Abstract
Introduction
Despite remarkable achievements in improving maternal and child health, early neonatal deaths still persist, with a sluggish decline in Ethiopia. As a pressing public health issue, it requires frequent and current studies to make appropriate interventions. Therefore, by using the most recent Ethiopian Mini Demographic Health Survey Data of 2019, we aimed to assess the magnitude and factors associated with early neonatal mortality in Ethiopia.
Methods
Secondary data analysis was conducted based on the demographic and health survey data conducted in Ethiopia in 2019. A total weighted sample of 5,753 live births was included for this study. A multilevel logistic regression model was used to identify the determinants of early neonatal mortality. The adjusted odds ratio at 95% Cl was computed to assess the strength and significance of the association between explanatory and outcome variables. Factors with a p-value of < 0.05 are declared statistically significant.
Results
The prevalence of early neonatal mortality in Ethiopia was 26.5 (95% Cl; 22.5–31.08) per 1000 live births. Maternal age 20–35 (AOR, 0.38; 95% Cl, 0.38–0.69), richer wealth index (AOR, 0.47; 95% Cl, 0.23–0.96), having no antenatal care visit (AOR, 1.86; 95% Cl, 1.05–3.30), first birth order (AOR, 3.41; 95% Cl, 1.54–7.56), multiple pregnancy (AOR, 18.5; 95% Cl 8.8–38.9), presence of less than two number of under-five children (AOR, 5.83; 95% Cl, 1.71–19.79) and Somali region (AOR, 3.49; 95% Cl, 1.70-12.52) were significantly associated with early neonatal mortality.
Conclusion
This study showed that, in comparison to other developing nations, the nation had a higher rate of early newborn mortality. Thus, programmers and policymakers should adjust their designs and policies in accordance with the needs of newborns and children’s health. The Somali region, extreme maternal age, and ANC utilization among expectant moms should all be given special consideration.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Early neonatal mortality is defined as the death of an infant within seven days of birth [1]. Globally, the number of neonatal deaths declined from 5 million in 1990 to 2.3 million in 2022. The majority of these deaths occurred during the early neonatal period, which accounts for about 1.7 million (75%) of the total neonatal deaths, and the majority (1 million) of early neonatal deaths occurred within 24 h of birth [2]. The majority of these deaths occurred in low- and middle-income nations, mostly in sub-Saharan Africa and South Asia [3,4,5]. Despite measurement actions and interventions like early initiation of breast feeding, institutional deliveries, immunization, and early newborn care for maternal and child health, neonatal mortality remains declining at a stagnant pace in Ethiopia [6, 7].
The early newborn period is the most vulnerable time for a child’s survival; neonatal mortality is a measure of the biological, demographic, and socioeconomic conditions of the nation, as well as the public health system, health system infrastructure, and pace of population growth [5, 8]. The etiology of early neonatal death is closely related to the level of country industrialization [9], which is also the direct way of measuring quality care received by a mother during antenatal care and child birth [10].
Prior research findings illustrate that socio-demographic characteristics of the mother and the children, teen pregnancy, a low level of maternal education, a skilled care provider, cultural practice, multiple births, and severe infections like sepsis, diarrhea, and asphyxia are among the major determinants of neonatal mortality [11,12,13]. However, the determinants of early neonatal mortality are still uninvestigated in the study area.
The governments of Ethiopia, in collaboration with other stakeholders, have made significant improvements in reducing maternal and child death in the past two to three decades by implementing the Health Sector Transformation Plan, Sustainable Development Goal 3, and performing strong leadership and efforts in community involvement in the health system. Thus, neonatal mortality decreased from 39 to 29 between 2005 and the 2016 Ethiopian Demographic and Health Survey (EDHS), but has remained stable after the 2016 EDHS and even showed increments to 30 deaths per 1000 live births in the 2019 EDHS [14].
It is obvious that a reduction in overall under-five mortality across the globe cannot be achieved without addressing the growing contribution of neonatal death, particularly early neonatal death, since most of the deaths were within one week of life [15]. Despite strategies that promote better survival during the neonatal period and remarkable achievements in improving maternal and child health in the country, Ethiopia is still under the burden of neonatal mortality. For instance, neonatal mortality decreased from 39 to 29 per 1,000 live births between 2005 and 2016 but has remained stable since 2016 in Ethiopia. Early neonatal mortality, which is the largest proportion of neonatal mortality, is still uninvestigated in Ethiopia.
Early neonatal death as a critical public health problem requires frequent and current studies to update information for the concerned bodies so that they might propose appropriate interventions. In addition, identifying the predictors of early neonatal mortality will help programmers and policymakers prioritize interventions. Therefore, by using the most recent Ethiopian Mini Demographic Health Survey Data of 2019, we aimed to assess the magnitude and determinants of early neonatal mortality in Ethiopia.
