Abstract
Background
It is still controversial for neonates or children to choose normal saline or heparin solution in the care of peripheral intravenous catheters. This meta-analysis aimed to evaluate the effects of heparin versus normal saline for the care of peripheral intravenous catheters in pediatrics, to provide reliable evidence support for clinical care.
Methods
Two authors searched the PubMed, EMbase, Ovid Medline, Cochrane Library, Web of Science, CBM, WanFang Data and China National Knowledge Infrastructure (CNKI) databases for randomized controlled trial (RCT) of heparin versus normal saline for the care of peripheral intravenous catheters in pediatrics until July 16, 2023. The bias of risk tool recommended by Cochrane was used for the quality evaluation of included RCTs. Meta-analysis was carried out by using RevMan 5.4 software.
Results
A total of 22 RCTs involving 3988 peripheral intravenous catheters were finally included. Compare with normal saline, heparin could significantly increase the catheter indwelling time (MD = 9.10, 95%CI:3.30 ~ 14.90). Subgroup analysis indicated that for compare with normal saline, heparin could significantly increase the catheter indwelling time in the neonate (MD = 9.63, 95%CI: 0.38 ~ 18.88) and neonate + children population (MD = 6.22, 95%CI:2.72 ~ 9.73, P < 0.001). Heparin could significantly reduce the incidence of catheter-associated complications (RR = 0.84, 95%CI: 0.70 ~ 0.95). Subgroup analysis indicated that heparin could significantly reduce the incidence of catheter-associated complications in the neonate (RR = 0.70, 95%CI: 0.61 ~ 0.89). There was no publication bias amongst the synthesized outcomes by Egger’s test (all P > 0.05).
Conclusions
Heparin may be worthy of being applicated in the neonate population in terms of prolonged indwelling time and less complications. Limited by the evidence quality, more studies from different area and populations with rigorous design are needed to investigate the role of heparin versus normal saline for the care of peripheral intravenous catheters in pediatrics.
Similar content being viewed by others
Introduction
Peripheral intravenous catheter is the most commonly used peripheral indwelling needle in clinical nursing practice [1]. The peripheral intravenous catheter is a transfusion device with a length of 2 to 6 cm through the peripheral vein, and the end of the catheter is located in the peripheral vein [2]. Peripheral venous catheter is mainly used for clinical short-term drug infusion, but due to the uncertain direction of blood vessels in different stages of children’s growth and development, differences in puncture techniques and whether it is effective to flush and lock the catheter, it is easy to have related complications after indwelling peripheral venous catheter, such as phlebitis, drug solution exudation, catheter blockage, which eventually lead to the removal of the catheter and increase the pain of re-puncture and medical expenses [3,4,5]. It has been reported that the obstruction rate of peripheral intravenous catheters can be as high as 60.55% after 48 h use [6]. Once the obstruction occurs in peripheral intravenous catheters, clinical nurses will generally choose to remove it directly, which may increase the cost of medical equipment of patients [7, 8]. Therefore, the effective and safe nursing care measures for peripheral intravenous catheters are very important in clinical practice.
Currently, there is still controversy about which kind of liquid to choose for peripheral venous catheter care [9]. The commonly used clinical nursing care for lock solution is normal saline and different concentrations of heparin solution [10]. Normal saline can maintain extracellular fluid volume and osmotic pressure, which is closely related to the balance of sodium and water in the body and blood circulation. Its advantage is that the use is not limited by the type of disease. It is especially suitable for patients with bleeding tendency, disturbance of blood coagulation mechanism and insufficiency of liver and kidney [11]. Heparin sodium is a highly effective anticoagulant, it has been reported that heparin sodium can reduce venous thrombosis and maintain vascular patency [12].
At present, there are more and more studies on the lock effect of indwelling needle, but no consensus has been reached on which kind of lock solution can reduce the incidence of blockage and phlebitis and prolong the indwelling time. In the latest nursing practice guide for intravenous infusion, there is no clear recommendation on which solution (normal saline or heparin solution) for newborns or children to lock the catheter [9, 13]. Therefore, this study systematically searched the related literatures and aimed to evaluate the effects and safety of heparin versus normal saline for the care of peripheral intravenous catheters in pediatrics, to provide useful evidence for the clinical nursing care.
