Abstract
Background
Generalized anxiety disorder (GAD) is one of the most reported diagnoses in psychiatry, but there is some discrepancy between the cases identified in community studies and those identified in tertiary care. This study set out to evaluate whether the use of clinicians as interviewers may provide estimates in a community survey close to those observed in primary or specialized care.
Methods
This is a community survey on a randomly selected sample of 2338 adult subjects. The Advanced Neuropsychiatric Tools and Assessment Schedule (ANTAS) was administered by clinicians, providing lifetime diagnosis based on the DSM-IV-TR. Health-related quality of life (HR-QoL) was measured with the Short-Form Health Survey (SF-12).
Results
Overall, 55 (2.3%) subjects met the criteria for GAD, with greater prevalence in women (3.6%) than in men (0.9%): OR = 4.02; 95%CI: 1.96–8.26. Up to 40% of those with GAD had at least another diagnosis of mood, anxiety, or eating disorders. The mean score of SF-12 in people with GAD was 32.33 ± 6.8, with a higher attributable burden than in other conditions except for major depressive disorder.
Conclusions
We found a relatively lower lifetime prevalence of GAD than in community surveys based on lay interviewers and a structured interview. The identified cases of GAD showed a strong impact on the quality of life regardless of co-morbidity and high risk in women, suggesting a profile similar to the one identified from studies in primary and specialized care.
Similar content being viewed by others
Background
Generalized anxiety disorder (GAD) is one of the most reported mental disorders in primary care and emergency services [1]. Prevalence estimates varied widely across countries, with higher lifetime prevalence in high-income countries than in middle−/low-income countries (5% versus 1.5 to 3%) [2]. The fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), describes the GAD as characterized by persistent, excessive, and unrealistic worry about everyday things, usually involving more than an area, such as finance, family, health, and the future [3]. Anxiety in GAD is difficult to control and is accompanied by many non-specific psychological and physical symptoms, like, among others, muscle tension, fatigue, sleep disturbances, difficulty in concentrating, and irritability (DSM-5 code: 300.02) [3]. This profile of symptoms corresponds to the profile described in the fourth edition of the DSM (DSM-IV) [4] and its text revision (DSM-IV-TR) [5], thus favoring the comparison of studies across time.
GAD manifests high comorbidity with mood and other anxiety disorders, up to 50% and over, depending on the disorder and sample [2, 6]. GAD is often comorbid with bipolar disorder (BD), and might be associated with a more severe BD course and increased risk of suicide [7]. Role impairment is common in people with GAD and may be severe [2], as well as the association with chronic non-psychiatric diseases [6].
The etiology of GAD is unknown. A combination of genetics, environmental factors such as adverse childhood experiences, somatic disorders (including diabetes), alcohol and substance use, and the impact of stressful life events is thought to contribute to the onset, the course, and the persistence of GAD across lifetime. Some, low quality, brain imaging studies support a role in the expression of GAD symptoms of areas related to decision making, memory, cognitive flexibility, emotion appraisal and regulation, and detection of threat [8, 9]. GAD imports a high cost-of-illness, in terms of health expenditure and lost productivity, which has been estimated to be increased by a factor of 2.60 (95%CI: 2.01–3.36) [10]. Only about half of those with GAD seek treatment [2]. Patients with GAD may benefit from pharmacotherapy [11, 12]. In clinical practice, a combination of benzodiazepines and antidepressants is often prescribed [11, 12]. However, current guidelines emphasize that benzodiazepines should be avoided for long-term management of GAD and should be restricted to short-term use for the risk of tolerance and dependence [13, 14]. Pregabalin and quetiapine can be prescribed for long-term treatment of GAD [15]. Besides pharmacotherapy, cognitive behavioral therapy has been proved to be effective for GAD [16], while physical activity [17] and the application of transcranial magnetic stimulation [18] or transcranial direct current stimulation [19] may help for decreasing symptoms in GAD.