Method
Study setting, design, and period
A population-based cross-sectional study was conducted using secondary analysis of data from 2019 that was collected from March 21, 2019 to June 28, 2019. The study was carried out in Ethiopia, a nation in the Horn of Africa with geographic coordinates of 40.48 97° East longitude and 9.145° N latitude. The estimated total surface area of the country is 1,126,829 km2. Its neighbors are Djibouti, Eritrea, Kenya, Somalia, South Sudan, Sudan, and Somaliland. Ethiopia is divided into twelve administrative regions: Sidama, South West Peoples (a newly formed region), Amhara, Gambela, Harari, Oromia, Somalia, Southern Nation Nationalities and Peoples Region (SNNP), and two city administrations (Addis Ababa and Diredawa). Each region was stratified into urban and rural areas (212 in rural areas and 93 in urban areas).
Data source and sampling procedure
The data for this study was obtained from the 2019 Ethiopian Mini Demographic and Health Survey (EMDHS). It is the second EMDHS and the fifth implemented in Ethiopia. EMDHS is the country-representative sample survey carried out between the Ethiopian Demographic and Health Survey (EDHS). It is also designed to provide data for measuring the up-to-date progress of health sector goals, such as estimating early childhood mortality [16]. The data was gathered in collaboration with Ethiopia’s Central Statistical Agency (CSA) and Ministry of Health. The survey used a two-stage stratified sampling technique. A two-stage stratified cluster sampling technique was employed, in the first stage, with probability proportional to the enumeration area (EA) size and independent selection in each sampling stratum. A household listing operation was carried out for all selected EAs. The generalized list of households was used as a sampling frame for the second stage of household selection. In the second step of the selection process, a specific number of 30 households in each group were selected proportionally from each enumeration area by using a systematic sampling method. A detailed description of data collection and sampling procedures has been presented in the 2019 EMDHS final report [17]. In this study, a total weighted sample of 5753 early neonates from mothers who were interviewed about births in the preceding 5 years before the survey was included in this analysis. For those women who had given birth to more than one child within the five years preceding the survey, the most recent birth was used. Then, using the Kids Record (KR) file dataset, early newborn mortality was determined as an outcome variable [17].
Source and study populations
All live births throughout a seven-day period comprised the source population, whereas all live newborns aged 0–7 days within the enumeration areas (EAs) comprised the study populations.
Outcome variable
The dependent variable was early neonatal mortality, which is the death of a newborn within 7 days of birth [18, 19] that the mother encountered five years preceding the survey, and it was dichotomized as “yes” (= 1) for newborns who had died within seven days of birth and “no” (= 0) for those who were alive within one week of life. A neonate who died within seven days of birth is said to have experienced early neonatal mortality.
Independent variables
Both individual and community-level factors were reviewed from different literatures, and these include types of pregnancy, maternal age and educational level, place and mode of delivery, types of pregnancy, ANC visit, PNC visit, and wealth index. Region, residence, community ANC utilization, community women’s education, and community wealth status were community-level factors aggregated from individual-level factors.
Wealth index were categorized as poor, middle, rich [20]. ANC was classified as optimal if a mother had more than 4 visits during pregnancy period [21]. Maternal education status was categorized as no formal education, primary, secondary and higher in our study and other EDHS [22].
Community level variables
Community-level ANC use, community-level women’s illiteracy, and community-level poverty were aggregated from individual women’s characteristics of ANC use, education, and wealth index, respectively. Since the aggregate values for all generated variables have no meaning at the individual level, they were categorized into groups based on median values. Median values were used to categorize as high and low because all aggregated variables were not normally distributed. Similar procedures were applied to all aggregate variables.
Regarding the analysis of aggregation, first the individual-level variables were re-categorized and cross-tabulated with the cluster variables using Stata version 17. Then, the proportions of ANC use, no education, and poor wealth index categories for each variable proportion were computed using Microsoft Excel 2010. Then, the proportion of each variable result was imported into Stata and combined with the original Stata using a one-to-many variable combination. Finally, we categorized the proportion of each variable as high or low based on the mean proportion. The details of independent variables and their categorization are described in supplementary Table 1 below. Supplementary Table 1.
Model building for multi-level analysis
In DHS, data variables are nested by clusters, and those within the same cluster show more similarities than those with separate clusters. Thus, using the traditional logistic regression model violates the assumptions of independent observation and equal variance across clusters. Therefore, a multi-level logistic regression analysis was employed in this study in order to account for the hierarchical nature of DHS data. A bivariate multi-level logistic regression model was employed in the study to identify the variables associated with early neonatal death. In the analysis, four models were fitted. The first (null) model contains only the outcome variables to test random variability and estimate the intra-cluster correlation coefficient (ICC). The second model contains individual-level variables; the third model contains only community-level variables; and the fourth model contains both individual-level and community-level variables [23]. A p-value of 0.05 was used to declare statistical significance. Due to the hierarchical nature of the model, models were compared using deviation = -2 (log likelihood ratio), and the best-fit model was determined by taking the model with the lowest deviance. Adjusted odds ratios with corresponding 95% confidence intervals (CIs) were calculated to identify independent predictors of early neonatal death. By calculating the variance inflation factors (VIF), the variables employed in the models were checked for multi-collinarity; the results were within acceptable ranges of one to ten [9, 24, 25].
