Abstract
Background
People with severe mental illness (SMI) living in low and middle-income countries can experience extended delays to diagnosis, which hinder access to medical treatment. The aims of this study were to describe the interval to diagnosis among these people in rural Vietnam and its associated factors.
Methods
A population-based cross-sectional study was conducted among people with SMI in two provinces in Vietnam. The delay to diagnosis was defined as the time between the first abnormal behaviour being observed by family members and the formal diagnosis of psychosis. A multilevel linear regression was used to examine the factors associated with the delay to diagnosis.
Results
Among 404 people with SMI from 370 households, the median delay to diagnosis was 11.5 months (IQR 0–168.0). Overall, 53.7% had a delay to diagnosis of less than one year (95% CI: 48.81–58.54). The financial burden of these people on their families was nearly USD 470/year. After adjusting for other factors at individual and household levels, living in a Northern province; older age, and having psychotic diagnosis before the implementation of the National Community Mental Health program (2003) were associated with a delay of more than twelve months to diagnosis.
Conclusions
These data indicate that the implementation of a national policy for community-based care has been effective in reducing the delay to diagnosis in rural Vietnam. Therefore, there is a need for strengthening the program and mental health policies, focusing on public communication to improve mental health literacy and reduce stigma against SMI.
Similar content being viewed by others

Background
Severe mental illness (SMI) is defined in three dimensions: clinical diagnosis, duration of the disorder, and the effect on social, family and workforce participation [1]. This term is commonly used to describe people experiencing psychotic disorders (such as schizophrenia, or bipolar, or schizoaffective disorders) which compromise their personal and social life long-term; and require care from both health and social sectors [2].
Substantial evidence suggests that prolonged delay to diagnosis is associated with worse treatment outcomes and lower likelihood of long-term recovery [3]. Therefore, identification of the onset of the first symptoms of SMI is critical to receiving an accurate diagnosis and to achieving optimal treatment outcomes [3,4,5]. However, many people with SMI experience a delay to diagnosis. Most studies have examined the delay to treatment for psychoses [3, 6,7,8]. There are limited research studies investigating nature of and reasons for the delay to diagnosis. Berk et al. recruited 240 adults with bipolar or schizoaffective disorders through public hospitals and the local print media in Melbourne and Geelong, Australia for a two-year prospective observational study (2006). The authors reported in the baseline data of this study that those who were aged 16–25 years received their first diagnosis of Bipolar I or Schizoaffective disorder around 6.5 years after their first experience of symptoms of mental illness. The delay decreased when the age of the study participants increased [9]. The delay in Berk et al.’s study included the period of having other diagnoses such as depression prior to the final diagnosis of psychotic disorders which contributed to the long delay to the ultimate diagnosis. In 2015, Patel et al. conducted a retrospective study using electronic mental health records from the South London and Maudsley NHS Foundation Trust (SLaM). The study used data about 1364 adults with bipolar disorders in the period 2007 to 2012. The delay to diagnosis was defined as the interval between the first time that participants presented to the SLaM and the time they received the diagnosis of bipolar disorders. The median delay was 62 days with a wide Inter Quartile Range from 17 to 243 days [10]. This delay is short when compared with Berk et al.’s study because it measured only the period from when these people started to seek medical support. Patel et al.’s study did not provide information about the interval from when the first psychotic symptoms were identified to medical help-seeking.
Several individual and family level factors have been associated with the delay to diagnosis among people with SMI. Spoorthy (2018) reported qualitative results of a hospital-based cross-sectional study in India of 25 people with SMI and their families. They concluded that individual level reasons such as unclear psychotic symptoms, onset coinciding with adverse life events, and impaired functioning influenced treatment seeking and interval to diagnosis. The influencing factors at household level were low mental health literacy, lack of social support, and financial constraints [11]. Other studies found that, at individual level, age and gender were associated with the delay [8, 9, 12,13,14]. Duration was greater among people who had first symptoms at a young age [9]. Gender was also implicated, with females being diagnosed first at a higher mean age compared to males [12]. Family-related factors such as financial burden on the family due to caring for a member with psychotic symptoms [8], lack of social support to the family [13], and lack of family awareness of the mental health problems of people with SMI and low mental health literacy [8, 13, 14] may increase the delay to diagnosis.