Methods
This study was performed according to the preferred reporting items for systematic review and meta-analysis (PRISMA) statement [14]. Because this study was a meta-analysis, there was no need for ethical approval and patients’ informed consent.
Inclusion and exclusion criteria
The inclusion criteria of randomized controlled trial (RCT) in this meta-analysis were: study type: RCT design. Population: Newborns to adolescents who need to indwelling peripheral venous catheters for intravenous infusion with age younger than or equal to 18 years old. Intervention: Nursing care of venous catheter sealing with heparin solution compared with 0.9% normal saline. Outcome indicators: primary outcome indicators: catheter indwelling time. Secondary outcome indicators: catheter-associated complications including phlebitis, drug extravasation and catheter blockage. The exclusion criteria for this meta-analysis were as follows: non- Chinese and English literatures; repeatedly published studies; articles that did not have access to full text or required data.
Search strategy
We searched the PubMed, EMbase, Ovid Medline, Cochrane Library, Web of Science, CBM, WanFang Data and China National Knowledge Infrastructure (CNKI) databases for RCTs of heparin versus normal saline for the care of peripheral intravenous catheters in pediatrics until July 16, 2023. The search strategies for this meta-analysis were as following: (“peripheral intravenous catheter” OR “peripheral indwelling needle” OR “PIVC” OR “catheter”) AND (“heparin” OR “normal saline” OR “NS” OR “flushing” OR “lock”) AND (“child” OR “children” OR “pediatric” OR “neonate” OR *infant” OR “newborn” OR “adolescent” OR “young adult”). The two authors searched the database independently and then imported it to the Endnote software for further analysis.
Literature screening and data extraction
In this meta-analysis, two evaluators independently conducted literature screening and data extraction, and cross-checked for accuracy. If there were differences, they would discuss and solve them for consensus. This meta-analysis used a pre-developed data extraction table to extract data, including: (1) the basic information included in the study, including the research topic, the name of the author, the journal published, the number of years published.; (2) the baseline characteristics of the study population, including the number of cases, gender, age, settings; (3) the specific details of the intervention measures; (4) the key elements of bias risk assessment; (5) the outcome data concerned.
Bias risk assessment
Two researchers independently evaluated the bias risk in the study and cross-checked the results. The bias risk assessment tool recommended by Cochrane library was used for the quality evaluation of included studies [15]. The tool included seven items: random sequence generation (selection bias), allocation concealment (selection bias), blinding of participants and personnel (performance bias), blinding of outcome assessment (detection bias), incomplete outcome data (attrition bias), selective reporting (reporting bias) and other bias. Every item could be rated as “high risk of bias”, “low risk of bias” and “unclear risk of bias”.
GRADE evidence assessment
The GRADE grading system [16] was used to evaluate the evidence quality of the outcome index, and the evidence quality was divided into four levels: high, medium, low and very low. The evidence quality grade of the outcome index was evaluated mainly from the bias of risk, inconsistency, indirectness, inaccuracy and publication bias of included RCTs.
Statistical analysis
The meta-analysis was carried out by using RevMan 5.4 software. Mean difference (MD) or standardized mean difference (SMD) were used as effect analysis statistics, and 95% confidence interval (CI) was calculated for each effect. The heterogeneity among the included results was analyzed by χ2 test (the test level was α = 0.1). At the same time, the heterogeneity was quantitatively judged by I2. If there was no statistical heterogeneity among the results of each study, the fixed effect model was used for meta-analysis. If there was statistical heterogeneity among the results, the source of heterogeneity was further analyzed. After excluding the obvious clinical heterogeneity, the random effect model was used for meta-analysis. The obvious clinical heterogeneity was treated by subgroup analysis or sensitivity analysis. Publication bias was evaluated by funnel plots and Egger’s test. The significance level for all the analysis was α = 0.05.
Results
Literature retrieval
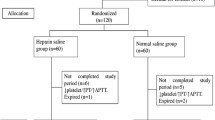
In this study, a total of 217 related literatures were obtained in the initial search, and 22 RCTs [17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38] were finally included after layer-by-layer screening. The literature screening process and results are shown in Fig. 1.
Characteristics of RCTs
As presented in Table 1, of the included 22 RCTs, 18 articles were reported from developed countries and regions, 4 articles from developing countries. 13 articles were published before 2000, 4 articles were published in 2000–2010, 5 articles were published in 2010 ~ 2023. The dose of heparin in RCTs varied from 0.5 to 10 U mL− 1, and the lock frequency of peripheral intravenous catheters remained different amongst included RCTs.
