Abstract
Background
Preterm birth is the leading cause of neonatal mortality accounting for 35% of all neonatal deaths worldwide, and the second most frequent cause of death for under five children. Despite different efforts, preterm neonatal mortality is still persistently high in Ethiopia. Little is known about death and its predictors among preterm neonates in the study area.
Objective
This study is aimed at estimating the incidence of mortality and its predictors among preterm neonates admitted to the NICU of NEMMCSH.
Methods and materials
: A hospital-based prospective follow-up study was conducted from January to November 2022. A total of 197 preterm neonates were selected consecutively and followed. The Kaplan-Meier survival and failure curves were used to describe the proportion of deaths over time and to compare groups. The independent effects of covariates on the hazard of death were analyzed using a multivariable Cox proportional hazard model.
Results
Preterm neonates were followed for 1840 person-days. The mean time to death was 5.68 days (SD = 5.54). The incidence of mortality was 26.08 (95% CI: 19.65, 34.61) per 1000 person days. Preterm neonates of mothers with eclamsia (AHR = 3.03), preterm neonates who have not received KMC (AHR = 2.26), and preterm neonates who have not exclusively breastfed (AHR = 4.4) had higher hazards of death as compared to their counterparts.
Conclusion and recommendation
: The mean time to death was 5.68 days (SD = 5.54). The incidence of mortality was 26.08 per 1000 person days. Eclamsia, KMC, and exclusive breastfeeding were significant predictors of death among preterm neonates. The role of KMC in reducing mortality rates and improving outcomes has to be emphasized for mothers and families. Caregivers have to ensure that mothers and families receive adequate support and resources to facilitate KMC, including access to lactation support, counseling, and assistance with practical aspects of caregiving. Counseling and practical support to enhance exclusive breastfeeding initiation and continuation have to be strengthened. Special attention has to be given to the preterm neonates of mothers with eclampsia.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
A live birth that occurs before 37 weeks of pregnancy is referred to as a preterm birth. It can occur spontaneously or be medically induced through elective cesarean birth or labor induction [1,2,3].
A premature newborn’s death during the first 28 days of life is known as preterm neonatal mortality [4]. Preterm delivery is still a major global public health issue due to its substantial role in the morbidity and death of newborns [5].
Preterm infants are at high risk for both short- and long-term complications, such as low birth weight, increased caloric needs, feeding difficulties [6], immature digestion and impaired absorption of carbohydrates and lipids [7], breathing problems [8, 9], cerebral palsy, impaired brain function, developmental delay, poorer cognitive function [10,11,12], vision and hearing problems [8, 12], perinatal asphyxia, respiratory distress syndrome (RDS), increased risk of sudden infant death, problems controlling body temperature, heart problems, hypoglycemia, and infections [12, 13].
Preterm infants place a heavy financial burden on families and hospitals because they require specialized medical care in a neonatal intensive care unit (NICU) and are more likely to need a prolonged hospital stay (days to months) [14,15,16,17].
An estimated 15 million (11%) preterm births worldwide (or 1 in 10 deliveries) take place each year (at a pace of 29 newborns each minute). 90% of preterm deliveries take place in low- and middle-income nations. Sub-Saharan Africa and South Asia account for 12.7 million preterm births, or about 85% of all preterm birth [18, 19]. The majority of sub-Saharan countries are seeing an increase in preterm birth rates [20].
Various policies, and programs are implemented worldwide with the aim of preventing and treating preterm birth and lowering mortality rates [21, 22]. Even so, it remains the leading cause of neonatal mortality accounting for 35% of all neonatal deaths worldwide, and the second most frequent cause of death for children under five accounting for 18% of all deaths [22,23,24]. Preterm delivery and its complications cause 1 million deaths in children under the age of five every year [25]. The likelihood of survival for a preterm baby is primarily determined by their place of residence; in low-income nations, over 90% of extremely preterm babies pass away in the first few days of life. However, in high-income nations, the death rate is less than 10% [19]. 13% of under-five deaths in sub-Saharan Africa and 25.5% in South Asia are attributed to preterm birth mortality [26].
The mortality rate for children under five has significantly decreased, but the fall in neonatal mortality has been sluggish, particularly in many low-income nations. Regretfully, families and medical professionals in many nations continue to believe that any premature baby will eventually die [27].
