Abstract
Background
The role of Interleukin-1 Receptor antagonist (IL-1Ra), an innate antagonist to pro-inflammatory cytokine IL-1, has attracted increasing attention due to its potential pathogenic and therapeutic implications in depression. However, the role of alcohol and adiposity in modulating IL-1Ra cytokine pathway in depressed patients has remainned unknown. The aim of this study was to follow the changes in IL-1Ra serum levels in depressed patients with or without simultaneous alcohol use disorder (AUD) and different degrees of adiposity during 6 months of follow-up.
Materials and methods
A total of 242 patients with depression were followed for 6 months. At baseline 99 patients had simultaneous AUD. Levels of serum IL-1Ra and common mediators of inflammation (IL-6, hs-CRP) were measured. Clinical assessments included Body Mass Index (BMI), Montgomery-Asberg Depression Rating Scale (MADRS) and Alcohol Use Disorders Identification Test (AUDIT) scores.
Results
Significant reductions in clinical symptoms and IL-1Ra were observed during 6-month follow-up. In hierarchical linear regression analysis, the effect of MADRS score, age, gender, and smoking had a combined effect of 2.4% in the model. The effect of AUDIT score increased the effect to 4.2% of variance (p = 0.08), whereas adding BMI increased the effect to 18.5% (p < 0.001).
Conclusion
Adiposity may influence the IL-1Ra anti-inflammatory response in depressed patients, whereas the effect of alcohol consumption in these patients seems insignificant. These findings should be considered in studies on the role of IL-1Ra in depression.
Trial registration
Ostrobothnia Depression Study in ClinicalTrials.gov , Identifier NCT02520271.
Similar content being viewed by others
Background
Major depressive disorder (MDD) is one of the leading causes of disability worldwide (WHO), and accumulating evidence suggests participation of activated immune-inflammatory pathways in the onset of depression [1,2,3]. Several studies have reported elevated levels of inflammatory mediators in patients with depression, as summarized in a recent review by Köhler et al. [4], and in translational models the administration of pro-inflammatory cytokines has been shown to induce depression-like symptoms [5]. Also, a persistent inflammatory state has been suggested to have a role in treatment-resistant depression [6, 7].
Interleukin I (IL-1) is a crucial mediator of the inflammatory response, playing an important role in the development of pathological conditions leading to inflammation. Currently a total of 11 members of the IL-1 family have been indentified, most importantly pro-inflammatory cytokines IL-1α and IL-1 β [8, 9]. IL-1 receptor antagonist (IL-1Ra) is synthesized and released in response to the same stimuli as IL-1, as a compensatory mechanism to attenuate inflammatory reaction [10]. Binding of IL-1Ra to IL-1 receptor inhibits signaling of IL-1, making IL-1Ra one of the most potent anti-inflammatory mediators [11].
Several studies have indicated significant associations between elevated serum IL-1 [12, 13] as well as IL-1Ra and depression [14,15,16,17]. Additionally, levels of IL-1 have been suggested to increase or to show failure to normalize in patients with persistent depressive symptoms despite medical treatment [15, 18,19,20]. Elevated levels of IL-1Ra have also been found in patients with treatment-resistant depression [15], but this association has not been confirmed.
Although alcohol use disorder (AUD) is an extremely common co-morbidity with depression [21], the question whether excessive alcohol drinking affects levels of IL-1Ra and patient recovery in depressed patients has remained unknown. Previous studies have reported compensatory increase in levels of IL-1Ra in response to pro-inflammatory state produced by AUD in pulmonary disease [22], and a potential use of IL-1Ra recombinant in the treatment of alcohol induced liver disease has been suggested [23]. However, a recent study by Bjorkhaug et al. [24] found no significant changes in levels of IL-1Ra in men with AUD, and these authors concluded that patients with AUD showed a cytokine profile suggestive of increased overall pro-inflammatory activity.
