Abstract
Background
Japanese Kawasaki disease (KD) risk scores cannot be adopted in non-Japanese patients. In North American populations a baseline coronary artery Z-score > 2 and the Son score are associated with coronary artery aneurysms (CAAs) at 4 and 8 weeks from disease onset. In European populations, the Kawanet and Kawanet-echo scores are associated with intravenous immunoglobulin resistance. This study aims to evaluate the association between KD risk scores and baseline coronary artery Z-scores with CAAs at one, two, and six months in a European population.
Methods
Historical cohort study of all the children diagnosed with KD in a tertiary care hospital in Milan, Italy, between 1st January 2015 and 31st May 2021. Univariate and multivariate (adjusting for age and corticosteroid therapy) logistic regression analyses were used to study the association between the risk scores, a baseline Z-score ≥ 2 and ≥ 2.5 with CAAs.
Results
Eighty-nine patients were diagnosed with KD at our Centre, and 12 were excluded based on the exclusion criteria. We included 77 patients, 51 (66%) males, and 26 (34%) females, with a median age at presentation of 27 months (IQR 13–46). A baseline Z-score ≥ 2 was correlated with CAAs at one and two-month follow-ups (odds ratio (OR) 10, 95% confidence interval (CI) 2–72, and OR 18, CI 3-357) but not at six-month follow-up. The Son score showed an association with one and two-month follow-up CAAs (OR 3, CI 1.3-7, and OR 3, CI 1.3-8) but not with a six-month follow-up.
Conclusions
Patients with a baseline Z-score ≥ 2 are at higher risk for CAAs in the long term. The Son score should be tested in larger European samples. Further studies should keep the observational periods longer than 8 weeks from KD onset.
Similar content being viewed by others
Background
Kawasaki disease (KD) is an acute self-limited vasculitis affecting medium-sized arteries with a predilection for coronary arteries. In Europe, incidence rates range from 4.5 to 9 per 100 000 children under 5, who represent almost 85% of affected patients [1]. Coronary artery aneurysms (CAAs) are a long-term consequence of KD that can lead to myocardial infarction, heart failure, or death. Without treatment, almost 25% of patients develop CAAs while treatment with intravenous immunoglobulin (IVIG) reduces their incidence to 3–5% [2, 3].
In Japan in 1991, the Harada risk score [4] was developed to recognize indications for treatment with IVIG but in 2014 a retrospective study using data from Cleveland Hospital concluded that it could be used for selecting USA children at high risk for CAA development, though not sufficiently specific for select initial treatment [5]. Around 2006 and 2007, three risk scores were created to predict IVIG resistance, called Egami, Kobayashi, and Sano [6,7,8]. . However, none of the aforementioned risk scores can be adopted systematically in non-Japanese patients [9]. In North American populations, Son et all found a high predictive of a baseline coronary artery Z-score ≥ 2 for later development of CAA [10] and in 2019 retrospectively developed a risk model for CAA in KD based on demographic, laboratory, and echocardiography findings [11]. The Kawanet score was developed in France in 2020 to predict IVIG resistance in non-Asian populations [12]. In 2022, a multicentre study in Italy and France developed the Kawanet-echo score, a combination of the Kawanet score with the baseline echocardiography findings, that showed a better performance for IVIG resistance prediction than the Kawanet score and a maximal Z-score ≥ 2 [13]. Table 1 shows the scoring systems evaluated in the present study.
The present investigation aims to assess the association of all these scores and of a baseline maximal coronary artery Z-score ≥ 2 and ≥ 2.5 with CAAs at one, two, and six months from the diagnosis in an Italian tertiary care Hospital.
Materials and methods
Design, setting, and patients
We performed a historical cohort study of patients diagnosed with KD in a tertiary care Hospital (IRCCS Fondazione Ca’ Granda Ospedale Maggiore Policlinico) in Milan, Northern Italy, between 1st January 2015 and 31st May 2021. Exclusion criteria were the second episode of KD, patients not treated with IVIG or treated after 10 days from the fever onset, no echocardiography data before the IVIG infusion or within 48 h after the IVIG infusion, not echocardiography data at one month nor two-month follow-up. The Milano Area 2 Ethical Committee approved the study, which included a waiver of informed consent because of the retrospective nature of the investigation (No 2018/0802).