The trend of newborn death rates in Ethiopia stayed largely unchanged. In 2005, it was 39; in 2011, it was 37; in 2016, it was 29, and in 2019, there were 30 mortalities per 1000 live births [28]. One-third of these deaths are caused by prematurity [29]. Due to the prolonged hospital stays and long-term complications on the newborn’s health, preterm deliveries place a strain on society’s healthcare resources [30].
Birth weight, gestational age, mode and place of delivery, HIV, exclusive breastfeeding (EBF), postnatal surfactant administration, presence of anomalies, multiple pregnancies, non-cephalic presentation, neonatal sepsis, respiratory distress, and a low APGAR score have all been found to be predictors of death in preterm neonatal deaths [14, 31,32,33,34,35,36].
Target #3.2 of Sustainable Development Goal 3 calls for ending all preventable deaths of newborns and children under the age of five by 2030, and addressing the problem of preterm birth is crucial to reaching this goal [37]. Well-designed, context-specific, representative cohort studies from low- and middle-income countries on preterm birth are therefore required to address data gaps on preterm birth, learn from successes, and adopt best fit models in low- and middle-income settings, as the majority of the evidence on care for preterm babies comes from high-income settings [5, 38].
In Ethiopia, a large number of preterm birth-related deaths are avoidable, particularly deaths of moderate-to late-preterm births (32–37 weeks) [39].
Ethiopia has adopted the target to lower preterm birth-related deaths by 2030 [40].
The country is implementing a number of policies and initiatives, such as an expanded Neonatal Intensive Care Unit (NICU), integrated management of neonatal and pediatric disorders, and a quality improvement program, to address newborn fatalities and accomplish the goal. Preterm infant mortality remains stubbornly high despite these measures.
Besides these efforts, preterm neonatal mortality is still persistently high [35, 41]. Every year, 320,000 premature births occur, and direct preterm problems result in the deaths of 23,100 children under the age of five [42].
Although some studies were done in Ethiopia on the incidence and predictors of preterm death, the risk factors were different across the studies. The majority of these studies used secondary data, which is prone to missing data and variables. There is no information about the incidence and predictors of preterm death in the study area.
Understanding the consequences of preterm births and the factors that increase their risk of death and morbidity affects how healthcare providers treat expectant mothers and their babies and facilitates the efficient use of available resources. It contributes to improving newborn care and lowering unfavorable outcomes in these kinds of difficult births. Estimating the incidence of mortality and its predictors among preterm neonates admitted to the NICU of NEMMCSH is the aim of this study.
Methods and materials
Study area and period
This study was carried out at NEMMCSH, which is located in Hossana town, Haddiya zone, from January to December 2022. Hossana Town, the capital of Central Ethiopia, is situated 230 km from Addis Ababa, the capital of Ethiopia. In addition to providing general and specialty medical care, NEMMCSH is a public hospital that serves as a teaching hospital for medical and other health science students. The neonatal Intensive Care Unit (NICU) offers newborn care services to both inborn and out born term and preterm neonates. A hospital-based prospective follow-up study was carried out.
Treatment protocols in NICU
The treatment protocol in a Neonatal Intensive Care Unit (NICU) varies depending on the specific medical conditions and needs of the newborn. NICUs are specialized units that provide intensive medical care for premature or ill newborns. Many premature infants have underdeveloped lungs and may require assistance with breathing. This can include mechanical ventilation and continuous positive airway pressure (CPAP). Premature babies often struggle to maintain their body temperature. Incubators or radiant warmers are used to keep the baby’s temperature stable. Continuous monitoring of vital signs such as heart rate, respiratory rate, and oxygen saturation is crucial in the NICU. This helps healthcare providers promptly address any changes in the baby’s condition. Neonates in the NICU are susceptible to infections, so strict infection control measures are implemented. This includes proper hand hygiene, aseptic techniques, and the judicious use of antibiotics. Many newborns experience jaundice, a yellowing of the skin and eyes due to elevated bilirubin levels. Phototherapy may be used to treat jaundice. NICUs often emphasize family-centered care, involving parents in the care of their newborns. This includes education on baby care, involvement in decision-making, and support for emotional well-being. Medications may be administered to address specific medical conditions or to support the baby’s physiological functions [43].
Population
All preterm neonates admitted to the NICU of NEMMCSH were the source population whereas all preterm neonates admitted to the NICU at NEMMCSH from January to November 2022 comprised the study population.