Adipose tissue is a substantial source for IL-1Ra secretion [25], and obesity has been shown to correlate with increased peripheral levels of IL-1Ra [24, 26]. In addition, cytokines in depressed patients are commonly expressed in a gender-dependent manner [27]. Although a large, population-based study recently reported elevated levels of IL-1Ra in males with depressive symptoms [28], the role of gender in the expression of IL-1Ra in psychiatric disorders has remained elusive.
While a putative role of IL-1Ra in depression has been suggested, there is inconsistency in findings of serum IL-1 or IL-1Ra levels in depressed patients with or without comorbidities such as alcohol use disorder (AUD), or with differing degrees of adiposity. Therefore, we explored changes in serum levels of IL-1Ra during a six-month follow-up of depressed patients with or without simultaneous AUD and with or without excess body weight.
Methods
Study design and participants
Patients were recruited between 2009 and 2013 from five psychiatric outpatient clinics and from one Finnish psychiatric hospital in the South Ostrobothnia Hospital District (population 200,000), in total 242 participants. Patients were suffering from depressive symptoms and possible co-morbid anxiety, self-destructiveness, insomnia or alcohol or other substance related problems.
Inclusion criterion for the study was clinical depression. The depressive state of all patients was assessed with the Beck Depression Inventory (BDI, version 1A). Patients with a BDI score ≥ 17 at the screening phase were consequently considered to be at least moderately depressed and were included in the study [29]. Exclusion criteria were primary diagnosis of psychotic disorders (ICD-10 codes F20–29), or organic brain disease or damage. The study was approved by the local ethics committee and all participants provided written informed consent. The study protocol is outlined and published at Ostrobothnia Depression Study in ClinicalTrials.gov, Identifier NCT02520271; first posted date 11/08/2015, and by Archer et al. [30]. The study protocol is described in detail: https://www.clinicaltrials.gov/ct2/show/NCT02520271?term=ODS&draw=2&rank=1.
At baseline, The Mini International Neuropsychiatric Interview 5.0 (MINI) diagnosis was available for 219 patients. However, all patients in this study were classified as depressed when evaluated with the BDI questionnaire. The baseline assessment for all patients included BDI-21, Montgomery-Åsberg Depression Rating Scale (MADRS), AUDIT-10 (Alcohol Use Disorders Identification Test) and additional questions about alcohol use following a timeline follow-back method (amounts per week, duration of harmful drinking). Patients also completed up a questionnaire on substance use other than alcohol from the past 12 months prior to the study. Since the number of patients with co-morbid substance use was relatively small (twenty patients in the AUD group and two patients in the non-AUD group), this was not chosen as an exclusion criterion for the study. Smoking status was also recorded based on patient self-reporting.
The clinical assessment included measurement of body mass index (BMI), and waist circumference to the nearest 0.5 cm obtained from the measurements between the lowest rib and iliac crest while the study subject was at minimal respiration. The clinical assessments were performed by a psychiatrist or a research nurse with long experience in the field of psychiatry and appropriate methodological training.
Participants were divided into two groups according to the baseline AUDIT-score, where patients with ≥11 AUDIT points were categorized as MDD + AUD. The WHO guidelines for AUDIT use in primary care [31] state that selection of cut-off point should be dependent on national and cultural standards, and in Finnish clinical practice with AUD patients, AUDIT score ≥ 11 points is considered to indicate significantly increased risk of harmful alcohol consumption. A concordance of 88% in AUDIT score and substance use disorder assessed with M.I.N.I. has been previously reported in this patient sample [32], confirming reliability of AUDIT score as an indicator of alcohol use disorder. All data were analyzed between study groups and between genders, where gender groups were formed based on the sex assigned at birth.
