Abstract
Introduction
: Mothers/caregivers should be aware of a newborn’s danger signs and promptly seek medical attention. Hence, this study assessed mothers’/caregivers’ awareness, healthcare seeking behaviors for neonatal danger signs and their determinants in the developing regional state of Ethiopia.
Methods
A community-based cross-sectional study was employed among mothers/caregivers of neonates in the developing regional state of Ethiopia. The sample was determined in collaboration with the Central Statistics Agency of Ethiopia. Stratified multi-stage cluster sampling was used to recruit the sample. Data were collected through an interviewer administered structured questionnaire using a tablet computer. Descriptive statistics and binary logistic regression were applied to identify determinants of awareness and treatment-seeking behavior for neonatal danger signs.
Results
The result of the study showed that nearly one-third (32.7%) of the respondents had a good level of awareness of neonatal danger signs, and 69.0% of the respondents had good healthcare-seeking practice about neonatal danger signs. Regional state (Benishangul-Gumuz) [AOR = 1.61; 95% CI (1.09, 2.39)], Muslim’s [AOR = 1.75; 95% CI (1.20, 2.55)] and permission to travel to a health facility [AOR = 0.48; 95% CI (0.37, 0.63)] were determinants of mothers’/caregivers’ awareness about neonatal danger signs. Antenatal care (ANC) attendance and institutional delivery were shown to have a positive association with neonatal healthcare seeking (AOR = 2.14 and AOR = 2.37, respectively).
Conclusion
In Ethiopia’s developing regional states, mothers/caregivers were remarkably unaware of neonatal danger signs. Region, religion, mothers’/caregivers’ age, and need for permission to travel to a health facility were predictor variables for neonatal danger sign awareness. Better healthcare seeking practices, which are determined by ANC attendance and institutional delivery, are observed in these regions. Federal and regional governments should give these regions due attention. Moreover, regional health bureaus and health professionals should tackle the problem by focusing on the identified factors.
Similar content being viewed by others
Introduction
The first 28 days after birth are the most critical time of human life. Annually, 2.6 million infants die before reaching 1 month across the globe [1]. On this basis, the World Health Organization considers efforts to address inequities as key components of global efforts aimed at improving newborn and child health and survival rates [2]. According to the United Nations Inter-Agency Group for Child Mortality Estimation 2020 report, the death proportion of neonates globally on average is 17 deaths per 1,000 live births in 2019, and it has dropped by 52% from 38 deaths per 1,000 in 1990 [3]. In addition, the report reveals that over 6,700 children pass away every day and that almost 2.4 million children die in their first month of existence [4]. About 75% of newborn deaths in 2019 happened within the first week following birth, and 33.33% happened within the first day[5].
In industrialized countries, there are less than eight child deaths per 1,000 live births, compared to 76 per 1,000 in sub-Saharan Africa [6, 7]. Research demonstrates that women’s decision-making autonomy is low, particularly in developing nations. Yet, increasing women’s influence in decision-making results in better healthcare access, poverty reduction, and household economic growth. In fact, women are largely viewed as the primary caregivers in low-income nations [8,9,10]. Although most neonatal deaths occur at home, few families seek medical attention for symptoms of neonatal sickness, and almost no neonates are brought to medical facilities when they are ill. Delayed healthcare seeking significantly increases neonatal mortality [11].
Healthcare services for mothers and children are a crucial determinant of their health outcomes [12]. Recent initiatives in Ethiopia to enhance newborn health outcomes have had positive effects. Newborn and infant mortality have steadily decreased as a result of other strategic efforts and the country’s health sector transformation plan being implemented. Ethiopia has decreased neonatal mortality from 39 to 30 deaths per 1,000 live births and infant mortality from 77 to 43 per 1,000 live births between 2005 and 2019. The most critical period for a child’s survival is, most importantly, the first 28 days of life [13]. Notwithstanding this outstanding accomplishment, Ethiopia still has 191,000 under-five fatalities annually [14]. Pneumonia (17%), diarrhea (8%), and newborn causes (47%) account for the majority of these fatalities, with malnutrition serving as a significant underlying risk [15].
Mothers´ and husbands´ higher educational achievement, living close to health facilities, previous experience of neonatal danger signs, ANC and PNC attendance, and access to television for information were positively associated with mothers´ good knowledge about neonatal danger signs [16, 17].
