Abstract
Background
Self-harm, whether attributed to suicidal or non-suicidal motives, is associated with several poor outcomes in young people, including eventual suicide. Much of our understanding of self-harm in young people is based on literature from Europe (particularly, the UK), North America, and Australia. We aimed to synthesise the available evidence on prevalence, the commonly reported self-harm methods, correlates, risk and protective factors, and reasons for self-harm, in adolescents (aged 10–25 years) in sub-Saharan Africa.
Method
We searched MEDLINE, PsycINFO, PubMed, African Journals OnLine, and African Index Medicus for records from 1950 through August 2019, without language restrictions. We supplemented the database searches by searching relevant portals for postgraduate theses, reference harvesting, contacting authors for unpublished studies, and hand searching relevant print sources. We applied narrative synthesis to the evidence.
Results
Seventy-four studies from 18 sub-Saharan African countries met the inclusion criteria. The median lifetime prevalence estimate was 10·3% (interquartile range [IQR] 4·6% – 16·1%); median 12-month prevalence estimate was 16·9% (IQR: 11·5% – 25·5%); median 6-month prevalence estimate was 18·2% (IQR: 12·7% – 21·8%); and the median 1-month prevalence estimate was 3·2% (IQR: 2·5–14·8%). Studies from Western sub-Saharan Africa reported the highest 12-month prevalence estimates (median = 24·3%; IQR = 16·9% – 27·9%). Clinical samples commonly reported overdose, whereas self-cutting was most commonly reported in non-clinical samples. Academic failure, sexual, emotional, and physical abuse, romantic relationship problems, family conflict, depression, and previous self-harm were identified as key correlates of self-harm. No study reported protective factors against self-harm.
Conclusion
Variation in estimates was explained by small sample sizes and variation in definitions and measures used. Exploration of associations, risks and protective factors was based upon concepts and measures derived from high income countries. More detailed and culturally sensitive research is needed to understand the context-specific risks and protective factors for self-harm in adolescents in sub-Saharan Africa.
Similar content being viewed by others
Background
The World Health Organisation (WHO) defines self-harm as “an act with non-fatal outcome in which an individual deliberately initiates a non-habitual behaviour, that without intervention from others will cause self-harm, or deliberately ingests a substance in excess of the prescribed or generally recognised therapeutic dosage, and which is aimed at realising changes that the person desires via the actual or expected physical consequences” [1, 2].
This definition does not distinguish acts of self-harm according to intent, and for brevity in this review we use the term “self-harm” to refer to acts that are attributed to suicidal and non-suicidal motivations. Self-harm among young people is a recognised problem in the mental health of populations in high income countries, where it is associated with a number of poor outcomes including eventual suicide [3, 4]. By comparison we know little about self-harm in young people in sub-Saharan Africa; instead much of our understanding is based on extrapolation from literature from Europe, particularly the UK, North America, and Australia [5,6,7,8]. Earlier regional reviews have either included only a few selected studies of young people from Africa, [9,10,11] or included only studies involving adult population samples from the region [12]. Thus, we have found no existing review that has systematically appraised the available published and unpublished evidence specifically on self-harm among adolescents in countries in sub-Saharan Africa.
The aims of the present review were to:
-
1)
Describe the lifetime, 12-month, 6-month, and 1-month prevalence estimates of self-harm in young people (aged 10–25 years) across sub-Saharan Africa.
-
2)
Describe the commonest methods of self-harm in young people identified across the previous studies.
-
3)
Identify the commonest associations, risks, and protective factors associated with self-harm in young people observed in previous studies across sub-Saharan Africa.
-
4)
Describe the self-reported reasons for self-harm in young people across sub-Saharan Africa.
Methods
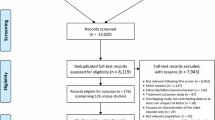
This systematic review followed PRISMA guidelines [13] (see Additional files 1 and 2). We searched MEDLINE, PsycINFO, PubMed, African Journals OnLine, African Index Medicus, and the South African national Electronic Theses and Dissertations (SA-ETD) portal, (Additional file 3) between January 1950 and August 2019, without language restrictions. The geographic search filter included names of the countries in English and languages relevant to the countries [14]. When a country’s name had changed after 1950 [15], both current and earlier names were included. We searched grey literature, institutional and organisational reports and national and international government reports (e.g., WHO, World Bank, UNICEF, UNDP) [16]. We hand searched edited books, the West African Journal of Medicine, Ghana Medical Journal, South African Medical Journal, Ethiopian Medical Journal, and the East African Medical Journal. We contacted academics with a research interest in self-harm and authors who published two or more articles on self-harm identified during our review (see Additional file 4). Reference harvesting used Science Citation Index, Google Scholar, and manual search. Criteria for inclusion and exclusion of studies are shown in Table 1.
We used EndNote (version X9.2) to collate and handle the identified records. All records were screened for eligibility by reading the titles, abstracts, methods, and results sections by EQ, with consensus discussion of 10–20% of studies with co-authors. Appraisal of the methodological quality of records used the mixed method appraisal tool (MMAT) [17]. There was substantial heterogeneity across the studies. We applied narrative synthesis to the evidence in the final set of studies; we present the prevalence estimates as median values and interquartile ranges (IQRs). We report pooled estimates (median and IQR) to aid presentation of the data, but note should be taken of the substantial heterogeneity in studies included [18, 19].
Results
Seventy-four studies involving adolescents aged 10–25 years were included after removing duplicates - one national report on adolescent health behaviour, seven (9·4%) postgraduate theses, one book chapter and 65 (87·8%) peer-reviewed articles published in indexed academic journals (see Additional file 5).
Characteristics of included studies
The majority of the studies, 54 (73%), used the terms “suicide attempt”, “suicidal attempt”, or “attempted suicide”, to describe self-harm. Although included studies distinguished between suicidal self-harm and non-suicidal self-harm in their findings none of the studies indicated if a definition or explanation of the core question was provided to participants [20]. Because we wanted to include all acts that meet the WHO definition, which does not include a requirement for a specific intent, given the contention about the soundness of the distinction between self-reported suicidal and non-suicidal acts [21], which is likely to be a particular problem in countries where suicide is illegal and where different languages may not readily reflect the distinction, and as individual suicide risk is known to reside in all acts of self-harm regardless of attribution, we have included all studies in our estimates of prevalence where it was clear that self-harm was the question put to participants, regardless of apparent intent.