The selection of the therapeutic treatment intervention was based on the baseline levels of alcohol use measured with AUDIT score and included behavioral activation therapy for all patients of this study and, additionally, motivational interview (MI) for patients with co-morbid alcohol use disorder (AUD). Use of medication was based on psychiatrist’s estimation, and the study protocol did not guide the choice of the pharmaceutical agent. Nonetheless, evaluation of the effectiveness and possible adjustments of medication were recommended when MADRS score exceeded 19 points at baseline. Data on medications taken before entering this study was not available. However, all patients were referred to psychiatric specialty unit following initial treatment period in general health services following the recommendations given in the Current Care Guidelines of Finland, with a requirement of medication attempt prior to referral. For statistical purposes all anti-depressant medications were converted-to equivalent doses of fluoxetine, and anti-psychotic medications to equivalent doses of chlorpromazine. Data on medication adherence was acquired from the medical records and by keeping paper-and-pencil diaries during the first 6 weeks of the study.
The number of visits during the study period varied based on the requirements of care for each patient. Six-month follow-up appointment included a visit to a research nurse, which included the assessment of the severity of depression with MADRS score and gathering information on alcohol use using the AUDIT questionnaire and analyses of blood biomarkers. Also, weight and waist circumference were measured, and BMI calculated.
Laboratory assays
Venous blood samples were drawn from each subject at baseline and at 6 months. The patients did not have specific appointment to the laboratory, but due to the operating hours of the regional laboratory services, the samples were obtained in the morning. Serum was separated by centrifugation and stored at − 80 °C prior to analysis. Serum IL-1Ra concentration was measured by Quantikine high sensitivity enzyme-linked immunosorbent assay (ELISA) (R&D Systems Europe, Abingdon, UK). The detection limit and the interassay coefficient of variation were 15.6 pg/ml and 7.4%, respectively. High Sensitivity CRP (hs-CRP) was measured using particle-enhanced immunoturbidimetric method on an automated clinical chemistry analyzer (Roche Diagnostics, Basel, Switzerland). Concentration of serum IL-6 was determined using Quantikine high sensitivity ELISA kit according to the instructions of the manufacturer (R&D Systems, Abington Science Park, UK).
Statistics
The data are reported as mean ± SD. The laboratory parameters showed a tendency towards lognormal distributions, although meeting the limits of normality, with the exception of 2–8 outliers per studied variable. To obtain non-skewed distributions with homogeneity of variance the data were transformed into + 2.5 SD levels as previously described by Miller [33]. Q-Q plots were drawn for all experimental laboratory tests, showing normality of distributions.
Comparison of means between genders and between patients with depression or depression + AUD were analyzed with independent samples t-test at baseline and after 6 months of treatment.
To analyze the association of baseline IL-1Ra levels and confounding factors hierarchical linear regression analyses were performed. The model was adjusted for MADRS score, age, gender, and regular smoking, whereas the effect of baseline AUDIT score was added at step two and BMI at step three of the analysis.
A linear mixed model for repeated measures was used to predict changes in IL-1Ra during the follow-up from baseline to 6 months with various possible confounding factors (gender, AUD status, smoking, severity of MDD estimated by MADRS score, age, BMI, and interaction terms time*AUD, and time *MADRS).
Pearson’s correlation coefficient was used to calculate correlations between known inflammatory biomarkers IL-6 and hs-CRP and anti-inflammatory IL-1Ra at baseline.
Results
The main characteristics of the study population are summarized in Table 1
A significant reduction of depressive symptoms was observed in all study groups during six-month follow-up (p < 0.001 for men and women, AUD and non-AUD). BMI increased in all study groups during the follow-up period, + 1.8% in women and + 3.3% in men (p < 0.05); + 1.2% in non-AUD and + 4.3% in AUD groups (p < 0.05).
Effect of gender and AUD on levels of serum IL-1Ra
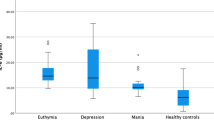
The levels of IL-1Ra changed during the six-month follow-up in all study groups, the mean concentration of all groups combined at baseline was 764 pg/ml, and at six-months 670 pg/ml (p = 0.05).
At baseline, the effect of gender on the levels of IL-1Ra was insignificant (t = 1.745; 95%CI -20.67 – 339.46; p = 0.08), as was in cases with alcohol use (t = 0.008; 95%CI -180.24 – 181.74; p = 0.99). After 6 months of treatment, the effect of gender and alcohol use remained insignificant (t = 0.881; 95%CI -97.09 - 252.74; p = 0.38 for gender, and t = 1.03; 95%CI -85.80 – 273.57; p = 0.30 for alcohol use).