Parameter estimation method
The likelihood of an early newborn death and independent variables at the individual and community levels were estimated using both fixed effects and random effect analysis.
The fixed effect or measure of association
For the bivariate and multivariate multilevel logistic regression analyses, the Stata syntax xtmelogit was used [26].
Where, πij: the probability of the ith newborn to be died, β0: intercept, βn: regression coefficient Xij: independent variables u0j: community level error, e0ij: individual level errors [27].
Random effect analysis
Variation of the outcome variable or random effects was assessed using the proportional change in variance (PCV), intra-class correlation coefficient (ICC), and median odds ratio (MOR) [28, 29].
The ICC shows the variation in early neonatal mortality due to community characteristics which was calculated as: ICC = σ2/(σ2 + π2/3), where, σ2, variance of the cluster [30]. The higher the ICC, the more relevant the community characteristics for understanding individual variation in early neonatal mortality.
MOR is the median value of the odds ratio between the areas with the highest early neonatal death and the area with the lowest early neonatal death when randomly picking out two neonates from two clusters, which was calculated as: MOR = \(\:\text{exp}\left(\surd\:*{\upsigma\:}2\text{*}0.6745\right)\sim\text{M}\text{O}\text{R}=\text{e}\text{x}\text{p}\left(0.95\text{*}{\upsigma\:}2\right)\), where σ2 is the variance of the cluster. In this study, MOR shows the extent to which the individual probability of early neonatal mortality is determined by residential area [31].
Furthermore, the PCV illustrates how different factors account for variations in the prevalence of early neonatal mortality and is computed as \(\:PCV=(Vnull-Vcluster)/Vnull\), where Vcluster is the cluster-level variance and Vnull, is the variance of the null model [32, 33].
Ethical consideration
The authors analyzed secondary, publicly available data obtained from the DHS program database. There was no additional ethical approval, and informed consent was obtained by the authors. In order to perform our study, we registered with the DHS web archive, requested the dataset, and were granted permission to access and download the data files. According to the DHS report, all participant data was anonymized during the collection of the survey data. More details regarding DHS data and ethical standards are available online at http://www.dhsprogram.com.
Result
Socio demographic, reproductive and neonatal related characteristics of early neonatal mortality
The analysis included a total of 5,753 live births (2,969 males and 2,784 females). More than half of mothers (54.74%) had no formal education. The majority of participants’ household heads were males (79.92%), and more than half of the children were delivered at home (51.36%). Moreover, the majority of women (93.9%) gave birth via spontaneous vaginal delivery. In addition, the majority of mothers did not follow postnatal care (PNC) checkups (87.29%). Nearly two-thirds of women’s antenatal care visits were optimal (73.34%). Table 1.
Prevalence and factors associated with early neonatal mortality in Ethiopia EDHS, 2019
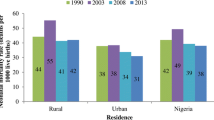
According to this study, the prevalence of early neonatal mortality in Ethiopia was 26.5 (95% Cl 22.5–31.08) per 1000 live births. The highest early neonatal mortality rate was observed in Benishingul Gumuz (54.7 per 1000 live births), whereas the lowest early neonatal mortality rate was recorded in Addis Ababa (13.7 per 1000 live births). Figure 1.
Random effect and fixed effect analysis
The null model was run to determine whether the data supported assessing randomness at the community level. The ICC value in the null model indicates 12.5% of the early neonatal mortality was due to the difference between clusters. In the null model, the median odds ratio of the odds of early neonatal mortality was 1.9 times variable between high and low clusters (heterogeneous among clusters). Regarding the final model PCV, about 92.92% of the variability in the probability of early neonatal mortality was attributed to both individual and community-level factors. The final model (III) was selected as the best-fitting model since it had the lowest deviance. Table 2.
Factors associated with early neonatal mortality
In the final model (model III) of the multivariable multilevel logistic regression model, maternal age above 35, the presence of less than two under-five children, women with no ANC visit, first birth order, multiple pregnancies, rich wealth index, and region were significantly associated with early neonatal mortality.