Quality of included RCTs
As presented in Figs. 2, 3 and 15 RCTs reported the detailed methods for random sequence generation. 6 RCTs reported the details of allocation concealment. No reports on the blinding of participants and personnel were found. 2 RCTs reported the design on the blinding of outcome assessment, no risk of bias in the incomplete outcome data, selective reporting and other bias were found.
Meta-analysis
19 RCTs reported the catheter indwelling time. As shown in Fig. 4, meta-analysis indicated that compared with normal saline, heparin could significantly increase the catheter indwelling time (MD = 9.10, 95%CI:3.30 ~ 14.90, P = 0.002). As presented in Table 2, subgroup analysis indicated that for compare with normal saline, heparin could significantly increase the catheter indwelling time in the neonate (MD = 9.63, 95%CI:0.38 ~ 18.88, P = 0.042) and neonate + children population(MD = 6.22, 95%CI:2.72 ~ 9.73, P < 0.001), no effect difference in the catheter indwelling time in the children population(MD = 6.94, 95%CI: -1.27 ~ 15.15, P = 0.100) were found.
19 RCTs reported the incidence of catheter-associated complications. As shown in Table 3, meta-analysis indicated that compare with normal saline, heparin could significantly reduce the incidence of catheter-associated complications (RR = 0.84, 95%CI: 0.70 ~ 0.95, P = 0.002). Subgroup analysis indicated that for compare with normal saline, heparin could significantly reduce the incidence of catheter-associated complications in the neonate (RR = 0.70, 95%CI: 0.61 ~ 0.89, P = 0.004). No effect differences in the catheter indwelling time in the children population (RR = 0.94, 95%CI: 0.62 ~ 1.41, P = 0.751) and neonate + children population (RR = 0.98, 95%CI: 0.71 ~ 1.33, P = 0.904) were found.
This study used the method of removing individual studies one by one for sensitivity analysis, the results showed that there was no significant change, suggesting that the results of this study were stable.
The funnel plot (Fig. 5) and results of Egger’s test of publication bias showed that the possibility of publication bias was small (All P > 0.05).
Evidence quality
As indicated in Table 4, the evidence on the catheter indwelling time was in middle level, and the evidence on the incidence of catheter-associated complications was in low level.
Discussions
Peripheral intravenous catheter is one of the most commonly used venous pathways in clinical practice. At present, the clinical lock solution for peripheral intravenous catheters has a portable solution of 0.9% normal saline, which can greatly reduce the workload and working time of clinical nurses, but the lock solution of peripheral intravenous catheters is also a controversial topic in clinical care [39, 40]. The previous systematic review [41] has shown that heparin cannot prolong the use of peripheral intravenous catheter compared with normal saline. However, the other systematic review [40] has reported that the use of heparin is beneficial to significantly prolong the use of peripheral intravenous catheters and reduce the incidence of complications. The above completely different conclusions may be related to the number of literatures included and the different concentrations of heparin infusion. With more RCTs included, the results of this meta-analysis have found that heparin have more advantages over normal saline for the care of peripheral intravenous catheter in indwelling time and the incidence of catheter-associated complications. Heparin may be more appropriate for the clinical care practice of peripheral intravenous catheters in pediatrics.
The application of peripheral intravenous catheters greatly satisfies the patients who need short-term infusion. Heparin sodium is a kind of acidic mucopolysaccharide and has strong anticoagulant effect both in vivo and in vitro [42]. Therefore, it can effectively reduce the blood flowing back into the indwelling needle to form blood clots and block the pipeline, which is widely used in clinical care. Sealing the tube with heparin can effectively reduce the incidence of blockage and shorten the time of blockage, so as to reduce the replacement of patients due to the blockage of indwelling needle, reduce the pain of puncture, and achieve the saving of medical resources in a certain range [43,44,45].