Caretakers in Ethiopia failed to seek medical attention when neonatal danger signs were present, which led to an increase in neonatal deaths at home [11]. The socioeconomic, emotional, fertility decisions, contraceptive usage, and sexual lifespan of women are impacted by poor participation in decision-making processes and limited access to health services, which leads to a demographic problem [18]. Utilization rates for health care services can be influenced by knowledge of disease origins, symptoms, and treatments, trust in providers. These factors can impact neonatal health. Lack of knowledge, perceived low-quality medical care, and parents’ inadequate education may cause parents to misjudge the effectiveness of care and lose faith in the medical system, which may drive them to turn to traditional healers [19, 20]. . Access to health services, such as availability of services, geographic accessibility, travel time, and affordability determine child health inequity. These factors mostly favour those who live closer to health facilities, and those who can afford both the direct and indirect costs of the service as well as the opportunity costs associated with receiving the service [21].
Identifying early maternal health care-seeking habits and understanding the characteristics associated with health care-seeking behavior for neonatal danger signals is crucial for nations such as Ethiopia, especially developing regional states. However, compared to the national average, developing regional states in Ethiopia (Afar, Benishangul-Gumuz, Gambella, and Somali) have demonstrated less improvement in critical health outcomes. Health activities, particularly health extension projects, were limited by distance, geography, topography, weather conditions, and security concerns in some regions and were not tailored to the unique settings of pastoralist communities. In Ethiopia’s developing regional states, there is still a great deal of work to be done to reduce morbidity and mortality rates, encourage newborn health care seeking, and foster a supportive attitude towards the diagnosis, treatment, and prevention of neonatal disorders. Thus, the goal of this study is to evaluate the factors that influence newborn healthcare seeking behavior in four of Ethiopia’s growing regional states.
Methods
Study setting and design
The study was conducted in the four developing regional states of Ethiopia, namely Gambela, Afar, Benshagu-Gumuz, and Somali. Regions with less developed infrastructure, sluggish growth in many sectors, and border disputes further complicate development. A community-based cross-sectional study design was conducted among 6,706 mothers and primary caregivers of children aged below five years in February 2021.
The study participants included mother-child pairs or primary caregivers of children aged 15 years and older.
Sample and sampling techniques
The sample was determined in collaboration with the Central Statistics Agency (CSA) of Ethiopia. To get an adequate sample, the necessary statistical power for analysis was considered, including a sub-sample of refugees living in camps or refugee settlements in each Developing Regional State (DRS). The assumptions used to determine the sample were: women’s awareness of neonatal danger to be 40.7% in Ethiopia [22], a 95% confidence level, a design effect of 3, a 5% non-response rate, which yielded a total sample size of 3246.
A stratified multi-stage cluster sampling design was applied with a target sample size from which 3,104 mother/caregivers fully responded to the survey and were aged 15 years and over. To recruit the study subjects, the sample was drawn by simple random sampling from the sampling frame of enumeration areas (EAs) prepared by the CSA in 2018–2019 for the upcoming Ethiopian population census. For the refugee sample, the CSA performed a simple random selection of camps/settlements from those located in each DRS. Unlike the general population, the CSA could not provide a frame for refugee households. As a result, 600 refugee samples were selected through a random route approach with a fixed selection interval of 5 households. Similar proportions of samples were recruited in each refugee camp in each developing regional state.
Data collection method and tool
The data were collected using a structured questionnaire administered by a professional interviewer using a tablet. Prior to the start of fieldwork, six days of training, including two days of field practice with the questionnaire were given to the data collectors. To identify the variable predictors of child healthcare service utilization, a socio-ecological model was used. Healthcare service variables like postnatal care, early healthcare seeking for neonatal danger signs, vaccination, knowledge, and response to common childhood illness danger were accordingly assessed for the sub-group targets (0–11 months, 12–23 months, and 24–59 months).
Operational definition
Symptoms that indicate a newborn baby should be taken to a health facility immediately were used to measure mothers’/caregivers’ awareness of neonatal danger signs; health seeking behavior of the mothers and caregivers was assessed whether they sought treatment for their baby when they faced the neonatal danger signs.