Accordingly, babies born from a maternal age above 35 years were 14% more likely (AOR = 1.14; 95% CI 1.14–3.6) to die as compared to babies born to a mother aged 20–34. Similarly, babies born from a rich wealth index family were 52% less likely (AOR = 0.48; 95% Cl, 0.24–0.98) to die as compared to newborns from poor mothers. First-born babies were three times (AOR = 3.41; 95% Cl, 1.54–7.56) more likely to die as compared to babies of four and above birth order. Multiple-born babies were 21 times (AOR = 21.12; 95% Cl, 12.99–44.81) more likely to die as compared to singleton birth. Babies born from mothers with no ANC visit were 92% times (AOR = 1.92; 95% Cl, 1.08–3.4) more likely to die as compared to babies born from mothers with an ANC visit. Similarly, the presence of less than two under-five children in the family made them six times (AOR = 5.8; 95% CI: 1.72–19.8) more likely to die, as opposed to women having more than three under-five children in the family. Babies born from the Somali region of Ethiopia were three times (AOR = 3.8; 95% Cl, 1.07–13.6) more likely to die as compared to babies born from the Tigray region of Ethiopia. Table 3.
Discussion
We conducted an analysis of the most recent EDHS data of 2019, as our findings revealed that the national prevalence of early neonatal mortality in Ethiopia was 26.5 (95% Cl 22.5–31.08) per 1000 live births. This study revealed a higher prevalence of early neonatal mortality in Ethiopia. Thus, it is essential to design newborn initiatives and policy priorities for the prevention of early newborn deaths. Special attention should be given to mothers with extreme maternal age, poor mothers, and the Somali region of Ethiopia.
This study finding is higher than the study done in Afghanistan, which was 14 per 1000 live births [34], and Ghana which was 16 per 1000 live births [35]. This could be due to the fact that Afghanistan has a better health care system than Ethiopia, as evidenced by the hospital bed-to-patient ratio, which was 39 per 1000 inhabitants, and the physician-to-patient ratio, which was 25 to 1000 patients as compared to Ethiopia, in which the hospital bed for 1000 inhabitants was 33 and the physician-to-patient ratio was 10 to 1000 patients [36]. In Ghana, the lower rate of early neonatal mortality could be due to differences in socio-cultural practices in handling early newborns. In addition, there are cultural, religious, and government priorities that differ for newborn care and delivery practices across countries in the world [37].
This study finding is also lower than the study done in Nigeria [38], which was 32 per 1000 live births, and Cameroon which was 126 per 1000 live birth [39]. The possible explanation could be that the Nigerian and Cameroonian studies were done prior to the Ethiopian studies. There is a time gap between the above studies and our study in which the country might have made improvements in decreasing early neonatal mortality but has not reported them. For instance, Ethiopia lowered early neonatal mortality to 26 per 1,000 live births in recent years. In addition, Cameroon studies utilized hospital records rather than demographic and health survey data, indicating that hospital records might hold an immediate obstetric, congenital, and infectious cause of early neonatal mortality over DHS data, which might lower the proportion of early newborn deaths since DHS data doesn’t incorporate variables indicating the immediate cause of early neonatal death like infectious, obstetric, asphyxia, and congenital causes of newborn death [40].
In this mixed-effects logistic regression analysis, maternal age, wealth index, birth order, multiple pregnancies, ANC visits, the number of under-five children, and the Somali region were found to be factors significantly associated with early neonatal mortality in Ethiopia.
Multiple-born babies were more likely to die as compared to single-born babies. This is supported by previous studies done in many countries across the globe [41,42,43,44]. The possible explanation could be that multiple births had a higher prevalence of prematurity [45, 46]; Prematurity is a known risk factor for early neonatal mortality, which increases neonatal death [9]. Moreover, babies born from multiple pregnancies have growth restrictions, a low Apgar score, and extremely low birth weight [47, 48]. In addition, multiple pregnancies are more likely to be complicated during pregnancy, labor, and after birth [49]. Thus, attention should be given to women with multiple pregnancies during ANC visits with early ultrasonography identification, special concern during delivery and post-partum counseling on immediate newborn care, early initiation of breastfeeding, and practicing infection prevention measures like hand washing, avoiding unnecessary contamination, and a ban on bottle feeding as much as possible.
In this study, neonates from mothers who had no ANC visit had an increased odds of early neonatal mortality as compared to neonates from mothers who had ANC visits. This finding is supported by different studies done in Bangladesh and developing countries [50, 51]. This is due to the fact that having no ANC visit during pregnancy has a negative outcome on newborn birth since early recognition and treatment of danger signs for the mother and newborn will be missed, which predisposes them to life-threatening complications. In addition, mothers with no ANC visit mightn’t acquire skilled attendants, which leads them to deliver without assistance, which leads to further complications and death [52]. Moreover, mothers who have not received an ANC visit during pregnancy are less likely to deliver in a health facility, and postnatal care might be impossible, further predisposing them to death [53]. Therefore, health education, government prioritization, and community involvement in antenatal care service utilization shall be promoted.