Association of severity of depression, smoking, adiposity, and excessive alcohol use on levels of serum IL-1Ra at baseline
Hierarchical linear regression analysis was used to assess factors affecting levels of IL-1Ra at baseline. The effect of MADRS score, age, gender, and regular smoking was adjusted, having a combined effect of only 2.4% in the model (F = 0.96; p = 0.43). The effect of AUDIT score increased the effect to 4.2% of variance (F = 3.08; p = 0.08). Adding BMI into the model increased the effect to 15.3% of variance (F = 27.38; p < 0.001). These results are presented in detail in Table 2.
Association of confounding factors with changes in the serum IL-1Ra levels during 6-months follow-up
In the linear mixed model for repeated measures analysis, we found levels of IL-1Ra to decrease during the study period (F = 10.38; p = 0.002). The effect of gender and smoking was insignificant, but adiposity at baseline (F = 46.99; p < 0.001) and age (F = 145.45; p = 0.036) had a significant effect on levels of IL-1Ra at 6 months follow-up. The effect of the interaction term time*MADRS was also significant (F = 8.11; p = 0.005). These results are presented in detail in Table 3.
Correlation of serum IL-1Ra with inflammatory biomarkers IL-6 and hs-CRP
A significant correlation of IL-1Ra and IL-6 at baseline was observed in women (r = 0.45; p < 0.001), in the non-AUD group (r = 0.42; p < 0.001) and in the AUD group (r = 0.31; p = 0.004), but not in men (r = 0.20; p = 0.07).
The correlation of IL-1Ra and hs-CRP at baseline was significant in women (r = 0.23; p = 0.01), men (r = 0.22; p = 0.05) and non-AUD (r = 0.29; p = 0.01) but not in the AUD group (r = 0.17; p = 0.13).
Discussion
Our study including 242 depressed patients indicates significant reductions in both depressive symptoms and levels of IL-1Ra during a six-month follow-up. The effect of AUD remained insignificant in relation to serum levels of IL-1Ra, whereas levels of IL-1Ra were found to be affected by adiposity.
Previous studies have emphasized the need for novel biomarkers to help detect processes in recovery of depression. All patients in this study were suffering from clinically significant depression, and we have previously reported a decrease in the depressive symptoms in all study groups during the 6 months follow-up [30]. We have also previously observed elevated serum levels in biomarkers of inflammation in depressed patients, and that the levels of these biomarkers appear to decrease during treatment [30].
Excessive ethanol consumption has been shown to play a key role in altering levels of cytokines and other mediators of inflammation in a variety of tissues [34, 35]. A recent review and meta-analysis by Adams et al. [36], reported increased concentrations of cytokines in AUD patients when comparing to healthy control. Furthermore, the levels of circulating cytokines have been found to be affected by the stage of illness [36]. Also, IL-1 receptor signaling has recently been suggested as an important player in the development of alcohol dependence, and as a key regulator of various neuroimmune responses [37]. Research has indicated elevated IL-1 and IL-1Ra levels in response to alcohol consumption [38], and Neupane et al. [39] have presented an experimental study where binge drinking induced elevated IL-1Ra levels in healthy volunteers. In light of previous studies, the assumption regarding the effect of AUD on IL-1Ra levels was justifiable, yet, based on our findings, one might suggest that anti-inflammatory response to alcohol consumption could be altered in this patient population. To the best of our knowledge, the present study is the first to examine changes in serum IL-1Ra levels in light of alcohol consumption in patients with depression, a clinically important subgroup of depressed population. When the correlation of IL-1Ra with other inflammatory biomarkers was compared between the AUD and non-AUD groups of this study, there was a strong correlation between serum levels of IL-1Ra and IL-6 in the non-AUD but not in the AUD group, thereby supporting the assumption that alcohol may modulate the mechanisms regulating the balance between pro- and anti-inflammatory response in depressed patients.