In comparison with high income countries, low and middle income countries are facing significant shortage of mental health professionals [15, 16], low mental health literacy, high stigma of mental illness [17] and huge treatment gap [18]. The underlying causes of these problems are the lack of mental health polices [18], low expenditure on mental health [19, 20], inappropriate organization and planning of mental health services [21], and lack of evidence based intervention and training [18].
In general, investigations of the delay to diagnosis have recruited participants from clinical facilities, not in the community or from the population at large and only limited individual and household factors have been examined. In addition, there was no consistency in the definitions of delays to diagnosis among these studies. Therefore, it may not represent the actual delay of people with SMI in the population. In order to address the gap, this study aimed to estimate the delay to diagnosis of people with SMI and its related factors at both individual and household level in a population-based sample in Vietnam.
Methods
Study design
The study used a population-based cross-sectional design with data collected in surveys of households with a member with SMI in rural provinces in the North and the South of Vietnam. The survey was conducted from May to June 2013.
Setting
Vietnam’s socio-political and geographic situation is described mainly in terms of its having Northern and Southern areas. In Vietnamese history, the Northern and Southern areas were ruled by different Lords. During the periods of colonial occupation by France and the United States, Northern Vietnam was most strongly affiliated with the communist states of the Soviet Union and China. Southern Vietnam, allied with France and America developed a free market economy, and a quasi-democratic government. In 1975, the two areas were united, however, there are many differences between them in terms of culture, language-use, living standards, and common individual characteristics.
The household survey was implemented in two provinces Thanh Hoa in the North and Ben Tre in the South which are representative of the Northern and Southern areas. Thanh Hoa has the third highest population in Vietnam with approximately 3.4 million people living in 27 districts. The province has 6 coastal, 11 mountainous and 10 plain land districts and a city. The average annual income per capita was approximately 19 million Vietnam dong (about USD 980) in 2013 [22]. Ben Tre province has a population of around 1,2 million people living in 1 city and 8 districts. All are located on plain land. The average annual income per capita was nearly 26 million Vietnam dong (more than USD 1300 in 2013) [23].
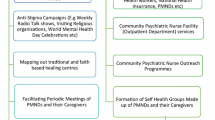
Vietnam’s national community mental health program has two main activities. First, psychiatrists of provincial mental health hospitals assess whether people identified by the commune health staff or caregivers have diagnosable conditions, including schizophrenia, bipolar disorders, and epilepsy. Second, the program distributes free medications through community outreach to people meeting diagnostic criteria for one of these conditions [24]. The program was initiated in 2000, to cover more than 7000 communes in the 63 provinces in Vietnam. The program was scaled up in Thanh Hoa and Ben Tre provinces in the period 2000–2003.
Random selection of households and sample size
A cluster sampling method was used. At national level, lists of provinces in each of the Northern and Southern areas were developed. One province was selected using simple random sampling from each list. In each province, an independent statistician chose 30 communes randomly by systematic sampling.
In each selected commune, 10 households were selected randomly from the list provided by commune health stations staff of households in which a person with a diagnosed SMI lived. People with SMI were defined as those who had been given a formal diagnosis of schizophrenia, or a bipolar affective disorder by a clinician from a public mental health hospital. They were managed by the national community mental health program at the local commune health station [24]. The household list included six households per commune for the interview, and four households to replace any of the six households if the person to be interviewed was not at home at the time the interviewers visited.
Data collection tools and sources
Data were gathered at household and individual levels by interviewing the main caregivers. At the individual level, information about the person with SMI was collected. At the household level, a structured schedule was used to ascertain household characteristics (Table 1).
Procedure
Local staff of the provincial Departments of Health and of Labour, Invalids and Social Affairs were employed for data collection due to their familiarity with local accents, customs, and transport access. They were trained for three days by the research team from the Research and Training Centre for Community Development (RTCCD) in Hanoi, which was the research implementing organisation. Staff members who were qualified in terms of interpersonal skills, comprehension of the schedule, and attention to details were selected as data collectors.
Village heads invited all main caregivers of people with SMI on the lists to attend an information session at the commune health station. Information about the research and an explanation that participation was voluntary were provided to caregivers before consent to participate in an interview was sought. On the scheduled day of the interview, village heads guided the data collectors to selected households in the list.