Inclusion and exclusion criteria
Preterm neonates admitted to the NICU during the time of data collection were included in the study. Preterm neonates of mothers who are unable to speak and those with no immediate caregiver were excluded from the study because there are some variables measured by interviewing either mothers or caregivers.
Sample size determination and sampling technique
Using Stata version 14, the sample size was calculated with respect to a hazard ratio of 2.186 for gestational age, a standard deviation of 0.186, a 95% confidence interval, a 5% probability of type I error, 80% power, and a 29.31% probability of success (death). Taking into account the aforementioned criteria, a total of 197 preterm neonates were included in the study [44].
Data collection tool and technique
Until the required sample size was attained, the study participants were consecutively recruited into the study. Interviewer administered questionnaire and checklist were used to collect the data. The aforementioned data collection tool were adapted from different studies. Upon admission, the data collectors recruited study subjects and continued to follow them throughout their stay in the facility, documenting all clinical events until the neonates die or censored. Data collection was done by trained nurses and supervision was done by two public health experts. Up until the neonatal death or censorship, newborn data were prospectively gathered from medical records. The neonates were followed for a maximum of 28 days from birth. To assure the quality of the data, the data collection tool was evaluated by pediatricians, and 1 day of training was given to the data collectors and supervisors about general research protocols. The Principal investigator reviewed the data before entering it to ensure it was consistent and complete.
Study variables
Dependent variable
Mortality of preterm neonates.
Independent variables
maternal age, place of residence, marital status, level of education, occupation, monthly income and sex of neonates, multiple pregnancy, parity, history of abortion and/or preterm birth, Birth interval, prolonged labour, ANC visits, human immunodeficiency virus (HIV) status, DM and place of delivery, mode of delivery, type of birth attendant, antenatal corticosteroid use, neonatal postnatal age at admission, anomalies, KMC, BMI, birth weight, 1 and 5-minute APGAR score and resuscitation history, gestational age, obstetric haemorrhage, eclampsia and preeclampsia, mal-presentation, feeding problem, asphyxia, neonatal sepsis, hypothermia, jaundice, HR, RR, SPO2, and hypoglycemia.
Data analysis
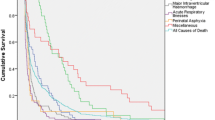
Data were entered into Epi-data for Windows and analyzed using Stata version 14. Percentages and frequencies were used to summarize categorical variables. The results were presented in tables, texts, and graphs based on the nature of the variables. The distribution of the continuous variables was checked by a box plot. Mean with standard deviation and median with interquartile range were used to summarize normally and non-normally distributed continuous variables, respectively. The Kaplan-Meier Survival and failure curve was used to describe the proportion of deaths over time and to compare groups.
Multivariable Cox proportional hazards regression
The independent effects of covariates on the hazard of death were analyzed using the multivariable Cox proportional hazards model. Variables with p-value < 0.25 in bivariable cox proportional hazards analysis were considered for multivariable cox proportional hazards analysis. Adjusted hazard ratios with their 95% confidence interval (CI) were estimated, and a p-value less than 0.05 was used to declare the presence of a significant association between predictors and preterm neonatal death.
Assessing model assumptions
The proportional hazard assumption states that the effect of the covariate is the same over time. It was tested using the global test running the estat phtest command in stata. The assumption was satisfied (p-value: 0.2042).
Operational definitions
Definitions of the terms are given in the table below (Table 1).
Results
Socio-demographic characteristics of the study participants
More than half (51.27) of the neonates were males, and 82.23% were aged less than 24 h at admission. The median gestational age was 35 weeks (IQR: 34 weeks, 35.8 weeks), and 90.82% were born at or after 32 weeks of conception. 86.29% of the neonates were born at a health facility. The mean age of the mothers was 28.74 years (SD: 5.72 years), and more than half (55.33%) of them were from rural areas (Table 2).
Maternal medical and obstetrics related characteristics
All mothers had ANC follow up and 66.33% of the neonates were born to mothers who had > = 3 ANC follow up. 31.98% of the women had multiple pregnancies, and 43.65% of the neonates were born to multipara mothers. More than three-fourths (77.66%) of the neonates were born to mothers who had not taken corticosteroids during pregnancy. More than half (21.32%) of the mothers had prolonged labor, and 3.55% of the mothers had obstetric hemorrhage. 22.34% of the neonates were born to mothers who had a history of abortion or preterm birth, and 13.71% and 9.64% of the women had preeclampsia and eclampsia, respectively (Table 3).