Treatment of the acute phase
All the patients included were treated with IVIG infusion at a dose of 2 g/Kg within 10 days from the fever onset. When the patients presented a resistant KD, defined as persistent or recrudescent fever after 36–48 h by the first IVIG infusion, a second IVIG infusion at the dose of 2 g/Kg was given as second treatment [3, 14, 15]. All the patients were treated with a high dose (30–50 mg/kg/day) of acetylsalicylic acid (ASA) until 48 h after disappearing of the fever, followed by a low dose (3–5 mg/kg/day) ASA continued depending on CAA development and size [14, 15]. Since the indications regarding corticosteroid therapy with IVIG and ASA were updated during the observational period [14], we adjusted our analyses for corticosteroid use as a possible confounding factor.
Definitions
According to the American Heart Association (AHA) diagnostic criteria [16], we defined CAA as a maximal Z-score ≥ 2.5 either in the left or right coronary artery. The coronary artery Z-score was calculated based on Dallaire and Dahdah Z-scores [17]. Following the AHA criteria [16], complete KD was defined by the presence of prolonged unexplained fever together with at least 4 of 5 of the principal features, incomplete/atypical KD by prolonged unexplained fever with fewer than 4 principal clinical findings.
Data collection and analysis
We collected data on demography (sex, birth date, and ethnicity), clinical symptoms (onset date defined as the first day the patient presented with signs related to KD, hospitalization date, clinical findings, and persisting or relapsing fever on day 2 after the initial IVIG therapy), therapy (treatment date, therapies used, therapeutic failure defined as the need of second-line therapy) and cardiac findings (date of echocardiography, coronary artery Z-scores, and other abnormalities as pericarditis, myocarditis and ventricular dysfunction). Data were collected from electronic records and patient charts.
We compared patients with baseline Z-score ≥ 2 and with patients with baseline Z-score < 2. The chi-square or Fisher’s exact tests were used for categorical variables and the Mann-Whitney U-test for continuous ones. Univariate and multivariate (adjusting for age and corticosteroid therapy) logistic regression analyses were used to derive the odds ratios (ORs) and 95% confidence intervals (CIs) between the risk scores, a baseline Z-score ≥ 2 and ≥ 2.5 with CAAs at one, two, and six-month follow-up. Statistical significance was considered as a p-value < 0.05. Statistical analysis was performed using R software (version 3.6.3 for Windows).
Results
During the observational period, 89 patients were diagnosed with KD. We excluded 2 patients who did not receive the IVIG therapy, 8 patients who received IVIG therapy 10 days after the presentation, and 2 patients who had no data for the scores. We included 77 patients, 51 (66%) male, and 26 (34%) female, with a median age at presentation of 27 months (IQR 13–46). Table 2 gives the baseline characteristics, clinical data, and treatments of the patients, and the CAAs at one, two, and six months. Twelve (16%) patients needed a second IVIG infusion. Ten (13%) children received adjunctive steroid therapy with the first IVIG therapy, 6 (8%) of them by the intravenous route, and 4 (5%) by oral route, none of them repeated the steroid infusion. One (1%) patient received a steroid intravenous infusion with the second IVIG therapy. None of the patients received cyclosporine or biologic response modifiers.
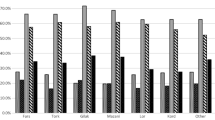
Overall, 26 (34%) patients had a baseline Z-score ≥ 2, and 22 (29%) had a baseline Z-score ≥ 2.5. Ten (13%) patients had at least one CAA at the one-month follow-up, 8 (10%) at the two-month follow-up, and 4 (5%) at the six-month follow-up. Five (6%) patients had a recent (< 8 weeks) or concurrent SARS-CoV-2 infection. Patients with a baseline Z-score ≥ 2 were younger than patients with a normal baseline Z-score (median age 14 vs. 34 months respectively, p-value < 0.01). We did not find any other difference between the two groups. Table 3 summarizes the results of the risk scores.
