Abstract
Background
Charles Bonnet Syndrome (CBS) is a rare clinical entity that is classically composed of visual hallucinations in the context of an altered optic pathway with preservation of reality judgment. This case aims to present the association of visual hallucinations with complex alterations of the nervous structures adjacent to the visual pathway and an atypical clinical presentation, thus explaining the possible mechanisms involved in the generation of these symptoms.
Case presentation
A 43-year-old man presents seeking care due to visual hallucinations with partial preservation of reality judgment and symptoms compatible with a major depressive disorder, including irritability and diminished hygiene habits. He has a history of complete gradual loss of vision and hyposmia. Due to poor treatment response during hospitalization, an MRI was obtained, which showed a frontal tumor lesion with meningioma characteristics adjacent to the olfactory groove and compression of the optic chiasm. He underwent surgical resection of the lesion, which remitted the psychotic symptoms, but preserving the visual limitation and depressive symptoms.
Conclusions
The presence of visual hallucinations, without other psychotic features as delusions, is a focus of attention for basic structural pathologies in the central nervous system. Affection at any level of the visual pathway can cause CBS. When finding atypical symptoms, a more in-depth evaluation should be made to allow optimization of the diagnosis and treatment.
Similar content being viewed by others
Background
Charles Bonnet Syndrome (CBS) is an infrequent entity that is often confused or misdiagnosed with other psychiatric pathologies and is classically observed in elderly patients with chronic visual deficits [1]. It was first described in 1760 by the Swiss scientist Charles Bonnet, who published an essay on the visual hallucinations his grandfather experienced after undergoing cataract surgery. Despite this, it was not until 1936 when the neurologist George de Morsier coined the term “Charles Bonnet Syndrome” [2].
There is no consensus for its definition, however, it is agreed that it presents with visual hallucinations in patients with previous alterations of the optic pathway, characteristically preserving the awareness of the reality, either partially or totally [3, 4]. By preserving the judgment of these visual abnormalities, it is said that one is facing the phenomenon called hallucinosis [3].
There are few publications in the scientific literature that focus on CBS. As of July 2020, 449 articles in Pubmed contained the words “Charles Bonnet” in the title or abstract, only 9 articles combined the words “brain tumor and hallucinations” and no article was found regarding brain tumor and CBS. Thus, the purpose of this article is to make a detailed description of an adult man with a brain tumor and CBS. This case report follows the CARE Guidelines [5].
Case presentation
We present the case of a 43-year-old man who attended the outpatient service of a Psychiatric Hospital in Mexico, with a nine-month evolution of complex visual and auditory hallucinosis. He presents with bilateral amaurosis, which began insidiously 4 years prior, with no associated triggers and no previous studies to identify the cause. Psychiatric family history was denied.
He began his current condition with persistent visual and auditory hallucinosis, with a predominance of the former. He referred seeing his previous partner, from whom he had separated two and a half years prior and whom he had no contact, adding that she visited him at his house, would sit on his bed and talk to him. These episodes lasted several minutes and occurred continuously throughout the day, occurring more frequently in low-light environments. It is worth mentioning that he was fully aware that this phenomenon was not real and he referred to it as part of a disease, however, it caused him discomfort and sometimes agitation.
After the complete vision loss he initiated with depressive symptoms which consisted of sadness, anhedonia, fatigue, weight loss and low self-esteem, later adding recurrent thoughts of death. Family members mentioned that he began with personality changes such as constant irritability, impulsivity and behavioral changes regarding personal hygiene and dressing, lasting weeks without taking a bath, a situation that had never happened before. For this reason, he was taken to a psychiatric evaluation and was hospitalized for diagnosis and treatment, initially admitted with an unspecified non-organic psychotic disorder.
During the initial assessment, an ophthalmological and neurological alteration was found, being unable to perceive light in both eyes, with preserved eye movements, both slightly mydriatic pupils and bilateral hyposmia. The photomotor and the consensual light reflex were conserved, and the accommodation reflex was abolished. The rest of the physical exam was normal. He denied the presence of any specific visual complaint except for the vision loss. He also denied any physical symptoms like headaches, nausea or dizziness. Unfortunately, before his admission, he had not visited an ophthalmologist or neurologist for a check-up regarding the visual loss.