Despite GAD being one of the most reported diagnoses in psychiatry, and the validity of the phenotype received some support [20], the autonomy of the diagnosis was questioned by the findings of some epidemiological surveys [21]. For example, some of the symptoms required for major depressive disorder (e.g.., sleep difficulties, fatigue, and decreased concentration) overlap with GAD ones (being easily fatigued, difficulty concentrating, sleep disturbance). Indeed, the symptoms of GAD overlap in a large proportion with those of many other psychiatric conditions and a very small percentage of people diagnosed with GAD do not show another mental health diagnosis (about 17%) [21]. This is against the expectation of zones of rarity between syndromes [22]. Autonomous entities should show identifiable discontinuities with related conditions, with mixed conditions expected to be rarer than the pure forms [23]. Eventually, the actual diagnostic algorithm of the GAD goes into a detailed list of exclusion criteria, from obvious ones (the exclusion of the physiological effects of a prescribed or abuse substance or of a medical condition) to a cumbersome list of other mental disorders that should be assessed and whose impact on the anxiety, worry, or physical symptoms should be excluded (e.g., among others, anxiety or worry about having panic attacks in panic disorder, negative evaluation in social anxiety disorder, reminders of traumatic events in posttraumatic stress disorder, physical complaints in somatic symptom disorder, having a serious illness in illness anxiety disorder). Such a kind of detailed evaluation can be done in epidemiological survey but it is less easily conducted in the clinical setting. Moreover, studies on clinical samples provide data somewhat inconsistent with epidemiological studies, e.g. in a special anxiety unit in Göttingen, Germany, the proportion of patients seeking help had about 50% a diagnosis of panic disorder (frequency in epidemiological surveys around 2–3%) and only 7.5% a diagnosis of GAD (around 4% in epidemiological surveys) [24, 25].
These inconsistencies might depend on the fact that the cases identified in community studies are not the same as those identified in tertiary care. Indeed, in a diagnosis in which a central symptom such as worries has a fundamental clinical relevance, the use of “lay” interviewers and structured interviews can flatten the clinical relevance of the symptom’s centrality in epidemiological surveys [26]. Conversely, in the clinical setting greater attention is paid to patients’ reporting of theirs worries. A competing explanation could be that clinicians that work in specialized and tertiary care centers may overlook milder, but still burdensome symptoms: they may actually underdiagnose more soft cases because their clinical judgment is biased towards more severe and complex mental problems. Several studies conducted in the primary medicine setting described cases of GAD, rare in general but more frequent in the elderly (unlike some epidemiological studies that found greater frequency among young people), and with a severe impairment of health-related quality of life (HR-QoL) regardless of comorbidity with other anxiety and depressive disorders [27, 28].
The purpose of this work is to estimate the prevalence of GAD in a nationwide Italian sample. The impact of GAD and its comorbidity in terms of HR-QoL will be quantified, too. In this study, clinicians such as interviewers and semi-structured interviews (instead of lay interviewers and structured interviews like most epidemiological studies) will be used, and this might lead to the identification of a GAD profile different from that of other epidemiological studies previously conducted [29,30,31,32,33,34,35,36].
Methods
This is an observational cross-sectional study (community survey).
Design and procedure
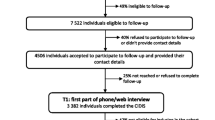
The study sample was selected by randomization after stratification in 8 cells (gender and age 18–24; 25–44; 45–64; > 64) from records of municipalities of six Italian regions (one urban, one suburban, and at least one rural municipalities each region). The selected regions were representative of geographic and socio-economic characteristics of the whole 20 Italian regions.
Trained physicians or clinical psychologists conducted the interview face to face at homes of the enrolled people. This study is a secondary research of a project whose main objective was to study the appropriateness of psychiatric diagnosis and use of prescribed drugs in the Italian population. Details on the sampling procedure and the characteristics of the sample can be found in the parent article [37].
Study tools
The psychiatric interviews were conducted by means of a semi-structured tool, the Advanced Tools and Neuropsychiatric Assessment Schedule (ANTAS) [37]. The ANTAS is a computerized tool inspired to the Structured Clinical Interview for DSM-IV (SCID) [38]. The ANTAS produces mood, anxiety and eating disorders diagnosis according to the DSM-IV-TR [5] with high cross-validity and reliability with SCID [37]. All diagnoses of psychiatric disorders were estimated as lifetime prevalence according to DSM-IV-TR criteria.