A wide array of previous studies have presented the inflammatory effect of adipose tissue in patients with depression [40, 41], and adipose tissue has also been reported to function as a major source of commonly known pro-inflammatory biomarkers such as IL-6 [42]. Therefore, the levels of IL-1Ra may rather express the ongoing inflammatory condition in depressed patients, than demonstrate the direct relation of increased adiposity.
Since smoking or alcohol use had no direct effect on serum IL-1Ra levels, we utilized linear mixed model to examine factors contributing to the change, using the combined effect of follow-up time and detected AUD as well as the effect of follow-up time and MADRS to represent the effects of a given variable on changes in levels of serum IL-1Ra over time. Gender and smoking did not affect the levels of IL-1Ra, but body adiposity had a significant effect, which corroborates existing knowledge of adipose tissue as a significant source of IL-1Ra. Even in this analysis, AUD or the combined effect of time and AUD had no significant effect on the change in IL-1Ra serum levels, whereas the severity of depressive symptoms measured as MADRS scores, and its interaction with the time variable had a significant effect.
The role of IL-1Ra in depression has recently attracted growing interest together with the development of anti-cytokine medications. It is widely acknowledged that only a part of depressed patients benefit from the present anti-depressive medications, and these findings have led to novel theories of treating depression with anti-inflammatory agents. A recent meta-analysis of the effects of anti-cytokine treatments for depressive symptoms by Kappelmann et al. [43] suggested improvement of depressive symptoms in patients treated with anti-cytokine agents adalimumab, etanercept, infliximab and tocilizumab, independent of changes in primary physical condition. In a study by Raison et al. [44], anti-TNF-α antibody infliximab was shown to have a significant effect on decreasing depressive symptoms in patients previously not responding to medication. IL-1Ra recombinant anakinra has been recently suggested as a novel biological response modifier drug for autoimmune inflammation [45] and the importance of controlling the effects of pro-inflammatory IL-1 with this molecule has also been suggested in psychiatric morbidities [46]. Determining and identifying potential subgroups of patients benefiting from this targeted treatment requires further investigation.
Strengths and limitations
The strength of this study lies in the naturalistic setting, with an interface to the clinical reality faced by psychiatrists. We assessed a clinically relevant dilemma in depression, where it is still widely unknown which patients are resistant to treatment, and what biological mechanisms could explain this. Substance use has hitherto been an exclusion criterion in many studies on depression, yet in this study we have specifically aimed to assess the role of alcohol consumption in biochemical changes observed in depression. Also, presenting longitudinal data, as we have done in this report, adds valuable information to the literature on depression.
The limitation of this study is the absence of a healthy, non-depressed study group. Nevertheless, this should not compromise the conclusions: the study parameters have been separately studied in several earlier reports. The extent of alcohol consumption was assessed by methods relying on self-evaluation. Yet we have previously reported a significant correlation between self-reports and blood biomarkers of alcohol use in this study sample and can therefore confirm the accuracy in the assessment of alcohol use [47].
Conclusions
Our data suggests that effects of adiposity markedly influences IL-1Ra anti-inflammatory response in patients with depression, whereas the direct immunomodulatory effect of alcohol consumption on IL-1Ra appears limited.
Availability of data and materials
The datasets generated and analyzed during the current study are not publicly available due to data containing sensitive information but are available from the corresponding author on reasonable request.
Abbreviations
- AUD :
-
Alcohol Use Disorder
- AUDIT:
-
Alcohol Use Disorders Identification Test
- BMI:
-
Body Mass Index
- hs-CRP:
-
High Sensitivity C-reactive Protein
- ICD-10:
-
International Statistical Classification of Diseases and Related Health Problems 10
- IL-1:
-
Interleukin 1
- IL-1Ra:
-
Interleukin 1 Receptor Antagonist
- IL-6:
-
Interleukin 6
- MADRS:
-
Montgomery Åsberg Depression Rating Scale
- MDD:
-
Major Depressive Disorder
- MI:
-
Motivational Interview
- MINI:
-
The Mini International Neuropsychiatric Interview
- TNF- α:
-
Tumor Necrosis Factor Alpha
- WHO:
-
World Health Organization
References
Dantzer R, O'Connor JC, Freund GG, Johnson RW, Kelley KW. From inflammation to sickness and depression: when the immune system subjugates the brain. Nat Rev Neurosci. 2008;9(1):46–56.