Data were available from all four geographical sub-regions of sub-Saharan Africa. The majority (44·6%) were from five countries within Southern sub-Saharan Africa (eSwatini, Mozambique, Namibia, South Africa, and Zambia) - South Africa ranked the highest with more than half (n = 37) of the total included records; 30·4% were based on data from six Western sub-Saharan African countries (Benin, Ghana, Ivory Coast, Mauritania, Nigeria, and Togo); 1·1% from Congo-Brazzaville in Central sub-Saharan Africa; and 23·9% of data obtained from six countries within Eastern sub-Saharan Africa (Ethiopia, Malawi, Rwanda, Seychelles, Tanzania, and Uganda). Seventy-two of the studies were in English and two were in French.
The majority of the studies (n = 56; 75·6%) utilised a quantitative cross-sectional design involving questionnaires administered to participants accessed in communities/households, a charity facility, hospitals, schools and universities (see Additional file 6). Five studies included only female participants [22,23,24,25,26]; and one study involved only male participants [27]. The majority (n = 49; 66·2%) of the studies sampled students from schools and universities. Six studies (8·1%) sampled young people who were out of the school environment, including adolescents living in poor, rural, war-affected communities [28], adolescents in children’s homes [29], children and youth living in slums and streets [30, 31], adolescents living in poor urban and rural villages [32], and out-of-school youth who were unstably housed, living in poor urban neighbourhoods [33].
The total sample covered by the studies was 205,132. Thirty-nine (52·7%) of the studies used some form of random selection in recruiting their participants. Across the 74 studies, only 14 (18·9%) provided information on the size of their target population and how their sample sizes were determined.
Six (8·1%) of the studies were rated “average quality” on the MMAT, 21 studies (28·4%) were rated “above average quality”; 22 studies (29·7%) were rated “high quality”, while the remaining 25 studies (33·8%) were rated to be of “very high quality” (see Additional file 7).
Main findings
Fifty-five (74·3%) of the studies reported prevalence estimates, though none reported lifetime, 12-month, 6-month, and 1-month estimates, with 12-month estimates favoured by the majority (n = 30; 54·5%). As shown in Table 2, the reported lifetime prevalence estimates ranged from 1·4% to 48·3% [28, 50]; the 12-month prevalence estimates varied between 0·9% and 35·8% [52, 72]; the reported 6-month prevalence ranged from 7·4% to 22·7% [55, 79]; and the 1-month reported prevalence estimates varied between 1·9% and 26·4% [31, 58].
The majority of the 55 prevalence studies (n = 46; 83·6%) focused on suicidal self-harm, seven studies (12·7%) focused on non-suicidal self-harm [48, 50, 52, 53, 60, 70, 76], while two studies simultaneously reported the prevalence estimates of both suicidal self-harm (suicidal attempt) and non-suicidal self-harm (self-injury) [28, 72].
Visual inspection of the forest plots and the I2 value ranges (98·84% to 99·71%, p < ·001) indicate that heterogeneity across each of these summaries is substantial (see Figs. 1, 2, 3 and 4). Median values with interquartile ranges were computed for the overall and sub-regional reported prevalence estimates (see Fig. 5). Considerable variability was found across the ranges of prevalence estimates reported: the median lifetime prevalence estimate was 10·3% (interquartile range [IQR] of 4·6% – 16·1%) and the median 12-month prevalence estimate was 16·9% (IQR: 11·5% – 25·5%). Studies from Western sub-Saharan Africa reported the highest 12-month prevalence estimates (median = 24·3%; IQR = 16·9% – 27·9%), while studies from Eastern (median = 11·5%; IQR = 11·1% – 18·3%) and Southern (median = 16·5%; IQR = 10·9% – 24·0%) sub-Saharan Africa reported relatively similar median 12-month prevalence estimates.
Median and interquartile range (IQR) of prevalence estimates of adolescent self-harm in sub-Saharan Africa. Source: Map created by authors, based on the list of countries within the sub-regional division of sub-Saharan Africa by the United Nations Statistics Division’s classification (list accessed on January 20, 2019: https://unstats.un.org/unsd/methodology/m49/)
Twenty (27%) of the 74 studies reported on the methods of self-harm (Table 3). Overdose of medication was frequently reported from clinic-based studies, while self-cutting was the predominant method reported in the non-clinic based studies.
Overall, 48 (64·9%) of the 74 studies reported on the associates, risks and protective factors. The evidence was organised by reported associates into four main domains: personal, family, school, and interpersonal (non-family). The interpersonal (non-family) included circumstances related to the individuals’ relationships with peers and neighbours, and other social relationships and interactions outside the family and school contexts. Additionally, based on the strong association of abuse and violence victimisation (within and outside the family context) and self-harm [11, 92,93,94], we created a separate category, abuse and violence, to capture all factors related to psychological, physical, emotional, and sexual abuse items.
Results are shown in Table 4. Common examples of associations included, at the personal level, depression, hopelessness and psychiatric illness; at the family level, conflict with parents, parental divorce; at school level, academic failure, and for the interpersonal level, relationship breakups and problems, and lack of social support. Abuse and violence-related factors included sexual abuse, dating violence, bullying, and physical fights. Only one study reported risk factors related to self-harm [56], while no study reported protective factors against self-harm.
Because of the substantial heterogeneity in samples, definition and measurement of associations, we regard any attempt at comparison or pooling of the reported prevalences of these associations (as opposed to simply their presence or absence) as potentially misleading. We noted, however, the proportion of included studies that reported associations in each category as follows: Personal = 41 / 48; Family = 31 / 48; Interpersonal = 24 / 48; Abuse and violence = 19 / 48; School = 13 / 48.
We further categorised the self-reported reasons for self-harm into “intrapersonal” (i.e., reasons intended to change one’s state or circumstances), and “interpersonal” (i.e., reasons intended to change the state or circumstances of significant others). Eight (10·8%) studies included self-reported reasons for self-harm – see Table 5. Five of these were clinic-based, [22,23,24, 26, 88] while three were non-clinic based [27, 29, 50].