The Mood Disorder Questionnaire (MDQ) [39, 40] was adopted to assess lifetime subthreshold hypomanic episodes. Despite low accuracy in screening DSM-defined cases of bipolar disorder [41], the tool is good at identifying subthreshold cases [42].
The 12 items Survey Short Form (SF–12) [43] was used to measure the HR-QoL. The HR-QoL is a construct encompassing the self-perception of physical and psychological health. It is currently utilized as whole outcome and of impairment indicator in chronic diseases [44].
Statistical analysis
The odds ratio (OR) in univariate analysis for DSM-IV TR GAD diagnosis and age, gender and comorbidity with DSM-IV-TR diagnosed disorders, was calculated using a single group as pivot by each table. The statistical significance of the associations was measured with the χ2, with or without Yates correction. The SF-12 mean scores between groups were compared with Analysis of Variance (ANOVA) one-way statistic.
The attributable burden on impairing HR-QoL of GAD was measured as difference between mean score on the SF-12 in a sample drawn from the same community survey database of people without GAD and the mean score of SF-12 of people with GAD. For this measure, the “healthy” control sample was obtained matching and randomization by blocks. For each person with GAD, a cell was created including all the people without GAD in the database of the same age and gender, thus four people for each cell were selected. The burden in impairing of HR-QoL attributable to GAD was also compared to a similar measure obtained to other diseases in previous case-control studies, which were carried out with the same methodology [45,46,47,48,49,50,51].
Ethics
The study was approved by the by the ethical committee of the Italian National Health Institute (Rome) and conducted according to the Declaration of Helsinki and its revisions [52]. All participants signed a written informed consent. They all received an appropriate referral to primary (general practitioner) or tertiary care (local psychiatric services) in case they manifest symptoms related to the disorders under investigation.
Results
Table 1 shows lifetime prevalence of GAD by sex and age, the overall lifetime prevalence in the sample was 2.3%, with a markedly higher frequency in women (3.6%) than in men (0.9%; OR = 4.02; 95%CI: 1.96–8.26) and a substantially stable frequency in age in both sexes.
The lifetime prevalence found by our research (2.3%) is lower than the one found in all other studies that were conducted through structured interviews administered by lay interviewers (Table 2).
With just the exception of the study of Chang in Singapore (1.6%), and the European Study of the Epidemiology of Mental Disorders (ESEMeD) [32], with estimates of 2.8%, the other studies ranged from 3.6% in Korea [34] to 10.5% in a small town in Taiwan [29].
As far as comorbidity was concerned, people with at least another diagnosis of mood, anxiety or eating disorders were 22 out 55 (40%). The most frequent diagnoses in comorbidity were: major depressive disorders (20%, OR = 5.97; 2.99–11.95), panic disorder (16.4%; OR = 17.4; 7.56–38.40), and simple phobia (16.3%; OR = 9.93; 4.58–21.55) (Table 3).
The level of HR-QoL in people with GAD (measured as mean score of SF-12) was 32.33 ± 6.8, without differences in people with (N = 22; 30.4 ± 7.0) or without comorbidities (N = 33; 33.6 ± 6.7): F (1;53) = 2.90; p = 0.094. Overall, with the only exception of major depressive disorder, GAD showed an attributable burden higher to that observed for the other investigated disorders from the same database (Table 4).
However, if we consider the cases of GAD without comorbidity, the “attributable burden” in impairing HR-QoL becomes comparable between GAD to that of most of the other disorders considered, except for panic disorder and simple phobia that resulted less impairing.
Discussion
This survey, conducted by clinical interviewers who employed a semi-structured interview, showed a lower frequency of GAD in a sample of Italian general population compared to all community surveys conducted recently with the use of lay interviewing and clinical interviews structured [29,30,31,32,33,34,35], with the only exception of the study of Chang in Singapore [36] and the ESEMeD study [32]. The Chang ‘study also showed an increase from 0.9 to 1.6% compared to a study conducted in Singapore a few years earlier [36].