Neonatal admission diagnosis and treatment related characteristics
Nearly three-fourth (75.63%) of the neonates were hypothermic at admission and 74.62% of them had neonatal sepsis. More than one-third (38.58%) of the neonates had jaundice and hypoglycemia, and nearly one-fourth of them had asphyxia (24.87%). More than one-third (34.04%) of the neonates had received CPAP, and 83.25% were given early antibiotics. More than half (58.88%) of them had received KMC, and 29.44% were resuscitated (Table 4).
Incidence of mortality
The mean duration of admission was 9.42 days (SD = 6.64) and the mean time to death was 5.68 days (SD = 5.54). The total person-day observation was 1840 days. Out of 197 neonates, 48 of them died. The incidence of mortality was 26.08 (95% CI: 19.65, 34.61) per 1000 person days. The incidence of mortality was the highest (46.13 per 100 person days) within the first 24 h. Between 2nd to 7th, 8th to 14th, 15th to 21st, and 22nd to 28th, the incidence of mortality was 29.65, 24.39, 11.42, and 18.86 per 1000 person days, respectively. The cumulative probability of mortality within the first 7, 14, 21, and 28 days was 0.1715, 0.3077, 0.3569, and 0.4664, respectively. The Kaplan-Meir graph increases rapidly during the first 5 days and between the 8th and 14th days, showing most neonates died during these periods (Figs. 1 and 2).
The cumulative probability of deaths were higher among neonates who were born to mothers who had mal-presentation, eclampsia, and neonates who had not exclusively breast fed, were not resuscitated and neonates with 1 min APGAR score of 4–7(Figs. 3, 4, 5, 6 and 7).
Predictors of mortality
In a bivariable cox regression ANC, preeclampsia, eclampsia, malpresentation, KMC, hypoglycemia, and exclusive breast feeding were considered for multivariable cox regression. In multivariable Cox regression, eclampsia, exclusive breast feeding, and KMC were found to be significant predictors of death among preterm neonates.
Preterm neonates of mothers with Eclampsia had 3.03 times higher hazards of death as compared to neonates of mothers without Eclampsia (AHR = 3.03).
The hazards of death were 2.26 times higher for preterm neonates who have not received KMC as compared to those who have received the care (AHR = 2.26). Preterm neonates who have not exclusively breastfed had 4.4 times higher hazards of death as compared to neonates who have exclusively breastfed (AHR = 4.4) (Table 5).
Discussion
Preterm neonates were followed for 1840 person-days. The mean time to death was 5.68 days (SD = 5.54). The incidence of mortality was 26.08 (95% CI: 19.65, 34.61) per 1000 person days. This is nearly similar to the incidence of death reported from studies in Addis Ababa, Ethiopia [45] and Northern Ethiopia [46].
KMC, exclusive breastfeeding, and Eclampsia were significant predictors of death among preterm neonates. The hazards of death were higher for preterm neonates who have not received KMC as compared to those who have received KMC. This finding is in line with the findings in studies done at Aksum Hospital [47], University of Gondar [48] and Addis Ababa public hospitals [45], and Southern Ethiopia [49].
The increased risk of mortality in preterm newborns who have not undergone Kangaroo Mother Care (KMC) could be attributed to inadequate control of body temperature and breathing. Premature babies frequently face challenges in regulating their body temperature, and without KMC, they may be at a higher risk of experiencing hypothermia or hyperthermia, both of which can lead to fatal outcomes [50, 51]. The physical contact with the mother’s chest can improve the infant’s respiratory rhythms, decreasing the likelihood of respiratory difficulties or issues. Premature babies who have not undergone Kangaroo Mother Care (KMC) are more susceptible to respiratory distress, which raises the chances of mortality [52, 53].
Inadequate nutrition, heightened susceptibility to infections, and elevated stress levels may also contribute to the elevated mortality risks in premature newborns who have not undergone Kangaroo Mother Care (KMC). Infants who have not experienced KMC are at a higher risk of malnutrition, increasing their vulnerability to infections and other health issues [54, 55]. Premature babies are at a higher risk of infections, and KMC has been linked to a decreased occurrence of infections. The soothing impact of KMC can alleviate stress in premature infants. Newborns who have not received KMC may experience heightened stress levels, which can impact their physiological functions and overall well-being [56, 57].