Across the eight studies reporting reasons for self-harm, participants concurrently reported both intrapersonal and interpersonal reasons for engaging in self-harm with no clear pattern discernible.
The findings of the prevalence studies regarding associates of self-harm were mixed in terms of age, although more reported higher estimates among young people between the ages of 15 and 17 years, compared to those aged 14 years and below, and 18 years or above [35, 39, 43, 73].
The majority of the prevalence studies reported higher estimates among female adolescents than in male adolescents [30, 34, 40, 45, 58, 59, 61, 62, 65, 73, 78], although seven studies (12·7%) found higher prevalence estimates in male adolescents [33, 35, 37, 52, 55, 67, 77].
Discussion
There are clearly problems with the literature we found. Despite the number of reported studies, and the extended search, we identified research from fewer than 40% (18/46) of the countries across the sub-region, and half of all studies came from one country – South Africa. This represents a serious gap in our knowledge about population mental health in those countries from which research is missing.
The reported prevalence estimates showed considerable variations within and between the countries and sub-regions of sub-Saharan Africa. Undoubtedly, real variations are likely to exist but there must also be methodological reasons to explain, for example, that estimates of lifetime prevalence appear lower than 12-month prevalence. One explanation is the origin and contextual relevance of the measures used by the studies, and the lack of consistency in definitions and choice of measures across studies. In this respect it is worth noting the widespread use of the term “attempted suicide” in studies which did not explain the term to those responding to the question. The consequence is that studies cannot be reliably categorised as reporting the prevalence of suicidal or non-suicidal behaviour. For example – as shown on Table 5 respondents in a study about “attempted suicide” might report that they intended to die as the result of an act while others might report that the act was intended to prevent suicide, or that the act was designed to change the nature of their relationships with others. We found no substantial study where participants were asked in detail about reasons for self-harm, after responding with an initial affirmative to a question about attempted suicide. Respondent bias due to the illegality, sensitivity, stigma, and taboo against suicide and other self-destructive behaviours in Africa [98] is likely to vary according to how and by whom inquiries were made.
Even so, the median 12-month prevalence estimate of 16·9% (IQR: 11·5% – 25·5%), and median 6-month prevalence estimate of 18·2% (IQR: 12·7% – 21·8%) particularly had reasonably narrow confidence intervals. What is striking is that these figures are of the same order as those reported from Europe and North America, as is the finding that young women report more self-harm than young men. Similarly, methods of self-harm were similar with overdose of medication frequently reported in clinic-based studies, while self-cutting was the predominant method reported in the non-clinic based studies.
Generally, the studies reported multiple factors to be associated with self-harm at the personal level - sex, age, depression, hopelessness, psychiatric illness, alcohol and illicit drug use, at the family level - conflict with parents, at school-level - academic failure, bullying victimisation, truancy, and at the interpersonal level - breakup, sexual and physical abuse, romantic relationship problems, social support.
Various forms of abuse and violence victimisation occurring in the family, school, and interpersonal contexts were also reported. It was not possible to tell from all the studies we reviewed how often relationship problems in family, school, or social groups was marked by violence or abuse, but the circumstances of life in Ghana suggests the possibility of frequent exposure to such experiences. Relative to high-income countries, these circumstances are arguably likely to be more common in sub-Saharan Africa due to poverty, unemployment, death of parents (to AIDS), physical and sexual abuses – including (forced) child marriage – displacement by wars and conflicts, substance use and abuse (due to less than ideally regulated access to prescription medication), family conflict, among others [99, 100]. Under the circumstances, it is surprising that rates are not higher in African studies.
Findings from the qualitative studies in this review suggest some reasons for the high levels of self-harm among young people: entrenched cultural and family rules of comportment and norms of obedience and respect and the sense of powerlessness experienced by both boys and girls as linked to self-harm [22,23,24, 27, 32]. The higher prevalence estimates in females have been attributed to socially and religiously sanctioned oppression and exploitative normative gender role discrimination against women and girls [101]. Compared to young males, young females tend to be victims of more domestic chore burdens, caretaking responsibilities, sexual abuse and exploitation, exclusion from education, unemployment, and exclusion from decision making [11, 101]. Thus, as found in regional reviews of studies involving adult samples [11, 12] and psychological autopsy studies of suicide in Africa [102, 103], self-harm and suicide among women has been interpreted as protestation against socially sanctioned abuse and oppressive control, while men’s self-harm and suicide represent a quest for lost masculinity.
Strengths and limitations of this review
Our comprehensive search strategy identified a substantial literature in a previously under-reviewed geographical area. Of the 74 studies, 12 (16·2%) were peer-reviewed articles exclusively indexed in the African regional academic databases searched. These 12 papers represent a valuable addition to previous reports covering parts of sub-Saharan Africa [10].
Our categorisation of the factors associated with self-harm into personal, family, school, interpersonal level factors was motivated by the wide variation and the general lack of meaningful classification of these factors across the studies and is not without limitations. For example, in terms of the factors associated with self-harm, there is likely to be significant inherent interdependence between, for example, personal level factors and family level factors – family factors could be influencing the onset of the personal level factors and vice-versa – or between personal, school and interpersonal levels. The categorisation into intrapersonal and interpersonal factors too is therefore likely to be subject to considerable interdependence.
Future directions
Future studies should explore the prevalence estimates of self-harm among young people in non-clinical contexts such as the community and schools [6,7,8]. Participants in such prevalence studies should include other minority and vulnerable groups of young people including the homeless, and other out-of-school children and youth; lesbian, gay, bisexual, and transgender (LGBT) youth; orphans, and other children and youth in especially difficult circumstances including those with disability and in juvenile detention, who are often unrepresented or under-represented in population based studies on issues affecting young people [27, 33]. Recently, evidence of school-based studies from sub-Saharan Africa – and across the African continent, generally – indicates that the population of young people reporting LGBT and other sexual minority orientation is growing [104]. However, studies on their (mental) health needs are limited [99, 100].
Recent systematic reviews and primary studies from high-income countries indicate that street-connected children and adolescents represent a good case example of a high-risk group whose self-harm has received inadequate attention in the recent research literature [105]. In carrying out future studies, researchers should clearly define self-harm and more importantly, present to participants the operational definition used in the study, in order to facilitate recall and accurate responses.