It is worth noting that our study highlights lower rates than research conducted on samples that are culturally closer, such as those examined by Faravelli’s study in a center of Tuscany in Italy [33]. Compared to this study, people with GAD in our sample have a lower frequency of comorbidity with other mood, anxiety or eating disorders (40% vs 70% of the study by Faravelli et al. [33]), and are more frequently women (4/1 ratio instead of 2/1). Another peculiar characteristic of our sample is that the frequency is stable over time and there is no higher frequency in the youth population as otherwise highlighted in the other community surveys conducted with structured interviews [25].
The stability of rates in different age groups, resulting in a higher rate in the elderly population (comparing with other community surveys) and the increased frequency in women makes our sample closer to the profile of GAD described in the specialist medical setting and/or primary care [27, 28]. It must be noted that a disorder like GAD, which should have a long course, should accumulate its frequency over time and, therefore, it would be logical to expect the lifetime rates in the elderly to be high. But this certainly applies to a disabling and high-impact disorder, less to a mild disorder that tends to be forgotten more frequently, generating higher recalling bias rates [53]. Nevertheless, several investigations noted a high prevalence of GAD in elderly people, with estimates around 10% or above [54,55,56]. A fraction of these cases were late-onset cases of GAD triggered by recent adverse life events and by chronic physical or mental (depression) health disorders. Adversities during childhood and a history of mental problems in parents were also related to recent onset GAD [55].
The GAD profile highlighted in our sample confirms that it has a severe impact on the lives of individuals, even independently of co-morbidity with other disorders, which, consistent with the cases highlighted in the primary medicine setting, defines a very well-defined pathology. Our study, therefore, seems to confirm that there may be a more clinically relevant (and less extensive) nucleus of people suffering from GAD and that the research conducted with hyper-structured methodology and using lay interviewers may produce an improper enlargement of the number of disorders that it may include people who are not properly suffering from a clinically important condition. This can be confirmed not only by the mismatch between the profile in community surveys and in health care agencies (which can be determined by barriers to access care for milder cases, although this is unlikely about primary care) but above all from the paradox of a progressive decrease over time of the lifetime frequency by age group.
The use of trained clinician interviewers is the strength of this study, together with the application of a standardized tool in community-based samples that were representative of the socio-cultural characteristics of the entire national territory. Nevertheless, some limitations must be acknowledged. The target of the original study was the lifetime prevalence of people diagnosed within the bipolar spectrum, which was estimated to involve 4% of participants. However, GAD and other anxiety disorders have lower lifetime prevalence, thus we were somehow underpowered to estimates some comorbid associations. We also lack information on somatic comorbidities, which may be relevant in GAD and reinforce the symptoms of anxiety in the disorder [6, 57].
Conclusions
Our community survey conducted with a methodology that used clinical interviewers and a semi-structured interview showed a relatively low GAD frequency in the community than in other community surveys based on lay interviewers and a structured interview. The characteristics of the GADs of our sample (as a strong impact on the quality of life regardless of co-morbidity and high risk in women) indicate a disorder with characteristics very similar to those identified from studies in primary care and specialized care agencies.
It should be noted that there is no undisputable gold standard about GAD and, given the essential differences between the focus and scope of the clinician-based and lay-administered assessment methods, it cannot be decided whether the prevalence estimates of this study are more precise than those that can be derived from epidemiological studies based on lay-administered assessment methods. Only a direct comparison of the methods may consent an answer to that.
Availability of data and materials
The dataset for this article is not publicly available because the agreement shared with the partners in the planning of the study, in the presentation for the assignment of the original grant and the request for authorization to the ethics committee was that the database (with anonymized records) would be available only under the review of the project leader as guarantor. Requests to access the dataset should be directed to Professor Mauro Giovanni Carta.
Abbreviations
- ANOVA:
-
Analysis Of Variance
- ANTAS:
-
Advanced Tools and Neuropsychiatric Assessment Schedule
- BD:
-
Bipolar disorder
- CI:
-
Confidence interval
- DSM-5:
-
Diagnostic and Statistical Manual of Mental Disorders, fifth edition
- DSM-IV-TR:
-
Diagnostic and Statistical Manual of Mental Disorders, fourth edition, text revision
- ESEMeD:
-
European Study of the Epidemiology of Mental Disorders
- GAD:
-
Generalized anxiety disorder
- HR-QoL:
-
Health related quality of life
- MDQ:
-
Mood Disorder Questionnaire
- NICE:
-
National Institute for Health and Care Excellence
- OR:
-
Odds ratio
- SCID:
-
Structured Clinical Interview for DSM-IV
- SF–12:
-
12 items Survey Short Form
References
Wittchen HU. Generalized anxiety disorder: prevalence, burden, and cost to society. Depress Anxiety. 2002;16(4):162–71. https://doi.org/10.1002/da.10065.