Data quality management and analysis
Data were entered in the field using Open Data Kit (ODK) data collection software while collecting the data, and they were exported to Excel then exported to SPSS version 26 for analysis. Data were cleaned, and descriptive statistics like frequencies, percentages, and proportion were done for the categorical variables. The mean and standard deviation were calculated for the continuous variable. The final model was developed using bivariate logistic regression at a p-value of 0.2. These variables were fitted to multivariable logistic regression to identify predictor variables for child healthcare service utilization. A P-value of 0.05 was used to declare an association between the explanatory and dependent variables as a cutoff point. For each sub-group of the study participants, independent analysis was done.
Because of the unavailability of a sampling frame for refugees, the refugee sample is unweighted. Refugee statistics are not included in the weighted total for the DRS. Consequently, the refugee statistics are shown in a column separated from the main, and only aggregated statistics are presented for the refugee population because the sample of refugees is too small for regional disaggregation.
Result
Awareness about neonatal danger signs
From the total mothers/caregivers of neonates included in the study, nearly three-thirds of them were in the age range of 25–34 years. 78% and 60% of the mothers attended antenatal care and gave birth in a health facility, respectively (Table 1).
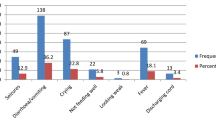
Based on 1,226 births that were delivered in the four developing regional states of Ethiopia in the year before the survey, the analysis was conducted. According to the analysis’s findings, nearly a third (32.7%) of respondents knew a good deal about neonatal warning signs. Of the refugees, 24% have good awareness about neonatal danger signs. Those participants within 25–34 years of age groups were with high proportion of awareness towards neonatal danger signs. When we see trust and frequency of information received towards neonatal danger signs, mass media and print communication materials (TV, Radio, Newspaper, SMS, Leaflet, and Poster) had a mean score of 7.63, the health workforce had a mean score of 19.50, the health institution had a mean score of 7.31, and other sources, including the community, had a mean score of 21.61. In this study, there is a 0.327 proportion with good awareness about danger signs. There are 0.061 Pseudo r-squared and Prob > chi2 is 0.000, 94.071 Chi-square and 1483.817 Akaike crit. (AIC) and Bayesian crit. (BIC) of 1555.379.
In the multivariable analysis, respondents from Benishangul Gumuz had an increased likelihood of having a good level of awareness regarding neonatal danger signs [AOR = 1.61 with 95% CI (1.09, 2.39)]. Similarly, refugees were significantly less likely to have good awareness of neonatal danger signs than non-refugees [AOR = 0.62 with a 95% CI (0.43, 0.90)]. Muslim respondents, compared to Christians, had a 75% increased likelihood of having a good awareness of neonatal danger signs [AOR = 1.75 with a 95% CI (1.20, 2.55)]. Women who required permission to travel to health facilities were significantly less likely to have a good understanding of neonatal warning signs compared with women with flexibility [AOR = 0.484, 95% CI 0.37, 0.63]. The level of trust and frequency of health information received from health institutions and the community promotes the level of awareness about neonatal danger signs. An increase in the score of trust and frequency of health information from health institutions positively increased the likelihood of awareness about neonatal danger signs (AOR = 1.01 with a p-value < 5%). Moreover, an increase in the score of trust and frequency of health information received from community sources improved the chance of having a good level of awareness about neonatal danger signs (AOR = 1.02 with a p-value < 5%) (Table 2).
Neonatal health care seeking
Regarding neonatal healthcare seeking, the analysis was based on 403 neonates that showed danger signs in the last four weeks after birth. Among these, 69.0% of the respondents had good neonatal healthcare seeking practices. Greater than 78% of the participants who gave birth at a health institution have good neonatal healthcare-seeking practice while only 54.3% of the participants who did not give birth at a health institution have good neonatal healthcare seeking practice. Regarding the proportion of neonatal health care seeking behavior by region, Gambela was the highest at 30.57% and Afar was the lowest at 16.18. In this study, 0.690 proportion of people who are aware of danger signs, there is a 0.090 pseudo-r-squared, a probability of > chi2 of 0.000, a 45.080 Chi-square, an Akaike critical of 470.027. (AIC), and a Bayesian crit. (BIC) of 502.019.