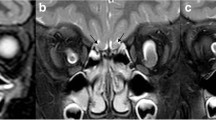
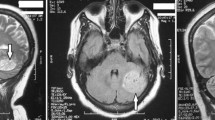
During his stay, the patient continued to present complex visual and auditory hallucinosis, referring that his ex-partner spoke to him and constantly warned him about his health, visiting him frequently in the hospitalization area: “Today I saw her. I was taking a bath and when I closed my eyes she told me to get ready, that something big was going to happen to me. I asked her what and she did not answer… I know that what I see is not real, it is a product of my mind, I know that I am not crazy … “ (sic patient). These symptoms did not ameliorate with the pharmacological treatment, which consisted of 3 mg of risperidone, 50 mg of sertraline and 0.25 mg of alprazolam every 24 h during 4 weeks. No neuropsychological tests were performed during his stay. Laboratory studies did not report abnormalities. The MRI revealed an occupational mass located at the anterior floor level of the skull adjacent to the olfactory groove in contact with the base of the sphenoid, with a mass effect on adjacent structures and significant compression of the optic chiasm, with characteristics suggestive of a benign meningioma (Fig. 1). He was referred to the neurosurgery department where a partial tumor resection was carried out by craniotomy with the confirmation of the pathology report of a benign meningioma (WHO Grade I) (Fig. 2). After the intervention, he achieved remission of the perception disturbances; however the visual impairment continued, which worsened the depressive symptoms. In addition to an exacerbation on impulsivity and low frustration tolerance, he carried out multiple suicide attempts, thus requiring six subsequent psychiatric hospitalizations. Information regarding his last follow- up reported him as stable, though apathetic and without senso-perceptive alterations. Neurologically he was reported with psychomotor retardation and frontal release signs. He remained unemployed and under his sister’s care.
Discussion
Charles Bonnet Syndrome is characterized by visual hallucinations and is usually associated with visual pathway lesions. There is no known exact prevalence, this is mainly due to the multiple disagreements to define the criteria of the syndrome, however, prevalence’s that vary from 0.8% to 10 to 15% have been reported in patients with some alteration of the visual pathway. It is estimated that up to 0.6% of older adults present this condition [6, 7]. Hallucinations come on suddenly and can be simple or complex. The simple ones are usually composed of flashes of light, figures with simple contours and squared or branched patterns; while complex ones are vivid, elaborate and repetitive; the most frequent correspond to people, faces, animals, plants and objects [1, 3]. Although characteristically the alterations are usually visual, a variant is also known in which auditory alterations occur concomitantly [4, 8].
The most accepted theory regarding the hallucinatory phenomenon is known as the Sensory Deprivation Theory and explains how the lack of visual stimuli as a consequence of an injury or deficit causes an activation of the visual cortex by a change in its excitability, thus creating the characteristic hallucinations [1, 3, 6, 9, 10].
Charles Bonnet Syndrome can occur with any condition that causes affection at some point of the visual pathway, being intracranial tumors an important but scarcely reported neurological cause [11]. Because of the slow growth, brain tumors can remain neurologically silent and only present with psychiatric symptoms, with a prevalence ranging from 50 to 90% [12, 13]. They can cause a wide variety of neuropsychiatric symptoms, specifically when they develop in the frontal lobe [11]. It has been reported that 1/1000 of hospitalized psychiatric patients have brain tumors [14].
Within intracranial tumors, meningiomas have been frequently associated with psychiatric manifestations when they are located, in particular, on the right side of the frontal lobe, classically observing changes in personality, mood disorders and visual hallucinations, being the less common the auditory hallucinations [11]. It has been found that benign meningiomas exhibit psychiatric symptoms in approximately 21% of the patients, with no neurological or physical signs [14].
Meningiomas are the most common primary intracranial tumors, 80% of which are benign, with 1–5% localized in the medial anterior skull base. The predominant histology of those tumors is meningothelial and are linked to mutations in SMO gene, locus 7p32.1 [15]. Due to the location of the tumor, this type of benign meningioma is suspected, however, genetic tests were not performed.
Alterations at the frontal level causes dysfunction on reality judgment and an inadequate modulation of the fronto-limbic system that limits the adaptation to reality, metacognition processes and impulse control [16]. Once the etiology is known, it is necessary to assess whether the clinical features have at least one of the five characteristics that define atypical CBS: impaired introspection, various types of hallucinations, atypical psychological reaction to the situation, cognitive impairment and concomitant psychiatric disorder. In the case presented, the patient presented complex auditory and visual hallucinosis and a severe major depressive disorder, the most common comorbidity. Psychotic symptoms remitted after surgery, which rules out that there was a consequence of the depressive disorder, however, the latter condition persisted and subsequently worsened. The presence and localization of the meningioma explains the modification of the personality and behavioral changes.
Conclusions
Charles Bonnet Syndrome should be suspected in the presence of visual perceptual alterations in patients with any previous condition that causes affection at some point of the visual pathway and who have an adequate awareness of the reality of the situation. In these cases, a joint initial psychiatric and neurological evaluation should be considered, because one of the causes, important and scarcely reported, are intracranial tumors. The atypical features are related with a worse prognosis due the difficulty of the diagnosis and the presence of poor insight and comorbidities. Close monitoring is important in similar cases since concomitant psychiatric disorders are frequent and there is a high risk of complications due to lack of timely and adequate diagnosis and treatment. Middle aged patients with new-onset psychiatric symptoms, sudden changes in personality, behavior or cognitive abilities need to be carefully studied; it is essential to search for focal or generalized neurologic symptoms, perform brain imaging and make a thorough neurological assessment [12,13,14].