Ruscio AM, Hallion LS, Lim CCW, et al. Cross-sectional comparison of the epidemiology of DSM-5 generalized anxiety disorder across the globe. JAMA Psychiatry. 2017;74(5):465–75. https://doi.org/10.1001/jamapsychiatry.2017.0056.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders (5th ed). Washington, DC: American Psychiatric Press; 2013.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-IV. Washington, DC: American Psychiatric Association; 1994.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders (4th ed., text revision). Washington, DC: American Psychiatric Press; 2000.
Balestrieri M, Isola M, Quartaroli M, Roncolato M, Bellantuono C. Assessing mixed anxiety-depressive disorder. A national primary care survey. Psychiatry Res. 2010;176(2–3):197–201. https://doi.org/10.1016/j.psychres.2008.11.011.
Preti A, Vrublevska J, Veroniki AA, Huedo-Medina TB, Fountoulakis KN. Prevalence, impact and treatment of generalised anxiety disorder in bipolar disorder: a systematic review and meta-analysis. Evid Based Ment Health. 2016;19(3):73–81. https://doi.org/10.1136/eb-2016-102412.
Madonna D, Delvecchio G, Soares JC, Brambilla P. Structural and functional neuroimaging studies in generalized anxiety disorder: a systematic review. Braz J Psychiatry. 2019;41(4):336–62. https://doi.org/10.1590/1516-4446-2018-0108.
Kolesar TA, Bilevicius E, Wilson AD, Kornelsen J. Systematic review and meta-analyses of neural structural and functional differences in generalized anxiety disorder and healthy controls using magnetic resonance imaging. Neuroimage Clin. 2019;24:102016. https://doi.org/10.1016/j.nicl.2019.102016.
Konnopka A, König H. Economic burden of anxiety disorders: a systematic review and meta-analysis. Pharmacoeconomics. 2020;38(1):25–37. https://doi.org/10.1007/s40273-019-00849-7.
Gomez AF, Barthel AL, Hofmann SG. Comparing the efficacy of benzodiazepines and serotonergic anti-depressants for adults with generalized anxiety disorder: a meta-analytic review. Expert Opin Pharmacother. 2018;19(8):883–94. https://doi.org/10.1080/14656566.2018.1472767.
Driot D, Bismuth M, Maurel A, et al. Management of first depression or generalized anxiety disorder episode in adults in primary care: a systematic metareview. Presse Med. 2017;46(12 Pt 1):1124–38. https://doi.org/10.1016/j.lpm.2017.10.010.
National Collaborating Centre for Mental Health (UK). Generalised anxiety disorder in adults: Management in Primary, secondary and community care. Leicester: British Psychological Society; 2011.
Andrews G, Bell C, Boyce P, et al. Royal Australian and new Zealand College of Psychiatrists clinical practice guidelines for the treatment of panic disorder, social anxiety disorder and generalised anxiety disorder. Aust N Z J Psychiatry. 2018;52(12):1109–72. https://doi.org/10.1177/0004867418799453.
Perna G, Alciati A, Riva A, Micieli W, Caldirola D. Long-term pharmacological treatments of anxiety disorders: an updated systematic review. Curr Psychiatry Rep. 2016;18(3):23. https://doi.org/10.1007/s11920-016-0668-3.
van Dis EAM, van Veen SC, Hagenaars MA, et al. Long-term outcomes of cognitive behavioral therapy for anxiety-related disorders: a systematic review and meta-analysis. JAMA Psychiatry. 2019;77(3):265–73. https://doi.org/10.1001/jamapsychiatry.2019.3986.
