Abstract
Background
The clinical characteristics of pediatric critically ill patients who need referral to a tertiary hospital is often unknown in resource limited settings where constraints in diagnosis capacity, resources, and infrastructures are common. There is a need to increase insight in the characteristics of these patients for capacity building strengthening and appropriate resource allocation. The aim of this study was to describe the clinical characteristics and outcomes of critically ill children who are referred to a tertiary referral teaching hospital in Yogyakarta.
Methods
A prospective observasional study was carried out from July 1st, 2022 -January 31st, 2023 which included all critically ill pediatric patients who were referred through the Integrated Referral System (SISRUTE) to the Pediatric Intensive Care Unit (PICU) of dr. Sardjito hospital. We excluded patients who were referred with a request for admission to the PICU, but were not admitted to the PICU due to their stable condition and lack of the need for intensive care.
Result
During the study period, we received 1046 emergency referral requests for pediatric patients via SISRUTE, of those, 562 (53.7%) patients were critically ill. The reasons of PICU referral request were the need of solely intensive care 504 (89.7%), the need of multidisciplinary team care, including intensive care 57 (10.1%) and parents request 1 (0.3%). The pre-referral emergency diagnosis was shock 226 (40.3%), respiratory distress/failure 151 (26.7%), central nervous system (CNS) dysfunction 135 (24.1%), trauma 33 (5.9%) and sepsis 17 (3%). Of the 562 critically ill PICU referral requests, 473 (84.2%) requests were accepted. One hundred and eighty-one (58.7%) patients were finally admitted to the PICU, 125 (40.3%) admitted to our regular ward due to stable condition, 4 (1.3%) patients died in Emergency Departement (ED). The remaining accepted patients on request did not arrive in our facility due to various reasons. The mean (SD) response time was 9.1 (27.6) minutes. The mean (SD) transfer time was 6.45 (4.73) hours. Mean (SD) PICU and hospital length of stay was 6.7 (8.3) days and 10.2 (9.2) days respectively. PICU and hospital mortality was 24.3% and 29.7%, respectively.
Conclusion
The mortality rate for critically ill pediatric patients referred to a tertiary PICU still high, with shock being the most common pre-referral emergency diagnosis. There is a discrepancy between the referring hospital’s and the referral hospital’s indication for PICU admission. The time required to reach the referral hospital is quite lengthy.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Introduction
The under-5 mortality rate has - with approximately 24 per 1000 live births- [1, 2] decreased in Indonesia during the last decades, yet it is still far from the set targets [1]. As a low- and middle-income country (LMIC) Indonesia faces many challenges in the healthcare field particularly in addressing childhood mortality. Understaffing, inadequate funding, scarcity of healthcare expertise, insufficient resources, deficient training and education were identified as contributors to the high mortality rates among children in LMICs [3,4,5,6].
One of the main elements of primary health care is the referral system, which allows patients to obtain services at health centers with superior facilities and infrastructure [7]. The necessity of an efficient referral system for critically ill children is a determinant in child survival that is less acknowledged and understood [8,9,10,11]. Lack of pre-referral communication, burden at the referred facility (staff and infrastructure), poor transport systems contributes to an imbalance in supply and demand [8, 12].
Indonesia still face the challenge of inadequate establishment of well-organized referral systems to address the needs of critically ill children. Our country has the Integrated Referral System (SISRUTE) as a means of communication between pre-referral and referral health services. SISRUTE is an Information and Technology (IT)-based integrated health service delivery information system that is launched for improving the performance of health care facilities and for accelerating the referral process according to the patient’s medical needs and the competences necessary. SISRUTE makes use of several communication channels, including Short Message Service (SMS), Android applications, and web-based platforms. This enables prompt information exchange between pre-referral hospitals and referred health care institutions, with the goal to improve patient safety and family/patient satisfaction [13].