It must be noted that two included RCTs have reported that intracranial hemorrhage is associated with the use of heparin. There is no significant difference in the incidence of intracranial hemorrhage between heparin and saline, but it still needs clinical attention. Besides, two included RCTs reported the occurrence of thrombocytopenia induced by heparin. Although there is no significant difference in thrombocytopenia induced by heparin the between heparin and normal saline, it was still necessary to detect the corresponding clinical indexes when using heparin in children with contraindications of heparin. Some scholars [46, 47] have reported that normal saline is safer than heparin sodium in patients with cardiovascular diseases, gastrointestinal bleeding and hematological diseases. Therefore, the lock solution can be used reasonably according to the specific conditions of the pediatrics [48].
There are several limitations of this study must be considered. Firstly, the RCTs included in this meta-analysis have been published for a relatively long time. With the development of materials and technology, there may be some differences in the quality and design of peripheral intravenous catheters. Secondly, there are very high statistical heterogeneity (I2 = 92%) in the synthesized outcome, which may be related to the wide age range of the participants, the different underlying diseases whose treatments might interfere with coagulation, the different characteristics of the prescriptions, the frequency of use, and the very different concentrations of heparin sodium. Most of the RCTs reports included in this meta-analysis are from developed countries, and there is still a lack of relevant report data from developing countries. Future studies with larger sample size from different area and populations are needed. Finally, most of the RCT studies included in this paper do not mention blind setting and allocation concealment. It is suggested that future studies should further improve the RCT design.
Conclusions
In summary, in the selection of lock solution of peripheral intravenous catheters in children, heparin saline can effectively prolong the indwelling time of peripheral intravenous catheters and reduce the incidence of related complications than normal saline. However, the evidence quality is not high, the findings should be treated with cautions. Under the circumstances of the shortage of medical resources and human resources of pediatric nurses, heparin may be recommended to the care of peripheral intravenous catheters in pediatrics when the children do not have blood coagulation dysfunction in clinical nursing care, which may effectively prolong the use of indwelling catheter and reduce the pain caused by repeated puncture.
Data availability
All data generated or analyzed during this study are included in this published article. The original data will be available from corresponding authors on reasonable request.
Abbreviations
- PRISMA:
-
Preferred reporting items for systematic review and meta-analysis
- RCT:
-
Randomized controlled trial
- NICU:
-
Neonatal intensive care unit
- PICU:
-
Pediatric intensive care unit
- MD:
-
Mean difference
- SMD:
-
Standardized mean difference
- CI:
-
Confidence interval
References
Alberto EC, Mastrianni A, Sullivan TM, McCarthy KH, Milestone ZP, Chung L, Cha N, Mapelli E, Sippel GJ, Marsic I, et al. Factors affecting Peripheral Intravenous Catheter Placement during Pediatric Trauma Resuscitation. J Surg Res. 2023;28(3):241–8.
Simeone S, Gargiulo G, Bosco V, Mercuri C, Botti S, Candido S, Paonessa G, Bruni D, Serra N, Doldo P. Peripheral intravenous catheter insertion and therapy administration: simulator learning. Acta Biomed. 2023;94(3):e2023130.
Shimoni Z, Houdhoud N, Isaacs Y, Froom P. Observational study of peripheral intravenous catheter outcomes in an internal medicine department. Intern Med J. 2023;53(2):221–7.
Indarwati F. Site selection and incidence of peripheral intravenous catheter complications. Evid Based Nurs. 2023;26(3):106–12.
Hontoria-Alcoceba R, López-López C, Hontoria-Alcoceba V, Sánchez-Morgado AI. Implementation of evidence-based practice in Peripheral Intravenous Catheter Care. J Nurs Care Qual. 2023;38(3):226–33.
Huang X, Quan X, Pu W. Investigation and analysis of standardized nursing management on the application of clinical peripheral superficial vein indwelling needle. Chin Contemp Nurses. 2022;26(7):4–6.
Wang G. Progress in clinical application of peripheral intravenous catheter. Mod Diagnosis Treat. 2023;34(10):1569–72.
Qiu J, Li Y, Zhang K, Jiang Y. Investigation on the use of peripheral venous indwelling needle in newborns. Chinesee Contemp Nurses. 2021;31(15):32–4.
Gorski LA, Hadaway L, Hagle ME, Broadhurst D, Clare S, Kleidon T, Meyer BM, Nickel B, Rowley S, Sharpe E, et al. Infusion Therapy standards of Practice, 8th Edition. J Infus Nurs. 2021;44(1):1–224.
children Wgoe-bgfcpoiiti. Evidence-based guidelines for clinical practice of intravenous infusion therapy in children. Chin J evidence-based Pediatr. 2021;16(1):1–142.