More examination is needed of risk-factors for self-harm, not least in attempting to identify the temporal sequence of reported associations to help clarify interdependence between such factors. Future research (including qualitative studies) should also consider exploring factors such as social support, parenting styles, and school climate, which serve to protect young people in sub-Saharan Africa from engaging in self-harm. Such research can inform programmes aimed at strengthening protective and promotive factors within families and schools, and at local community levels can have significant positive effects on improving the developmental outcomes of vulnerable young people [106].
Too much research into risk and protective factors in self-harm has used concepts and measures developed in high income countries. We need to know more about specific features of life in sub-Saharan countries.
Conclusion
Together, the studies in this review suggest that self-harm is a public (mental) health challenge in young people across countries within sub-Saharan Africa. Given what we know about the link between self-harm and poor mental health, impaired social function and increased suicide risk, more research into the epidemiology, causes and treatment of self-harm in this setting is justified. Too few studies from too few countries have examined the methods of self-harm, risks, protective factors, and the reasons associated with self-harm from a culturally and socially sensitive perspective. The findings of the reviewed studies were overly influenced by the use of pre-existing Western derived models and measures.
Availability of data and materials
An unpublished protocol guiding this review was completed in June 2016 by following PRISMA-P statement [107]. A copy of the protocol is available from the first author on reasonable request. All data generated or analysed during this study are included in this published article and its supplementary information files.
Abbreviations
- IQR:
-
interquartile range
- MMAT:
-
mixed method appraisal tool
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- PRISMA-P:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analysis protocols
- SA-ETD:
-
South African national Electronic Theses and Dissertations
- WHO:
-
World Health Organization
- UNICEF:
-
United Nations International Children’s Emergency Fund
- UNDP:
-
United Nations Development Programme
References
Platt S, Bille-Brahe U, Kerkhof A, Schmidtke A, Bjerke T, Crepet P, De Leo D, Haring C, Lonnqvist J, Michel K, et al. Parasuicide in Europe: The WHO/EURO multicentre study on parasuicide: I. Introduction and preliminary analysis for 1989. Acta Psychiatrica Scandinavica. 1992;85(2):97–104. https://doi.org/10.1111/j.1600-0447.1992.tb01451.x..
World Health Organization. Practice manual for establishing and maintaining surveillance systems for suicide attempts and self-harm. Geneva: WHO; 2016.
Grandclerc S, De Labrouhe D, Spodenkiewicz M, Lachal J, Moro M-R. Relations between nonsuicidal self-injury and suicidal behavior in adolescence: a systematic review. PLoS One. 2016;11(4):e0153760. https://doi.org/10.1371/journal.pone.0153760.
Mars B, Heron J, Klonsky ED, Moran P, O'Connor RC, Tilling K, Wilkinson P, Gunnell D. Predictors of future suicide attempt among adolescents with suicidal thoughts or non-suicidal self-harm: a population-based birth cohort study. Lancet Psychiatry. 2019;6(4):327–37. https://doi.org/10.1016/S2215-0366(19)30030-6.
Madge N, Hewitt A, Hawton K, Wilde EJ, Corcoran P, Fekete S, Heeringen KV, Leo DD, Ystgaard M. Deliberate self-harm within an international community sample of young people: comparative findings from the Child & Adolescent Self-harm in Europe (CASE) study. J Child Psychol Psychiatry. 2008;49(6):667–77. https://doi.org/10.1111/j.1469-7610.2008.01879.x.
Muehlenkamp JJ, Claes L, Havertape L, Plener PL. International prevalence of adolescent non-suicidal self-injury and deliberate self-harm. Child Adolesc Psychiatry Ment Health. 2012;6(1):10. https://doi.org/10.1186/1753-2000-6-10.
Swannell SV, Martin GE, Page A, Hasking P, St John NJ. Prevalence of nonsuicidal self-injury in nonclinical samples: systematic review, meta-analysis and meta-regression. Suicide Life Threat Behav. 2014;44(3):273–303. https://doi.org/10.1111/sltb.12070.
Valencia-Agudo F, Burcher GC, Ezpeleta L, Kramer T. Nonsuicidal self-injury in community adolescents: a systematic review of prospective predictors, mediators and moderators. J Adolesc. 2018;65:25–38. https://doi.org/10.1016/j.adolescence.2018.02.012.
Mortier P, Cuijpers P, Kiekens G, Auerbach R, Demyttenaere K, Green J, Kessler R, Nock M, Bruffaerts R. The prevalence of suicidal thoughts and behaviours among college students: a meta-analysis. Psychol Med. 2018;48(4):554–65. https://doi.org/10.1017/S0033291717002215.
Aggarwal S, Patton G, Reavley N, Sreenivasan SA, Berk M. Youth self-harm in low-and middle-income countries: systematic review of the risk and protective factors. Int J Soc Psychiatry. 2017;63(4):359–75. https://doi.org/10.1177/0020764017700175.
Canetto SS. Suicidal behaviors among Muslim women. Patterns, pathways, meanings, and prevention. Crisis. 2015;36(6):447–58. https://doi.org/10.1027/0227-5910/a000347.
Mars B, Burrows S, Hjelmeland H, Gunnell D. Suicidal behaviour across the African continent: a review of the literature. BMC Public Health. 2014;14(1):606. https://doi.org/10.1186/1471-2458-14-606.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6(7):e1000100. https://doi.org/10.1371/journal.pmed.1000100.
Pienaar E, Grobler L, Busgeeth K, Eisinga A, Siegfried N. Developing a geographic search filter to identify randomised controlled trials in Africa: finding the optimal balance between sensitivity and precision. Health Inform Libraries J. 2011;28(3):210–5. https://doi.org/10.1111/j.1471-1842.2011.00936.x.
Davis RHJ. Independent Africa (1960 to present). In: Encyclopedia of African history and culture. Vol. V. New York: Facts on File; 2005.
Haddaway NR, Collins AM, Coughlin D, Kirk S. The role of Google scholar in evidence reviews and its applicability to grey literature searching. PLoS One. 2015;10(9):e0138237. https://doi.org/10.1371/journal.pone.0138237.
Hong QN, Pluye P, Fàbregues S, Bartlett G, Boardman F, Cargo M, Dagenais P, Gagnon M-P, Griffiths F, Nicolau B. VP26 A critical appraisal tool for systematic mixed studies reviews. Int J Technol Assessment Health Care. 2018;34(S1):166. https://doi.org/10.1017/s0266462318003471.
