Abstract
Aim
To synthesize available evidence on the association between change in linear growth (height for age z score, HAZ) beyond the first two years of life with later child neurodevelopment outcomes in Low- and middle-income countries (LMICs).
Methods
We searched PubMed, Web of Science, and EMBASE for cohort studies on the association between change in HAZ after age two and neurodevelopment outcomes in middle or late childhood. Data extraction was done independently by two reviewers.
Results
A total of 21 studies, that included 64,562 children from 13 LMICs were identified. Each unit increase in change in HAZ above two years is associated with a + 0.01 increase (N = 8 studies, 27,393 children) in the cognitive scores at 3.5 to 12 years of age and a + 0.05-standard deviation (SD) increase (95% CI 0.02 to 0.08, N = 3 studies, 17,830 children) in the language score at 5 to 15 years of age. No significant association of change in HAZ with motor (standardized mean difference (SMD) 0.04; 95% CI: -0.10, 0.18, N = 1 study, 966 children) or socio-emotional scores (SMD 0.00; 95% CI: -0.02, 0.01, N = 4 studies, 14,616 participants) was observed.
Conclusion
Changes in HAZ after the first two years of life appear to have a small or no association with child neurodevelopment outcomes in LMICs.
Similar content being viewed by others
Introduction
Children from low-and middle-income countries (LMICs) settings have been shown to suffer from linear growth faltering, manifested as a high proportion of stunting [1, 2]. Additionally, a substantial number of children from these settings are also documented to not reach their full developmental potential [3, 4]. The largest number of children estimated to not reach their full developmental potential are from sub-Saharan Africa followed by South Asia, which are also regions that experience high levels of stunting [2, 4]. The relationship between linear growth and neurodevelopment in children under two years of life is well documented [5, 6]. Children who are stunted or those with linear growth deficits have been shown to have suboptimal cognitive, psychological language, and motor performance as well as poorer academic performance [7,8,9]. On similar lines, optimal linear growth in the first two years of life has been shown to be associated with better developmental outcomes. Cognition represents the intellectual abilities of children, such as their intelligent quotient (IQ), executive functions, reasoning skills, and academic abilities like early math or reading skills. Motor development includes both fine and gross motor skills, and it involves milestones like when a child starts to walk. Socioemotional development encompasses aspects like behavior, attachment, emotional expression, and temperament [5]. Language development pertains to a child's ability to communicate thoughts and feelings using words and symbols that are part of their community's native language [10]. A meta-analysis of 68 studies from 29 LMICs showed that each unit increase in HAZ score for children ≤ 2 years was associated with a 0.22-SD increase in cognition at 5 to 11 years [5]. This review focused on cross-sectional studies, exploring the connection between length of age z scores (LAZ) or HAZ scores and neurodevelopment. However, it did not provide summary estimates for studies for examining the relationship between changes in HAZ or height over time and child development [5].
It is believed that in the early formative years of life, both poor linear growth and sub-optimal neurodevelopment share overlapping causes such as inadequate nutrition, high burden of infections and hospitalization, and sub-optimal care at home [11]. In infancy, deficiencies in essential micronutrients like iodine, zinc, iron, copper, vitamin B12, and choline can impede neurocognitive development. Neonatal iodine deficiency is associated with compromised mental abilities, including cretinism in severe cases, and can lead to a 10–15-point reduction in population-level IQ. Insufficient iron intake early in life can result in irreversible behavioral issues [12,13,14]. The presence of any of these exposures, either alone or in combination may therefore negatively impact both growth and development. With the publication of recent studies that show that recovery from stunting is possible beyond the first 2–3 years of life, there is growing interest in understanding if this improvement leads to enhanced neurodevelopment in children [15,16,17,18]. It may mean that if such an association is established, it may lead to more focus on improving the linear growth of children in later years of life. However, it should be noted that neurodevelopment in children is multi-factorial and influenced by key factors such as home environment, nutrition, environmental hygiene, caregiving practices, opportunities for learning, and morbidity prevention. Linear growth is largely a proxy for nutritional and morbidity status and therefore, efforts to improve linear growth would mean more investment in enhancing the nutritional status and reducing the morbidities with a secondary benefit of improving neurodevelopment, school performance, and adult productivity [11, 19].
Based on evidence from recent studies that show the possibility of recovery from early growth failure, we aimed to examine whether growth catch up after 2 years of age was associated with neurodevelopmental outcomes [20,21,22,23]. While there are studies exploring the association between change in child HAZ between early and middle/late childhood and neurodevelopment, given that contemporary literature has shown that there is a possibility of catch-up growth after the initial years of life, there has been no systematic effort to synthesize the evidence on this aspect. More so, the findings from individual studies are not coherent. Therefore, we conducted a systematic review and meta-analysis of observational studies that examined the relationship of change in HAZ with neurodevelopmental outcomes. The review is intended to inform whether interventions that promote growth-catch up after the first two years of life may also impact child development outcomes in LMICs.
Methods
Data sources and search strategy
This review was registered in PROSPERO (registration number CRD42022352290). We followed the standard PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines for the conduct of this review [24]. The electronic search aimed at identifying studies published from database inception until 31st December 2022. We used three databases i.e., PubMed®, Web of Science, and EMBASE® to perform a literature search. There were no date or language restrictions. The search strategy used for the three databases has been presented in Additional Table 1. The reference lists of the selected articles were searched manually to identify additional relevant articles.