At the household, information about the household was collected first. All caregivers were given an oral or written explanatory form of the study and were asked to sign a consent form for the collection of the household characteristics and information of people with severe mental illness by the data collectors. Those who could not write provided a thumbprint or verbal consent witnessed by the village heads. The interview about household characteristics was conducted first, then it was followed by the interview to collect the information of people with SMI. All interviews were implemented a private room to ensure the confidentiality.
The research team from RTCCD selected 5% of the completed interview schedules to re-interview caregivers using the same schedule for quality checking. All schedules were checked onsite by field supervisors for missing values and logical mistakes for correction. No name was written on the paper-based schedule.
Consent forms and completed paper-based schedules were handed to the research team at the end of the data collection day by data collectors and were stored in a locked box at the provincial Department of Labour, Invalids and Social Affair. It was returned to the RTCCD office in Hanoi city with the research team in a sealed box.
Data management and analysis
Data from the completed paper-based schedules were manually double-entered into a password protected Access database at the RTCCD office in Hanoi. Each informant had a unique identification number that allowed the research team to distinguish individual and household characteristics. The paper records were stored in a locked cabinet and were accessible only to the research team.
Delay to diagnosis was defined as the period of time between the first symptoms of disturbed thinking or behaviour being observed by family members and the first diagnosis of a psychotic illness by a mental health specialist. As all study communes had implemented the national community mental health program by the end of 2003, comparisons were made between durations of delay to diagnoses prior to December 2003 and from January 2004 to when data were collected in 2013.
The financial burden of people with SMI on their families was calculated by deducting personal annual expenses of and costs of care from their personal annual government financial support. Among income sources of people with SMI, the monthly government financial support is a fixed and stable income. Whereas, other income sources such as income from paid jobs and donations or gifts are unstable and may change over time. All costs were collected in Vietnam dong and converted to US dollars using the exchange rate in June 2013 (1USD = 20,858 Vietnam dong). The human capital method is a widely used approach among economic studies. It measures productivity costs by estimating earnings lost due to provision of informal care [25] This method was used to estimate the productivity costs of informal care valued at USD 7.67 for eight working hours in rural Vietnam.
We used Stata, Version 13.0 to analyse the data. A p-value less than 0.05 was set as the level of statistical significance. The sample had two levels (households and individuals). People in the same household shared similar household characteristics. First, we conducted a descriptive analysis at individual and household levels. Second, univariate analyses were implemented to identify factors associated with duration of delay to first diagnosis and the financial burden on the families having members with mental illness. Finally, a two-level logistic regression was performed. The dependent variable (delay to diagnosis) is binary, with a value of 0 indicating the delay to diagnosis within 1 year, and a value of 1 indicating otherwise.
Results
In total, 380 households were visited, and 370 caregivers gave consent and were included in the study. The recruitment fraction was 97%. The main reason for refusal to participate was the absence of the main caregiver from home at the time the data collectors visited. There was no difference in refusal rates between the northern and southern provinces. Overall, 370 caregivers of 404 people with SMI from 370 households provided information for the study.
Socio-economic characteristics of people with an SMI
The socio-economic characteristics of people with an SMI and their households are presented in Table 2. Most people with an SMI in the study were described as not having completed secondary school, being cared for by family members, not being married, and having no co-morbid chronic physical health problems. Most of the households had disadvantaged and mid-level economic status; and were in rural areas.
The estimated delay to diagnosis
Among 404 study participants, the median delay to diagnosis was 11.5 months. The Inter Quartile Range was from 0 to 168.0 months. The distribution of the interval to diagnosis was skewed left. Given the date at which the National Community Mental Health program had been implemented, a binary variable was created to divide the sample into two groups: those who had been diagnosed within and those diagnosed more than one year after symptoms were first apparent. Overall 217 people (53.7, 95% Confidence Interval: 48.81–58.54) had a delay to diagnosis of up to one year, and 187 people (46.3, 95% Confidence Interval: 41.46–51.19) a delay to diagnosis of more than one year.