Wu X-H, Chen L-C, Liu G-L, Zhang T-T, Chen X-S. Heparin versus 0.9% saline solution to maintain patency of totally implanted venous access ports in cancer patients: a systematic review and meta-analysis. Int J Nurs Pract. 2021;27(2):e12913.
Sharma SK, Mudgal SK, Gaur R, Sharma R, Sharma M, Thakur K. Heparin flush vs. normal saline flush to maintain the patency of central venous catheter among adult patients: a systematic review and meta-analysis. J Family Med Prim Care. 2019;30(8):2779–92.
Pittiruti M, Boxtel TV, Scoppettuolo G, Carr P, Konstantinou E, Miluy GO, Lamperti M, Goossens GA, Simcock L, Dupont C, et al. European recommendations on the proper indication and use of peripheral venous access devices (the ERPIUP consensus): a WoCoVA project. J Vasc Access. 2023;24(1):165–82.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;29(6):372–80.
Higgins JPT, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JAC, et al. The Cochrane collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343(18):d5928.
Guyatt GH, Oxman AD, Schunemann HJ, Tugwell P, Knottnerus A. GRADE guidelines: a new series of articles in the Journal of Clinical Epidemiology. J Clin Epidemiol. 2011;64(4):380–2.
Alpan G, Eyal F, Springer C, Glick B, Goder K, Armon J. Heparinization of alimentation solutions administered through peripheral veins in premature infants: a controlled study. Pediatrics. 1984;74(3):375–8.
Brown K, Tay-Uyboco JS, McMillan DD. Heparin is not required for peripheral intravenous locks in neonates. Paediatr Child Health. 1999;4(1):39–42.
Heilskov J, Kleiber C, Johnson K, Miller J. A randomized trial of heparin and saline for maintaining intravenous locks in neonates. J Soc Pediatr Nurs. 1998;3(3):111–6.
Klenner AF, Fusch C, Rakow A, Kadow I, Beyersdorff E, Eichler P, Wander K, Lietz T, Greinacher A. Benefit and risk of heparin for maintaining peripheral venous catheters in neonates: a placebo-controlled trial. J Pediatr. 2003;143(6):741–5.
Upadhyay A, Verma KK, Lal P, Chawla D, Sreenivas V. Heparin for prolonging Peripheral Intravenous Catheter Use in neonates: a randomized controlled trial. J Perinatol. 2015;35(4):274–7.
White ML, Crawley J, Rennie EA, Lewandowski LA. Examining the effectiveness of 2 solutions used to flush capped pediatric peripheral intravenous catheters. J Infus Nurs. 2011;34(4):260–70.
Tripathi S, Kaushik V, Singh V. Peripheral IVs: factors affecting complications and patency–a randomized controlled trial. J Infus Nurs. 2008;31(3):182–8.
Treas LS, Latinis-Bridges B. Efficacy of heparin in peripheral venous infusion in neonates. J Obstet Gynecol Neonatal Nurs. 1992;21(3):214–9.
Sun Y. Comparison of the effect of two kinds of sealing solution in neonatal peripheral venous catheterization. China Maternal and Child Health Research. 2016;36(2):2–4.
Schultz AA, Drew D, Hewitt H. Comparison of normal saline and heparinized saline for patency of IV locks in neonates. Appl Nurs Res. 2002;15(1):28–34.
Paisley MK, Stamper M, Brown J, Brown N, Ganong LH. The use of heparin and normal saline flushes in neonatal intravenous catheters. Pediatr Nurs. 1997;23(5):521–7.
Nelson TJ, Graves SM. 0.9% sodium chloride injection with and without heparin for maintaining peripheral indwelling intermittent-infusion devices in infants. Am J Health Syst Pharm. 1998;55(6):570–3.
Mudge B, Forcier D, Slattery MJ. Patency of 24-gauge peripheral intermittent infusion devices: a comparison of heparin and saline flush solutions. Pediatr Nurs. 1998;24(2):142–9.
Mok E, Kwong TKY, Chan MF. A randomized controlled trial for maintaining peripheral intravenous lock in children. Int J Nurs Pract. 2007;13(1):33–45.
Moclair A, Bates I. The efficacy of heparin in maintaining peripheral infusions in neonates. Eur J Pediatr. 1995;154(7):567–70.
