlated significantly with Mini-ICF-APP total scores at baseline and follow-up and across assessment time points.
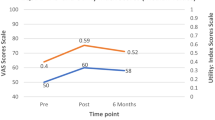
Outcome 2: Functional impairment of remitted and non-remitted patients
At follow-up, 94 (45.4%) participants met the criteria for remission according to BDI-II. Figure 2 shows that functional impairment of both remitted and non-remitted patients decreased over time. However, at baseline, the level of impairment of the later remitted and non-remitted patients was comparable. There were no significant differences except for endurance (U = 3985.00; p < 0.001). At follow-up, there were significant differences between remitted and non-remitted patients in all items (Table 4). The most heavily impaired capacities in non-remitted patients were judgement, spontaneous activity, and endurance. The main remaining limitations in remitted patients concerned judgement, flexibility and intimate relationships. However, means below 1 in Mini-ICF-APP always indicate the absence of or only small problems without the need of external assistance. The areas of self-care, adherence to regulations, and mobility played a minor role in both groups.
Discussion
Mini-ICF-APP is frequently used to assess therapeutic progress in psychiatric rehabilitation and is often applied for the assessment and prediction of a return to work. As initially stated, there are several studies on clinical samples with different psychiatric diagnoses, but often only values at hospital admission and discharge are reported. This study provides a more detailed picture of the long-term progress of formerly hospitalised patients. We examined a large and – in contrast with other studies [4, 5, 19, 20] – narrowly defined diagnostic sample of patients with mood and anxiety disorders as primary diagnoses. Participants were recruited in diverse inpatient treatment settings available in Germany. Initial severity of illness ranged from acute suicidality to full job functioning until admission. Furthermore, our follow-up 1 year after discharge from index hospitalisation adds valuable evidence to the results of former studies [5, 19].
During hospitalisation, our sample was heavily burdened by limited capacities. This is especially true for structuring of tasks, endurance, spontaneous activities, flexibility, and competency, which may be closely related to typical symptoms of acute mood and anxiety disorders. The levels of impairment were comparable to those found in outpatients with schizophrenia [10] and the participants of a multidisciplinary work disability evaluation [7], but were distinctly higher than in psychosomatic rehabilitation inpatients [21]. However, caution is advised to compare these results directly because a similar reference context for judgement of Mini-ICF-APP is necessary in order to draw valid conclusions. In some of these studies, the context is not explicitly specified; others focus primarily on working abilities [21].
However, each of these limited capacities improved after 1 year, especially those most affected. This confirms that the Mini-ICF-APP is able to measure changes and can be used to monitor therapeutic progress. The distribution of mean scores 1 year after discharge is strongly skewed, indicating high rates of complete recovery, also in terms of functional impairment. Nevertheless, a smaller fraction still needed external support in some areas due to limited abilities. The extent of improvement varied for the individual items. Therefore, it seems useful to take a close look at the individual items, i.e. 13 capacities each for itself [4, 10]. Similar to other studies [20, 22], our results indicate a strong relationship between the capacities assessed by Mini-ICF-APP and working abilities. This underlines the external validity of the instrument as a comprehensive assessment of functional capacity.
On average, there was a moderate correlation between the severity of symptoms and limitations of functioning, and symptomatic improvement appeared to be associated with functional improvement. This suggests that symptom severity varies with capacity impairment, but that, at the same time, symptoms and capacity impairments are distinct aspects of illness. At follow-up, the prevalence of symptoms was highly correlated with the level of functioning. This is a strong argument for increased therapeutic efforts to decrease the symptom severity, because at the same time this may increase functioning.
At baseline, there were no significant differences in the impairment of capacities between the later non-remitted and remitted patients, except for endurance. Both groups started at a high level of impairment and improved over time, but the symptomatically remitted patients improved considerably more. There is a fair bit of literature on persisting functional impairment even after symptomatic remission in depression [8, 9]. Some capacities recover only with a time lag after complete symptom remission, which might impede the return to everyday life. Even the mean impairment scores of our remitted subsample were not zero at the end. Thus, several remitted patients still had minor problems even when they did not need help. This is consistent with Collard and colleagues [8], who demonstrated persistent differences between remitted depressed patients and healthy controls.
Regarding the limitations of our study, our sample was limited to inpatients with mood and anxiety disorders. On the one hand, this was an opportunity to take a more detailed look at the group of inpatients with the most prevalent mental disorders (apart from substance-related disorders) in Germany [23]. On the other hand, these diagnostic categories include a heterogeneous spectrum that can range from depression to manic episodes or from specific phobias to reactions on severe stress. Although depressive episodes and anxiety were the most common diagnoses in our sample, there was still a percentage of participants with other symptoms. Thus, we may not attribute our results solely to depression and anxiety disorders but keep in mind the complete spectrum of F3 and F4 disorders according to ICD-10. Moreover, we refrain from generalizing our results to the great number of patients who suffer from anxiety or depression but have never taken advantage of inpatient treatment before. The use of BDI-II as a measure of symptomatic outcome might be criticised as it is intended to assess symptoms of depression. Self-assessment symptom scales, however, cannot be specific for recording a particular disorder. The symptoms asked about in the scales are nonspecific and may be present in many disorders (e.g., sleep, concentration, or various emotional disturbances). Self-assessment scales are therefore primarily useful for expressing patients’ self-reported levels of burden, but do not assess “diagnoses” in a strict sense. Indeed, there was considerable overlap between comorbid diagnoses in our sample [11], and the problems recorded with BDI-II were equally relevant to patients with a primary diagnosis of mood or anxiety disorders. The sample’s attrition rate during the study was considerable despite the lack of a systematic bias beyond the age variable. We cannot rule out an attrition bias in the completers due to unassessed factors. Finally, as we did not assess the functional impairment at the moment of discharge, we cannot draw any conclusion on the progress of functional recovery and the treatment effect during hospitalisation.