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Abbreviations
- CBS:
-
Charles Bonnet syndrome
- mg:
-
Milligrams
- MRI:
-
Magnetic resonance imagining
References
Forgnone, I. & Siguero-Angui, A. (2016). Alucinaciones visuales sin deterioro cognitivo. Síndrome de Charles Bonnet. Un síndrome poco conocido. Semergen: revista española de medicina de familia, (3), 17–18.
López-Mompó C, López-Pavón I, Ruiz-Izquierdo J, Ferro JI. Alucinaciones visuales en ancianos sin deterioro cognitivo: síndrome de Charles Bonnet. Semergen Rev Esp Med Fam. 2011;37(5):263–6. https://doi.org/10.1016/j.semerg.2010.11.011.
Gupta R, Singhal A, Goel D, Srivastava R, Mittal S. Charles bonnet syndrome: two case reports. J Neuropsychiatry Clin Neurosci. 2008;20(3):377–8. https://doi.org/10.1176/jnp.2008.20.3.377.
Pang L. Hallucinationsexperiencedbyvisuallyimpaired: Charles bonnet syndrome. Optometry and VisionScience. 2016;93(12):1466–78. https://doi.org/10.1097/OPX.0000000000000959.
Riley DS, Barber MS, Kienle GS, Aronson JK, von Schoen-Angerer T, Tugwell P, et al. CARE 2013 explanation and elaborations: reporting guidelines for case reports. J Clin Epi. 2017;89:218–35. https://doi.org/10.1016/jclinepi.2017.04.026.
Russell G, Burns A. Charles bonnet syndrome and cognitive impairment: a systematic review. Int Psychogeriatr. 2014;26(9):1431–43. https://doi.org/10.1017/S1041610214000763.
Yoldi-Negrete M, Ramírez-Bermúdez J, Pérez-Esparza R. Síndrome de Charles Bonnet: aspectos neuropsiquiátricos. Arch Neurociencias. 2011;16(2):70–2.
Schadlu AP, Schadlu R, Shepherd JB. Charles bonnet syndrome: a review. Currentopinion Ophthalmol. 2009;20(3):219–22.
Cifuentes-Canorea P, Camacho-Bosca I, Perucho-González L, Santos-Bueso E. Síndrome de Charles Bonnet en paciente joven con antecedentes de epilepsia. Neurología. 2019;34(7):488–90. https://doi.org/10.1016/j.nrl.2016.11.001.
Coetzer R. Auditory hallucinations secondary to a right frontal meningioma. J Neuropsychiatry Clin Neurosci. 2014;26(3):E15. https://doi.org/10.1176/appi.neuropsych.13060142.
Chen JJ. Diagnosis and treatment of psychiatric comorbidity in a patient with Charles bonnet syndrome. Case Rep Psychiatry. 2014;2014:1–8.
Ghandour, F., Squassina, A., Karaky, R., Diab-assaf, M., Fadda, P., & Pisanu, C. (2021). Brain sciences presenting psychiatric and neurological symptoms and signs of brain tumors before diagnosis : a systematic review.
Pranckeviciene A, Bunevicius A, Deltuva VP, Tamasauskas A. Olfactory fossa meningioma presenting as depressive disorder: a case report. Cogn Behav Neurol. 2016;29(2):107–12.
Bunevicius, A., Deltuva, V. P., Deltuviene, D., Tamasauskas, A., & Bunevicius, R. (2008). Brain lesions manifesting as psychiatric disorders: eight cases. CNS Spectrums, 13(11), 950–958. https://doi.org/https://doi.org/10.1017/S1092852900014000.
Birzu C, Peyre M, Sahm F. Molecular alterations in meningioma: prognostic and therapeuticperspectives. Curr Opin Oncol. 2020;32(6):613–22.
Kosman KA, Silbersweig DA. Pseudo-Charles bonnet syndrome with a frontal tumor: visual hallucinations, the brain, and the two-hit hypothesis. J Neuropsychiatry Clin Neurosci. 2018;30(1):84–6. https://doi.org/10.1176/appi.neuropsych.17040076.
Acknowledgements
The authors want to thank the Centro de Atención Integral enSalud Mental Estancia Prolongada for the opportunity to attend and study their patients, to the centro universitario de ciencias de la salud, universidad de Guadalajara and the Instituto Jalisciense de Salud Mental for their support on continuous education.
Funding
No funding was obtained for this case report.
Author information
Authors and Affiliations
Contributions
JC was the treating physician of the patient during his stay in hospitalization and guide in the writing of the report. DL performed the data collection and participated in writing the manuscript. GP, AL and SDA, participated in writing, translating and editing the manuscript. All authors read and approved the final version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written informed consent was obtained from the brother of the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the authors.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Diana, LL., Carmona-Huerta, J., Patiño, J.G. et al. Atypical Charles Bonnet syndrome secondary to frontal meningioma: a case report. BMC Psychiatry 21, 365 (2021). https://doi.org/10.1186/s12888-021-03360-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12888-021-03360-6