In our setting the attending doctors or nurses can send a referral request to multiple referral hospitals at their choice via SISRUTE website https://sisrute.kemkes.go.id. The choice of a referral hospital typically depends on the necessary medical resources, the distance from the referring hospital, and occasionally the preferences of the patient’s family. At specific referral hospitals, particularly tertiary referral hospitals, there are senior ED Nurses who have been assigned as Pre hospital Emergency Communication Centre (PECC) officers. These officers are responsible for regularly monitoring incoming referral request via SISRUTE. However, the majority of referring hospitals lack personnel of this nature, resulting of communication which is not always in real time. Phone communication is consistently available for submitting emergency referral requests to our hospital, which will be received by the PECC officers. At currently, SISRUTE does not have a specialized section to accommodate referring patients with critically ill condition, who necessitate prompt responses and decisions.
In term of transport system, we do not have a dedicated transport team for critically ill patients. The patients were stabilized and transported by the attending physician, who was primarily a general practitioner, and a nurse from the referring hospital, use their ambulance. In smaller healthcare facilities, the presence of ambulances may be restricted, leading to potential delays in the patient referral process. Limited data is available regarding the clinical profile and outcome of pediatric critically ill referral cases in Indonesia. We conducted this study to explore clinical, referral characteristics and outcome of pediatric critically ill referral cases to tertiary referral teaching hospital in Yogyakarta, Indonesia.
Methods
Study design and setting
A prospective observational study was conducted in the Emergency Department (ED) at Dr. Sardjito hospital, Yogyakarta. Dr Sardjito hospital is a tertiary public university-based hospital in Yogyakarta Province, Indonesia which serves approximately 4000 pediatric inpatients per year and provides ED services to an average of 2000 pediatric patients per year. The Pediatric Intensive Care Unit (PICU) is equipped with 16 medical and surgical intensive care unit beds and has approximately 900 admissions per year. Our team consists of three pediatric intensivists who manage patients in PICU. Additionally, we have general practitioners who have received specialized training in pediatrics and work in rotating shifts. The PICU at our facility adopts a semi-closed system.
Patients and operational definition
We included all emergency referral that have requested admission to our PICU in patient aged 1 month to 18-year-old via SISRUTE from July 1st 2022 – January 31st 2023. Patients who were admitted to PICU were prospectively followed up until the discharged or the day they deceased. We define SISRUTE’s response time as the time between the referral request sent via SISRUTE by the referring hospital and the initial response from our hospital as the referral hospital. We defined the transfer time as the duration between the initial response and the arrival of the patient at our ED. We defined PICU mortality as the occurrence of patient deaths during the course of care within PICU. We defined hospital mortality as the occurrence of patient deaths during the course of care within hospital. We define early mortality as mortality that occurred ≤ 48 h after PICU admission. The Indonesian Ministry of Health current regulations adhere to the Pediatric Assessment Triangle (PAT) method of identifying and categorizing emergency diagnosis in pediatric patients. This method has been adapted for use in Indonesia, and has been widely disseminated and incorporated into medical education programs [14]. Our PICU admission standards adhere to the guidelines issued by the American Academy of Pediatrics in 2019, with necessary adjustments made to suit specific conditions in Indonesia as per the guidelines set by the Ministry of Health [15].
Data collection tool, procedure and data quality assurance
Data collection was conducted using a structured case record form, administered by pediatric residents overseeing the ED. The initial data collection commenced immediately upon contact from the pre-referral hospital. Information gathered for referral cases including age, sex, required type of care, province of referral origin, reasons for patient referral, emergency diagnosis at the referring hospital, referral acceptance status, reasons for declining referral, and the final condition post referral request acceptance including the emergency diagnosis at OUR ED.
After admission to PICU at dr Sardjito hospital, we recorded patient demographic data, SISRUTE’s response time, transfer time, length of stay (LOS) at the PICU, overall LOS in our hospital, mortality, and early mortality. We also collected data on PELOD-2 [16] scores within the first 24 h of patients being admitted to the PICU.
Data analysis
The results are presented in a descriptive manner, utilizing absolute numbers, percentages, medians, and interquartile ranges as suitable for the data. Data analysis was performed using Excel version 16.16.21 (Microsoft). We used the t-test for normally distributed continuous variables and the Mann-Whitney U-test for non-normally distributed continuous variables to determine differences between two populations.