The results from the multivariable logistic regression showed that the practice of neonatal health care seeking was highly prevalent in Gambela (AOR = 2.26 with a p-value < 5%). ANC attendance and institutional delivery were shown to have a positive association with neonatal healthcare seeking, AOR = 2.14 and AOR = 2.37, respectively (Table 3).
Discussion
In the rapidly emerging regional state of Ethiopia, this research sought to assess mothers’ and primary caregivers’ awareness of neonatal danger signs and healthcare seeking behavior for neonatal sickness. The study confirmed that a third (32.7%) of mothers/caregivers had good awareness of neonatal danger signs. This study is in line with the study findings from Madagascar, where 31.2% of themothers had good knowledge of neonatal danger signs [20]. This result is significantly lower than that of a study conducted in Kigali, Rwanda, health centers, where 67% of parents knew something about neonatal danger signs [23]. Sociocultural differences and the study setting could be the reasons for the variance. Similar research from a remote Pakistani community revealed that 76% of child care providers were aware of the symptoms of diarrhea. On the other hand, just 21% of the same caregivers were aware that pneumonia might cause breathing difficulties [24]. Age difference for the concerned children, and awareness of childhood illnesses’ symptoms could be a justification for the difference. This is also lower than a study from a rural county in the southwest of China (42%) [25]. The level of development in the country could be the reason for the difference.
Furthermore, many studies from other parts of Ethiopia — 40.8% in Dire Dawa [26], 39% in Sheko District in Southwest Ethiopia [27], 48.1% in Gidan District Health Centers, North Wollo, Ethiopia [28], 40.7% in Gurage Zone, Southern Ethiopia [29] and 50.2% in Southern Ethiopia [30] —found that mothers or caregivers were more aware of neonatal danger signs. These investigations were conducted in Ethiopia’s developed regional states, where improved health information access is anticipated. Sociocultural distinctions between Ethiopia’s developed and emerging regional states may be largely responsible for the noticeable discrepancies.
Among the main sources of information for mothers and other people who care for children were health professionals, media and communication materials such as (TV, Radio, Newspaper, SMS, Leaflet, and Poster), and other sources such as community platforms. This study is supported by research done in health centers in Kigali, Rwanda, where neighbors, media outlets like TV, radio, and magazines, as well as healthcare professionals and community health extension workers, are primary sources of information for parents of children about neonatal danger signs [23]. Studies conducted in other regions of Ethiopia revealed the same results [26, 30, 31].
Mothers’ or caregivers’ awareness of neonatal danger signs is significantly influenced by factors such as region, being a refugee, religion of the respondents, permission required to travel to a health facility, and mothers’ or caregivers’ trust in and use of information from health professionals. Respondents from refugee camps, Christian religion followers, and respondents who needed permission to travel to a health facility were less likely to have good neonatal danger sign awareness. Responses from refugee camps and those who need permission to visit healthcare facilities are likely to have limited access to information. Similar to this study finding, ethnic groups in China [25] and information from healthcare facilities in Kigali, Rwanda [23] were among the factors influencing neonatal danger signs in mother or child care providers. Unfair information service dissemination among the region or ethnic group and cultural differences in information seeking among the region or ethnic group could be justified. A study from Northern Wollo Ethiopia and Southeastern Ethiopia found that health education and counseling can significantly increase awareness of neonatal danger signs among mothers and child care caregivers [28, 30].
According to the study, 69.0% of mothers and caregivers in Ethiopia’s emerging regional states sought neonatal healthcare. This result is significantly higher than the treatment-seeking behavior of mothers and other caregivers of sick children in three separate studies from Nigeria, which were 31.4%, 36%, and 18.6% [27, 32, 33]. The three studies from Nigeria examined specific pediatric diseases, and the older age of the children in those studies may have contributed to the difference. Additionally, the context of the study and cultural differences may also be factors. The appropriate healthcare seeking behavior for childhood illness among mothers in Malawi (61%) and Northern Uganda (50%) was significantly lower than this study’s findings [34, 35]. Similarly, studies on mothers or caregivers from Northwest Ethiopia [36], Woldia Town Administration, Northeast Ethiopia [30], and Efratana Gidim District, East Amhara, Ethiopia [37] had lower appropriate healthcare seeking behavior for common childhood illnesses. Experiencing older children’s illness could also delay mothers or caregivers from good or appropriate healthcare seeking.