Study selection and data extraction
We selected cohort/follow-up studies that included children of 2 years and above and showed the relationship between change in HAZ over time and child development. As a result, studies had to have at least two HAZ measurements and should have examined the association between the later–first HAZ measurement with neurodevelopment outcomes. The neurodevelopment outcomes encompass cognition (IQ, executive functioning, and reasoning skills), motor (gross and fine), language, socioemotional-like behavior, temperament, and social competence of a child. There was no exclusion based on the timing between measurements. Although not the primary exposure of interest, we were also interested in documenting whether a change in stunting status was associated with child development outcomes. Therefore, we also included studies that presented data on the change in stunting status after two years of age and its association with neurodevelopmental outcomes. We excluded studies with cross-sectional or case–control designs and from high-income countries, as defined by the World Bank criteria [25]. The primary outcomes of interest were cognition, motor, language, and socio-emotional performance. In addition, we were interested in other aspects of development, including academic achievements, performance in subjects like math and language, school attendance, and other indicators of human capital, as reported in the included studies. All outcomes were reported at the latest follow-up. For the assessment of cognition, language, motor skills, and socio-emotional domains, a variety of neurodevelopmental tools were utilized [26,27,28,29,30,31,32]. All such tools used by the authors for assessment will be reported in the summary table.
We used Covidence systematic review software, Veritas Health Innovation, Melbourne, Australia [33]. Two review authors (BGP, SR) independently screened the titles and abstracts to identify the relevant citations, followed by a full-text review. The data was extracted using a modified version of the Cochrane Effective Practice and Organisation of Care Group data collection checklist (Cochrane EPOC Group 2017) [34]. This included study identifiers, study design, participant characteristics, sample size, tools for outcome assessments, and outcome effects. The disagreements or discrepancies between reviewers were resolved by discussions or by referring to a third senior review author (RPU).
Data analysis and quality assessment
Analysis was performed using Stata 16 software (TX, USA). We reported standardized mean difference (SMD) along with 95% confidence intervals (CIs). As an apriori decision, we decided to include adjusted reported effect sizes from the studies. We defined a set of important variables that preferably should have been adjusted, based on our reading of prior literature. This included variables such as gender, maternal years of schooling, maternal age, maternal depressive symptoms, paternal years of schooling, socio-economic status, residence (urban or rural), child stimulation at home, birth order, and food security. Different studies used different variables for adjustment. However, those that had adjusted for one or more of the variables in our list were eligible to be included in our meta-analysis. The standardized mean difference (SMD) was used as summary statistic as the studies used different psychometric scales for assessing the outcomes of interest. For studies that reported outcomes, especially the IQ/cognitive scores, as mean difference, we calculated SMD using the reported standard deviation (SD) of the overall sample for that particular outcome. We decided to use the random effects model, using the restricted maximum likelihood method (REML), as the included studies differed in their methodology with respect to outcomes considered and tools for measurement, age at outcome assessment and were from different demographic settings. These differences were bound to create substantial heterogeneity (indicated by I2 greater than 50%) and therefore, random effects model was considered to be a reliable analytic choice [35]. In the studies included in our review, there was a significant disparity in follow-up duration. Some studies had relatively short follow-up periods of less than 5 years, while others extended beyond 10 years. Presenting subgroup analysis based on periods of follow-up allowed us to examine how changes in linear growth over time (short and long periods) might impact neurodevelopment. We also provided an overall estimate by including studies, irrespective of the duration of follow-up, to complete the entire picture. This approach allowed us to investigate the dynamic relationship between growth catch-up and neurodevelopmental outcomes across different time frames. Understanding the effects of linear growth catch-up over a short and long term follow up on neurodevelopment can have important clinical and policy implications. For example, it might inform healthcare providers and governments to decide for how long programmatic efforts should be made to improve linear growth in children, with an additional benefit of improving neurodevelopment. Additionally, to examine heterogeneity resulting from these variations in follow-up duration, we categorized the follow-up periods into two groups: those less than 5 years and those exceeding 5 years. Publication bias was assessed using Egger’s test and funnel plots [36]. Assessment of the quality of studies was done using the Newcastle–Ottawa Scale [37].
Results
The study flow chart is presented in Fig. 1. Our literature search, as detailed in Supplementary Box 1, initially yielded 5,996 unique citations. After removing 266 duplicates and conducting title and abstract screenings, we proceeded to review the full text of 99 studies. Following this assessment, 82 studies were excluded (see Fig. 1). Subsequently, a bibliographic review of the remaining 17 studies led us to identify an additional 4 relevant studies. As a result, a total of 21 studies were included in this review (Supplementary Table 1). The 21 studies reported on 64,562 children from 13 countries, representing low-income, low-middle-income, and upper-middle-income countries (Table 1). Among the studies that contributed to the quantitative analysis, there were 13 studies that presented data on the cognitive score [16, 18, 38,39,40,41,42,43,44,45,46,47,48], one on motor score [45] and four on language [17, 39, 40, 49] and four on socio-emotional score [39, 44, 45, 48].
Four studies analyzed data from the Young Lives study [17, 42, 49, 52]. Fink et al. included the older cohort of children aged 8 years and above [49]. Crookston et al. (2010) included children with first/baseline HAZ measured at 6–18 months and endline at 4–6 years and examined the association of change in HAZ with cognitive scores [42]. Crookston et al. (2013), and Georgiadis et al. (2017) included children with baseline HAZ at 12 months and follow-up HAZ at 8 years. These two studies examined the association between HAZ and verbal scores [17, 52]. We expected a substantial, if not complete, overlap of subjects among these two studies and decided to include Georgiadis et. al. (2017) in the quantitative analysis as this was a comparatively recent study [17]. As Crookston et al. (2013) reported on additional outcomes such as academic performance and math scores, we included it for the narrative synthesis of findings [52]. We also reported on few additional outcomes i.e., school overage, academic performance, and human capital metrics which were extracted from some of the included studies [15, 44, 46, 48, 50, 51]. There were 17 good quality studies [9, 15,16,17, 39, 40, 42,43,44,45,46,47,48,49, 51,52,53] and remaining four were of fair quality [18, 38, 41, 54] (Supplementary Table 2).