We calculated the cut-off point of the PELOD 2-score in the population using the Youden’s J index. Youden’s J is the likelihood of a positive test result in subjects with the condition versus those without the condition. It is also the probability of an informed decision (as opposed to a random guess). Youden’s J index combines sensitivity and specificity into a single measure (Sensitivity + Specificity − 1) and has a value between 0 and 1. In a perfect test, Youden’s index equals 1. It is also equivalent to the vertical distance above the diagonal no discrimination (chance) line to the ROC curve for a single decision threshold [17].
Ethical consideration
Ethic approval was obtained from the Medical and Health Research Ethic Committee (MHREC) with the Ref No: KE/FK/0907/EC/2022. Confidentiality and privacy were strictly maintained. Only the principal investigator and the research assistants can access the data. All methods throughout the study were performed in accordance with the relevant guidelines and regulations.
Results
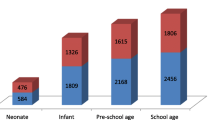
Between July 1st 2022 – January 31st 2023, dr Sardjito hospital’s ED received 1108 pediatric and neonatal referral requests, of which 1046 were sent via SISRUTE. The 62 emergencies pediatric patient referral requests that were done directly via telephone due to errors in SISRUTE and also errors in internet connection in referring hospital are not included in the analysis. In total 562 of the 1046 SISRUTE referral requests (52.8%) were requests for PICU care, 217 (20.4%) were neonatal cases, and 267 (25.1%) were regular ward care cases. Of the 562 PICU care requests, 473 (84.2%) were accepted and 89 (15.8%) were refused predominantly due to unavailability of PICU beds (Fig. 1). Due to logistical constraints we were unable to analyze the outcome of these 89 patients. The referral origin provinces predominantly were from Yogyakarta 254 (45.2%) and Central Java 208 (37.0%) (Table 1). One case of critically ill referral request came from another island (Riau province in north Sumatra).
Of the 473 referral requests that initially were accepted as PICU cases, 163 patients were not transferred due to these reasons: 59 (36.2%) patients never arrived in our hospital without further information; 11 (6.8%) patients improved and their referral was cancelled; 23 (14.1%) patients died before transport; 60 (36.8%) patients were accepted to another (lower level) hospital; and the parents of 10 patients (6.1%) refused the transfer.
Of the remaining 310 patients who actually arrived at our ED, 125 (40.3%) were not critically ill and were then admitted to the regular ward. The remaining 185 (59.7%) patients were triaged as having indications for admission to the PICU. Of these, 4 (2.2%) patients died in the ED and 181 (97.8%) patients were finally admitted to the PICU.
The most common pre-referral emergency diagnosis based on PAT method was shock 226 (40.3%). The other pre-referral diagnosis was respiratory distress/failure 151 (26.7%), central nervous system (CNS) dysfunction 135 (24.1%), trauma 33 (5.9%) and sepsis 17 (3%) (Table 1). The most common diagnoses in our ED also based on PAT method were cardiorespiratory failure in 57 (30.8%) patients, respiratory distress in 43 (23.2%) patients, shock in 35 (18.9%) patients, respiratory failure in 28 (15.1%) patients and CNS dysfunction in 22 (11.9%) patients (Table 2).
The overall hospital mortality rate was 29.7%, of whom 32.7%. suffered from early mortality, while PICU Mortality was 24.3%. Overall mean (± SD) response time mean was 9.1 (± 27.6 ) minutes and overall mean (± SD) transfer time mean was 6.45 (± 4.73 h ) (Table 2). Both response time and transfer time were not associated with mortality rate. (Table 3). In Figs. 2 and 3, scatter plots illustrate the response time and transfer time for both deceased and survive groups.
We were able to calculate the PELOD 2-score for 177 patients admitted to PICU. The mean (± SD) PELOD 2- score was 7.7(± 5.1) for the group of patients who died, and 3.0 (± 2.9) for the group who survived. This mean difference is statistically significant with P < 0.0001. In this study, The PELOD 2_Score cut-off result was 5, with a sensitivity of 65.5% and a specificity of 85.35% (Fig. 4).