Ioannidis JP, Patsopoulos NA, Rothstein HR. Reasons or excuses for avoiding meta-analysis in forest plots. BMJ. 2008;336(7658):1413–5. https://doi.org/10.2307/20510099.
Petticrew M, Roberts H. Systematic reviews in the social sciences: a practical guide. Oxford: John Wiley & Sons; 2006.
Omigbodun O, Dogra N, Esan O, Adedokun B. Prevalence and correlates of suicidal behaviour among adolescents in Southwest Nigeria. Int J Soc Psychiatry. 2008;54(1):34–46. https://doi.org/10.1177/0020764007078360.
Kapur N, Cooper J, O'Connor RC, Hawton K. Non-suicidal self-injury v. attempted suicide: new diagnosis or false dichotomy? Br J Psychiatry. 2013;202(5):326–8. https://doi.org/10.1192/bjp.bp.112.116111.
Sefa-Dedeh A, Canetto, SS.: Women, Family and suicidal behaviour in Ghana. In: Psychology in international perspective: 50 years of the international council of psychologists. Edited by Gielen UP, Adler, LL., Milgram, NA. Amsterdam/Lisse: Swets & Zeitlinger B.V.; 1992: 299–309.
Wassenaar DR, van der Veen MB, Pillay AL. Women in cultural transition: suicidal behavior in south African Indian women. Suicide Life Threat Behav. 1998;28(1):82–93. https://doi.org/10.1111/j.1943-278X.1998.tb00628.x.
Beekrum R, Valjee SR, Collings SJ. An emic perspective on the dynamics of non-fatal suicidal behaviour in a sample of south African Indian women. S Afr J Psychol. 2011;41(1):63–73. https://doi.org/10.1177/008124631104100107.
Gage AJ. Association of child marriage with suicidal thoughts and attempts among adolescent girls in Ethiopia. J Adolesc Health. 2013;52(5):654–6. https://doi.org/10.1016/j.jadohealth.2012.12.007.
Kritzinger AM. Investigations into adolescent non-fatal suicidal behaviour at a Gauteng public hospital: patient and staff experiences. Doctoral thesis. Pretoria: University of Pretoria; 2018.
Meissner BL, Bantjes J. Disconnection, reconnection and autonomy: four young south African men’s experience of attempting suicide. J Youth Stud. 2017;20(7):781–97. https://doi.org/10.1080/13676261.2016.1273512.
Kinyanda E, Kizza R, Levin J, Ndyanabangi S, Abbo C. Adolescent suicidality as seen in rural northeastern Uganda. Crisis. 2011;32(1):43–51. https://doi.org/10.1027/0227-5910/a000059.
Pretorius S. Deliberate self-harm among adolescents in south African children’s homes Master Thesis. South Africa: University of Pretoria; 2011.
Swahn MH, Palmier JB, Kasirye R, Yao H. Correlates of suicide ideation and attempt among youth living in the slums of Kampala. Int J Environ Res Public Health. 2012;9(2):596–609. https://doi.org/10.3390/ijerph9020596.
Asante KO, Meyer-Weitz A. Prevalence and predictors of suicidal ideations and attempts among homeless children and adolescents in Ghana. J Child Adolesc Ment Health. 2017;29(1):27–37. https://doi.org/10.2989/17280583.2017.1287708.
Shilubane HN, Ruiter RA, Bos AE, van den Borne B, James S, Reddy PS. Psychosocial determinants of suicide attempts among black south African adolescents: a qualitative analysis. J Youth Stud. 2012;15(2):177–89. https://doi.org/10.1080/13676261.2011.634400.
Cheng Y, Li X, Lou C, Sonenstein FL, Kalamar A, Jejeebhoy S, Delany-Moretlwe S, Brahmbhatt H, Olumide AO, Ojengbede O. The association between social support and mental health among vulnerable adolescents in five cities: findings from the study of the well-being of adolescents in vulnerable environments. J Adolesc Health. 2014;55(6):S31–8. https://doi.org/10.1016/j.jadohealth.2014.08.020.
Flisher A, Ziervogel C, Chalton D, Leger P, Robertson B. Risk-taking behaviour of cape peninsula high-school students. Part II. Suicidal behaviour. S Afr Med J. 1993;83(7):474–6.
Kebede D, Ketsela T. Suicide attempts in Ethiopian adolescents in Addis Abeba high schools. Ethiop Med J. 1993;31(2):83–90.
Peltzer K, Cherian V, Cherian L. Cross-cultural attitudes towards suicide among south African secondary school pupils. East Afr Med J. 2000;77(3):165–7.
Madu S, Matla M. The prevalence of suicidal behaviours among secondary school adolescents in the Limpopo Province, South Africa. S Afr J Psychol. 2003;33(2):126–32. https://doi.org/10.1177/008124630303300208.
Wild LG, Flisher AJ, Lombard C. Suicidal ideation and attempts in adolescents: associations with depression and six domains of self-esteem. J Adolesc. 2004;27(6):611–24. https://doi.org/10.1016/j.adolescence.2004.03.001.
Sommer M. Suicidal behaviour of high school students: attempts, ideation and risk factors of south African and German adolescents Master' Thesis. South Africa: University of South Africa; 2005.
Flisher AJ, Ward CL, Liang H, Onya H, Mlisa N, Terblanche S, Bhana A, Parry CD, Lombard CJ. Injury-related behaviour among south African high-school students at six sites. S Afr Med J. 2006;96(9):825–30.
Shiferaw S, Fantahun M, Bekele A. Psychosocial problems among students in preparatory school, in Dessie town, north East Ethiopia. Ethiop J Health Dev. 2006;20(1):47–55.
Peltzer K. Social support and suicide risk among secondary school students in Cape Town, South Africa. Psychol Rep. 2008;103(3):653–60. https://doi.org/10.2466/pr0.103.3.653-660.
Mashego TB, Madu S. Suicide-related behaviours among secondary school adolescents in the Welkom and Bethlehem areas of the Free State province (South Africa). S Afr J Psychol. 2009;39(4):489–97. https://doi.org/10.1177/008124630903900410.