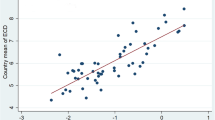
Cognitive scores
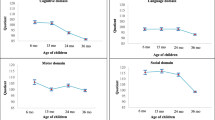
A total of 8 studies presented the relationship between the change in the HAZ and cognitive scores [38,39,40, 44,45,46,47,48]. Our analysis noted that each unit increase in change in HAZ was associated with a + 0.01 SD increase in the cognitive score at 3.5 to 12 years of age (95% CI: 0.00, 0.03, I2 = 0.08%, N = 8 studies, 27,393 participants) (Fig. 2). Egger’s test did not suggest the presence of publication bias (P = 0.40) and the funnel plot is presented in Supplementary Fig S1. In the subgroup analysis, we observed one study had a follow-up period of less than 5 years, and was associated with a unit increase in change in HAZ was -0.02 SD (95% CI: -0.14, 0.10, N = 1 study, 966 participants) [45] whereas with studies having longer follow up period (≥ 5 years), the pooled effect size was + 0.01 SD (95% CI: 0.00, 0.03, I2 = 0.03%, N = 7 studies, 26,427 participants) (Fig. 2) [38,39,40, 44, 46,47,48].
Compared to children who were “never stunted” in the period between early and middle childhood, those who “recovered” from stunting had similar cognitive scores (SMD -0.08; 95% CI: -0.19, 0.04, I2 = 70.82%, N = 6 studies, 5,300 participants) (Fig. 3) [16, 18, 41,42,43, 47]. No publication bias was present ( Supplementary Fig S2). On pooling of studies with short (< 5 years) duration of follow up, children who recovered from stunting had similar scores to those never stunted (SMD -0.10; 95% CI: -0.25, 0.05, I2 = 79.6%, N = 4 studies, 4,416 participants) (Fig. 3) [16, 18, 42, 43]. Similar finding was observed when studies with long duration (≥ 5 years) of follow up were pooled (SMD 0.01; 95% CI: -0.16, 0.17, I2 = 12.02%, N = 2 studies, 884 participants) (Fig. 3) [41, 47].
Motor domain scores
Only one study [45] reported on motor domain scores and found that each unit increase in change in HAZ after 18 months of age was not significantly associated with motor score at 4 to 6 years of age (SMD 0.04; 95% CI: -0.10, 0.18, N = 1 study, 966 participants).
Socio-emotional domain scores
For the socioemotional domain, estimates were reported in four studies [39, 44, 45, 48]. We noted no association between change in HAZ and socio-emotional scores (SMD 0.00; 95% CI: -0.02, 0.01, I2 = 0.00%, N = 4 studies, 14,616 participants) in children aged 3.5 to 12 years of age (Fig. 4). Egger’s test did not suggest the presence of publication bias (P = 0.61) and the funnel plot is presented is Supplementary Fig. S3. Subgroup analysis based on the duration of follow up also showed findings supporting lack of significant association (Fig. 4).
Language domain scores
Each unit increase in change in HAZ was significantly associated with language scores at ages 5 to 15 years (SMD 0.05; 95% CI: 0.02, 0.08, I2 = 0.00%, N = 3 studies, 17,830 participants) (Fig. 5) [39, 40, 49]. Egger’s test did not suggest the presence of publication bias (P = 0.48) and the funnel plot is presented is Supplementary Fig. S4. Georgiadis (2017) reported the findings from four low- and middle-income countries but did not provide pooled findings [17]. Hence, we have pooled the country-specific data from this study. Compared to children who were “never stunted”, those who “recovered” from stunting had similar scores (SMD -0.01; 95% CI: -0.03, 0.01, I2 = 62.5%, N = 1 study including 4 countries, 4,723 participants) at 12 years of age (Fig. 3) [17].
Other measures of development
The association of linear growth improvement beyond the early childhood with academic performance has been explored by some studies and the findings have been mixed. Four of the included studies analysed data from the Young Lives cohort and indicated that improvement in linear growth beyond the first two years may be associated with better academic outcomes [17, 49, 52]. Crookston et al. (2013) evaluated the schooling “overage” that denoted whether a child lagged behind the age-appropriate grade as per country-specific schooling norms. The authors noted that the change in HAZ from 1 to 8 years of age was inversely associated with overage for the grades [52]. Further, an increase in change in HAZ was found to be positively associated with performance in mathematics and reading comprehension [52]. Fink et al. reported that children who were stunted at age 8 years but managed to catch up with their peers by age 15 years, had better mathematics skills and educational achievement than did children who remained stunted [49]. Another Young Lives study found that children who showed persistent recovery from stunting from 1 to 8 years (i.e., those that were not stunted at age 5 and 8 years) performed better than children who remained stunted during this period in mathematical skills [17]. Glewwe et al. examined the impact of change in HAZ from 2 to 8 years on cognitive outcomes in a longitudinal cohort from the Philippines. However, the same cohort was also used in another study by Poveda et al. to assess the association between changes in HAZ and cognitive outcomes. As a result, we have presented the findings from the Glewwe study in Table 1 and decided not to include the study for pooled analysis to prevent data overlap [54].