Raison CL, Capuron L, Miller AH. Cytokines sing the blues: inflammation and the pathogenesis of depression. Trends Immunol. 2006;27:24–31.
Yuan N, Chen Y, Xia Y, Dai J, Liu C. Inflammation-related biomarkers in major psychiatric disorders: a cross-disorder assessment of reproducibility and specificity in 43 meta-analyses. Transl Psychiatry. 2019;9(1):233.
Köhler CA, Freitas TH, Maes M, de Andrade NQ, Liu CS, Fernandes BS, et al. Peripheral cytokine and chemokine alterations in depression: a meta-analysis of 82 studies. Acta Psychiatr Scand. 2017;135(5):373–87.
Yirmiya R. Endotoxin produces a depressive-like episode in rats. Brain Res. 1996;711(1–2):163–74.
Beurel E, Toups M, Nemeroff CB. The Bidirectional Relationship of Depression and Inflammation: Double Trouble. Neuron. 2020;107(2):234–56.
Strawbridge R, Arnone D, Danese A, Papadopoulos A, Herane Vives A, Cleare AJ. Inflammation and clinical response to treatment in depression: A meta-analysis. Eur Neuropsychopharmacol. 2015;25(10):1532–43.
Akdis M, Burgler S, Crameri R, Eiwegger T, Fujita H, Gomez E, et al. Interleukins, from 1 to 37, and interferon-γ: receptors, functions, and roles in diseases. J Allergy Clin Immunol. 2011;127(3):701–21.e1–70.
Dinarello CA. Interleukin-1 in the pathogenesis and treatment of inflammatory diseases. Blood. 2011;117(14):3720–32.
Maes M, Berk M, Goehler L, Song C, Anderson G, Gałecki P, et al. Depression and sickness behavior are Janus-faced responses to shared inflammatory pathways. BMC Med. 2012;29(10):66.
Dinarello CA. Immunological and inflammatory functions of the interleukin-1 family. Annu Rev Immunol. 2009;27:519–50.
Howren MB, Lamkin DM, Suls J. Associations of depression with C-reactive protein, IL-1, and IL-6: a meta-analysis. Psychosom Med. 2009;71(2):171–86.
Dowlati Y, Herrmann N, Swardfager W, Liu H, Sham L, Reim EK, et al. A meta-analysis of cytokines in major depression. Biol Psychiatry. 2010;67(5):446–57.
Maes M, Vandoolaeghe E, Ranjan R, Bosmans E, Bergmans R, Desnyder R. Increased serum interleukin-1-receptor-antagonist concentrations in major depression. J Affect Disord. 1995;36(1–2):29–36.
Maes M, Bosmans E, De Jongh R, Kenis G, Vandoolaeghe E, Neels H. Increased serum IL-6 and IL-1 receptor antagonist concentrations in major depression and treatment resistant depression. Cytokine. 1997;9(11):853–8.
Rief W, Pilger F, Ihle D, Bosmans E, Egyed B, Maes M. Immunological differences between patients with major depression and somatization syndrome. Psychiatry Res. 2001;105(3):165–74.
Milaneschi Y, Corsi AM, Penninx BW, Bandinelli S, Guralnik JM, Ferrucci L. Interleukin-1 receptor antagonist and incident depressive symptoms over 6 years in older persons: the InCHIANTI study. Biol Psychiatry. 2009;65(11):973–8.
Baune BT, Dannlowski U, Domschke K, Janssen DG, Jordan MA, Ohrmann P, et al. The interleukin 1 beta (IL1B) gene is associated with failure to achieve remission and impaired emotion processing in major depression. Biol Psychiatry. 2010;67(6):543–9.