Preterm neonates who have not initiated exclusive breastfeeding have greater hazards of death as compared with those who have initiated exclusive breastfeeding. Similar findings were observed in studies done in Tanzania [58], Ghana [59], India [60] and two systematic reviews [61, 62].
The increased likelihood of infections resulting from weakened immunity could clarify the greater mortality risks in premature newborns who have not exclusively breastfed [63].
The hazards of death were higher among preterm neonates of mothers who have eclampsia compared to neonates of mothers without eclampsia. A similar finding was observed in a study done in Addis Ababa [64].
The insufficient blood supply to the placenta and challenges during labor and delivery could account for the higher risks of mortality among premature newborns. Babies born prematurely to mothers with Eclampsia may experience complications such as low birth weight, respiratory issues, and underdeveloped organs, increasing their chances of mortality. Additionally, inadequate placental blood flow can lead to intrauterine growth restriction (IUGR), which is linked to low birth weight and a heightened risk of neonatal death. Eclampsia can result in labor and delivery complications like placental abruption or fetal distress, further contributing to negative outcomes for the newborn [65].
Conclusion and recommendation
Preterm neonates were followed for 1840 person-days. The mean time to death was 5.68 days (SD = 5.54). The incidence of mortality was 26.08 (95% CI: 19.65, 34.61) per 1000 person days. Eclampsia, KMC, and exclusive breastfeeding were significant predictors of death among preterm neonates. Awareness should be created for parents and caregivers about the benefits and importance of KMC for preterm neonates. The role of KMC in reducing mortality rates and improving outcomes has to be emphasized for mothers and families. Caregivers have to ensure that mothers and families receive adequate support and resources to facilitate KMC, including access to lactation support, counseling, and assistance with practical aspects of caregiving. Early and thorough nutritional assessments for preterm neonates are essential to identify those who may face challenges with exclusive breastfeeding. Counseling and practical support to enhance breastfeeding initiation and continuation have to be strengthened. Special attention has to be given to the preterm neonates of mothers with eclampsia.
Data availability
All data generated or analysed during this study are included in this published article [and its supplementary information files].
References
Goldenberg RL, Culhane JF, Iams JD, Romero R. Epidemiology and causes of preterm birth. Lancet. 2008;371(9606):75–84.
Walani SR. Global burden of preterm birth. Int J Gynecol Obstet. 2020;150(1):31–3.
Taha Z, Ali Hassan A, Wikkeling-Scott L, Papandreou D. Factors associated with preterm birth and low birth weight in Abu Dhabi, the United Arab Emirates. Int J Environ Res Public Health. 2020;17(4):1382.
Chang HH, Larson J, Blencowe H, Spong CY, Howson CP, Cairns-Smith S, Lackritz EM, Lee SK, Mason E, Serazin AC. Preventing preterm births: analysis of trends and potential reductions with interventions in 39 countries with very high human development index. Lancet. 2013;381(9862):223–34.
Vogel JP, Chawanpaiboon S, Moller A-B, Watananirun K, Bonet M, Lumbiganon P. The global epidemiology of preterm birth. Best Pract Res Clin Obstet Gynecol. 2018;52:3–12.
Engle WA, Tomashek KM, Wallman C. Late-preterm infants: a population at risk. Pediatrics. 2007;120(6):1390–401.
Barlow S, Finan D, Lee J, Chu S. Synthetic orocutaneous stimulation entrains preterm infants with feeding difficulties to suck. J Perinatol. 2008;28(8):541–8.
Ward RM, Beachy JC. Neonatal complications following preterm birth. BJOG: Int J Obstet Gynecol. 2003;110:8–16.
Baraldi E, Filippone M. Chronic lung disease after premature birth. N Engl J Med. 2007;357(19):1946–55.
Vincer MJ, Allen AC, Joseph K, Stinson DA, Scott H, Wood E. Increasing prevalence of cerebral palsy among very preterm infants: a population-based study. Pediatrics. 2006;118(6):e1621–6.
Ophthalmology AAoPSo. Screening examination of premature infants for retinopathy of prematurity. Pediatrics. 2013;131(1):189–95.
Vohr B. Long-term outcomes of moderately preterm, late preterm, and early term infants. Clin Perinatol. 2013;40(4):739–51.
De Jong M, Verhoeven M, van Baar AL. School outcome, cognitive functioning, and behaviour problems in moderate and late preterm children and adults: a review. In: Seminars in fetal and neonatal medicine: 2012: Elsevier; 2012: 163–9.