A baseline Z-score ≥ 2 was associated with CAA development at one month (OR 10, CI 2–72, p-value < 0.01 using the univariate analysis and OR 6, CI 1.2–42, p-value = 0.04 using the multivariate analysis) and two months (OR 18, CI 3-357, p-value < 0.01 univariate, OR 11, CI 2-226, p-value = 0.03 multivariate) but not at six-month follow-up. A baseline Z-score ≥ 2.5 showed a positive association with aneurysm development at one month (OR 8, CI 2–39, p-value < 0.01 univariate, OR 6, CI 1.3–33, p-value = 0.03 multivariate), two months (OR 10, CI 2–73, p-value < 0.01 univariate, OR 7, CI 1.4–55, p-value = 0.03 multivariate), but not at six months (OR 3, CI 0.3–23, p-value = 0.3). Table 4 gives the sensitivity and specificity of the baseline Z-score ≥ 2 and ≥ 2.5 to predict CAAs at one, two and six-month follow-up.
The Son score showed a positive association with CAAs at one month (OR 3, CI 1.3-7, p-value = 0.01), two months (OR 3, CI 1.3-8, p-value = 0.01), but not at six months (OR 2, CI 0.6-7, p-value 0.2). After adjusting for age and corticosteroid therapy, we did not find an association between the Son and CAAs during the follow-up period (OR 2, CI 0.8-5, p-value 0.2 at one month, OR 2, CI 0.8-6, p-value 0.1 at two months and OR 1.3, CI 0.3-5, p-value 0.7 at six months).
None of the other risk scores were associated with CAA development at one, two, and six-month follow-ups. Table 5 shows their ORs and p-values.
Discussion
To our knowledge, this is the first study to evaluate the association between risk scores and baseline coronary Z-scores with CAAs and coronary dilations in Italy. We found a strong association of initial Z-score ≥ 2 and ≥ 2.5 with CAAs at one and two months of illness, with higher ORs of the baseline Z-score ≥ 2. These findings are consistent with the study conducted by Son et all in North America that reported a high predictive utility of a baseline Z-score ≥ 2 for CAA development [10]. Among the scores we tested, only the Son score showed a high predictive value for CAAs at one and two months of illness [11]. In our sample, a Z-score ≥ 2 showed a stronger association with CAAs at one and two-month follow-ups. We also extended our follow-up until six months, while Son et all evaluated only the presence of CAAs at 4 and 8 weeks of illness [10, 11]. The baseline Z-scores were not significantly associated with CAAs at 6 months, but this result could be affected by the low number of patients who presented CAAs at 6 months, which limits the power of the study.
We tested both a baseline Z-score ≥ 2 and ≥ 2.5, with a Z-score ≥ 2 showing higher associations with the outcomes. We also evaluated the Kawanet and the Kawanet-echo score performances, which were developed in the European cohort [12, 13], but none of them was associated with CAAs. Consisting with previous studies, we found that Japanese scores have low performance for the non-Japanese population [9, 10, 12, 18, 19].
The European guidelines recommend that all KD patients should undergo echocardiography at baseline, then after 2 weeks after IVIG administration, and then after 6–8 weeks after disease onset [14]. The Italian guidelines for KD recommend an echocardiogram on all patients when diagnosed with KD, then at 2, 4, and 8 weeks for uncomplicated cases and assessing the Z-score of the coronary artery at every stage [15]. If echocardiography is not available the IVIG infusion should not be delayed [14, 15].
Our findings suggest that patients with a baseline Z-score ≥ 2 have a higher risk for CAAs in the long term and that in our contest the baseline Z-score is the best predictor for CAAs development. Since the CAA is the most serious complication in KD [20], we encourage that multi-centric European studies be performed in this subgroup of patients to test more aggressive treatment from the diagnosis.
We found that 34% of our patients had baseline Z-score ≥ 2 and 29% had a baseline CAA. Our incidence of coronary artery dilatation and aneurysm is higher than the one found by Son et al. (29% and 19% respectively) [11] but lower than the one found by Dallaire et al. (65% and 33.5% respectively) [21]. The incidence of coronary artery dilation in different ethnic groups is not established and, in accord with the AHA, it could be more common than previously thought [16].