The history of antenatal care follow-up, institutional delivery, and region of the respondents were the predictor variables for neonatal healthcare seeking. However, in most of the similar studies, these variables were not among those have an association with healthcare seeking for neonatal illness except the region, which was also a predictor variable in a study conducted in Malawi [35]. Similar to this study, the age of mothers or caregivers was not statistically associated with healthcare seeking behavior [31, 38, 39].
Conclusion and recommendation
Awareness of mothers/caregivers about neonatal danger signs was remarkably lacking in developing regional states (Gambella, Benishangul-Gumuz, Afar, Somali and refugees from these regions) of Ethiopia. Mothers in the Gambella region and refugee camps have lower neonatal danger signs awareness. Region, religion, and the request for permission to travel to a health facility continue to be the best predictor of neonatal danger sign awareness. Despite low awareness of neonatal danger signs among mothers and caregivers, better healthcare seeking practices are observed in these regions. Contrary to mothers’ awareness of neonatal danger signs, healthcare seeking practice is encouraged in Gambella. Despite the fact that better healthcare seeking is expected among mothers with better awareness of neonatal danger signs, a large proportion was observed among mothers with low awareness. The history of antenatal care follow-up, institutional delivery utilization and the region have significant roles in healthcare seeking for neonatal danger signs.
The federal government, regional state administrations, and stakeholders in these regions should give due consideration to these regions. Health extension workers and different health professionals are expected to provide information on neonatal danger signs for mothers/caregivers at any opportunity. This is to increase awareness of neonatal danger signs for better healthcare seeking practices. The identified factors should be taken into consideration at all stages of the intervention. It is recommended that researchers conduct a further study with a strong design.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ANC:
-
Antenatal Care
- AOR:
-
Adjusted Odd Ration
- CI:
-
Confidence Interval
- COR:
-
Crude Odd Ratio
- CSA:
-
Central Statistics Agency
- DRS:
-
Developing Regional States
- LL:
-
Lower Limit
- Ref.:
-
Reference group
- SPSS:
-
Statistical Package for the Social Sciences
- TV:
-
Television
- UL:
-
Upper Limit
- UNICEF:
-
United Nations International Children’s Emergency Fund
References
UNICEF. United Nations Inter-Agency Group for Child Mortality Estimation (UN IGME). Monit Situation Child Women. 2019;386:2276–86.
World Health Organization. The global strategy for women’s, children’s and adolescent’s health. WHO.2016. 108 p.
UNICEF. Levels and trends in child mortality United Nations Inter-Agency Group For Child Mortality Estimation (UN IGME). Report 2022: estimates developed by the UN Inter-agency Group for Child Mortality Estimation. New York: ONU; 2023.
Survey E.M.D.A.H., Ethiopian mini demographic health survey. 2019, Ethiopian public health institute: Addis Ababa, Ethiopia, and Rockville, Maryland UC.
UNICEF., Neonatal mortality - UNICEF DATA Monitoring the situation of children and women. 2020.
You D, Hug L, Ejdemyr S, Idele P, Hogan D, Mathers C et al. United Nations inter-agency Group for Child Mortality Estimation (UN IGME).
Global regional. National levels and trends in under-5 mortality between 1990 and 2015, with scenario-based projections to 2030: a systematic analysis by the UN Inter-agency Group for Child Mortality Estimation. Lancet. 2015;386(10010):2275–86.
Maitra P, et al. Parental bargaining, health inputs and child mortality in India. J Health Econ. 2004;23(2):259–91. Asweto C.
Maternal autonomy. distance to health care facility and ANC attendance: findings from Madiany Division of Siaya County, Kenya. American Journal of Public Health Research. 2014;2(4):153–8. Munabi-Babigumira S.
Munabi-Babigumira S, Glenton C, Lewin S, Fretheim A, Nabudere H. Factors that influence the provision of intrapartum and postnatal care by skilled birth attendants in low‐and middle‐income countries: a qualitative evidence synthesis. Cochrane Database Syst Reviews. 2017(11).
Herbert HK, Lee ACC, Chandran A, Rudan I, Baqui AH. Care seeking for neonatal illness in low- and middle-income countries: a systematic review. PLoS Med. 2012;9(3):e1001183.
Ethiopia Central Statistical Agency and ICF. Ethiopia Demographic and Health Survey 2016. Maryland, USA: Addis Ababa, Ethiopia, and Rockville; 2016.