Kunle-Olowu OE, Peterside O, Adeyemi OO. Prevalence and outcome of preterm admissions at the neonatal unit of a tertiary health centre in Southern Nigeria. Open Journal of Pediatrics 2014, 2014.
Tongo O, Orimadegun A, Ajayi S, Akinyinka O. The economic burden of preterm/very low birth weight care in Nigeria. J Trop Pediatr. 2009;55(4):262–4.
Feldman R, Eidelman AI. Direct and indirect effects of breast milk on the neurobehavioral and cognitive development of premature infants. Dev Psychobiology: J Int Soc Dev Psychobiol. 2003;43(2):109–19.
Vohr BR, Poindexter BB, Dusick AM, McKinley LT, Higgins RD, Langer JC, Poole WK. Persistent beneficial effects of breast milk ingested in the neonatal intensive care unit on outcomes of extremely low birth weight infants at 30 months of age. Pediatrics. 2007;120(4):e953–9.
Hug L, Alexander M, You D, Alkema L, for Child UI-aG. National, regional, and global levels and trends in neonatal mortality between 1990 and 2017, with scenario-based projections to 2030: a systematic analysis. Lancet Global Health. 2019;7(6):e710–20.
WHO. WHO fact sheet Preterm Birth N°363. In.; November; 2015.
Chawanpaiboon S, Vogel JP, Moller A-B, Lumbiganon P, Petzold M, Hogan D, Landoulsi S, Jampathong N, Kongwattanakul K, Laopaiboon M. Global, regional, and national estimates of levels of preterm birth in 2014: a systematic review and modelling analysis. Lancet Global Health. 2019;7(1):e37–46.
Soon BT. The global action report on preterm birth. Geneva: World Health Organization; 2012.
Sheet WRF. Preterm births. Geneva, swizterland 2016.
Beck S, Wojdyla D, Say L, Betran AP, Merialdi M, Requejo JH, Rubens C, Menon R, Van Look PF. The worldwide incidence of preterm birth: a systematic review of maternal mortality and morbidity. Bull World Health Organ. 2010;88:31–8.
Adane AA, Ayele TA, Ararsa LG, Bitew BD, Zeleke BM. Adverse birth outcomes among deliveries at Gondar University hospital, Northwest Ethiopia. BMC Pregnancy Childbirth. 2014;14(1):1–8.
Blencowe H, Cousens S, Chou D, Oestergaard M, Say L, Moller A, Kinney M, Lawn J. Chap. 2: 15 million preterm births: Priorities for action based on national, regional and global estimates. Born too soon: the global action report on preterm birth 2012.
Liu L, Oza S, Hogan D, Chu Y, Perin J, Zhu J, Lawn JE, Cousens S, Mathers C, Black RE. Global, regional, and national causes of under-5 mortality in 2000–15: an updated systematic analysis with implications for the Sustainable Development Goals. Lancet. 2016;388(10063):3027–35.
Lawn JE, Davidge R, Paul VK, von Xylander S, de Graft Johnson J, Costello A, Kinney MV, Segre J, Molyneux L. Born too soon: care for the preterm baby. Reproductive Health. 2013;10(1):1–19.
Mini E, Demographic E. Health survey 2019: key indicators report. The DHS Program ICF; 2019.
Kinney MV, Rhoda NR. Understanding the causes of preterm birth: solutions depend on context. Lancet Global Health. 2019;7(8):e1000–1.
Wang P, Liou S-R, Cheng C-Y. Prediction of maternal quality of life on preterm birth and low birthweight: a longitudinal study. BMC Pregnancy Childbirth. 2013;13(1):1–11.
Agbeno EK, Osarfo J, Ashong J, Anane-Fenin B, Okai E, Ofori AA, Aliyu M, Opoku DA, Ken-Amoah S, Ashong JA. Determinants of preterm survival in a tertiary hospital in Ghana: a ten-year review. PLoS ONE. 2021;16(1):e0246005.
Aynalem YA, Mekonen H, Akalu TY, Gebremichael B, Shiferaw WS. Preterm neonatal mortality and its predictors in Tikur Anbessa Specialized Hospital, Addis Ababa, Ethiopia: a retrospective cohort study. Ethiop J Health Sci 2021, 31(1).
Haghighi L, Nojomi M, Mohabbatian B, Najmi Z. Survival predictors of preterm neonates: hospital based study in Iran (2010–2011). Iran J Reproductive Med. 2013;11(12):957.