Sunny et al. found that children who had improved HAZ scores over time (i.e., from 16 months to 8 years) performed better in schools compared to children who were persistently stunted [50]. Adair et al. concluded that faster linear growth between age 2 years to mid-childhood (6 to 9 years) was associated with a reduced risk of not completing secondary school [51]. Poveda et al. evaluated school attainment among children and concluded that linear growth from birth to ∼2 y of age was associated with higher school attainment, but similar associations were not noted for linear growth between 2 years to mid-childhood (6 to 9 years) [46]. Gandhi et al. reported that height gain was positively associated with mathematics test results (p = 0.003), reduced grade repetitions (p = 0.011), and the highest grade completed (p = 0.049) among children who attended school. However, no significant association was found between height gain and the highest grade completed (p = 0.194) when children who never attended school were included [53].
Other related aspects of child development were also explored by some studies. For instance, Nguyen et al. concluded that child linear growth, both during and beyond the first 1000 days, was positively associated with mental health during the early school-age years [44]. Sachdev et al. measured human capital metrics consisting of education, male occupation, and material possession [15]. They concluded that height gain from 6 to 24 months was significantly associated with adult education, male occupation, and material possession while height gain after 24 months (till 5 years) was not significantly associated with other components of human metrics except male occupation [15].
Additionally, five studies conducted their baseline assessment of HAZ/LAZ prior to the age of 2 years. Hence, we have undertaken a sensitivity analysis, excluding studies that assessed baseline HAZ measurements before 24 months (Supplementary Fig. S5 to S8). To enhance the transparency of baseline assessment age, we have included a graph that incorporates all studies and their respective baseline assessment ages (Supplementary Fig. S9).
Discussion
We conducted this systematic review and meta-analysis to primarily understand if the change in linear growth after the first two years of life is associated with improvement in neurodevelopmental outcomes in middle and late childhood. We noted that with each unit increase in change in HAZ, there was a small improvement in cognitive and language score. We observed no association with motor or socio-emotional scores. Additionally, we also found that children who recovered from stunting after the first two years of life had statistically similar cognitive and language scores compared to those who were never stunted. There was also mixed evidence on the relationship of change in HAZ or stunting status with schooling attainment.
Sudfeld et al. in their meta-analysis included cross-sectional studies and found that each unit increase in HAZ among children aged above two years was associated with improvement in scores for cognitive ability (+ 0.09 SD) [5]. Our pooled effect size for association between change in HAZ and cognitive score was comparatively attenuated (+0.01 SD). This could be because we considered the exposure as change in HAZ through inclusion of cohort studies. An interesting observation in our study was that even though the improvement in cognitive and language scores with each unit increase in change in HAZ was small in magnitude, the children who recovered from stunting had similar scores to those who were never stunted. This may mean that those who recovered had their initial HAZ scores nearer to the cut-off for stunting (i.e., -2 SD) and even a small improvement in their HAZ would have had shifted them above the cut-off. Furthermore, this finding could be due to the use of an inaccurate method to measure changes in stunting over time, i.e., the use of a cut-off in HAZ scores to estimate recovery. The inadequacy of this approach has been demonstrated by Leroy and colleagues [19].
Available evidence strongly supports that the first 1000 days (conception through age 24 months) are foundational for brain development [55, 56]. During this period, brain development is rapid with specific neuronal processes occurring over specific time periods. Both adverse and positive experiences during this period critically shape children’s trajectories with respect to health, educational attainment, psychological well-being and economic capacity. Interventions in these early years are critical for brain growth and functioning [57, 58]. In response, many governments and multi-sectoral organizations have begun investing in early child development (ECD) and are promoting programmes addressing children’s development in the early years.
Over the past years, studies have established a fairly strong evidence base to suggest that linear growth in the first two years of life are associated with both concurrent and later childhood neurodevelopment outcomes [6]. The possible explanation for this association could be the shared factors, such as nutrition, repeated infections and morbidities, that influence both these child outcomes [10]. This observed association has been employed to such an extent that some consider linear growth in early childhood to be a proxy for child development. Consequently, public health programs largely invest in improving linear growth with the intent of securing an additional advantage of optimizing cognitive and other aspect of neurodevelopment. There is an added question which largely remains unaddressed systematically i.e., whether there is some potential in the period following the initial two years wherein investments for improving growth could provide dividends with respect to improving child developmental outcomes. Till recent, it was considered that there is limited likelihood of catch-up growth after the first 2–3 years of life as the children continue to remain living in the deprived environments that contributes to continued poor growth [10]. However, contemporary studies have undoubtedly shown that recovery from growth failure can occur [11,12,13,14]. Nevertheless, a limitation of this evidence is that few studies have utilized the cut-off HAZ scores for assessing recovery, and this method is an unreliable method [19]. This further demands an exploration of whether this recovery could also improve their cognitive and behavioural functioning as well as academic performance. In focusing on LMICs, our attention is drawn to their disproportionate burden of child stunting—an essential marker of childhood underdevelopment with enduring consequences. The choice of Height-for-Age Z score (HAZ) in this study is deliberate, given its simplicity, cost-effectiveness, and minimal equipment requirements, making it suitable for resource-limited LMICs. HAZ not only reflects early childhood growth but also acts as an early indicator for potential neurodevelopmental delays. Recognizing the challenges in healthcare systems and access to interventions for stunting in these regions, understanding the relationship between HAZ after 2 years and neurodevelopment becomes pivotal. This insight can guide decisions on the timing and cost-effectiveness of interventions, emphasizing the early identification of stunting and the initiation of targeted interventions before the age of 2. By leveraging HAZ, our goal is to promptly identify at-risk children, enabling tailored interventions for enhanced long-term outcomes in these resource-constrained settings.