The financial burden on families of care for people with SMI
The annual per capita income of people with SMI was about USD 260. The main income was from the government financial support (nearly USD 160 per year). Expenses of caring for them were more than USD 620 per year in which living costs and caregiving time contributed the most (approximately USD 500 per year). After deducting expenses from annual income, the financial burden on the families was more than USD 450 per year (Table 2).
Factors associated with delay to diagnosis
In the univariate analyses, at individual level, participants who lived in the Northern province, had a diagnosis made before 2003, were younger, and had lower functioning scores were more likely to have been diagnosed more than a year of onset of symptoms (Table 3). At household level, there was no statistically significant association between household factors and delay to diagnosis of more than one year (Table 4).
In the multi-level mixed-effects logistic regression, controlling for other factors (see Table 5), only living in Ben Tre province; younger age, and having psychotic diagnosis after 2003 made significant independent contributions.
Discussion
The major finding of this study is that the data reveal the benefit of the national policies for community-based outreach care on reducing the delay to diagnosis among people with severe mental illness in the community. While the government’s financial support contributed a major component to the income of people with SMI, which reduced the financial burden of informal care on their families, it but did not remove it.
The study had several strengths: [1] the use of multistage random sampling method from lists at national, provincial and commune levels to recruit a representative sample of caregivers of people with SMI. The recruitment fraction was high (97%), and data collection protocols were adhered to strictly by the local data collection teams. The interview schedule was carefully tested with local people prior to implementation to ensure that it was comprehensible.
However, we acknowledge some limitations. The quality of treatment in both public inpatient and outpatient mental health facilities is generally poor by international standards and characterised by human rights violations. Treatment adherence is low due to the use of old generation medication which are less effective and less well tolerated because of side effects [26]. Many people with SMI have partially or untreated symptoms. The main one being that people with SMI were not invited to contribute data about their own perspectives because when the project was designed expert advice that they were likely to be affected by chronic or acute symptoms of psychosis, to have cognitive impairments and to be unable to participate in an interview. Data about them were collected from their main caregivers. Second, telescoping bias is the recall effect in which people can perceive recent events as being more remote than they were and distant events as being more recent than they are. We acknowledge that this might have influenced estimates of the duration of the interval between recognition of symptoms and diagnosis. The estimates were based on the main caregiver’s recall and it is possible that the duration of the interval for people diagnosed a longer time ago was underestimated and that of people diagnosed more recently was over estimated because of telescoping bias. Overall, we don’t believe that this would have had a significant impact on our main finding about the impact of the National Community Mental Health program on reducing the delay to diagnosis for people with SMI. In addition, due to the limited mental health literacy of the population in Vietnam, the first experience of symptoms of mental illness may not have been recognised as requiring health care [27]. Finally, although the modified and adapted Social Capital assessment tool was validated for use in Vietnam, the SLOF was translated but had not been formally validated against a gold standard or other local comparator. We believe nevertheless that the strengths outweigh the limitations and that the results can be generalised nationally with considerable confidence.
Delay from first symptoms of mental illness to diagnosis
In this study, the delay to diagnosis was nearly one year with a wide inter quartile range. This is higher than found by Patel et al. in London [10], but lower than reported by Berk et al. in regional Australia [9]. In addition to the difference in the definition of the delay period used and the sample recruitment method in these studies, the most important reason to explain the short delay is low mental health literacy among Vietnamese. It contributes to prevent family members from observation of first psychotic symptoms. The symptoms are noticed when they become mild/severe or dangerous to the family or the community [27].
Financial burden of people with SMI on their family
To date, there are limited studies calculating the financial burden on the family in low and middle income countries of having members with SMI. Informal care provided by family members, relatives and friends contributes substantially to the total cost in non-health-service studies [25]. The costs are mostly attributable to productivity loss because of caregiving responsibilities for people with SMI, which preclude income generating work. In the United Kingdom (UK) (2005), these costs accounted for nearly 50% of the total discounted costs of care for people newly diagnosed with schizophrenia. The study also reported costs of £421.2 million being born by families [28]. However, due to limited information of cost estimation method, it is difficult to compare the annual expense in this study to the study in UK.