According to this study, first-birth-order early neonates were more likely to die as compared to fourth- and above-birth-order neonates. This is consistent with the study done in India, in which first-born newborns had a higher risk of neonatal mortality [1, 54]. The possible explanations could be the parental child-bearing trend and the lower utilization of maternity services observed in developing countries. Moreover, younger women had experienced pregnancy-related complications that ended in poor neonatal outcomes during delivery [54, 55].
Maternal age was also significantly associated with ENM in this study; accordingly, babies from advanced maternal age (above 35 years) had higher odds of death as compared to newborns from average reproductive life (20–34 years). Previous studies also depicted that extreme maternal age (< 20 and > 35 years) had a paramount influence on neonatal mortality [34, 56]. The younger maternal age could be due to the fact that mothers have no physical or reproductive capacity to bear a child [57]. Infants born to young mothers were also vulnerable to prematurity, low birth weight, and congenital anomalies [56, 58]. In addition, younger mothers lack experience in child care [59, 60]. On the other hand, late maternal age predisposes the newborn to extreme birth weight and complications during pregnancy and delivery, which increase the odds of early neonatal morbidity and mortality [34, 61, 62].
This study revealed that a higher wealth index is also negatively associated with early neonatal mortality [63]. This finding is consistent with previous investigations in Pakistan [51, 64, 65]. Child mortality has a negative correlation with a higher household wealth index. This is due to the fact that better living conditions and greater access to health care services are found in wealthier households. In wealthier households, this might lessen the chance of neonatal mortality. Conversely, less wealthy households are less likely to have access to essential amenities like drinking water, sanitary toilets, and health facilities [64].
Early neonates from families with less than or equal to two under-five children were more likely to die as compared to families with three or more under-five children in the household. This might be related to birth order, in which families may have fewer or less than two under-five children if their firstborn and subsequent babies die, since, as our studies and other studies depict, firstborn babies are more likely to die as compared to high birth-order children that might lower the number of under-five in the household [66]. Moreover, most mothers who gave birth to only one child were presumed to be young mothers who suffered one of the risks of prematurity, which is the immediate cause of newborn death [67]. Furthermore, there might be RH incompatibility in the parents that preceding newborns might be lost, which lowers the number of under-fives in the household.
Newborns from the Somali region had higher odds of mortality as compared to newborns from the Tigray region. It is known that the Somali region of Ethiopia has the highest recorded burden of neonatal death as compared to other regions of the country [68,69,70]. This could be the result of the region’s poor child and neonatal health-seeking behavior, which includes low socioeconomic status, a lack of exposure to health information, a fear of modern medical practices, an unhygienic environment in healthcare facilities, and barriers to transportation and distance that contribute to early neonatal deaths in the emerging region [71,72,73]. Hence, the government, policymakers, concerned bodies, and other stakeholders should give special attention to the Somali region of Ethiopia.
This study has its own strengths and limitations. Since it is based on data from a nationwide survey, the study has the potential to help programmers and policymakers develop effective interventions at the national level. But the DHS is primarily dependent on respondents’ self-reports, so there is a chance of recall bias in this study. Since the DHS is secondary data, variables related to obstetrics, birth asphyxia, congenital anomalies, and infectious-related variables were not incorporated or missed. In addition, due to the cross-sectional nature of the data, it cannot establish a cause-and-effect relationship and analyze behavior over a period of time. Thus, future research considering missed variables will be done.
Conclusion
The study discovered that both individual and community-level characteristics were related to early neonatal mortality. In our study, having no ANC visit, first birth order, multiple pregnancies, and socio-economic inequalities were the major determinants of early neonatal mortality. Thus, policymakers, researchers, health planners, and implementers need to give due emphasis to educating women on pregnancy, ANC visits, and improving household socio-economic status, with special attention given to the Somali region.
Data availability
The anonymized data collected is publicly available online at https://www.dhsprogram.com. The datasets used and/or analyzed during the current study will be available from the corresponding author on reasonable request.
Abbreviations
- ANC:
-
Antenatal Care
- EA:
-
Enumeration Area
- EDHS:
-
Ethiopian Demographic Health Survey
- ICC:
-
Inter cluster correlation
- ENMR:
-
Early Neonatal Mortality Rate
- LR:
-
Logistic Regression
- MOR:
-
Median Odds ratio
- PCH:
-
Primary Health care
- PCV:
-
Proportional Change in Variance
- RH:
-
Rhesus iso-immunization
References
Kumar C, Singh PK, Rai RK, Singh L. Early neonatal mortality in India, 1990–2006. J Community Health. 2013;38:120–30.
https://www.who.int/news-room/fact-sheets/detail/newborn-mortality
Sharrow D, Hug L, You D, Alkema L, Black R, Cousens S, et al. Global, regional, and national trends in under-5 mortality between 1990 and 2019 with scenario-based projections until 2030: a systematic analysis by the UN Inter-agency Group for Child Mortality Estimation. Lancet Global Health. 2022;10(2):e195–206.