SARS-CoV-2 seems to trigger both KD and multisystem inflammatory syndrome (MIS-C) phenotypes [22]. We did not include MIS-C patients according to the World Health Organization and Centers for Disease Control and Prevention Guidelines who did not meet KD diagnostic criteria [23, 24]. Differential diagnosis between KD and MIS-C could be difficult because they share overlapping clinical presentations [25, 26]. All the patients included in the present study were discharged with a diagnosis of KD, moreover, four expert clinicians, two paediatric immunologists and two paediatric cardiologists, analysed the cases to include to better discriminate between the two diagnoses. A Korean study did not find differences in cardiac complications between patients with KD with and without a recent COVID-19 infection [27]. Since in our sample, only five patients had recent or concurrent SARS-CoV-2 infection, we did not evaluate the differences between the two groups. Larger studies should evaluate the difference in cardiac complications in European cohorts.
We had a variation in echocardiogram timing. The indications regarding corticosteroid therapy changed during the observational period [14], which could have resulted in different therapeutic management of our patients. We tried to reduce the bias of this possible confounding factor by adjusting our analyses for corticosteroid therapy. Moreover, we could not calculate the score value for many patients, such as Sano and Kobayashi scores which were calculated for less than half of the sample. Despite the European and Italian recommendations, many centres cannot perform an echocardiogram before the initiation of the treatment [28]. Even if relatively large, our dataset could not allow us to assess the association between the scores and baseline Z-score with CAAs at six-month follow-up, because only 4 patients had CAAs at 6 months.
We tested seven scores, some of them recently proposed, anyway, we did not test the recently developed score in the Chinese population from Lui et all [29], whose performance should be assessed in the non-Asian population. However, the Lui score does not contain the baseline Z-score as a variable and our results suggest that it is not the best scoring system in our contest.
The strengths of our research are the introduction of the six-month follow-up outcome that, even if the limited sample size could not allow us to make a firm conclusion, shows a result changing from the two-month follow-up, suggesting that future studies should extend the observational period. We uniformly assessed the coronary artery Z-score in referring to Dallaire and Dahdah Z-scores [17]. Moreover, the monocentric setting allows a more uniform coronary Z-scores measurement.
Conclusion
Patients with a baseline Z-score ≥ 2 are at higher risk for CAAs in the long term, suggesting that more aggressive treatment should be tested with ad hoc studies. Even if inferior to the baseline Z-score alone, the Son score was associated with CAAs at 4 and 8 weeks from disease onset, it should be evaluated in larger European samples. Moreover, predictors for CAAs outcome should be considered in a longer observational period than 8 weeks from disease onset, since we found changes in our results between the two- and six-month follow-up.
Data availability
Data are available at the corresponding author upon reasonable request.
Abbreviations
- AHA:
-
American Heart Association
- ASA:
-
Acetylsalicylic acid
- CAA:
-
Coronary artery aneurysm
- CI:
-
Confidence interval
- IVIG:
-
Intravenous immune globulin
- KD:
-
Kawasaki disease
- MIS-C:
-
Multisystem inflammatory syndrome
- OR:
-
Odds ratio
References
Watts RA, Hatemi G, Burns JC, Mohammad AJ. Global epidemiology of vasculitis. Nat Rev Rheumatol. 2022;18(1):22–34. https://doi.org/10.1038/s41584-021-00718-8. Epub 2021 Dec 1. PMID: 34853411; PMCID: PMC8633913.
Kato H, Sugimura T, Akagi T, Sato N, Hashino K, Maeno Y, Kazue T, Eto G, Yamakawa R. Long-term consequences of Kawasaki disease. A 10- to 21-year follow-up study of 594 patients. Circulation. 1996;94(6):1379-85. https://doi.org/10.1161/01.cir.94.6.1379. PMID: 8822996.
Newburger JW, Takahashi M, Burns JC, Beiser AS, Chung KJ, Duffy CE, Glode MP, Mason WH, Reddy V, Sanders SP et al. The treatment of Kawasaki syndrome with intravenous gamma globulin. N Engl J Med. 1986;315(6):341-7. https://doi.org/10.1056/NEJM198608073150601. PMID: 2426590.