McDowell CP, Dishman RK, Gordon BR, Herring MP. Physical activity and anxiety: a systematic review and meta-analysis of prospective cohort studies. Am J Prev Med. 2019;57(4):545–56. https://doi.org/10.1016/j.amepre.2019.05.012.
Cirillo P, Gold AK, Nardi AE, et al. Transcranial magnetic stimulation in anxiety and trauma-related disorders: a systematic review and meta-analysis. Brain Behav. 2019;9(6):e01284. https://doi.org/10.1002/brb3.1284.
Sagliano L, Atripaldi D, De Vita D, D'Olimpio F, Trojano L. Non-invasive brain stimulation in generalized anxiety disorder: a systematic review. Prog Neuro-Psychopharmacol Biol Psychiatry. 2019;93:31–8. https://doi.org/10.1016/j.pnpbp.2019.03.002.
Rutter LA, Brown TA. Reliability and validity of the dimensional features of generalized anxiety disorder. J Anxiety Disord. 2015;29:1–6. https://doi.org/10.1016/j.janxdis.2014.10.003.
Faravelli C, Castellini G, Benni L, et al. Generalized anxiety disorder: is there any specific symptom? Compr Psychiatry. 2012;53(8):1056–62. https://doi.org/10.1016/j.comppsych.2012.04.002.
Kendell R, Jablensky A. Distinguishing between the validity and utility of psychiatric diagnoses. Am J Psychiatry. 2003;160(1):4–12. https://doi.org/10.1176/appi.ajp.160.1.4.
Kendell RE, Brockington IF. The identification of disease entities and the relationship between schizophrenic and affective psychoses. Br J Psychiatry. 1980;137:324–31. https://doi.org/10.1192/bjp.137.4.324.
Bandelow B. Epidemiology of depression and anxiety. In: Kasper S, den Boer JA, Sitsen AJM, editors. Handbook on depression and anxiety. New York, NY: M. Dekker; 2003. p. 49–68.
Bandelow B, Michaelis S. Epidemiology of anxiety disorders in the 21st century. Dialogues Clin Neurosci. 2015;17(3):327–35.
Balestrieri M, Baldacci S, Bellomo A, et al. Clinical vs. structured interview on anxiety and affective disorders by primary care physicians. Understanding diagnostic discordance. Epidemiol Psichiatr Soc. 2007;16(2):144–51. https://doi.org/10.1017/s1121189x00004772.
Porensky EK, Dew MA, Karp JF, et al. The burden of late-life generalized anxiety disorder: effects on disability, health-related quality of life, and healthcare utilization. Am J Geriatr Psychiatry. 2009;17(6):473–82. https://doi.org/10.1097/jgp.0b013e31819b87b2.
Stanley MA, Diefenbach GJ, Hopko DR, et al. The nature of generalized anxiety in older primary care patients: preliminary findings. J Psychopathol Behav Assess. 2003;25:273–80. https://doi.org/10.1023/A:1025903214019.
Hwu HG, Yeh EK, Chang LY. Prevalence of psychiatric disorders in Taiwan defined by the Chinese diagnostic interview schedule. Acta Psychiatr Scand. 1989;79(2):136–47. https://doi.org/10.1111/j.1600-0447.1989.tb08581.x.
Bourdon KH, Rae DS, Locke BZ, Narrow WE, Regier DA. Estimating the prevalence of mental disorders in U.S. adults from the epidemiologic catchment area survey. Public Health Rep. 1992;107(6):663–8.
Kessler RC, McGonagle KA, Zhao S, et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Results from the National Comorbidity Survey. Arch Gen Psychiatry. 1994;51(1):8–19. https://doi.org/10.1001/archpsyc.1994.03950010008002.
Alonso J, Angermeyer MC, Bernert S, et al. Prevalence of mental disorders in Europe: results from the European study of the epidemiology of mental disorders (ESEMeD) project. Acta Psychiatr Scand Suppl. 2004;420:21–7. https://doi.org/10.1111/j.1600-0047.2004.00327.x.
Faravelli C, Abrardi L, Bartolozzi D, et al. The Sesto Fiorentino study: background, methods and preliminary results. Lifetime prevalence of psychiatric disorders in an Italian community sample using clinical interviewers. Psychother Psychosom. 2004;73(4):216–25. https://doi.org/10.1159/000077740.