Liu L, Oza S, Hogan D, Chu Y, Perin J, Zhu J, et al. Global, regional, and national causes of under-5 mortality in 2000–15: an updated systematic analysis with implications for the Sustainable Development Goals. Lancet. 2016;388(10063):3027–35.
Målqvist M. Neonatal mortality: an invisible and marginalised trauma. Global Health Action. 2011;4(1):5724.
Bellizzi S, Bassat Q, Ali MM, Sobel HL, Temmerman M. Effect of puerperal infections on early neonatal mortality: a secondary analysis of six demographic and health surveys. PLoS ONE. 2017;12(1):e0170856.
Nagalo K, Dao F, Tall FH, Yé D. Ten years morbidity and mortality of newborns hospitalized at the Clinic El-Fateh Suka (Ouagadougou, Burkina Faso). Pan Afr Med J. 2013;14:153.
Lehtonen L, Gimeno A, Parra-Llorca A, Vento M, editors. Early neonatal death: a challenge worldwide. Seminars in fetal and neonatal medicine. Elsevier; 2017.
Roy S, Haque MA. Effect of antenatal care and social well-being on early neonatal mortality in Bangladesh. BMC Pregnancy Childbirth. 2018;18:1–6.
Lawn J, Shibuya K, Stein C. No cry at birth: global estimates of intrapartum stillbirths and intrapartum-related neonatal deaths. Bull World Health Organ. 2005;83:409–17.
Titaley CR, Dibley MJ, Agho K, Roberts CL, Hall J. Determinants of neonatal mortality in Indonesia. BMC Public Health. 2008;8:1–15.
Saugstad OD. Reducing global neonatal mortality is possible. Neonatology. 2011;99(4):250–7.
Ethiopia M. Demographic and Health Survey 2019.
Collaborators MDS. Causes of neonatal and child mortality in India: a nationally representative mortality survey. Lancet. 2010;376(9755):1853–60.
Ephi M. Ethiopian Demographic and Health Survey 2019. Maryland, USA: The DHS Program ICF.: Rockville; 2021.
Ephi I. Ethiopian public health Institute (EPHI)[Ethiopia] and ICF. Ethiopia mini demographic and health survey. 2019.
Kumar C, Singh PK, Rai RK. Singh LJJoch. Early neonatal mortality in India, 1990–2006. 2013;38:120 – 30.
Lawn JE, Cousens S, Zupan JJT. 4 million neonatal deaths: when? Where? Why? 2005;365(9462):891–900.
Bitew FH. Spatio-temporal inequalities and predictive models for determinants of Undernutrition among women and children in Ethiopia. The University of Texas at San Antonio; 2020.
Belay AT, Fenta SM, Birhan Biresaw H, Abebaw Moyehodie Y, Melkam Yelam M, Mekie M. The magnitude of optimal antenatal care utilization and its associated factors among pregnant women in South Gondar zone, Northwest Ethiopia: a cross-sectional study. International journal of reproductive medicine. 2022;2022.
Neves PA, Barros AJ, Gatica-Domínguez G, Vaz JS, Baker P, Lutter CK. Maternal education and equity in breastfeeding: trends and patterns in 81 low-and middle-income countries between 2000 and 2019. Int J Equity Health. 2021;20:1–13.
Sommet N, Morselli D. Keep calm and learn multilevel logistic modeling: a simplified three-step procedure using Stata, R, mplus, and SPSS. Int Rev Social Psychol. 2017;30:203–18.
Akinyemi JO, Bamgboye EA, Ayeni O. Trends in neonatal mortality in Nigeria and effects of bio-demographic and maternal characteristics. BMC Pediatr. 2015;15(1):1–12.
Reyes J, Ramírez RP, Ramos LL, Ruiz LG, Vázquez EB, Patino VR. Neonatal mortality and associated factors in newborn infants admitted to a neonatal care unit. Arch Argent Pediatr. 2018;116(1):42–8.
Goldstein H. Multilevel statistical models. Wiley; 2011.
Snijders TA, Bosker R. Multilevel analysis: An introduction to basic and advanced multilevel modeling. 2011.
Penny W, Holmes A. Random effects analysis. Statistical parametric mapping: the analysis of functional brain images. 2007;156:165.
Borenstein M, Hedges LV, Higgins JP, Rothstein HR. A basic introduction to fixed-effect and random‐effects models for meta‐analysis. Res Synthesis Methods. 2010;1(2):97–111.
Rodriguez G, Elo I. Intra-class correlation in random-effects models for binary data. Stata J. 2003;3(1):32–46.