By obtaining this cut off point value, we divided the subjects based on their PELOD 2-score ≤ 5 and PELOD 2 –score > 5 and analyzed it with Kaplan Meier curve (Fig. 5). The curve reveals that patients with a PELOD 2-Score of ≤ 5 demonstrate higher survival compared to those with a PELOD 2-Score > 5.
Discussion
We found that only 59.7% of all patient with critically ill referral cases who arrived in our hospital had a true indication for PICU admission. This means that over 40% of the patients were in a stable condition and thus considered appropriate for hospitalization in the general ward. This could either be caused by the effectiveness of the initial treatment administered at the referring hospital, or it suggests discrepancies in the assessment of PICU admission indication in pediatric patients between the referring hospital and the referral hospital. Yet, this also contributed a burden of the PICU limited capacity since a PICU bed was unjustified reserved for a substantial number of patients. Multiple studies have identified strategies to address this discrepancies, including enhancing inter-hospital communication through direct interaction with the PICU personnel, enhancing referral documentation, and developing transport system involving the transport team from the referral hospital [18,19,20,21].
On the other hand, mortality of the transferred patients was almost 30% (of who more than one-third diedwithin the first 48 h), which is substantial higher than the overall mortality rate of 23.5% in our unit. The death rates reported in the literature is lower than we found in our study and range from 3.9 to 17% [18,19,20, 22]. Yet, this is influenced by a variety of factors, including demographic and socioeconomic characteristics, disease-related factors, health system-based factors, as well as factors related to pre-referral management, referral processes, and transportation [9, 23,24,25]. A study conducted by Shinozaki et al., (2021) in Los Angeles, USA, examined the impact of transport time on the mortality rate and length of stay for critically ill pediatric patients undergoing inter-facility transport [18]. The findings of this study indicated that there was no significant association between the duration of transport time and these outcomes. Other study done by Seaton et al., (2020) in United Kingdom found transport time to PICU of referral hospital may be associated with a small reduction in PICU length of stay [20]. Both studies were conducted within the setting of developed countries, where the availability of transport teams for critical ill children was present.
Taken together, our findings imply that there is room for improvement of the initial treatment and stabilization of the patients in the referring hospitals as well as improvement of the transportation system. Indeed in many studies it has been reported that the lack of organized emergency and intensive care services and expertise in the peripheral hospitals, causes referral hospitals to bear large numbers of referrals and admissions particularly those with unfavorable outcomes [8, 9, 26].
In our study, we observed disparities in PICU admission indication between the referring hospital and the referral hospital, particularly with the favorable patient state upon arrival at our ED. The most common diagnosis to refer patients to PICU was shock, respiratory distress/failure, or CNS dysfunction. In line with aforementioned discrepancies a disparity exists between the emergency diagnosis rendered by the referring hospital and the emergency diagnostic rendered at the referral hospital.
There are several possible options for addressing these problems include enhancing transportation infrastructure, providing comprehensive training for doctors in peripheral hospitals, establishing standardized protocols for pediatric emergency assessments, and implementing telemedicine consultations [27,28,29,30]. These opportunities have the potential to contribute to the improvement of the overall referral process for critically ill children. More studies must be done to investigate those problems for the purpose to improve the overall effectiveness of the referral system for pediatric critical ill patients. It is expected that improving the referral system for critically ill children will contribute to a reduction in child mortality in our setting.
With the objective to capture the clinical profile and outcome of critically ill children referred to a tertiary hospital our study has several limitations. This study had been done in only one tertiary referral hospital in Indonesia and in a short time period, there may be difference characteristics found in other referral hospitals with longer study duration. Additionally, the findings may not fully represent different healthcare settings or regions, and establishing causality remains challenging. We also lacked sufficient data on the therapy conducted before referral and the specific stabilization efforts implemented.
However, this is among the first studies to investigate the referral system of critically ill child in Indonesia. Further investigation is necessary to examine the concerns surrounding the referral system in critically ill children, particularly for determining the reasons for delayed response and transfer time, with the goal of improving patient survival.