Survey EMDAH. Ethiopian mini demographic health survey. Ethiopian public health institute: Addis Ababa, Ethiopia, and Rockville, Maryland UC and I, editor; 2019.
UNICEF Division of Policy and Strategy. Committing to Child Survival: A Promise Renewed. Progress Report 2019.
World Health Organization. The global strategy for women’s, children’s and adolescent’s health. WHO.2015.
Degefa N, Diriba K, Girma T, Kebede A, Senbeto A, Eshetu E et al. Knowledge about neonatal Danger signs and Associated Factors among mothers attending immunization clinic at Arba Minch General Hospital, Southern Ethiopia: a cross-sectional study. Hindawi BioMed Res Int. 2019;2019:9180314.].
Abu-Shaheen A, Al Fayyad I, Riaz M, Nofal A, AlMatary A, Khan A, et al. Mothers´ and Caregivers´ knowledge and experience of neonatal Danger signs: a cross-sectional survey in Saudi Arabia. Biomed Res Int. 2019;2019:1750240.
Mekonnen T, et al. Women’s empowerment as a determinant of contraceptive use in Ethiopia: further analysis of the 2011 Ethiopia Demographic and Health Survey D.F.A.R.N. 82. Maryland, USA: ICF International: Calverton; 2013.
O’Donnell O. Access to health care in developing countries: breaking down demand side barriers. Cad Saude Publica. 2007;23(12):2820–34. PMID: 18157324.
Waiswa P, Kemigisa M, Kiguli J, Naikoba S, Pariyo GW, Peterson S. Acceptability of evidence-based neonatal care practices in rural Uganda—implications for programming. BMC Pregnancy Childbirth. 2008;8(1):21.
Ekwochi U, Ndu IK, Osuorah CDI, Onah KS, Obuoha E, Odetunde OI et al. Delays in healthcare deliv- ery to sick neonates in Enugu South-East Nigeria: an analysis of causes and effects. J Public Heal (United Kingdom). 2016.
Ramamonjinirina TP, Tsifiregna RL, Rabemananjara A, Rakotondravelo SM, Rabesandratana N. Knowledge, attitudes and practices of mothers on neonatal Danger signs. Int J Pediatr Res. 2022;8:101.
Mujawimana P, Uwingabire F, Kankindi F, Dusabe R, Meharry P. Parents’ knowledge of neonatal danger signs and associated factors at health centers in Kigali, Rwanda. Rwanda J Med Health Sci. 2020;3(2):128–38.
Aftab W, Shipton L, Rabbani F, Sangrasi K, Perveen S, Zahidie A, Naeem I, Qazi S. Exploring health care seeking knowledge, perceptions and practices for childhood diarrhea and pneumonia and their context in a rural Pakistani community. BMC Health Serv Res. 2018;18(1):1–0.
Demis A, Gedefaw G, Wondmieneh A, Getie A, Alemnew B. Women’s knowledge towards neonatal danger signs and its associated factors in Ethiopia: a systematic review and meta-analysis. BMC Pediatr. 2020;20(1):1–3.
Zhou J, Hua W, Zheng Q, Cai Q, Zhang X, Jiang L. Knowledge about neonatal danger signs and associated factors among mothers of children aged 0–12 months in a rural county, Southwest of China: a cross-sectional study. BMC Pregnancy Childbirth. 2022;22(1):346.
Guta A, Sema A, Amsalu B, Sintayehu Y. Knowledge of neonatal danger signs and associated factors among mothers of < 6 months old child in dire Dawa, Ethiopia: a community based cross-sectional study. Int J Women’s Health 2020 Jul 24:539–48.
Yosef T, Nigussie T, Asefa A. Knowledge of neonatal danger signs and its associated factors among mothers attending child vaccination centers at Sheko district in Southwest Ethiopia. International journal of pediatrics. 2020;2020.
Yitayew YA, Tadele AS, Yalew ZM, Mamuye SA, Jember DA. Knowledge of neonatal danger signs and associated factors among mothers attending pediatric immunization clinics in Gidan District Health Centers, North Wollo, Ethiopia. Heliyon. 2021;7(7):e07553.