Mekasha A, Tazu Z, Muhe L, Abayneh M, Gebreyesus G, Girma A, Berhane M, McClure EM, Goldenberg RL, Nigussie AK. Factors Associated with the death of Preterm Babies Admitted to neonatal intensive care units in Ethiopia: a Prospective, cross-sectional, and Observational Study. Global Pediatr Health. 2020;7:2333794X20970005.
Mengesha HG, Wuneh AD, Lerebo WT, Tekle TH. Survival of neonates and predictors of their mortality in Tigray region, Northern Ethiopia: prospective cohort study. BMC Pregnancy Childbirth. 2016;16(1):1–13.
Opio C, Malumba R, Kagaayi J, Ajumobi O, Kamya C, Mukose A, Adoke Y, Muneza F, Kisaakye A, Nalwadda C. Survival time and its predictors among preterms in the neonatal period post-discharge in Busoga region-Uganda June–July 2017. Journal of Interventional Epidemiology and Public Health 2019, 2(9).
Nations U. Sustainable Development Goal 3. Ensure healthy lives and promote well-being for all at all ages. https://www.un.org/sustaunable edevelopment/health/. In.
Organization WH. Survive and thrive: transforming care for every small and sick newborn: key findings. In.: World Health Organization; 2018.
Ahmad A, Madanijah S, Dwiriani CM, Kolopaking R. Complementary feeding practices and nutritional status of children 6–23 months old: formative study in Aceh, Indonesia. Nutr Res Pract. 2018;12(6):512–20.
Organization WH. Born too soon: the global action report on preterm birth. 2012.
Bekele A, Mussema Y, Tadesse Y, Taylor ME. Reaching every newborn: delivering an Integrated Maternal and Newborn Health Care Package: reaching every newborn. Ethiop Med J 2019(3).
USAID P, GAPPS A. Profile of Preterm and Low Birth Weight Prevention and Care-Ethiopia.; 2017. In.; 2019.
Sharma Y, Bansal S, Kaur R. Decision making in NICU–Role of neonatal scores in predicting/maintaining neonate’s health. Published on 24 Mar 2017. In.
Mekasha A, Tazu Z, Muhe L. Factors Associated with the death of Preterm Babies Admitted to neonatal intensive care units in Ethiopia: a Prospective, cross-sectional, and Observational Study. 2020, 7:2333794x20970005.
Birhanu D, Gebremichael B, Tesfaye T, Tadesse M, Belege F, Godie Y, Wodaje M, Tamiru E. Survival status and predictors of mortality among preterm neonates admitted to neonatal intensive care unit of Addis Ababa public hospitals, Ethiopia, 2021. A prospective cohort study. BMC Pediatr. 2022;22(1):1–12.
Girma B, Berhe H, Mekonnen F, Nigussie J. Survival and predictors of mortality among preterm neonates in Northern Ethiopia: a retrospective follow-up study. Front Pead. 2023;10:1083749.
Gebremeskel TG. MAMO S: Proportion And Factors Of Death Among Preterm Neonates Admitted In Aksum University Compressive Specialized Hospital Neonatal Intensive Care Unit Northern Ethiopia 2019. 2020.
Yismaw AE, Gelagay AA, Sisay MM. Survival and predictors among preterm neonates admitted at University of Gondar comprehensive specialized hospital neonatal intensive care unit, Northwest Ethiopia. Ital J Pediatr. 2019;45:1–11.
Huka AE, Oljira L, Weldesenbet AB, Bushra AA, Ahmed IA, Tura AK, Tuluka AA. Predictors of time to death among preterm neonates admitted to neonatal intensive care units at public hospitals in southern Ethiopia: a cohort study. PLoS ONE. 2023;18(10):e0283143.
Ludington-Hoe SM, Johnson MW, Morgan K, Lewis T, Gutman J, Wilson PD, Scher MS. Neurophysiologic assessment of neonatal sleep organization: preliminary results of a randomized, controlled trial of skin contact with preterm infants. Pediatrics. 2006;117(5):e909–23.
Messmer PR, Rodriguez S, Adams J, Wells-Gentry J, Washburn K, Zabaleta I, Abreu S. Effect of kangaroo care on sleep time for neonates. Pediatr Nurs. 1997;23(4):408–15.
Ludington-Hoe M. Evidence-based review of physiologic effects of kangaroo care. Curr Women’s Health Reviews. 2011;7(3):243–53.