In Vietnam there is a lack of comprehensive care for people with SMI in the community such as no rehabilitation, mental health communication provided. The national community mental health program providing free medications is the only mental service in rural areas. The adherence to antipsychotic treatment of this program was reported to be low in the community [29]. The findings of this study found that the government financial support accounted for more than 60% of the income sources. Although, this support was nearly $US160 annually, it contributed significant to reduce the financial insecurity of people with SMI due to the disadvantaged household economic status. According to the Law on persons with disabilities (2010), people who are diagnosed of having severe mental illness may receive financial support from the Ministry of Labour, Invalids and Social Affairs. The financial subsidy may vary because it depends on the state budget and the severity of the mental illness [30]. The time that family members had to spend to take care of people with SMI which was mentioned as the productivity loss of informal care contributed a huge component of the expense. It is due to the low quality of treatment and the low treatment adherence of people with SMI. It led to difficult behaviours and severe disability among this group, hence their family members must spend more time of caring for them. Consequently, the average annual financial burden on the family was nearly a half of the average annual income per capita in the two provinces in 2013 (US $ 980 in Thanh Hoa and US$1300 in Ben Tre) [22, 23]. It illustrates the necessity of a comprehensive mental health care for people with SMI including rehabilitation, family education, occupational therapies, and integration activities into the community life. It would help to improve the quality of life of people with SMI and reduce the financial burden on the family.
Associated factors of the delayed duration of diagnosis
At the individual level, we found that there were several factors related to the delay to diagnosis. First, people having the diagnosis before 2003 were more likely to delay to seek diagnosis of more than one year, 2003 is the time that all study communes implemented the national community mental health program. Therefore, this result may due to the benefit of the program. The program provided examinations to all probable cases, hence people with psychotic symptoms were more likely to receive formal diagnosis. In addition, people with schizophrenia, or bipolar disorders were provided free medications from the commune health stations, and were reviewed to receive monthly financial support from the government [29]. This encouraged caregivers to disclose and seek diagnosis for their members who had psychotic symptoms or abnormal behaviour. Therefore, the program contributed to reduce the delay to diagnosis of people with SMI in the community.
Second, participants living in the Sothern province was found to have more people with the delay to diagnosis of less than one year when comparing with those in the Northern province. This may due to the difference in economic status between the two provinces. The Northern province had 60% of participants with disadvantaged economic status, while this prevalence in the Southern province was less than 40% in this study. It is clear that poor families having members with SMI often could not afford the costs of traveling to the psychiatric hospitals and health service use. This finding is similar to the results of other studies among people with psychotic disorders that financial constraint is one of the key barriers that prevent people from seeking treatment [8, 13]. In addition, stigma and discrimination related to mental disorders, especially SMI are the common problems in low and middle income countries [31]. In Vietnam, having mental illness is not a personal problem, it also affects the honour of the family [32, 33]. Therefore, it prevents family members from seeking formal diagnosis. Southern people receive a better natural living standard and were under the long-term colonisation of American and French. Their common individual characteristics were more flexible, acceptable to a new concept. As a result, less stigma related to mental illness among Southern people when comparing with the North of Vietnam. People living in the South of Vietnam are more likely to disclose and seek diagnosis and treatment of SMI.
Finally, younger age was found to be associated positively with the group of people having the delay to diagnosis of less than one year. The result was not similar to the study in Australia among people with bipolar disorder. It found that the delayed duration decreased when the age of the study participants was increased [9]. It may be explained that in our study context, caregivers may pay more attention to younger people, then it is more likely to identify the onset of psychotic symptoms. Hence, younger may be sought diagnosis and have shorter delay. Whereas, older people may have their first symptoms long time ago, family members and caregivers may be familiar with their abnormal behaviours. It may contribute to a longer delay to diagnosis among those people.
Overall, the associated factors suggest a significant need of a communication campaign to improve mental health literacy of the community and families having a member with SMI in terms of common early symptoms, and myths of SMI. It will contribute directly to reduce the delay to diagnosis.