Conclusion
Shock is the most common pre-referral emergency diagnosis. High mortality rates, discrepancy in PICU admission indication and a long referral process are the problems surrounding pediatric critical ill referral case that we encounter in our setting.
Data availability
All data generated or analyzed during this study are included in the submission. The raw data are available from the corresponding author on reasonable request.
Abbreviations
- PICU:
-
Pediatric intensive care unit
- PELOD:
-
Pediatric Logistic Organ Dysfunction
- HR:
-
Hazard ratio
References
Rachmawati PD, Kurnia ID, Asih MN, Kurniawati TW, Krisnana I, Arief YS, et al. Determinants of under-five mortality in Indonesia: a nationwide study. J Pediatr Nurs. 2022;65:e43–8.
Ministry of Health of the Republic of Indonesia. Indonesia Health Profile 2020. Ministry of Health of the Republic of Indonesia; 2021.
Rudd KE, Kissoon N, Limmathurotsakul Di, Bory S, Mutahunga B, Seymour CW, et al. The global burden of sepsis: barriers and potential solutions. Crit Care. 2018;22(1):123305059.
Harahap NC, Handayani PW, Hidayanto AN. Barriers and technologies of maternal and neonatal referral system in developing countries: a narrative review. Inf Med Unlocked. 2019;15(April).
Kitila SB, Tesema AA, Bekele G, Olika AK, Biratu Terfa Y, Ololo Sinkie S, et al. Average time spent in referral process and its Determinants among Clients of Maternal and Child Health Service in 2 districts of Jimma Zone, Ethiopia. J Patient Experience. 2022;9:1–7.
Japiong KB, Asiamah G, Owusu-Dabo E, Donkor P, Stewart B, Ebel BE, et al. Availability of resources for emergency care at a second-level hospital in Ghana: a mixed methods assessment. Afr J Emerg Med. 2016;6(1):30–7.
Seyed-Nezhad M, Ahmadi B, Akbari-Sari A. Factors affecting the successful implementation of the referral system: A scoping review. J Family Med Prim Care [Internet]. 2021;10(12):4364. http://www.jfmpc.com/article.asp?issn=2249-4863;year=2017;volume=6;issue=1;spage=169;epage=170;aulast=Faizi.
Ezhumalai G, Jayashree M, Nallasamy K, Bansal A, Bharti B. Referrals to a pediatric emergency department of a tertiary care teaching hospital before and after introduction of a referral education module - A quality improvement study. BMC Health Serv Res. 2020;20(1):1–7.
Praveen K, Nallasamy K, Jayashree M, Kumar P. Brought in dead cases to a tertiary referral paediatric emergency department in India: a prospective qualitative study. BMJ Paediatrics Open. 2020;4(1):1–8.
Gilpin D, Hancock S. Referral and transfer of the critically ill child. BJA Educ. 2016;16(8):253–7.
Newbrander W, Ickx P, Werner R, Mujadidi F. Compliance with referral of sick children: a survey in five districts of Afghanistan. BMC Pediatr. 2012;12.
Power N, Plummer NR, Baldwin J, James FR, Laha S. Intensive care decision-making: identifying the challenges and generating solutions to improve inter-specialty referrals to critical care. J Intensive Care Soc. 2018;19(4):287–98.
Directorate of Referral Health Services. Government Agency Performance Accountability Report. 2020.
Horeczko T, Enriquez B, McGrath NE, Gausche-Hill M, Lewis RJ. The Pediatric Assessment Triangle: Accuracy of its application by nurses in the triage of children. J Emerg Nurs. 2013;39(2):182–9.
Hsu BS, Hill V, Frankel LR, Yeh TS, Simone S, Arca MJ et al. Executive summary: Criteria for critical care of infants and children: PICU admission, discharge, and triage practice statement and levels of care guidance. Pediatrics. 2019;144(4).
Stéphane Leteurtre A, Duhamel J, SaUeron B, Grandbastien JL, Leclerc F. Physical therapy for the critically ill in the ICU: a systematic review and meta-analysis. Crit Care Med. 2013;41(6):1543–54.