Shitu S, Abebe H, Adane D, Wassie A, Mose A, Yeshaneh A. Knowledge of neonatal danger signs and associated factors among husbands of mothers who gave birth in the last 6 months in Gurage Zone, Southern Ethiopia, 2020: a community-based cross-sectional study. BMJ open. 2021;11(8):e045930.
Getachew T, Assebe Yadeta T, Gereziher T, Eyeberu A, Dheresa M. Determinants of maternal knowledge on neonatal danger signs and care-seeking practices in a rural area of southeastern Ethiopia. Int Health. 2022;14(6):610–8.
Demelash DY, Mebratu W. Health care seeking behavior of mothers for common childhood illness and associated factors in Woldia town administration, Northeast Ethiopia. Fam Med Med Sci Res. 2020;10(1).
Abdulkadir MB, Abdulkadir ZA, Johnson WB. An analysis of national data on care-seeking behaviour by parents of children with suspected pneumonia in Nigeria. South Afr J Child Health. 2016;10(1):92–5.
Oluchi SE, Manaf RA, Ismail S, Udeani TK. Predictors of health-seeking behavior for fever cases among caregivers of under-five children in malaria-endemic area of Imo State. Nigeria Int J Environ Res Public Health. 2019;16(19):3752.
Awor P, Kimera J, Brunner NC, Athieno P, Tumukunde G, Angiro I, Signorell A, Delvento G, Lee T, Amutuhaire M, Opigo J. Care seeking and treatment of febrile children with and without danger signs of severe disease in Northern Uganda: results from three household surveys (2018–2020). Am J Trop Med Hyg. 2022;107(4):934–8.
Ng’ambi W, Mangal T, Phillips A, Colbourn T, Mfutso-Bengo J, Revill P, Hallett TB. Factors associated with healthcare seeking behaviour for children in Malawi: 2016. Tropical Med Int Health. 2020;25(12):1486–95.
Simieneh MM, Mengistu MY, Gelagay AA, Gebeyehu MT. Mothers’ health care seeking behavior and associated factors for common childhood illnesses, Northwest Ethiopia: community based cross-sectional study. BMC Health Serv Res. 2019;19:1–7.
Getahun GK, Abebil F, Mahmud S, Firdawok E. Magnitude of common childhood illness, Health Care seeking behavior, and Associated Factors in Efratana Gidim District, East Amhara, Ethiopia, 2020. Int J Nanatechnol Nanomed. 2022;7(1):100–11.
Asrat H, Gezahagn T, Kaba Z, Wondimu R, Abera T. Healthcare seeking behavior of mothers or care givers for common childhood illness of under five years children and associated factors in Kimbibit District, Ethiopia, 2020. Sci J Public Health. 2021;9(4):121.
Abegaz NT, Berhe H, Gebretekle GB. Mothers/caregivers healthcare seeking behavior towards childhood illness in selected health centers in Addis Ababa, Ethiopia: a facility-based cross-sectional study. BMC Pediatr. 2019;19(1):1–9.
Acknowledgements
We would like to thank the study participants, UNICEF and Ethiopian Health Education and Promotion Association and all other peoples who had formally or informally involved in the accomplishment of this research.
Funding
The study was supported by UNICEF Ethiopia.
Author information
Authors and Affiliations
Contributions
ND, LD, TD, TY, TG, RS, HSM, TS and HA. conceived and designed the study. TD analyzed the data and interpreted the data. ND, LD, TD and TY assisted analysis and interpretation of the data. ND and LD drafted and critically reviewed the manuscript. TD, TY, TG, RS, HSM, TS and HA critically reviewed the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical issue was approved by the ethical review board of UNICEF, Ethiopia. All administrative bodies were communicated hierarchically. Informed consent was sought from the study participants. For participants/caregivers aged 15–17, interview was made after receiving informed consent from parent or legal guardian explaining the objective of the study. The right to participate or to withdraw at any time in between of the interview was clearly explained for the participants. These all were approved by the ethical committee. Respondents’ identities were kept anonymous by using non-identifiers. Data were kept confidential and used only for research purposes.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Dida, N., Abute, L., Dejene, T. et al. Awareness and healthcare seeking behavior of neonatal danger signs, and predictor variables among mothers/caregivers in four developing regional state of Ethiopia. BMC Pediatr 24, 188 (2024). https://doi.org/10.1186/s12887-024-04656-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-024-04656-8