Lindqvist D, Janelidze S, Hagell P, Erhardt S, Samuelsson M, Minthon L, et al. Interleukin-6 is elevated in the cerebrospinal fluid of suicide attempters and related to symptom severity. Biol Psychiatry. 2009;66(3):287–92.
Yoshimura R, Hori H, Ikenouchi-Sugita A, Umene-Nakano W, Ueda N, Nakamura J. Higher plasma interleukin-6 (IL-6) level is associated with SSRI- or SNRI-refractory depression. Prog Neuropsychopharmacol Biol Psychiatry. 2009;33(4):722–6.
DeVido JJ, Weiss RD. Treatment of the depressed alcoholic patient. Curr Psychiatry Rep. 2012;14(6):610–8.
O'Halloran EB, Curtis BJ, Afshar M, Chen MM, Kovacs EJ, Burnham EL. Alveolar macrophage inflammatory mediator expression is elevated in the setting of alcohol use disorders. Alcohol. 2016;50:43–50.
Mathews S, Gao B. Therapeutic potential of interleukin 1 inhibitors in the treatment of alcoholic liver disease. Hepatology. 2013;57(5):2078–80.
Bjørkhaug ST, Neupane SP, Bramness JG, Aanes H, Skar V, Medhus AW, et al. Plasma cytokine levels in patients with chronic alcohol overconsumption: Relations to gut microbiota markers and clinical correlates. Alcohol. 2020;85:35–40.
Juge-Aubry CE, Somm E, Giusti V, Pernin A, Chicheportiche R, Verdumo C, et al. Adipose tissue is a major source of interleukin-1 receptor antagonist: upregulation in obesity and inflammation. Diabetes. 2003;52(5):1104–10.
Ballak DB, Stienstra R, Tack CJ, Dinarello CA, van Diepen JA. IL-1 family members in the pathogenesis and treatment of metabolic disease: Focus on adipose tissue inflammation and insulin resistance. Cytokine. 2015;75(2):280–90.
Bekhbat M, Neigh GN. Sex differences in the neuro-immune consequences of stress: Focus on depression and anxiety. Brain Behav Immun. 2018;67:1–12.
Ovaskainen Y, Koponen H, Jokelainen J, Keinänen-Kiukaanniemi S, Kumpusalo E, Vanhala M. Depressive symptomatology is associated with decreased interleukin-1 beta and increased interleukin-1 receptor antagonist levels in males. Psychiatry Res. 2009;167(1–2):73–9.
Beck AT, Steer RA, Manual for the Beck Depression Inventory. San Antonio. TX: The Psychological Corporation; 1993.
Archer M, Niemelä O, Luoto K, Kultti J, Hämäläinen M, Moilanen E, et al. Status of inflammation and alcohol use in a 6-month follow-up study of patients with major depressive disorder. Alcohol. 2019 Dec;81:21–6.
Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. AUDIT - The Alcohol Use Disorders Identification Test, guidelines for use in primary care. World Health Organization, Department of Mental Health and Substance Dependence. 2001. http://apps.who.int/iris/bitstream/10665/67205/1/WHO_MSD_MSB_01.6a.pdf
Archer M, Niemelä O, Hämäläinen M, Moilanen E, Leinonen E, Kampman O. The effects of adiposity and alcohol use disorder on adipokines and biomarkers of inflammation in depressed patients. Psychiatry Res. 2018;264:31–8.
Miller J. Reaction time analysis with outlier exclusion: bias varies with sample size. Q J Exp Psychol A. 1991;43(4):907–12.
Crews FT, Bechara R, Brown LA, Guidot DM, Mandrekar P, Oak S, et al. Cytokines and alcohol. Alcohol Clin Exp Res. 2006;30(4):720–30.
Achur RN, Freeman WM, Vrana KE. Circulating cytokines as biomarkers of alcohol abuse and alcoholism. J Neuroimmune Pharmacol. 2010;5(1):83–91.