Nanewortor FS. Impact of religiosity, Africentric values and psychological distress on adolescent suicidal ideation. Master Thesis. Ghana: University of Ghana; 2011.
Campbell CS. Life stressors and resources as predictors of adolescent suicide attempt Master Thesis. South Africa: University of the Free State; 2012.
Van Niekerk L, Scribante L, Raubenheimer P. Suicidal ideation and attempt among south African medical students. South Afr Med J. 2012;102(6):372–3. https://doi.org/10.7196/samj.5503.
Vawda NB. Associations between family suicide and personal suicidal behaviour among youth in KwaZulu-Natal, South Africa. South Afr Fam Practc. 2012;54(3):244–9. https://doi.org/10.1080/20786204.2012.10874222.
Muula AS, Siziya S, Rudatsikira E. Self-inflicted serious injuries among adolescents in Zambia. Tanzania J Health Res. 2013;15(1):1–8. https://doi.org/10.4314/thrb.v15i1.7.
Shilubane HN, Ruiter RA, van den Borne B, Sewpaul R, James S, Reddy PS. Suicide and related health risk behaviours among school learners in South Africa: results from the 2002 and 2008 national youth risk behaviour surveys. BMC Public Health. 2013;13(1):926. https://doi.org/10.1186/1471-2458-13-926.
van Rooyen C. An exploratory study of deliberate self-harm in a south African student population Master Thesis. South Africa: University of Pretoria; 2013.
Chinawa J, Manyike P, Obu H, Odetunde O, Aniwada E, Ndu I, Chinawa A. Behavioral disorder amongst adolescents attending secondary school in Southeast Nigeria. Behav Neurol. 2014;2014:1–10. https://doi.org/10.1155/2014/705835.
Lippi C. An exploratory study of the relationship between deliberate self-harm and symptoms of depression and anxiety among a south African university population. Master Thesis. South Africa: University of Pretoria; 2014.
Penning SL, Collings SJ. Perpetration, revictimization, and self-injury: traumatic reenactments of child sexual abuse in a nonclinical sample of south African adolescents. J Child Sex Abuse. 2014;23(6):708–26. https://doi.org/10.1080/10538712.2014.931319.
Randall JR, Doku D, Wilson ML, Peltzer K. Suicidal behaviour and related risk factors among school-aged youth in the Republic of Benin. PLoS One. 2014;9(2):e88233. https://doi.org/10.1371/journal.pone.0088233.
Shilubane HN, Ruiter RA, Bos AE, van den Borne B, James S, Reddy PS. Psychosocial correlates of suicidal ideation in rural south African adolescents. Child Psychiatry Hum Dev. 2014;45(2):153–62. https://doi.org/10.1007/s10578-013-0387-5.
Cluver L, Orkin M, Boyes ME, Sherr L. Child and adolescent suicide attempts, suicidal behavior, and adverse childhood experiences in South Africa: a prospective study. J Adolesc Health. 2015;57(1):52–9. https://doi.org/10.1016/j.jadohealth.2015.03.001.
Ng LC, Kirk CM, Kanyanganzi F, Fawzi MCS, Sezibera V, Shema E, Bizimana JI, Cyamatare FR, Betancourt TS. Risk and protective factors for suicidal ideation and behaviour in Rwandan children. Br J Psychiatry. 2015;207(3):262–8. https://doi.org/10.1192/bjp.bp.114.154591.
Giru BW. Prevalence and associated factors of suicidal ideation and attempt among high school adolescent students in Fitche Town, north Shoa, Oromia region, Ethiopia, 2012: Institutional based cross sectional study. J Health Medi Nurs. 2016;23(2016):1–12.
Shaikh MA, Lloyd J, Acquah E, Celedonia KL, Wilson ML. Suicide attempts and behavioral correlates among a nationally representative sample of school-attending adolescents in the republic of Malawi. BMC Public Health. 2016;16(1):843. https://doi.org/10.1186/s12889-016-3509-8.
van der Walt F. Self-harming behaviour among university students: a south African case study. J Psychol Afr. 2016;26(6):508–12. https://doi.org/10.1080/14330237.2016.1250420.
Akanni OO, Koleoso ON, Olashore AA, Adayonfo EO, Osundina AF, Ayilara OO. Gender and other risk factors associated with risky behaviours among Nigerian adolescents. J Adolesc. 2017;57:13–7. https://doi.org/10.1016/j.adolescence.2017.03.002.
Asante KO, Kugbey N, Osafo J, Quarshie EN-B, Sarfo JO. The prevalence and correlates of suicidal behaviours (ideation, plan and attempt) among adolescents in senior high schools in Ghana. SSM-Population Health. 2017;3:427–34. https://doi.org/10.1016/j.ssmph.2017.05.005.
James S, Reddy SP, Ellahebokus A, Sewpaul R, Naidoo P. The association between adolescent risk behaviours and feelings of sadness or hopelessness: a cross-sectional survey of south African secondary school learners. Psychol Health Med. 2017;22(7):778–89. https://doi.org/10.1080/13548506.2017.1300669.
Nyandindi US. Tanzania Mainland Global School-based Student Health Survey Country Report; 2017.
Peltzer K, Pengpid S. Lifestyle and mental health among school-going adolescents in Namibia. J Psychol Afr. 2017;27(1):69–73. https://doi.org/10.1080/14330237.2016.1268293.
Stansfeld SA, Rothon C, Das-Munshi J, Mathews C, Adams A, Clark C, Lund C. Exposure to violence and mental health of adolescents: south African health and well-being study. BJPsych Open. 2017;3(5):257–64. https://doi.org/10.1192/bjpo.bp.117.004861.
Amare T, Meseret Woldeyhannes S, Haile K, Yeneabat T. Prevalence and associated factors of suicide ideation and attempt among adolescent high school students in Dangila town, Northwest Ethiopia. Psychiatry J. 2018;2018. https://doi.org/10.1155/2018/7631453.
Khuzwayo N, Taylor M, Connolly C. High risk of suicide among high-school learners in uMgungundlovu district, KwaZulu-Natal Province, South Africa. South Afr Med J. 2018;108(6):517–23. https://doi.org/10.7196/samj.2018.v108i6.12843.