Prado et al. in their recent meta-analysis showed that nutritional supplementation studies had comparatively higher impacts on linear growth compared to child development outcomes [59]. Further, studies that focused on child stimulation had higher impact on development outcomes compared to growth. Based on these findings, we agree with the authors that the factors that affect linear growth and cognition in later childhood may either not be entirely similar. Consequently, there is a need to specifically target determinants of neurodevelopment rather than attempting to achieve improvement through increase in linear growth.
Through this systematic review and meta-analysis, we also noted that the studies that have conducted long term follow up of children in a systematic and thorough manner are limited. Most studies performed assessments of growth and neurodevelopment at the time of recruitment in the study and at the time of follow-up assessment. One of the reasons could be the limited amount of funding available to carry out such an exercise. The limitation with this nature of assessment and subsequent analysis looking at the relationship between change in linear growth and neurodevelopment outcomes is that the data from the intermediate period is unavailable and information on many of the variables that could influence child neurodevelopment is lacking. Some of these variables include quality of care and stimulation at home, infections and morbidities, transitional changes in anthropometric measures, food security and quality of nutrition. These considerations call for a more supervised and robust follow up wherein data on important variables is captured at frequent intervals.
This is probably one of the first attempts to provide synthesized evidence on the association of “change in linear growth” between early and middle or late childhood and neurodevelopment outcomes. We have reported pooled estimates for this association for a wide range of outcomes i.e., cognitive, language, and socioemotional, as well as recovery from stunting with cognitive and language measures. Moreover, the extensive inclusion of 64,562 children in our study enhances the statistical power of our analysis, while our broad coverage of 13 countries across different income brackets (low, LMICs, and UMIC) enhances the generalizability of our findings. There are some limitations of our analysis that should be considered while interpreting the findings. First, all the included studies were observational in design and therefore, it may not be possible to ascertain a causal link between change in linear growth and neurodevelopmental outcomes. Second, for outcomes other than cognitive performance, the number of available studies were few and therefore, reliable pooled estimates could not be calculated. We noted significant heterogeneity for some of the outcomes. This could be due to differences in the tools measuring neurodevelopment, age at which the children were recruited for baseline assessment, age at follow up assessment, the duration of follow up and variables adjusted for in the statistical analysis. Further, for the cognitive outcome, we included data on a number of related constructs (such as attention, reasoning, IQ) that may have led to some degree of imprecision. An important limitation is the possibility of overlap of children studied in the publications arising out of the Young Lives cohort data [17, 42, 49, 52]. We identified four relevant studies but excluded two studies from the quantitative synthesis because, upon careful examination of the study methods, we found significant overlap of children in this study with another study from the same cohort [17, 52]. However, the possibility that such an overlap still persists among the three remaining studies cannot be overruled. A notable limitation in some studies included in this review is the use of non-validated scales for participant assessment. This calls for caution when interpreting the study findings and drawing conclusions about child neurodevelopment in LMICs. When one uses tools with standards that are not specific to the study population, the direction of association observed may not be impacted; however, the strength of association may not reflect the true estimate. The absence of validated tools and LMIC-specific norms raises concerns that children deemed to have "low" scores may not actually be experiencing developmental delays. These tools might introduce bias by adhering to norms established in high-income countries (HICs), potentially exaggerating the prevalence of delays in LMIC populations. Conversely, the absence of validated tools and LMIC norms may overlook children with genuine developmental challenges, resulting in underdiagnosed and missed opportunities for early intervention. Another possible limitation is that we studied the association of change in HAZ score with selected domains of child development and therefore, the findings may not be applicable to other important aspects of development. Furthermore, the studies included in our analysis provided data on HAZ scores, and there exists a point of contention regarding the concept of catch-up growth within our investigation. This is especially pertinent given that standard deviations for height are not consistent throughout early childhood; they notably increase from birth to 5 years of age. Consequently, when the height for age difference (HAD) (the observed height minus the median height for age according to growth standards) is negative but remains stable as a child ages, the Z-score will actually increase over time. This increase suggests catch-up growth in height, not because the absolute height deficit has diminished, but simply due to the denominator (the standard deviation) increasing [19]. Therefore, it is imperative that future studies investigate the relationship between HAD beyond 24 months of age and the subsequent development of children.
Conclusion
Based on the findings, we conclude that changes in HAZ during childhood after the first two years of life does not have strong associations with children’s development across domains. Additional follow up studies with robust methodology and periodic data collection on important factors that could influence neurodevelopment is needed to confirm our observations.
Availability of data and materials
All the data utilized for the analysis is presented in this manuscript. Any further query could be addressed to the corresponding author.
Abbreviations
- BMI:
-
Body mass index
- C.I.:
-
Confidence interval
- ECD:
-
Early childhood development
- HAZ:
-
Height for age z scores
- LAZ:
-
Length for age z scores
- HOME:
-
Home observation for measurement of the environment tool
- HCM:
-
Human capital metrics
- IQ:
-
Intelligence quotient
- LBW:
-
Low birth weight
- LMIC:
-
Low-Middle-income countries
- PRISMA:
-
Preferred reporting items for systematic review and meta-analysis
- REML:
-
Restricted maximum likelihood method
- SMD:
-
Standardized mean difference
- SD:
-
Standard deviation
- SES:
-
Socio-economic status
References
Mapping child growth failure across low- and middle-income countries. (1476–4687 (Electronic)).