Adams C, Conigrave JH, Lewohl J, Haber P, Morley KC. Alcohol use disorder and circulating cytokines: A systematic review and meta-analysis. Brain Behav Immun. 2020;89:501–12.
Marshall SA, Casachahua JD, Rinker JA, Blose AK, Lysle DT, Thiele TE. IL-1 receptor signaling in the basolateral amygdala modulates binge-like ethanol consumption in male C57BL/6J mice. Brain Behav Immun. 2016;51:258–67.
Bell S, Mehta G, Moore K, Britton A. Ten-year alcohol consumption typologies and trajectories of C-reactive protein, interleukin-6 and interleukin-1 receptor antagonist over the following 12 years: a prospective cohort study. J Intern Med. 2017;281(1):75–85.
Neupane SP, Skulberg A, Skulberg KR, Aass HC, Bramness JG. Cytokine Changes following Acute Ethanol Intoxication in Healthy Men: A Crossover Study. Mediators Inflamm. 2016;2016:3758590.
Capuron L, Lasselin J, Castanon N. Role of Adiposity-Driven Inflammation in Depressive Morbidity. Neuropsychopharmacology. 2017;42(1):115–28.
Himmerich H, Patsalos O, Lichtblau N, Ibrahim MAA, Dalton B. Cytokine Research in Depression: Principles, Challenges, and Open Questions. Front Psychiatry. 2019;7(10):30.
Fantuzzi G. Adipose tissue, adipokines, and inflammation. J Allergy Clin Immunol. 2005;115(5):911–9. quiz 920
Kappelmann N, Lewis G, Dantzer R, Jones PB, Khandaker GM. Antidepressant activity of anti-cytokine treatment: a systematic review and meta-analysis of clinical trials of chronic inflammatory conditions. Mol Psychiatry. 2018;23(2):335–43.
Raison CL, Rutherford RE, Woolwine BJ, Shuo C, Schettler P, Drake DF, et al. A randomized controlled trial of the tumor necrosis factor antagonist infliximab for treatment-resistant depression: the role of baseline inflammatory biomarkers. JAMA Psychiatry. 2013;70(1):31–41.
Mertens M, Singh JA. Anakinra for rheumatoid arthritis: a systematic review. J Rheumatol. 2009;36(6):1118–25.
Maes M, Song C, Yirmiya R. Targeting IL-1 in depression. Expert Opin Ther Targets. 2012;16(11):1097–112.
Archer M, Kampman O, Bloigu A, Bloigu R, Luoto K, Kultti J, et al. Assessment of alcohol consumption in depression follow-up using self-reports and blood measures including inflammatory biomarkers. Alcohol Alcohol. 2019;54(3):243–50.
Acknowledgements
The authors express their warmest thanks to Antti Koivukangas, MD, PhD, Antero Lassila, MD, PhD, and research nurses Susanna Ahola, RN, Marja Koivumäki, RN, and Kati Huhtala, RN, and to all participating units for their collaboration during the study. Ms. Terhi Salonen, Mrs. Salla Hietakangas and Mrs. Taana Sandman are gratefully acknowledged for excellent technical assistance.
Funding
This work was supported by a grant from the Finnish Alcohol Research Foundation, funds from Seinäjoki Hospital District Research Fund (EVO1114) and the competitive research funding of Tampere University Hospital, Tampere, Finland. These sources of funding were not involved in observation, commenting or guidance of scientific protocols or reporting of results.
Author information
Authors and Affiliations
Contributions
MA; study design, statistical analysis, manuscript preparation. MH, EM; laboratory methodology design and analysis. ON, EL, OK; study design, supervising, reviewing and editing the manuscript. All authors have approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the local ethics committee (The ethical committee of South Ostrobothnia Hospital District) and all participants provided written informed consent. All ethical aspects of this study follow the guidelines in the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Archer, M., Niemelä, O., Hämäläinen, M. et al. The role of alcohol use and adiposity in serum levels of IL-1RA in depressed patients. BMC Psychiatry 22, 158 (2022). https://doi.org/10.1186/s12888-022-03784-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12888-022-03784-8