Merlo J, Chaix B, Ohlsson H, Beckman A, Johnell K, Hjerpe P, et al. A brief conceptual tutorial of multilevel analysis in social epidemiology: using measures of clustering in multilevel logistic regression to investigate contextual phenomena. J Epidemiol Community Health. 2006;60(4):290–7.
Eshete T, Kumera G, Bazezew Y, Mihretie A, Marie T. Determinants of inadequate minimum dietary diversity among children aged 6–23. Agric Food Secur. 2018;7(1):1–8. months in Ethiopia: secondary data analysis from Ethiopian Demographic and Health Survey 2016.
Tesema GA, Mekonnen TH, Teshale AB. Individual and community-level determinants, and spatial distribution of institutional delivery in Ethiopia, 2016: spatial and multilevel analysis. PLoS ONE. 2020;15(11):e0242242.
Kibria GMA, Burrowes V, Choudhury A, Sharmeen A, Ghosh S, Mahmud A, et al. Determinants of early neonatal mortality in Afghanistan: an analysis of the demographic and Health Survey 2015. Globalization Health. 2018;14:1–12.
Engmann C, Walega P, Aborigo RA, Adongo P, Moyer CA, Lavasani L, et al. Stillbirths and early neonatal mortality in rural Northern Ghana. Tropical Med Int Health. 2012;17(3):272–82.
https://www.worlddata.info/country-comparison.php?country1=AFG&country2=ETH.
Sutan R, Berkat S. Does cultural practice affects neonatal survival-a case control study among low birth weight babies in Aceh Province, Indonesia. BMC Pregnancy Childbirth. 2014;14:1–13.
Dahiru T. Determinants of early neonatal mortality in Nigeria: results from 2013 Nigeria DHS. J Pediatr Neonatal Care. 2015;2(5):1015406.
Koum D, Essomba N, Odile N, Ngwe I, Ndanga M, Ndombo PK, et al. Factors associated with early neonatal morbidity and mortality in an urban district hospital. Int J Latest Res Sci Technol. 2015;5(3):9–43.
Sankar M, Natarajan C, Das R, Agarwal R, Chandrasekaran A, Paul V. When do newborns die? A systematic review of timing of overall and cause-specific neonatal deaths in developing countries. J Perinatol. 2016;36(1):S1–11.
Jahn A, KYNAST-WOLF G, Kouyaté B, Becher H. Multiple pregnancy in rural Burkina Faso: frequency, survival, and use of health services. Acta Obstet Gynecol Scand. 2006;85(1):26–32.
Owais A, Faruque ASG, Das SK, Ahmed S, Rahman S, Stein AD. Maternal and antenatal risk factors for stillbirths and neonatal mortality in rural Bangladesh: a case-control study. PLoS ONE. 2013;8(11):e80164.
Kayode GA, Ansah E, Agyepong IA, Amoakoh-Coleman M, Grobbee DE, Klipstein-Grobusch K. Individual and community determinants of neonatal mortality in Ghana: a multilevel analysis. BMC Pregnancy Childbirth. 2014;14:1–12.
Bellizzi S, Sobel H, Betran AP, Temmerman M. Early neonatal mortality in twin pregnancy: findings from 60 low-and middle-income countries. J Global Health. 2018;8(1).
Giuffrè M, Piro E, Corsello G. Prematurity and twinning. J Maternal-Fetal Neonatal Med. 2012;25(sup3):6–10.
Qazi G. Obstetric and perinatal outcome of multiple pregnancy. J Coll Physicians Surg Pak. 2011;21(3):142–5.
Doyle P. The outcome of multiple pregnancy. Hum Reprod. 1996;11(suppl4):110–20.
Vogel JP, Torloni MR, Seuc A, Betrán AP, Widmer M, Souza JP, et al. Maternal and perinatal outcomes of twin pregnancy in 23 low-and middle-income countries. PLoS ONE. 2013;8(8):e70549.
Nwankwo T, Aniebue U, Ezenkwele E, Nwafor M. Pregnancy outcome and factors affecting vaginal delivery of twins at University of Nigeria Teaching Hospital, Enugu. Niger J Clin Pract. 2013;16(4).
Rahman MM, Abidin S. Factors affecting neonatal mortality in Bangladesh. J Health Manage. 2010;12(2):137–52.
Islam MA, Butt ZA, Sathi NJ. Prevalence of neonatal mortality and its Associated factors: a Meta-analysis of demographic and Health Survey Data from 21 developing countries. Dr Sulaiman Al Habib Med J. 2022;4(3):145–52.
Adjiwanou V, LeGrand T. Does antenatal care matter in the use of skilled birth attendance in rural Africa: a multi-country analysis. Soc Sci Med. 2013;86:26–34.
Pervin J, Moran A, Rahman M, Razzaque A, Sibley L, Streatfield PK, et al. Association of antenatal care with facility delivery and perinatal survival–a population-based study in Bangladesh. BMC Pregnancy Childbirth. 2012;12:1–12.