Ssentongo P, Ssentongo AE, Ba DM, Ericson JE, Na M, Gao X, et al. Global, regional and national epidemiology and prevalence of child stunting, wasting and underweight in low- and middle-income countries, 2006-2018. Sci Rep. 2021;11(1):5204.
McCoy DC, Peet ED, Ezzati M, Danaei G, Black MM, Sudfeld CR, Fawzi W, Fink G. Early childhood developmental status in low- and middle-income countries: national, regional, and global prevalence estimates using predictive modeling. PLoS Med. 2016;13(6): e1002034.
Grantham-McGregor S, Cheung YB, Cueto S, Glewwe P, Richter L, Strupp B. Developmental potential in the first 5 years for children in developing countries. Lancet. 2007;369(9555):60–70.
Sudfeld CR, McCoy DC, Danaei G, Fink G, Ezzati M, Andrews KG, Fawzi WW. Linear growth and child development in low- and middle-income countries: a meta-analysis. Pediatrics. 2015;135(5):e1266-1275.
Prado EL, Abbeddou S, Adu-Afarwuah S, Arimond M, Ashorn P, Ashorn U, Bendabenda J, Brown KH, Hess SY, Kortekangas E, et al. Predictors and pathways of language and motor development in four prospective cohorts of young children in Ghana, Malawi, and Burkina Faso. J Child Psychol Psychiatry. 2017;58(11):1264–75.
Nahar B, Hossain M, Mahfuz M, Islam MM, Hossain MI, Murray-Kolb LE, et al. Early childhood development and stunting: Findings from the MAL-ED birth cohort study in Bangladesh. Matern Child Nutr. 2020;16(1):e12864
Walker SP, Chang SM, Powell CA, Simonoff E, Grantham-McGregor SM. Early childhood stunting is associated with poor psychological functioning in late adolescence and effects are reduced by psychosocial stimulation. J Nutr. 2007;137(11):2464–9.
Sunny BS, DeStavola B, Dube A, Kondowe S, Crampin AC, Glynn JR. Does early linear growth failure influence later school performance? A cohort study in Karonga district, northern Malawi. PLoS ONE. 2018;13.
Etchepareborda MC, Mulas F, Gandia R, Abad-Mas L, Moreno F, Díaz-Lucero A. Techniques for the functional evaluation of neurodevelopmental disorders. Rev Neurol. 2006;42(Suppl 2):S71-81.
Leroy JL, Frongillo EA. Perspective: what does stunting really mean? A critical review of the evidence. Adv Nutr. 2019;10(2):196–204.
Semba RD, Delange F. Iodine in human milk: perspectives for infant health. Nutr Rev. 2001;59(8 Pt 1):269–78.
Adamo AM, Oteiza PI. Zinc deficiency and neurodevelopment: the case of neurons. BioFactors. 2010;36(2):117–24.
Lockyer F, McCann S, Moore SE: Breast Milk Micronutrients and Infant Neurodevelopmental Outcomes: A Systematic Review. Nutrients 2021, 13(11).
Sachdev HS, Kathuria A K, Sinha Sikha, Anand D, Bhargava SK. Association of human capital with physical growth from birth to adulthood evidence from the new delhi birth cohort, India.2020.available from Association of Human Capital with Physical Growth from Birth to Adulthood : Evidence from the New Delhi Birth Cohort, India (worldbank.org). Accessed 3 Aug 2022.
Casale D, Desmond C Recovery from stunting and cognitive outcomes in young children: evidence from the South African Birth to Twenty Cohort Study. (2040–1752 (Electronic)).
Georgiadis A, Benny L, Duc LT, Galab S, Reddy P, Woldehanna T. Growth recovery and faltering through early adolescence in low- and middle-income countries: Determinants and implications for cognitive development. Soc Sci Med. 2017;179:81–90.
Sokolovic N, Selvam S, Srinivasan K, Thankachan P, Kurpad AV, Thomas T. Catch-up growth does not associate with cognitive development in Indian school-age children. (1476–5640 (Electronic)).
Leroy JL, Ruel M, Habicht J-P, Frongillo EA. Using height-for-age differences (HAD) instead of height-for-age z-scores (HAZ) for the meaningful measurement of population-level catch-up in linear growth in children less than 5 years of age. BMC Pediatr. 2015;15(1):145.
Anand P, Behrman JR. Dang H-AH, Jones S: Varied patterns of catch-up in child growth: Evidence from Young Lives. Soc Sci Med. 2018;214:206–13.
Schott WB, Crookston BT, Lundeen EA, Stein AD, Behrman JR. Periods of child growth up to age 8 years in Ethiopia, India, Peru and Vietnam: key distal household and community factors. Soc Sci Med. 2013;97:278–87.
Desmond C, Casale D. Catch-up growth in stunted children: Definitions and predictors. PLoS ONE. 2017;12(12): e0189135.
Lundeen EA, Stein AD, Adair LS, Behrman JR, Bhargava SK, Dearden KA, Gigante D, Norris SA, Richter LM, Fall CH, et al. Height-for-age z scores increase despite increasing height deficits among children in 5 developing countries. Am J Clin Nutr. 2014;100(3):821–5.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339: b2700.
Fantom NJ, Serajuddin U: The World Bank's Classification of Countries by Income. World Bank Policy Research Working Paper Series 2016.