Harada K. Intravenous gamma-globulin treatment in Kawasaki disease. Acta Paediatr Jpn. 1991;33(6):805–10. https://doi.org/10.1111/j.1442-200x.1991.tb02612.x
Tewelde H, Yoon J, Van Ittersum W, Worley S, Preminger T, Goldfarb J. The Harada score in the US population of children with kawasaki disease. Hosp Pediatr. 2014;4(4):233–8. https://doi.org/10.1542/hpeds.2014-0008
Egami K, Muta H, Ishii M, et al. Prediction of resistance to intravenous immunoglobulin treatment in patients with Kawasaki disease. J Pediatr. 2006;149(2):237–40. https://doi.org/10.1016/j.jpeds.2006.03.050
Kobayashi T, Inoue Y, Takeuchi K, et al. Prediction of intravenous immunoglobulin unresponsiveness in patients with Kawasaki disease. Circulation. 2006;113(22):2606–12. https://doi.org/10.1161/CIRCULATIONAHA.105.592865
Sano T, Kurotobi S, Matsuzaki K, et al. Prediction of non-responsiveness to standard high-dose gamma-globulin therapy in patients with acute Kawasaki disease before starting initial treatment. Eur J Pediatr. 2007;166(2):131–7. https://doi.org/10.1007/s00431-006-0223-z
Rigante D, Andreozzi L, Fastiggi M, Bracci B, Natale MF, Esposito S. Critical overview of the risk scoring systems to predict non-responsiveness to intravenous immunoglobulin in Kawasaki syndrome. Int J Mol Sci. 2016;17(3):278. https://doi.org/10.3390/ijms17030278
Son MBF, Gauvreau K, Kim S, et al. Predicting coronary artery aneurysms in Kawasaki disease at a north American center: an assessment of baseline z scores. J Am Heart Assoc. 2017;6(6):e005378. https://doi.org/10.1161/JAHA.116.005378. Published 2017 May 31.
Son MBF, Gauvreau K, Tremoulet AH, et al. Risk model development and validation for prediction of coronary artery aneurysms in Kawasaki disease in a North American population. J Am Heart Assoc. 2019;8(11):e011319. https://doi.org/10.1161/JAHA.118.011319
Piram M, Darce Bello M, Tellier S, et al. Defining the risk of first intravenous immunoglobulin unresponsiveness in non-asian patients with Kawasaki disease. Sci Rep. 2020;10(1):3125. https://doi.org/10.1038/s41598-020-59972-7. Published 2020 Feb 20.
Ouldali N, Dellepiane RM, Torreggiani S, et al. Development of a score for early identification of children with Kawasaki disease requiring second-line treatment in multi-ethnic populations in Europe: a multicentre retrospective cohort study. Lancet Reg Health Eur. 2022;22:100481. https://doi.org/10.1016/j.lanepe.2022.100481. Published 2022 Aug 6.
de Graeff N, Groot N, Ozen S, et al. European consensus-based recommendations for the diagnosis and treatment of Kawasaki disease - the SHARE initiative. Rheumatology (Oxford). 2019;58(4):672–82. https://doi.org/10.1093/rheumatology/key344
Marchesi A, Tarissi de Jacobis I, Rigante D, et al. Kawasaki disease: guidelines of the Italian society of pediatrics, part I - definition, epidemiology, etiopathogenesis, clinical expression and management of the acute phase. Ital J Pediatr. 2018;44(1):102. https://doi.org/10.1186/s13052-018-0536-3. Published 2018 Aug 30.
McCrindle BW, Rowley AH, Newburger JW, Burns JC, Bolger AF, Gewitz M, et al. Diagnosis, treatment, and long-term management of Kawasaki disease: a scientific statement for health professionals from the American Heart Association. Circulation. 2017;135(17). https://doi.org/10.1161/cir.0000000000000484
Dallaire F, Dahdah N. New equations and a critical appraisal of coronary artery Z scores in healthy children. J Am Soc Echocardiogr. 2011;24(1):60–74. https://doi.org/10.1016/j.echo.2010.10.004
Davies S, Sutton N, Blackstock S, et al. Predicting IVIG resistance in UK Kawasaki disease. Arch Dis Child. 2015;100(4):366–8. https://doi.org/10.1136/archdischild-2014-307397
Sleeper LA, Minich LL, McCrindle BM, et al. Evaluation of Kawasaki disease risk-scoring systems for intravenous immunoglobulin resistance. J Pediatr. 2011;158(5):831–835e3. https://doi.org/10.1016/j.jpeds.2010.10.031
Mossberg M, Mohammad AJ, Kahn F, Segelmark M, Kahn R. High risk of coronary artery aneurysm in Kawasaki disease. Rheumatology (Oxford). 2021;60(4):1910–4. https://doi.org/10.1093/rheumatology/keaa512. PMID: 33150451; PMCID: PMC8023999.