Conclusion
The delay to diagnosis among people with SMI in Vietnam community was found to be associated strongly with the time receiving psychotic diagnosis. The findings suggested that the National Community Mental Health program had significant benefit in improving the delay to diagnosis of people with SMI. A need for strengthening the program to improve mental health literacy of the population is recommended.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- RTCCD:
-
Research and Training Centre for Community Development, Vietnam
- SLaM:
-
South London and Maudsley NHS Foundation Trust
- SMI:
-
Severe mental illness
- UK:
-
The United Kingdom
References
Schinnar AP, Rothbard AB, Kanter R, Jung YS. An empirical literature review of definitions of severe and persistent mental illness. Am J Psychiatry. 1990;147:1602–8.
Spanish Ministry of Health and Social Policy. Clinical Practice Guidelines for Psychosocial Interventions in Severe Mental Illness. Spain Ministry of Science and Innovation; 2009.
Lieberman JA, Fenton WS. Delayed detection of psychosis: causes, consequences, and effect on public health. Am J Psychiatry. 2000;157(11):1727–30.
Drancourt N, Etain B, Lajnef M, Henry C, Raust A, Cochet B, et al. Duration of untreated bipolar disorder: missed opportunities on the long road to optimal treatment. Acta Psychiatr Scand. 2013;127(2):136–44.
Díaz-Caneja CM, Pina-Camacho L, Rodríguez-Quiroga A, Fraguas D, Parellada M, Arango C. Predictors of outcome in early-onset psychosis: a systematic review. NPJ Schizophr. 2015;1:14005.
Suppes T, Leverich GS Jr, Keck PE, Nolen WA, Denicoff KD, Altshuler LL, et al. The Stanley Foundation bipolar treatment outcome network II. Demographics and illness characteristics of the first 261 patients. J Affect Disord. 2001;67:45–9.
Hirschfeld RMA, Lewis L, Vormik LA. Perceptions and impact of bipolar disorder: how far have we really come? Results of the national depressive and manic-depressive association 2000 survey of individuals with bipolar disorder. J Clin Psychiatry. 2003;64:161–74.
Qiu Y, Li L, Gan Z, Wang J, Zheng L, Zhao J, et al. Factors related to duration of untreated psychosis of first episode schizophrenia spectrum disoder. Early Interv Psychiatry. 2017;13:1–7.
Berk M, Dodd S, Callaly P, Berk L, Fitzgerald P, de Castella AR, et al. History of illness prior to a diagnosis of bipolar disorder or schizoaffective disorder. J Affect Disord. 2007;103:181–6.
Patel R, Shetty H, Jackson R, Broadbent M, Stewart R, Boydell J, et al. Delays before diagnosis and initiation of treatment in patients presenting to mental health services with bipolar disorder. PLoS One. 2015;10(5):e0126530.
Spoorthy M. Factors responsible for delay in treatment seeking in patients with psychosis- a qualitative study from central India. In: Carpenter WT, editor. Sixth Biennial SIRS conference. Oxford: Oxford University Press; 2018. p. Sumpplement 1.
Piccinelli M, Homen FG. Gender differences in the epidemiology of affective disorders and schizophrenia. Geneva: Division of Mental Health and Prevention of Substance Abuse, World Health Organization; 1997.
Spoorthy M. Factors responsible for delay in treatment seeking in patients with psychosis- a qualitative study from Central India. Schizophr Bull. 2018;44(Suppl 1):S322.
O’Callaghan E, Turner N, Renwick L, Jackson D, Sutton M, Foley SD, et al. First episode psychosis and the trail to secondary care: help-seeking and health-system delays. Soc Psychiat Epidemiol. 2010;45(3):381–91.
The China Health Statistical Yearbook in 2012 [press release]. Beijing, China: China Statistics Press; 2012.
World Health Organization. Mental health atlas 2017. Geneva: World Health Organization; 2018.
Cultural Adaptation of CBT for Serious Mental Illness: A Guide for Training and Practice [press release]. West Sussex, UK: Wiley Blackwell; 2015.
Shanaya R, Narsimha P, Muhammed I, Paul G, Pranay R, Lina G, et al. Mental health service provision in low and middle incom countries. Health Serv Insights. 2017;10:1–7.
Atlas Mental Health Resources in the World [press release]. Geneva, Switzerland: World Health Organization; 2001.
World Health Organization. Mental Health Atlas 2011. Geneva: Department of Mental Health and Substance Abuse; 2011.