Brooks BL, Sherman EMS, Strauss E. NEPSY-II: A Developmental Neuropsychological Assessment. Second Edition Child Neuropsychol. 2009;16(1):80–101.
Gomez R, Vance A, Watson SD: Structure of the Wechsler Intelligence Scale for Children - Fourth Edition in a Group of Children with ADHD. Front Psychol 2016, 7:737.
Balasundaram P, Avulakunta ID: Bayley Scales Of Infant and Toddler Development: StatPearls Publishing, Treasure Island (FL); 2022.
Lamsal R, Dutton DJ, Zwicker JD. Using the ages and stages questionnaire in the general population as a measure for identifying children not at risk of a neurodevelopmental disorder. BMC Pediatr. 2018;18(1):122.
Srinithiwat B, Ularntinon S: Concurrent validity of the Ages & Stages Questionnaires, Third Edition, Thai-version (ASQ-3 Thai) with the Denver Developmental Screening Test II (DDST-II) in developmental screening of 18, 24, and 30 months old children at Queen Sirikit National Institute of Child Health. J Med Assoc Thai 2014, 97 Suppl 6:S6–13.
Goriot C, van Hout R, Broersma M, Lobo V, McQueen James M, Unsworth S. Using the peabody picture vocabulary test in L2 children and adolescents: effects of L1. Int J Biling Educ Biling. 2021;24(4):546–68.
Clark DA, Donnellan MB, Durbin CE, Brooker RJ, Neppl TK, Gunnar M, Carlson SM, Le Mare L, Kochanska G, Fisher PA, et al. Using item response theory to evaluate the Children’s Behavior Questionnaire: Considerations of general functioning and assessment length. Psychol Assess. 2020;32(10):928–42.
Covidence systematic review software, Veritas Health Innovation, Melbourne, Australia. Available at https://www.covidence.org.
Effective Practice and Organisation of Care (EPOC). EPOC Resources for review authors. 2017. Available at: https://epoc.cochrane.org/resources/epoc-resources-review-authors.
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.3 (updated February 2022). Cochrane, 2022. Available from https://www.training.cochrane.org/handbook.
Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34.
Wells G, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa (NOS) for assessing the quality of nonrandomized studies in meta-analysis. Ottawa: Ottawa Hospital Research Institute. Available from: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
Cheung Y, Ashorn P. Continuation of linear growth failure and its association with cognitive ability are not dependent on initial length-for-age: a longitudinal study from 6 months to 11 years of age. Acta Paediatr. 2010;99(11):1719–23.
Yang S, Tilling K, Martin R, Davies N, Ben-Shlomo Y, Kramer MS. Pre-natal and post-natal growth trajectories and childhood cognitive ability and mental health. Int J Epidemiol. 2011;40(5):1215–26.
Pongcharoen T, Ramakrishnan U, DiGirolamo AM, Winichagoon P, Flores R, Singkhornard J, Martorell R. Influence of prenatal and postnatal growth on intellectual functioning in school-aged children. Arch Pediatr Adolesc Med. 2012;166(5):411–6.
Berkman DS, Lescano AG, Gilman RH, Lopez SL, Black MM. Effects of stunting, diarrhoeal disease, and parasitic infection during infancy on cognition in late childhood: a follow-up study. Lancet. 2002;359(9306):564–71.
Crookston BT, Penny Me Fau - Alder SC, Alder Sc Fau - Dickerson TT, Dickerson Tt Fau - Merrill RM, Merrill Rm Fau - Stanford JB, Stanford Jb Fau - Porucznik CA, Porucznik Ca Fau - Dearden KA, Dearden KA. Children who recover from early stunting and children who are not stunted demonstrate similar levels of cognition. (1541–6100 (Electronic)).
Mo-Suwan L, Intusoma U, Sangsupawanich P. AGE AT HEIGHT CATCH-UP AFFECTS THE COGNITIVE OUTCOME OF STUNTED CHILDREN: A BIRTH COHORT STUDY. Eur J Pediatr. 2016;175:1393–880.
Nguyen PA-O, Tran LM, Khuong LQ, Young MA-O, Duong TH, Nguyen HC, DiGirolamo AM, Martorell RA-O, Ramakrishnan UA-O. Child Linear Growth During and After the First 1000 Days Is Positively Associated with Intellectual Functioning and Mental Health in School-Age Children in Vietnam. (1541–6100 (Electronic)).
Ocansey MA-O, Adu-Afarwuah SA-O, Kumordzie SM, Okronipa HA-O, Young RR, Tamakloe SM, Oaks BM, Arimond MA-O, Dewey KG, Prado EA-OX. The association of early linear growth and haemoglobin concentration with later cognitive, motor, and social-emotional development at preschool age in Ghana. (1740–8709 (Electronic)).
Poveda NA-OX, Hartwig FA-O, Victora CA-O, Adair LA-O, Barros FA-O, Bhargava SK, Horta BA-OX, Lee NR, Martorell RA-O, Mazariegos MA-O, et al. Patterns of Growth in Childhood in Relation to Adult Schooling Attainment and Intelligence Quotient in 6 Birth Cohorts in Low- and Middle-Income Countries: Evidence from the Consortium of Health-Oriented Research in Transitioning Societies (COHORTS). (1541–6100 (Electronic)).
Upadhyay RP, Hysing M, Taneja S, Kvestad I, Bhandari N, Strand TA. Linear Growth between Early and Late Childhood and Cognitive Outcomes at 6–9 Years of Age. (1097–6833 (Electronic)).