Mishra S, Ram B, Singh A, Yadav A. Birth order, stage of infancy and infant mortality in India. J Biosoc Sci. 2018;50(5):604–25.
Singh PK, Rai RK, Alagarajan M, Singh L. Determinants of maternity care services utilization among married adolescents in rural India. PLoS ONE. 2012;7(2):e31666.
Kim Y-N, Choi D-W, Kim DS, Park E-C, Kwon J-Y. Maternal age and risk of early neonatal mortality: a national cohort study. Sci Rep. 2021;11(1):814.
Fraser AM, Brockert JE, Ward RH. Association of young maternal age with adverse reproductive outcomes. N Engl J Med. 1995;332(17):1113–8.
Kang G, Lim JY, Kale AS. Adverse effects of young maternal age on neonatal outcomes. Singapore Med J. 2015;56(3):157.
Kamal SM. What is the association between maternal age and neonatal mortality? An analysis of the 2007 Bangladesh demographic and Health Survey. Asia Pac J Public Health. 2015;27(2):NP1106–17.
Suparmi S, Chiera B, Pradono J. Low birth weights and risk of neonatal mortality in Indonesia. Health Sci J Indonesia. 2016;7(2):113–7.
Chaudhary S, Contag S. The effect of maternal age on fetal and neonatal mortality. J Perinatol. 2017;37(7):800–4.
Fretts RC, Schmittdiel J, McLean FH, Usher RH, Goldman MB. Increased maternal age and the risk of fetal death. N Engl J Med. 1995;333(15):953–7.
Gebremichael SG, Fenta SM. Factors associated with U5M in the Afar Region of Ethiopia. Adv Public Health. 2020;2020:1–9.
Asif MF, Pervaiz Z, Afridi JR, Safdar R, Abid G, Lassi ZS. Socio-economic determinants of child mortality in Pakistan and the moderating role of household’s wealth index. BMC Pediatr. 2022;22:1–8.
McKinnon B, Harper S, Kaufman JS, Bergevin Y. Socioeconomic inequality in neonatal mortality in countries of low and middle income: a multicountry analysis. Lancet Global Health. 2014;2(3):e165–73.
Wakgari N, Wencheko E. Risk factors of neonatal mortality in Ethiopia. Ethiop J Health Dev. 2013;27(3):192–9.
McDermott J, Steketee R, Wirima J. Perinatal mortality in rural Malawi. Bull World Health Organ. 1996;74(2):165.
Elmi Farah A, Abbas AH, Tahir Ahmed A. Trends of admission and predictors of neonatal mortality: a hospital based retrospective cohort study in Somali region of Ethiopia. PLoS ONE. 2018;13(9):e0203314.
Tesema GA, Worku MG. Individual-and community-level determinants of neonatal mortality in the emerging regions of Ethiopia: a multilevel mixed-effect analysis. BMC Pregnancy Childbirth. 2021;21:1–11.
Ahmed AT, Farah AE, Ali HN, Ibrahim MO. Determinants of early neonatal mortality (hospital based retrospective cohort study in Somali region of Ethiopia). Sci Rep. 2023;13(1):1114.
Jalu MT, Ahmed A, Hashi A, Tekilu A. Exploring barriers to reproductive, maternal, child and neonatal (RMNCH) health-seeking behaviors in Somali region, Ethiopia. PLoS ONE. 2019;14(3):e0212227.
Wondimu H, Dejene K. Determinants of under-five malnutrition, significant changes, and policy implications in the Ethiopian Demographic Health Survey, 2019. Discover Sustain. 2022;3(1):16.
Carruth L, Mendenhall E. Wasting away: diabetes, food insecurity, and medical insecurity in the Somali Region of Ethiopia. Soc Sci Med. 2019;228:155–63.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
Berhan Tekeba made Conceptualization and drafts the original manuscript. Tadesse Tarik Tamir made software analysis. Alemneh Tadesse Kassie conceived and designs the study. Belayneh Shetie Workneh designed run the analysis. Alebachew Ferede Zegeye made supervision. Almaz Tefera Gonete made data curation. Mohammed Seid Ali wrote the summery. Mulugeta Wassie made collecting resources and edits the entire manuscript. Tewdros Getaneh Alemu checked the analysis and made substantial contributions in reviewing the design of the study and the draft manuscript. Enyew Getaneh Mekonen critically reviewed the manuscript for important intellectual content and contributed to the final approval of the version to be submitted.
Corresponding author
Ethics declarations
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Tekeba, B., Tamir, T.T., Workneh, B.S. et al. Early neonatal mortality and determinants in Ethiopia: multilevel analysis of Ethiopian demographic and health survey, 2019. BMC Pediatr 24, 558 (2024). https://doi.org/10.1186/s12887-024-05027-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-024-05027-z