Breuer E, De Silva M, Shidaye R, Petersen I, Nakku J, Jordans MJ, et al. Planning and evaluating mental health services in low- and middle-income countries using theory of change. Br J Psychiatry. 2016;208:s55–62.
Thanh Hoa Portal. Vietnam Thanh Hoa Provincial People’s Committe 2017. Available from: http://en-us.thanhhoa.gov.vn/portal/Pages/default.aspx
Ben Tre Portal. Ben Tre: Ben Tre Provincial People’s Comittee 2017. Available from: http://www.bentre.gov.vn/Pages/Homepage.aspx
Ng CH, Than PT, La CD, Than QV, Dieu CV. The national community mental health care project in Vietnam: a review for future guidance. Australas Psychiatry. 2011;19(2):143–50.
Gray AM, Clarke PM, Wolstenholme JL, Wordsworth S. Applied methods of cost-effectiveness analysis in health care. Oxford: Oxford University Press; 2011.
Nguyen T, Tran T, Tran H, Tran T, Fisher J. Challenges in integrating mental health into primary care in Vietnam. In: Okpaku S, editor. Innovations in global mental health. Cham: Springer International Publishing; 2019. p. 1–21.
Lvd H, Wright P, Van TV, Doan VDK, Broerse JEW. Perceptions of mental health and help-seeking behavior in an Urban Community in Vietnam: an explorative study. Community Ment Health J. 2011;47:574–82.
Guest J, Cookson R. Cost of schizophrenia to UK Society. An incidence-based cost-of-illness model for the first 5 years following diagnosis. Pharmacoeconomics. 1999;15(6):597–610.
Tuan T, La B, Nguyen T. Evaluation of national community mental health care project Vietnam Research and Training Center for Community Development; 2007.
Vietnam National Assembly. Law on Persons with Disabilities 2010;No. 51/2010/QH12.
Semrau M, Evans-Lacko S, Koschorke M, Ashenafi L, Thornicroft G. Stigma and discrimination related to mental illness in low- and middle-income countries. Epidemiol Psychiatr Sci. 2015;24(5):382–94.
Do M, Pham NN, Wallick S, Nastasi BK. Perceptions of mental illness and related stigma among Vietnamese populations: findings from a mixed method study. J Immigr Minor Health. 2014;16(6):1294–8.
Minas H, Edington C, La N, Kakuma R. Mental health in Vietnam. In: Minas H, Lewis M, editors. Mental health in Asia and the Pacific: historical and cultural perspectives. Springer; 2017.
Mucci A, Rucci P, Rocca P, Bucci P, Gibertoni D, Merlotti E, et al. The specific level of functioning scale: construct validity, internal consistency and factor structure in a large Italian sample of people with schizophrenia living in the community. Schizophr Res. 2014;159(1):144–50.
Schneider L, Struening E. SLOF: a behavioral rating scale for assessing the mentally ill. Soc Work Res Abstr. 1983;19:9–21.
Silva M, Harpham T, Tuan T, Bartolini R, Penny ME, Huttly SR. Psychometric and cognitive validation of a social capital measurement tool in Peru and Vietnam. Soc Sci Med. 2006;62:941–53.
Acknowledgments
We would like to thank the Research and Training Center for Community Development (RTCCD) Vietnam and its members for their support in this study.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
TT1 and HT designed the study and coordinated the data collection. TN analysed the data and drafted the manuscript. TT2 provided statistical support. SG, AH helped with shaping the manuscript. JF provided detailed input to the reporting and interpretation of the data and revisions of the manuscript. All authors have read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The protocol and the consent procedure to obtain information from people with severe mental illness in this study were approved by an independent Ethics Committee of Vietnam Union of Science and Technology Associations (Decision No.25/12/QĐ-RTCCD) and the Monash University Human Research Ethics Committee (certificate number: 9515).
The study participants were given an oral or written plain language description of the study and were asked to sign a consent form. Those who could not write provided a thumbprint or verbal consent witnessed by an independent observer.
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Nguyen, T., Tran, T., Green, S. et al. Delays to diagnosis among people with severe mental illness in rural Vietnam, a population-based cross-sectional survey. BMC Psychiatry 19, 385 (2019). https://doi.org/10.1186/s12888-019-2367-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12888-019-2367-1