Conclusion
Most studies have used the Mini-ICF-APP in the context of rehabilitation and sick leave [2, 19, 20, 22]. Our study provides results and reference values of a clinical population with mood or anxiety disorders, from different inpatient treatment settings, and with different degrees of severity [11]. We have found this tool to be useful in the context of general psychiatry as well. It can be used to precisely determine capacity limitations and to support treatment planning beyond the focus on symptom reduction. We provided follow-up data over a one-year interval, after the former inpatients had returned to their “normal” life. Our results show that the Mini-ICF-APP is a valuable instrument to monitor functional status and change in psychiatric samples, both in terms of the total score and the individual items. Our reference values of symptomatically remitted and non-remitted subgroups can hopefully contribute to the future standardization of the Mini-ICF-APP, and thus also to promoting the application of the Mini-ICF-APP in clinical practice.
Availability of data and materials
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.
Change history
22 June 2022
A Correction to this paper has been published: https://doi.org/10.1186/s12888-022-04051-6
Abbreviations
- Mini-ICF-APP:
-
Mini-ICF Rating for Mental Disorders
- GAF:
-
Global Assessment of Functioning
- M.I.N.I.:
-
Mini International Neuropsychiatric Interview
- BDI-II:
-
Beck Depression Inventory II
- GSI:
-
Global severity index in the Brief Symptom Inventory
References
World Health Organisation. International classification of functioning, disability and health. Geneva: World Health Organisation; 2001.
Linden M, Baron S, Muschalla B. Mini-ICF-APP. Mini-ICF-Rating für Aktivitäts- und Partizipationsstörungen bei psychischen Erkrankungen. Ein Kurzinstrument zur Fremdbeurteilung von Aktivitäts- und Partizipationsstörungen bei psychischen Erkrankungen in Anlehnung an die Internationale Klassifikation der Funktionsfähigkeit, Behinderung und Gesundheit (ICF) der Weltgesundheitsorganisation. Bern: Huber; 2009, 2015a.
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. Washington: 4th Ed, Text Revision (DSM-IV-TR) American Psychiatric Association; 2000.
Balestrieri M, Isola M, Bonn R, Tam T, Vio A, Linden M, et al. Validation of the Italian version of Mini-ICF-APP, a short instrument for rating activity and Participation restrictions in psychiatric disorders. Epidemiol Psychiatr Sci. 2013;22(1):81–91. https://doi.org/10.1017/S2045796012000480.
Egger ST, Weniger G, Müller M, Bobes J, Seifritz E, Vetter S. Assessing the severity of functional impairment of psychiatric disorders: equipersentile linking the mini-ICF-APP and CGI. Health Qual Life Outcomes. 2019;17:174. https://doi.org/10.1186/s12955-019-1235-5.
Braunger C, Müller G, von Wietersheim J, Oster J. Veränderung der Symptombelastung und der Funktionsfähigkeit gemäß ICF in der stationären psychosomatischen Rehabilitation. Die Rehabilitation. 2019;58(01):24–30. https://doi.org/10.1055/s-0043-124308.
Rosburg T, Kunz R, Trezzini B, Schwegler U, Jeger J. The assessment of capacity limitations in psychiatric work disability evaluations by the social functioning scale Mini-ICF-APP. BMC Psychiatry. 2021;21:480. https://doi.org/10.1186/s12888-021-03467-w.
Collard RM, Wassink VS, Schene AH, Naarding P, Verhaak P, Voshaar RCO, et al. Symptomatic and functional recovery in depression in later life. Soc Psychiatry Psychiatr Epidemiol. 2018;53(1071–1079). https://doi.org/10.1007/s00127-018-1540-z.
Iancu SC, Wong YM, Rhebergen D, van Balkom AJLM, Batelaan NM. Long-term disability in major depressive disorder: a 6-year follow-up study. Psychol Med. 2020;50(10):1644–52. https://doi.org/10.1017/S0033291719001612.
Pinna F, Fiorillo A, Tusconi M, Guiso B, Carpiniello B. Assessment of functioning in patients with schizophrenia and schizoaffective disorder with the Mini-ICF-APP: a validation study in Italy. Int J Ment Health Syst. 2015;9:37. https://doi.org/10.1186/s13033-015-0030-x.