McMullen A, Fioravanti ID, Pollack V, Rideout K, Sciera M. Heparinized saline or normal saline as a flush solution in intermittent intravenous lines in infants and children. MCN Am J Matern Child Nurs. 1993;18(2):78–85.
Kotter RW. Heparin vs saline for intermittent intravenous device maintenance in neonates. Neonatal Netw. 1996;15(6):43–7.
Kleiber C, Hanrahan K, Fagan CL, Et A. Heparin Vs. saline for peripheral I. V. Locks in children. Pediatr Nurs. 1993;19(4):405–9.
John S, Vetriselvi. Comparison of efficacy of normal saline with heparinised saline flushing on patency of Peripheral Intravenous Catheters-A Randomized double blind clinical trial. Int J Curr Res. 2015;7(11):23286–90.
Goldberg M, Givelichian L, Sankaran K. Maintaining patency of peripheral infusion Devices with saline and heparinized saline. A Randomized Control Trial. Pediatr Res. 1999;11(3):6–14.
Beecroft P, Bossert E, Chung K. Intravenous lock patency in children: dilute heparin versus saline. Pediatrics. 1997;15(3):10–7.
Arnts IJJ, Heijnen JA, Wilbers HTM, Wilt G-J, Groenewoud JMM, Liem KD. Effectiveness of heparin solution versus normal saline in maintaining patency of intravenous locks in neonates: a double blind randomized controlled study. J Adv Nurs. 2011;67(12):2677–85.
Thorpe M, Berry W, Soper J. Duration of peripheral intravenous catheter patency in children. Paediatr Child Health. 2020;26(1):32–4.
Kumar M, Vandermeer B, Bassler D, Mansoor N. Low-dose heparin use and the patency of peripheral IV catheters in children: a systematic review. Pediatrics. 2013;131(3):864–72.
Shah PS, Ng E, Sinha AK. Heparin for prolonging peripheral intravenous catheter use in neonates. Cochrane Database Syst Rev. 2005;19(4):CD002774.
You T, Jiang J, Chen J, Xu W, Xiang L, Jiao Y. Necessity of heparin for maintaining peripheral venous catheters: a systematic review and meta-analysis. Exp Ther Med. 2017;14(2):1675–84.
López-Briz E, Garcia VR, Cabello JB, Bort-Marti S, Sanchis RC, Burls A. Heparin versus 0.9% sodium chloride intermittent flushing for prevention of occlusion in central venous catheters in adults. Cochrane Database Syst Rev. 2014;8(10):CD008462.
López-Briz E, Garcia VR, Cabello JB, Bort-Martí S, Sanchis RC. Heparin versus 0.9% sodium chloride locking for prevention of occlusion in central venous catheters in adults. Cochrane Database Syst Rev. 2022;7(7):CD008462.
Wen Z, Shen M, Wang Z. Meta analysis of the effect of PICC irrigating with normal saline and heparin sodium. J Nurs. 2017;24(1):6–9.
Xie G, Huang X, Zou J. A comparative study on the effect of preflushing catheter irrigator and heparin sodium saline on intravenous BD indwelling needle sealing. Jilin Med. 2019;40(2):3–6.
Li S, Di Y. Meta analysis of sealing effects of different concentrations of heparin sodium and normal saline with peripheral venous indwelling needle in patients with ischemic stroke. Chin Maternal Child Health Res. 2017;40(16):2–6.
Wang W, Wang Y, Kang Q. Systematic evaluation and Meta analysis of heparin or normal saline prolonging the indwelling time of short peripheral venous catheters. Chin J evidence-based Pediatr. 2022;17(1):28–34.
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Contributions
RL, L Z designed research; R L, Q Z, N C, L Z conducted research; R L, Q Z, N C analyzed data; R L, Q Z wrote the first draft of manuscript; L Z had primary responsibility for final content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
In this study, all methods were performed in accordance with the relevant guidelines and regulations. There are no need for Ethics approval and consent to participate since the study was a meta-analysis.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Li, R., Zheng, Q., Chen, N. et al. Heparin versus normal saline for the care of peripheral intravenous catheters in pediatrics: a meta-analysis of randomized controlled trials. BMC Pediatr 24, 48 (2024). https://doi.org/10.1186/s12887-023-04515-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-023-04515-y