Liu X, Huang Y, Liu Y. Prevalence, distribution, and associated factors of suicide attempts in young adolescents: school-based data from 40 low-income and middle-income countries. PLoS One. 2018;13(12):e0207823. https://doi.org/10.1371/journal.pone.0207823.
van der Wal W, George AA. Social support-oriented coping and resilience for self-harm protection among adolescents. J Psychol Afr. 2018;28(3):237–41. https://doi.org/10.1080/14330237.2018.1475508.
Baiden P, Kuuire VZ, Shrestha N, Tonui BC, Dako-Gyeke M, Peters KK. Bullying victimization as a predictor of suicidal ideation and suicide attempt among senior high school students in Ghana: results from the 2012 Ghana global school-based health survey. J Sch Violence. 2019;18(2):300–17. https://doi.org/10.1080/15388220.2018.1486200.
Brittain K, Myer L, Phillips N, Cluver LD, Zar HJ, Stein DJ, Hoare J. Behavioural health risks during early adolescence among perinatally HIV-infected south African adolescents and same-age, HIV-uninfected peers. Aids Care. 2019;31(1):131–40. https://doi.org/10.1080/09540121.2018.1533233.
Darré T, Consuela KAC, Saka B, Djiwa T, Ekouévi KD, Napo-Koura G. Suicidal ideation and suicide attempts in subjects aged 15–19 in Lomé (Togo). BMC Res Notes. 2019;12(1):187. https://doi.org/10.1186/s13104-019-4233-0.
Koyanagi A, Oh H, Carvalho AF, Smith L, Haro JM, Vancampfort D, Stubbs B, Devylder JE. Bullying victimization and suicide attempt among adolescents aged 12–15 years from 48 countries. J Am Acad Child Adolesc Psychiatry. 2019;58(9):907–18. https://doi.org/10.1016/j.jaac.2018.10.018.
Koyanagi A, Stubbs B, Oh H, Veronese N, Smith L, Haro JM, Vancampfort D. Food insecurity (hunger) and suicide attempts among 179,771 adolescents attending school from 9 high-income, 31 middle-income, and 4 low-income countries: a cross-sectional study. J Affect Disord. 2019;248:91–8. https://doi.org/10.1016/j.jad.2019.01.033.
Nguyen KH, Padilla M, Villaveces A, Patel P, Atuchukwu V, Onotu D, Apondi R, Aluzimbi G, Chipimo P, Kancheya N. Coerced and forced sexual initiation and its association with negative health outcomes among youth: results from the Nigeria, Uganda, and Zambia violence against children surveys. Child Abuse Negl. 2019;96:104074. https://doi.org/10.1016/j.chiabu.2019.104074.
Quarshie ENB, Cheataa-Plange HV, Annor F, Asare-Doku W, Lartey JKS. Prevalence of suicidal behaviour among nursing and midwifery college students in Ghana. Nursing Open. 2019;6:897–906. https://doi.org/10.1002/nop2.271.
Shayo FK, Lawala PS. Does food insecurity link to suicidal behaviors among in-school adolescents? Findings from the low-income country of sub-Saharan Africa. BMC Psychiatry. 2019;19(1):227. https://doi.org/10.1186/s12888-019-2212-6.
Thornton VJ, Asanbe CB, Denton ED. Clinical risk factors among youth at high risk for suicide in South Africa and Guyana. Depression Anxiety. 2019;36(5):423–32. https://doi.org/10.1002/da.22889.
Tolulope O, Olutayo A, Babatunde S, Adesanmi A. Suicidality in a non-clinical sample of Nigerian adolescents: prevalence and correlates. Suicidology Online. 2019;10(7):1–8.
Uddin R, Burton NW, Maple M, Khan SR, Khan A. Suicidal ideation, suicide planning, and suicide attempts among adolescents in 59 low-income and middle-income countries: a population-based study. Lancet Child Adolescent Health. 2019;3(4):223–33. https://doi.org/10.1016/s2352-4642(18)30403-6.
Vancampfort D, Stubbs B, Mugisha J, Firth J, Van Damme T, Smith L, Koyanagi A. Leisure-time sedentary behavior and suicide attempt among 126,392 adolescents in 43 countries. J Affect Disord. 2019;250:346–53. https://doi.org/10.1016/j.jad.2019.03.053.
Cummins R, Allwood C. Suicide attempts or threats by children and adolescents in Johannesburg. S Afr Med J. 1984;66:726–9.
Schlebusch L. Self-destructive behaviour in adolescents. S Afr Med J. 1985;68(11):792–5.
Pillay AL. Factors precipitating parasuicide among young south African Indians. Psychol Rep. 1987;61(2):545–6. https://doi.org/10.2466/pr0.1987.61.2.545.
Pillay AL. Methods of self-destructive behaviour in adolescents and young adults. Psychol Rep. 1988;63(2):552–4. https://doi.org/10.2466/pr0.1988.63.2.552.
Pillay AL, Wassenaar DR. Rescue expectations and hopelessness in adolescent parasuicides. Percept Mot Skills. 1991;72(2):363–6. https://doi.org/10.2466/pms.1991.72.2.363.
Mhlongo T, Peltzer K. Parasuicide among youth in a general hospital in South Africa. Curationis. 1999;22(2):72–6. https://doi.org/10.4102/curationis.v22i2.735.
Yéo-Tenena YJ, Yao YP, Bakayoko AS, N'dja GR, Kouamé LM, Soro SJ, Delafosse RC. Étude descriptive des conduites suicidaires des adolescents à Abidjan (Descriptive study of suicidal adolescents conducted in Abidjan). L'Encephale. 2010;36:D41–7. https://doi.org/10.1016/j.encep.2008.08.007.
Okoko AR, Ekouya Bowassa G, Oko APG, Mbika-Cardorelle A, Dzalamou M, Moyen GM. Tentatives de suicide de l’enfant et de l’adolescent a` Brazzaville (Suicide attempts by children and teenagers in Brazzaville). Archives de Pediatrie. 2011;18(7):810–1. https://doi.org/10.1016/j.arcped.2011.04.018.
Fine G, Alison H, Van der Westhuizen D, Krüger C. Predicting frequency of suicide attempts of adolescent outpatients at Weskoppies hospital using clinical and demographic characteristics. S Afr J Psychiatry. 2012;18(1):22–6. https://doi.org/10.4102/sajpsychiatry.v18i1.271.