Bichescu-Burian D, Cerisier C, Czekaj A, Grempler J, Hund S, Jaeger S, et al. Patienten mit Störungen nach ICD-10 F3 und F4 in Psychiatrie und Psychosomatik – wer wird wo behandelt? Merkmale der Zuweisung aus der PfAD Studie. Nervenarzt. 2017;88:61–9. https://doi.org/10.1007/s00115-015-0058-9.
Bichescu-Burian D, Jaeger S, Steinert T, Uhlmann C, Flammer E. Poststationäre Weiterbehandlung von Patienten mit ICD-Diagnosen F3 und F4 in Psychiatrie und Psychosomatik. Psychiatr Prax 2021 (epub). https://doi.org/10.1055/a-1349-6257.
Uhlmann C, Jaeger S, Steinert T, Schmid P. Erkrankungsverläufe depressiver und Angststörungen über ein Jahr - Direkter Vergleich von vier Behandlungssettings in Psychiatrie und Psychosomatik - Ergebnisse der PfAD-Studie. Nervenarzt. 2021;92:468–78. https://doi.org/10.1007/s00115-020-00980-3.
Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(Suppl 20):22–33 (quiz34–57).
Wittchen H-U, Zaudig M, Fydrich T. SKID-Strukturiertes Klinisches Interview für DSM-IV. Göttingen: Hogrefe; 1997.
Franke GH. BSI. Brief Symptom Inventory –Deutsche Version. Manual Göttingen: Beltz. 2000.
Hautzinger M, Keller F, Kühner C. BDIII. Beck-Depressions-Inventar. Revision, 13. Aufl: Frankfurt: Pearson Assessment; 2009.
Linden M, Baron S, Muschalla B. Mini-ICF-APP Mini-ICF-Rating für Aktivitäts- und Partizipationsstörungen bei psychischen Erkrankungen Kurzinstrument zur Fremdbeurteilung von Aktivitäts- und Partizipationsstörungen bei psychischen Erkrankungen in Anlehnung an die Internationale Klassifikation der Funktionsfähigkeit, Behinderung und Gesundheit (ICF) der Weltgesundheitsorganisation Ankerdefinitionen. Göttingen: Hogrefe; 2015b.
Molodynski A, Linden M, Juckel G, Yeeles K, Anderson C, Vazquez-Montes M, et al. The reliability, validity, and applicability of an English language version of the Mini-ICF-APP. Soc Psychiatry Psychiatr Epidemiol. 2013;48:1347–54. https://doi.org/10.1007/s00127-012-0604-8.
Linden M, Baron S, Muschalla B. Relationship between Work-Related Attitudes, Performance and Capacities according to the ICF in Patients with Mental Disorders. Psychopathology. 2010;43:262–7. https://doi.org/10.1159/000315125.
Baron S, Linden M. Wirksamkeitsanalyse einer stationären psychosomatischen Rehabilitation anhand des Mini-ICF-APP. [Analyzing the Effectiveness of Inpatient Psychosomatic Rehabilitation Using the Mini-ICF-APP]. Rehabilitation. 2009;48(145–153). https://doi.org/10.1055/s-0029-1220740.
Habermeyer B, Kaiser S, Kawohl W, Seifritz E. Rentenrelevante Arbeitsunfähigkeit und Mini-ICF-APP. Neuropsychiatr. 2017;31(4):182–6. https://doi.org/10.1007/s40211-017-0246-x.
Jacobi F, Höfler M, Strehle J, Mack S, Gerschler A, Scholl L, et al. Psychische Störungen in der Allgemeinbevölkerung. Studie zur Gesundheit Erwachsener in Deutschland und ihr Zusatzmodul “Psychische Gesundheit” DEGS1-MH. Nervenarzt. 2014;85:77–87.
Acknowledgements
The authors would like to thank all study participants. We would also like to thank Gerd Weithmann, Julia Grempler, Agata Czekaj, Christina Cerisier, and Susi Hund for their contributions to study conception, material preparation and data collection, and Peter Schmid for programming the database.
Funding
Open Access funding enabled and organized by Projekt DEAL. The study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
All authors, SJ, CU, PS, DBB, EF and TS, contributed substantially to the study conception and design. DBB contributed to the acquisition of data. PS did the statistical analysis. SJ, PS and CU interpreted the data, wrote and revised the manuscript. All authors commented on previous versions and revisions of the manuscript. All authors read and approved the final manuscript
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Data analysis was performed with the approval of the ethics committee of the University of Ulm (vote of December 09, 2011, no. 284–11). All methods were performed in accordance with the relevant guidelines and regulations. Written informed consent was obtained from each participant.
Consent for publication
Not applicable.
Competing interests
The authors declare that there are no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original version of this article was revised: the names have been updated.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Jaeger, S., Uhlmann, C., Bichescu-Burian, D. et al. One-year follow-up of functional impairment in inpatients with mood and anxiety disorders – Potentials of the Mini-ICF-APP. BMC Psychiatry 22, 334 (2022). https://doi.org/10.1186/s12888-022-03977-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12888-022-03977-1