Dallaire F, Fournier A, Breton J, Nguyen T-D, Spigelblatt L, Dahdah N. Marked variations in serial coronary artery diameter measures in kawasaki disease: a new indicator of coronary involvement. J Am Soc Echocardiogr. 2012;25(8):859–65. https://doi.org/10.1016/j.echo.2012.05.019
Biesbroek G, Kapitein B, Kuipers IM, Gruppen MP, van Stijn D, Peros TE, van Veenendaal M, Jansen MHA, van der Zee CW, van der Kuip M, von Asmuth EGJ, Mooij MG, den Boer MEJ, Landman GW, van Houten MA, Schonenberg-Meinema D, van Tutu AM, van Boele M, Scherpbier H, van Meijgaarden KE, Ottenhoff THM, Joosten SA, Ketharanathan N, Blink M, Brackel CLH, Zaaijer HL, Hombrink P, van den Berg JM, Buddingh EP, Kuijpers TW. Inflammatory responses in SARS-CoV-2 associated multisystem inflammatory syndrome and Kawasaki disease in children: an observational study. PLoS ONE. 2022;17(11):e0266336. https://doi.org/10.1371/journal.pone.0266336. PMID: 36449533; PMCID: PMC9710748.
Living guidance for clinical management of COVID-19. World Health Organization; 2021 [cited 2023 Nov 29]. Available from: https://www.who.int/publications/i/item/WHO-2019-nCoV-clinical-2021-2
Han archive – 00432. Centers for Disease Control and Prevention; 2020 [cited 2023 Nov 30]. Available from: https://emergency.cdc.gov/han/2020/han00432.asp
Fabi M, Dondi A, Andreozzi L, Frazzoni L, Biserni GB, Ghiazza F, et al. Kawasaki disease, multisystem inflammatory syndrome in children, and adenoviral infection: a scoring system to guide differential diagnosis. Eur J Pediatrics. 2023;182(11):4889–95. https://doi.org/10.1007/s00431-023-05142-6
Henderson LA, Canna SW, Friedman KG, Gorelik M, Lapidus SK, Bassiri H, et al. American college of rheumatology clinical guidance for multisystem inflammatory syndrome in children associated with SARS–cov-2 and hyperinflammation in pediatric Covid‐19: Version 2. Arthritis & Rheumatology. 2021;73(4). https://doi.org/10.1002/art.41616
Roh DE, Lim YT, Kwon JE, Kim YH. Kawasaki disease following SARS-CoV-2 infection: stronger inflammation with no increase in cardiac complications. Front Pediatr. 2022;10:1036306. https://doi.org/10.3389/fped.2022.1036306. Published 2022 Nov 17.
Koné-Paut I, Piram M. Importance of predicting non-response to intravenous immunoglobulin therapy in non-asian patients with Kawasaki disease. Lancet Reg Health Eur. 2022;22:100507. https://doi.org/10.1016/j.lanepe.2022.100507. PMID: 36106336; PMCID: PMC9465312.
Liu HH, Chen WX, Niu MM, et al. A new scoring system for coronary artery abnormalities in Kawasaki disease. Pediatr Res. 2022;92(1):275–83. https://doi.org/10.1038/s41390-021-01752-8
Acknowledgements
not applicable.
Funding
This study was partially funded by Italian Ministry of Health - Current research IRCCS.
Author information
Authors and Affiliations
Contributions
RMD, LM, CA and AL conceptualized and designed the study. RS, AL, RA, RMD and LM designed the data collection instruments and collected data. AL was responsible for the analysis and interpretation of data. AL drafted the manuscript. CA, RMD, LM, LAB and RS performed a critical revision of the manuscript and gave a significant contribution in their field of expertise. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was conducted in accordance with the Declaration of Helsinki. The Milano Area 2 Ethical Committee approved the study, which included a waiver of informed consent because of the retrospective nature of the investigation (No 2018/0802).
Consent for publication
not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
La Vecchia, A., Stracquadaino, R., Mauri, L. et al. Risk factors and scores for prediction of coronary artery aneurysms in Kawasaki disease: a European monocentric study. BMC Pediatr 24, 139 (2024). https://doi.org/10.1186/s12887-024-04623-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-024-04623-3