Devries KM, Mak JY, Bacchus LJ, Child JC, Falder G, Petzold M, Astbury J, Watts CH. Intimate partner violence and incident depressive symptoms and suicide attempts: a systematic review of longitudinal studies. PLoS Med. 2013;10(5):e1001439. https://doi.org/10.1371/journal.pmed.1001439.
Serafini G, Canepa G, Adavastro G, Nebbia J, Murri MB, Erbuto D, Pocai B, Fiorillo A, Pompili M, Flouri E, et al. The relationship between childhood maltreatment and non-suicidal self-injury: a systematic review. Front Psychiatry. 2017;8. https://doi.org/10.3389/fpsyt.2017.00149.
Liu RT, Scopelliti KM, Pittman SK, Zamora AS. Childhood maltreatment and non-suicidal self-injury: a systematic review and meta-analysis. Lancet Psychiatry. 2018;5(1):51–64. https://doi.org/10.1016/s2215-0366(17)30469-8.
Pillay AL, Wassenaar DR. Family dynamics, hopelessness and psychiatric disturbance in parasuicidal adolescents. Aust N Z J Psychiatry. 1997;31(2):227–31. https://doi.org/10.3109/00048679709073825.
Madu SN, Matla M-QP. Family environmental factors as correlates for adolescent suicidal behaviors in the Limpopo Province of South Africa. Soc Behav Pers Int J. 2004;32(4):341–53. https://doi.org/10.2224/sbp.2004.32.4.341.
Carvalho AF, Stubbs B, Vancampfort D, Kloiber S, Maes M, Firth J, Kurdyak PA, Stein DJ, Rehm J, Koyanagi A. Cannabis use and suicide attempts among 86,254 adolescents aged 12–15 years from 21 low-and middle-income countries. European Psychiatry. 2019;56:8–13. https://doi.org/10.1016/j.eurpsy.2018.10.006.
Osafo J, Akotia CS, Andoh-Arthur J, Quarshie EN-B. Attempted suicide in Ghana: motivation, stigma, and coping. Death Studies. 2015;39(5):274–80. https://doi.org/10.1080/07481187.2014.991955.
Kabiru CW, Izugbara CO, Beguy D. The health and wellbeing of young people in sub-Saharan Africa: an under-researched area? BMC Int Health Hum Rights. 2013;13(1):11. https://doi.org/10.1186/1472-698x-13-11.
Patton GC, Sawyer SM, Santelli JS, Ross DA, Afifi R, Allen NB, Arora M, Azzopardi P, Baldwin W, Bonell C. Our future: a lancet commission on adolescent health and wellbeing. Lancet. 2016;387(10036):2423–78. https://doi.org/10.1016/S0140-6736(16)00579-1.
Petroni S, Patel V, Patton G. Why is suicide the leading killer of older adolescent girls? Lancet. 2015;386(10008):2031–2. https://doi.org/10.1016/S0140-6736(15)01019-3.
Kizza D, Knizek B, Kinyanda E, Hjelmeland H. An escape from agony: a qualitative psychological autopsy study of women's suicide in a post-conflict northern Uganda. Int J Qual Stud Health Well Being. 2012;7(1):18463. https://doi.org/10.3402/qhw.v7i0.18463.
Adinkrah M. Better dead than dishonored: masculinity and male suicidal behavior in contemporary Ghana. Soc Sci Med. 2012;74(4):474–81. https://doi.org/10.1016/j.socscimed.2010.10.011.
Mucherah W, Owino E, McCoy K. Grappling with the issue of homosexuality: perceptions, attitudes, and beliefs among high school students in Kenya. Psychol Res Behav Manag. 2016;9:253–62. https://doi.org/10.2147/PRBM.S112421.
Woan J, Lin J, Auerswald C. The health status of street children and youth in low-and middle-income countries: a systematic review of the literature. J Adolescent Health. 2013;53(3):314–21. e312. https://doi.org/10.1016/j.jadohealth.2013.03.013.
Patel V, Flisher AJ, Nikapota A, Malhotra S. Promoting child and adolescent mental health in low and middle income countries. J Child Psychol Psychiatry. 2008;49(3):313–34. https://doi.org/10.1111/j.1469-7610.2007.01824.x.
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1. https://doi.org/10.1186/2046-4053-4-1.
Acknowledgements
We wish to thank Judy Wright (a Senior Information Specialist at the University of Leeds) for her assistance with developing comprehensive systematic literature search strategies for this review. We also thank Thirze Hermans, and acknowledge Pauline Oustric in the School of Psychology, University of Leeds, for the translation of eligible French publications into English. We are also grateful to all the suicidologists, authors and self-harm researchers who responded to our correspondence requesting for papers from their personal records for inclusion in this systematic review.
Funding
This systematic review was supported by the Leeds International Research Scholarship (LIRS) at the University of Leeds, School of Psychology, in the form of a doctoral scholarship to the first author (EQ) - [Grant №: CFN/sy/200631403]. The funder of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Author information
Authors and Affiliations
Contributions
EQ, MW and AH conceived this study; EQ performed the literature search, extracted the data and conducted narrative analysis; AH and MW contributed to the eligibility screening consensus discussion to ensure accuracy of data extraction; EQ drafted the manuscript. All the authors contributed to the interpretation of results and revision of the manuscript and approved the final version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This systematic review received ethical approval from the School of Psychology Ethics Committee University of Leeds, UK (Ref. №: 16–0373). Consent to participate is not applicable.
Consent for publication
Not applicable.
Competing interests
EQ authored two of the cross-sectional studies included in this review. We declare no other competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1.
PRISMA flow chart.
Additional file 2.
PRISMA checklist.
Additional file 3.
Search strategies.
Additional file 4.
Authors contacted.
Additional file 5.
Sources of included studies.
Additional file 6.
Methods and designs used by studies.
Additional file 7.
Methodological quality ratings of studies.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Quarshie, E.NB., Waterman, M.G. & House, A.O. Self-harm with suicidal and non-suicidal intent in young people in sub-Saharan Africa: a systematic review. BMC Psychiatry 20, 234 (2020). https://doi.org/10.1186/s12888-020-02587-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12888-020-02587-z