Bera A, Ghosh J, Singh AK, Hazra A, Som T, Munian D. Effect of kangaroo mother care on vital physiological parameters of the low birth weight newborn. Indian J Community Medicine: Official Publication Indian Association Prev Social Med. 2014;39(4):245–9.
Heidarzadeh M, Hosseini MB, Ershadmanesh M, Gholamitabar Tabari M, Khazaee S. The Effect of Kangaroo Mother Care (KMC) on breast feeding at the time of NICU Discharge. Iran Red Crescent Med J. 2013;15(4):302–6.
Lamy Filho F, Silva AAMd, Lamy ZC, Gomes MASM, Moreira MEL. Evaluation of the neonatal outcomes of the kangaroo mother method in Brazil. Jornal De Pediatria. 2008;84:428–35.
Feldman R, Rosenthal Z, Eidelman AI. Maternal-preterm skin-to-skin contact enhances child physiologic organization and cognitive control across the first 10 years of life. Biol Psychiatry. 2014;75(1):56–64.
Cristóbal Cañadas D, Parrón Carreño T. Benefits of Kangaroo Mother Care on the Physiological Stress Parameters of Preterm Infants and mothers in neonatal intensive care. 2022, 19(12).
Natchu UCM, Liu E, Duggan C, Msamanga G, Peterson K, Aboud S, Spiegelman D, Fawzi WW. Exclusive breastfeeding reduces risk of mortality in infants up to 6 mo of age born to HIV-positive Tanzanian women. Am J Clin Nutr. 2012;96(5):1071–8.
Edmond KM, Kirkwood BR, Amenga-Etego S, Owusu-Agyei S, Hurt LS. Effect of early infant feeding practices on infection-specific neonatal mortality: an investigation of the causal links with observational data from rural Ghana. Am J Clin Nutr. 2007;86(4):1126–31.
Phukan D, Ranjan M, Dwivedi LK. Impact of timing of breastfeeding initiation on neonatal mortality in India. Int Breastfeed J. 2018;13(1):27.
Sankar MJ, Sinha B, Chowdhury R, Bhandari N, Taneja S, Martines J, Bahl R. Optimal breastfeeding practices and infant and child mortality: a systematic review and meta-analysis. Acta Paediatr. 2015;104:3–13.
Hossain S, Mihrshahi S. Exclusive breastfeeding and childhood morbidity: a narrative review. Int J Environ Res Public Health. 2022;19(22):14804.
Ip S, Chung M, Raman G, Chew P, Magula N, DeVine D, Trikalinos T, Lau J. Breastfeeding and maternal and infant health outcomes in developed countries. Evid report/technology Assess. 2007;153:1–186.
Dilla E, Dessie E. Determinants of mortality among Preterm neonates admitted with respiratory distress in Addis Ababa Public Hospitals Neonatal Intensive Care Units, 2021, Multi-Center Prospective Follow-Up Study.
Backes CH, Markham K, Moorehead P, Cordero L, Nankervis CA, Giannone PJ. Maternal preeclampsia and neonatal outcomes. Journal of pregnancy 2011, 2011.
Acknowledgements
We would like to thank Wachemo University for giving us the opportunity to conduct this study.
Funding
no funding.
Author information
Authors and Affiliations
Contributions
L.L. conceived the study and prepared the first draft of the manuscript. L.L., A.S., D.E., S.A., A.H., L.M., E.M., and M.G. did data acquisition, statistical analysis, manuscript editing, and manuscript review.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
We will obtain ethical approval was obtained from the Institutional Review Board (IRB) of Wachemo University. Research Ethics Review Committee of WCU. A letter of permission was obtained from the clinical Director of NEMMCSH. Detailed informed consent (with a summary of the study and benefits of the study in the local language) was obtained from caregivers of preterm neonates. All information collected from patient was kept strictly confidential, and the names of patients were not included in the checklist. All methods were performed following the relevant guidelines and regulations and complied with the Declaration of Helsinki.
Consent for publication
N/A.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Tirore, L.L., Erkalo, D., Abose, S. et al. Incidence of mortality and its predictors among preterm neonates in nigist eleni mohammed memmorial comprehensive specialized hospital, Hossana, Ethiopia: a prospective follow-up study. BMC Pediatr 24, 511 (2024). https://doi.org/10.1186/s12887-024-04992-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-024-04992-9