Prado EL, Sebayang SK, Adawiyah SR, Alcock KJ, Ullman MT, Muadz H, Shankar AH. Maternal depression is the predominant persistent risk for child cognitive and social-emotional problems from early childhood to pre-adolescence: A longitudinal cohort study. Soc Sci Med. 2021;289: 114396.
Fink G, Rockers PC. Childhood growth, schooling, and cognitive development: further evidence from the Young Lives study. Am J Clin Nutr. 2014;100(1):182–8.
Sunny BA-O, DeStavola B, Dube A, Kondowe S, Crampin AC, Glynn JR. Does early linear growth failure influence later school performance? A cohort study in Karonga district, northern Malawi. (1932–6203 (Electronic)).
Adair LS, Fall CHD, Osmond C, Stein AD, Martorell R, Ramirez-Zea M, Sachdev HS, Dahly DL, Bas I, Norris SA, et al. Associations of linear growth and relative weight gain during early life with adult health and human capital in countries of low and middle income: findings from five birth cohort studies. The Lancet. 2013;382(9891):525–34.
Crookston BT, Schott W Fau - Cueto S, Cueto S Fau - Dearden KA, Dearden Ka Fau - Engle P, Engle P Fau - Georgiadis A, Georgiadis A Fau - Lundeen EA, Lundeen Ea Fau - Penny ME, Penny Me Fau - Stein AD, Stein Ad Fau - Behrman JR, Behrman JR. Postinfancy growth, schooling, and cognitive achievement: Young Lives. (1938–3207 (Electronic)).
Gandhi M, Ashorn P, Maleta K, Teivaanmäki T, Duan X, Cheung YB. Height gain during early childhood is an important predictor of schooling and mathematics ability outcomes. Acta Paediatr. 2011;100(8):1113–8.
Glewwe P, King EM. The Impact of Early Childhood Nutritional Status on Cognitive Development: Does the Timing of Malnutrition Matter? World Bank Econ Rev. 2001;15(1):81–113.
Fox SE, Levitt P Fau - Nelson CA, 3rd, Nelson CA, 3rd: How the timing and quality of early experiences influence the development of brain architecture. (1467–8624 (Electronic)).
Martorell R: Improved nutrition in the first 1000 days and adult human capital and health. Am J Hum Biol 2017, 29(2).
Darling JC, Bamidis PD, Burberry J, Rudolf MCJ. The First Thousand Days: early, integrated and evidence-based approaches to improving child health: coming to a population near you? Arch Dis Child. 2020;105(9):837–41.
Cusick SE, Georgieff MK. The Role of Nutrition in Brain Development: The Golden Opportunity of the “First 1000 Days.” J Pediatr. 2016;175:16–21.
Prado EL, Larson LM, Cox K, Bettencourt K, Kubes JN, Shankar AH. Do effects of early life interventions on linear growth correspond to effects on neurobehavioural development? A systematic review and meta-analysis. Lancet Glob Health. 2019;7(10):e1398–413.
Acknowledgements
Not applicable.
Funding
No funding was obtained for this study.
Author information
Authors and Affiliations
Contributions
Ravi Prakash Upadhyay and Barsha Gadapani Pathak contributed equally to the first authorship. Ravi Prakash Upadhyay conceptualized the scientific question, performed the statistical analysis, drafted the manuscript, revised the manuscript based on important intellectual inputs from co-authors, and performed the overall coordination. Barsha Gadapani Pathak framed the search strategy, performed data extraction, and quality assessment of studies, conducted the statistical analysis, prepared Figs. 1, 2, 3, 4 and 5, Table 1, and provided inputs in drafting the manuscript. Shrish Vijaykumar Raut, Dilesh Kumar, and Diksha Singh framed the search strategy, conducted the search for eligible studies, provided inputs in drafting the manuscript. Sunita Taneja and Nita Bhandari provided administrative coordination, arranged for resources, provided technical inputs, and critically reviewed the manuscript for important intellectual content. Christopher R. Sudfeld and Tor A. Strand conceptualized the study question, reviewed the analysis, provided inputs on the interpretation of the findings, and reviewed the manuscript. All authors provided important intellectual content and approved the final manuscript as submitted. The authors agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplementary Box 1.
Search Strategy used for identifying relevant studies for the meta-analysis. Supplementary Table1. Summary of the included studies. Supplementary Table 2. Assessment of quality of the included cohort studies. Fig S1. Funnel plot for change in height-for-age z scores over time with cognitive scores. Fig S2. Funnel plot for recovery from stunting with cognitive scores. Fig S3. Funnel plot for change in height-for-age z scores over time with socioemotional scores. Fig S4. Funnel plot for change in height-for-age z scores over time with verbal scores. Fig S5. Sensitivity analysis for association of change in height for age z-score (HAZ), post the first 2 years of age, with cognitive scores in middle to late childhood. Fig S6. Sensitivity analysis for association of recovery from stunting with cognitive, post the first 2 years of age, compared to children who were never stunted. Fig S7. Sensitivity analysis for association of change in height for age z-score (HAZ), post the first 2 years of age, with socio-emotional scores in middle to late childhood. Fig S8. Sensitivity analysis for association of change in height for age z-score (HAZ), post the first 2 years of age, with language scores in middle to late childhood. Fig S9. Baseline age of the height/length for age (HAZ/LAZ) assessment among the included studies.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Upadhyay, R.P., Pathak, B.G., Raut, S.V. et al. Linear growth beyond 24 months and child neurodevelopment in low- and middle-income countries: a systematic review and meta-analysis. BMC Pediatr 24, 101 (2024). https://doi.org/10.1186/s12887-023-04521-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-023-04521-0