Cho MJ, Kim JK, Jeon HJ, et al. Lifetime and 12-month prevalence of DSM-IV psychiatric disorders among Korean adults. J Nerv Ment Dis. 2007;195(3):203–10. https://doi.org/10.1097/01.nmd.0000243826.40732.45.
Kessler RC, Petukhova M, Sampson NA, Zaslavsky AM, Wittchen H. U. Twelve-month and lifetime prevalence and lifetime morbid risk of anxiety and mood disorders in the United States. Int J Methods Psychiatr Res. 2012;21(3):169–84. https://doi.org/10.1002/mpr.1359.
Chang S, Abdin E, Shafie S, et al. Prevalence and correlates of generalized anxiety disorder in Singapore: results from the second Singapore mental health study. J Anxiety Disord. 2019;66:102106. https://doi.org/10.1016/j.janxdis.2019.102106.
Carta MG, Aguglia E, Bocchetta A, et al. The use of antidepressant drugs and the lifetime prevalence of major depressive disorders in Italy. Clin Pract Epidemiol Ment Health. 2010;6:94–100Published 2010 Aug 27. https://doi.org/10.2174/1745017901006010094.
First M, Spitzer R, Gibbon M, Williams J. Structured clinical interview for DSM-IV axis I disorders, research version, non-patient edition (SCID-I/NP). New York: Biometrics Research, New York State Psychiatric Institute; 1997.
Hirschfeld RM, Calabrese JR, Weissman MM, Reed M, Davies MA, Frye MA, et al. Screening for bipolar disorder in the community. J Clin Psychiatry. 2003;64:53–9. https://doi.org/10.4088/JCP.v64n0111.
Hardoy MC, Cadeddu M, Murru A, Dell’Osso B, Carpiniello B, Morosini PL, et al. Validation of the Italian version of the “mood disorder questionnaire” for the screening of bipolar disorders. Clin Pract Epidemiol Ment Health. 2005;1:8. https://doi.org/10.1186/1745-0179-1-8.
Zimmerman M, Galione JN, ChelminskiI I, Young D, Dalrymple K. Psychiatric diagnoses in patients who screen positive on the mood disorder questionnaire: implications for using the scale as a case-finding instrument for bipolar disorder. Psychiatry Res. 2011;185:444–9. https://doi.org/10.1016/j.psychres.2010.06.025.
Karam EG, Salamoun MM, Yeretzian JS, Mneimneh ZN, Karam AN, Fayyad J, et al. The role of anxious and hyperthymic temperaments in mental disorders: a national epidemiologic study. World Psychiatry. 2010;9:103–10. https://doi.org/10.1002/j.2051-5545.2010.tb00287.x.
Ware J Jr, Kosinski M, Keller SD. A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220–33. https://doi.org/10.1097/00005650-199603000-00003.
Mantovani G, Astara G, Lampis B, et al. Evaluation by multidimensional instruments of health-related quality of life of elderly cancer patients undergoing three different “psychosocial” treatment approaches. A randomized clinical trial. Support Care Cancer. 1996;4(2):129–40. https://doi.org/10.1007/BF01845762.
Carta MG, Tondo L, Balestrieri M, et al. Sub-threshold depression and antidepressants use in a community sample: searching anxiety and finding bipolar disorder. BMC Psychiatry. 2011;11:164Published 2011 Oct 10. https://doi.org/10.1186/1471-244X-11-164.
Carta MG, Preti A, Moro MF, et al. Eating disorders as a public health issue: prevalence and attributable impairment of quality of life in an Italian community sample. Int Rev Psychiatry. 2014;26(4):486–92. https://doi.org/10.3109/09540261.2014.927753.
Carta MG, Moro MF, Aguglia E, et al. The attributable burden of panic disorder in the impairment of quality of life in a national survey in Italy. Int J Soc Psychiatry. 2015;61(7):693–9. https://doi.org/10.1177/0020764015573848.
Sancassiani F, Romano F, Balestrieri M, et al. The prevalence of specific phobia by age in an Italian Nationwide survey: how much does it affect the quality of life? Clin Pract Epidemiol Ment Health. 2019;15:30–7Published 2019 Feb 20. https://doi.org/10.2174/1745017901915010030.