Ruopp MD, Perkins NJ, Whitcomb BW, Schisterman EF. Youden Index and Optimal Cut-Point estimated from observations affected by a lower limit of detection. Biom J. 2008;50(3):419–30.
Shinozaki RM, Schwingshackl A, Srivastava N, Grogan T, Kelly RB. Pediatric interfacility transport effects on mortality and length of stay. World J Pediatr. 2021;17(4):400–8.
Hatherill M, Waggie Z, Reynolds L, Argent A. Transport of critically ill children in a resource-limited setting. Intensive Care Med. 2003;29(9):1547–54.
Seaton SE, Ramnarayan P, Davies P, Hudson E, Morris S, Pagel C, et al. Does time taken by paediatric critical care transport teams to reach the bedside of critically ill children affect survival? A retrospective cohort study from England and Wales. BMC Pediatr. 2020;20(1):1–11.
Khilnani P, Chhabra R. Transport of critically ill children: how to utilize resources in the developing world. Indian J Pediatr. 2008;75(6):591–8.
Saz EU, Turan C, Anıl M, Bal A, Gökalp G, Yılmaz HL, et al. Characteristics and outcomes of critically ill children transported by ambulance in a Turkish prehospital system: a multicenter prospective cohort study. Turk J Pediatr. 2021;63(1):59–67.
Manongi R, Mtei F, Mtove G, Nadjm B, Muro F, Alegana V, et al. Inpatient child mortality by travel time to hospital in a rural area of Tanzania. Trop Med Int Health. 2014;19(5):555–62.
Beyene H, Hailu D, Tadele H, Persson LÅ, Berhanu D. Insufficient referral practices of sick children in Ethiopia shown in a cross-sectional survey. Acta Paediatr Int J Paediatrics. 2020;109(9):1867–74.
Jofiro G, Jemal K, Beza L, Bacha Heye T. Prevalence and associated factors of pediatric emergency mortality at Tikur Anbessa specialized tertiary hospital: a 5 year retrospective case review study. BMC Pediatr. 2018;18(1):1–10.
Lahmini W, Bourrous M. Mortality at the pediatric emergency unit of the Mohammed VI teaching hospital of Marrakech. BMC Emerg Med. 2020;20(1):4–9.
Smith G. Pre-hospital factors that lead to increased mortality and morbidity in trauma patients in developing countires: a systematic review. University of Arizona College of Medicine. University of Arizona College of Medicine; 2019.
Sharifi Kia A, Rafizadeh M, Shahmoradi L. Telemedicine in the emergency department: an overview of systematic reviews. J Public Health (Germany). 2023;31(8):1193–207.
Conlon C, Nicholson E, Rodríguez-Martin B, O’Donovan R, De Brún A, McDonnell T, et al. Factors influencing general practitioners decisions to refer paediatric patients to the emergency department: a systematic review and narrative synthesis. BMC Fam Pract. 2020;21(1):1–11.
Hu Y, Zheng B, Zhu L, Tang S, Lu Q, Song Q, et al. The effectiveness of emergency knowledge training of pediatric medical workers based on the knowledge, skills, simulation model: a quasi-experimental study. BMC Med Educ. 2022;22(1):1–11.
Acknowledgements
We thank all those who provided excellent technical support and assistance during the study.
Funding
The authors did not receive funding for this study.
Author information
Authors and Affiliations
Contributions
DR and JBMVW contributed to the completion of interpretation of the data and the manuscript. DR and JBMVW contributed substantially to the concept, design, interpretation of the data, and completion of the study and manuscript. VO, AHP, FM contributed to critical revision of the manuscript for important intellectual content. All authors had access to all the data in the study and had final responsibility for the decision to submit for publication. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Medical and Health Research Ethics Committee of the Faculty of Medicine, Universitas Gadjah Mada (KE/FK/0907/EC/2022).
Consent to publish
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Rusmawatiningtyas, D., Oktaria, V., Pudjiadi, A.H. et al. Clinical characteristics and outcome of critically ill children referred to a tertiary hospital in Indonesia: a prospective observational study. BMC Pediatr 24, 478 (2024). https://doi.org/10.1186/s12887-024-04940-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-024-04940-7