Sancassiani F, Carmassi C, Romano F, et al. Impairment of quality of life associated with lifetime diagnosis of post-traumatic stress disorder in women - a National Survey in Italy. Clin Pract Epidemiol Ment Health. 2019;15:38–43Published 2019 Feb 28. https://doi.org/10.2174/1745017901915010038.
Carta MG, Fineberg N, Moro MF, et al. The burden of comorbidity between bipolar Spectrum and obsessive-compulsive disorder in an Italian community survey. Front Psychiatry. 2020;11:188Published 2020 Mar 31. https://doi.org/10.3389/fpsyt.2020.00188.
Preti A, Piras M, Cossu G, et al. The burden of agoraphobia in worsening quality of life in a community survey in Italy. Psychiatry Investig. 2021. In press. [accepted for publication].
World Medical Association. World medical association declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191–4. https://doi.org/10.1001/jama.2013.281053.
Haagsma J, Bonsel G, de Jongh M, Polinder S. Agreement between retrospectively assessed health-related quality of life collected 1 week and 12 months post-injury: an observational follow-up study. Health Qual Life Outcomes. 2019;17(1):70Published 2019 Apr 23. https://doi.org/10.1186/s12955-019-1139-4.
Beekman AT, Bremmer MA, Deeg DJ, van Balkom AJ, Smit JH, de Beurs E, et al. Anxiety disorders in later life: a report from the longitudinal aging study Amsterdam. Int J Geriatr Psychiatry. 1998;13(10):717–26. https://doi.org/10.1002/(sici)1099-1166(1998100)13:10<717::aid-gps857>3.0.co;2-m.
Zhang X, Norton J, Carrière I, Ritchie K, Chaudieu I, Ancelin ML. Risk factors for late-onset generalized anxiety disorder: results from a 12-year prospective cohort (the ESPRIT study). Transl Psychiatry. 2015;5(3):e536. https://doi.org/10.1038/tp.2015.31.
Zhang X, Norton J, Carrière I, Ritchie K, Chaudieu I, Ancelin ML. Generalized anxiety in community-dwelling elderly: prevalence and clinical characteristics. J Affect Disord. 2015;172:24–9. https://doi.org/10.1016/j.jad.2014.09.036.
Kohlmann S, Gierk B, Hilbert A, Brähler E, Löwe B. The overlap of somatic, anxious and depressive syndromes: a population-based analysis. J Psychosom Res. 2016;90:51–6. https://doi.org/10.1016/j.jpsychores.2016.09.004.
Acknowledgements
None.
Funding
This study was supported by a grant of AIFA (Agenzia Italiana del Farmaco) Number FARM54S73S, approved in 2005. The funding body did not have had any further role in study design; in the collection, analysis, and interpretation of data; in the writing of the report; and in the decision to submit the paper for publication.
Author information
Authors and Affiliations
Contributions
MGC, FR, MB, FC, LD, GD, FD, MCH, RR, CF, MA: Conceptualization, Methodology, Software; MGC, AP, FR, MB, FC, LD, GD, FD, MCH, RR, CF, MA, CIAG: Data curation, Writing, Original draft preparation; MGC, FR, MB, FC, LD, GD, FD, MCH, RR, CF, MFM: Visualization, Investigation; MGC, AP: Formal analysis; MGC, MA, FR, MB, FC, LD, GD, FD, MCH, RR, CF, CIAG: Supervision; AP, MGC, RD, GC, CIAG, CK, FC, MFM: Writing, Reviewing and Editing; MCG: Funding acquisition; MCG: Project administration. All authors read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the by the ethical committee of the Italian National Health Institute (Rome) and conducted according to the Declaration of Helsinki and its revisions (WMA, 2013). All participants signed a written informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Preti, A., Demontis, R., Cossu, G. et al. The lifetime prevalence and impact of generalized anxiety disorders in an epidemiologic Italian National Survey carried out by clinicians by means of semi-structured interviews. BMC Psychiatry 21, 48 (2021). https://doi.org/10.1186/s12888-021-03042-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12888-021-03042-3